Mice without TAM receptor spontaneously develop IRBP-specific CD4+ T cells and are more susceptible to retinal autoantigen immunization. Immunization with IRBP or adoptive transfer of the IRBP-specific T cells from immunized mutants caused lymphocyte infiltration into the KO retina.
Abstract
Purpose.
TAM receptors are expressed mainly by dendritic cells and macrophages in the immune system, and mice lacking TAM receptors develop systemic autoimmune diseases because of inefficient negative control of the cytokine signaling in those cells. This study aims to test the susceptibility of the TAM triple knockout (tko) mice to the retina-specific autoantigen to develop experimental autoimmune uveoretinitis (EAU).
Methods.
TAM tko mice that were or were not immunized with interphotoreceptor retinoid-binding protein (IRBP) peptides were evaluated for retinal infiltration of the macrophages and CD3+ T cells by immunohistochemistry, spontaneous activation of CD4+ T cells, and memory T cells by flow cytometry and proliferation of IRBP-specific CD4+ T cells by [3H]thymidine incorporation assay. Ocular inflammation induced by IRBP peptide immunization and specific T cell transfer were observed clinically by funduscopy and confirmed by histology.
Results.
Tko mice were found to have less naive, but more activated, memory T cells, among which were exhibited high sensitivity to ocular IRBP autoantigens. Immunization with a low dose of IRBP and adoptive transfer of small numbers of IRBP-specific T cells from immunized tko mice caused the infiltration of lymphocytes, including CD3+ T cells, into the tko retina.
Conclusions.
Mice without TAM receptor spontaneously develop IRBP-specific CD4+ T cells and are more susceptible to retinal autoantigen immunization. This TAM knockout mouse line provides an animal model with which to study the role of antigen-presenting cells in the development of T cell–mediated uveitis.
The TAM family of receptor tyrosine kinases, made up of the three members Tyro3,1,2 Axl,3,4 and Mertk,5,6 has received much attention because of its regulatory roles in controlling dendritic cell (DC) cytokine signaling7 and macrophage phagocytosis.8 Two structurally closely related proteins, growth-arrest-specific 6 (Gas6) and protein S, have been identified as ligands of TAM family receptors.9 Gas6 is a gene specifically induced on growth arrest of cultured mouse fibroblasts10 and is a member of the vitamin K-dependent proteins,11 whereas protein S belongs to the protein C anticoagulation cascade and acts as a cofactor in the degradation of blood coagulation factors Va and VIIIa.12 Both proteins are expressed in the eye and function as ligands for their receptors.13
Mutation of all three receptors in mice (TAM tko mice) leads to autoimmune diseases affecting multiple organs.8,14 The clinical manifestations in TAM tko mice include splenomegaly, lymphocytic tissue infiltrates, glomerulonephritis, and capillary leakage. A wide spectrum of autoantibodies, including anti-DNA and anti-phosphatidyl lipid antibodies, has been detected.14 Each of the three gene mutations contributes to the severity of autoimmune dysfunction, with the Mertk mutation having the largest effect.8,14
Furthermore, a recent study on TAM signal transduction in DCs showed that the TAM receptor functions as a negative regulator in cytokine receptor signaling by inhibiting the toll-like receptor-induced production of proinflammatory cytokines, such as TNF-α, interleukin-6 (IL-6), and type I interferons.7 This inhibition results from upregulation of the expression of suppressor of cytokine signaling (SOCS) proteins SOCS-1 and SOCS-3, two master negative regulators in cytokine receptor signaling.7 Cells without TAM receptors show impaired SOCS production and thus impaired activation of the negative-feedback loop, maintaining the cell in a state of uncontrolled activation. Overactivation of TAM mutant DCs in response to pathogens stimulating innate immunity causes overreaction of the adaptive response and, subsequently, the development of systemic autoimmunity.7,14
Uveitis is a term used to describe uveal autoimmune disease in humans and accounts for approximate 10% of cases of legal blindness in the United States alone.15 Systemic autoimmune disorders frequently cause inflammation in the eye, especially posterior uveitis, which affects the back of the uveal tract16 and the retinal layer. An animal model of human uveitis can be induced by immunization with retinal autoantigens, such as interphotoreceptor retinoid-binding protein (IRBP), in complete Freund's adjuvant (CFA) and is termed experimental autoimmune uveoretinitis (EAU). Adoptive transfer of retinal antigen-specific T cells can also induce EAU.17 Uveitis is an inflammatory disease caused largely by T cell activity, and destruction of the target tissue causes irreversible damage to photoreceptors and loss of vision.18,19
In this study, we showed that mice lacking TAM receptors had high levels of activated CD4+ T cells, including those specific for IRBP. In addition, these mutant mice were more sensitive to immunization with retinal antigen and generated increased numbers of IRBP-specific CD4+ T cells. Immunization of TAM tko mice with a low dose of IRBP or adoptive transfer of lower than pathogenic number of the retinal antigen-specific T cells caused T-cell invasion and colonization of the tko host retina but failed to induce these effects in wild-type (WT) mice. These results show that TAM tko knockout mice can serve as a mouse model for studying the role of antigen-presenting cells (APCs) in the development of T cell–mediated retinal autoimmunity.
Materials and Methods
Animal and Reagents
The TAM gene knockout mice, which were created in a C57BL/6 and 129 mixed background,20 have been backcrossed into a wild-type pure C57BL/6 background for at least 11 generations in our laboratory. All animals were housed in a pathogen-free facility and handled according to the regulations of the Institutional Animal Care and Use Committee, and all procedures adhered to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Induction of EAU by Active Immunization
Female mice aged 6 to 8 weeks were immunized subcutaneously over six spots at the tail base and the flank with 150 to 250 μg human IRBP1–20 peptide (amino acids 1–20 of IRBP) in 0.2 mL of a 1:1 vol/vol emulsion in CFA containing Mycobacterium tuberculosis strain H37RA (2.5 mg/mL; Difco, Detroit, MI) 2 hours after intraperitoneal injection with Bordetella pertussis toxin (0.2 μg/mouse; Sigma-Aldrich, St. Louis, MO). Eyes for histologic EAU evaluation were harvested at days 0, 7, 14, and 21 after immunization, and paraffin-embedded sections were prepared for hematoxylin and eosin (H&E) and immunohistochemical staining.
Preparation of IRBP1–20–Specific T Cells
IRBP1–20–specific T cells for adoptive transfer of EAU were prepared as described previously.21 Briefly, B6 WT and TAM tko mice at 6 to 8 weeks of age were immunized with 150 μg IRBP1–20 in CFA per mouse, as described. Fourteen days later, total T cells were isolated from pooled spleens and draining lymph nodes (inguinal and iliac) by a nylon wool column filtration method and were expanded for 2 days on γ-irradiated syngeneic splenic cells as APCs in the presence of 10 μg/mL IRBP1–20 with T-cell/APC cell ratio of 4:1. The expanded IRBP-specific CD4+ T cells were then purified before transfer, using a mouse CD4+ T cell enrichment kit (EasySep Negative Selection; Stem Cell Technologies, Vancouver, BC, Canada) according to the manufacturer's instructions.
Induction of EAU by Adoptive Transfer of IRBP-Primed CD4+ T Cells
EAU was induced in naive WT and TAM tko mice by adoptive transfer of 1 × 106 IRBP1–20–specific CD4+ T cells, a much smaller number of donor cells than that used in previously described protocols.22,23 Clinical signs of uveitis were examined by funduscopy under a binocular microscope after pupil dilation using 0.5% tropicamide and 1.25% phenylephrine hydrochloride ophthalmic solutions. Funduscopy was performed during the posttransfer period of week 1 to week 8, and EAU was graded on a scale of 0 to 4 in half-point increments, as described previously.22 Histologic examination and immunohistochemistry using anti-CD3 antibodies (1:100; Dako, Carpinteria, CA) were performed on paraffin-embedded sections prepared from recipient mice 35 days after adoptive transfer.
Supplementary Material (http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.10-6700/-/DCSupplemental), including other routine experimental procedures such as flow cytometry, immunohistochemistry, TUNEL assay, T cell proliferation assays, statistical analysis, and four figures, can be found with this article online.
Results
Mertk Mutation in TAM tko Mice Causes Rapid Photoreceptor Degeneration and Lymphocyte Infiltration in Retina
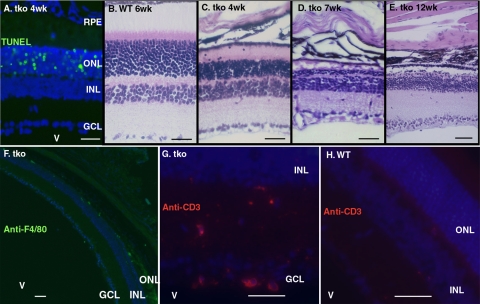
TAM tko mice show complete postnatal degeneration of a variety of tissues,20 including photoreceptors (Fig. 1A). This photoreceptor degeneration phenotype is similar to that of the Royal College Surgeons rat, in which Mertk was identified as the responsible gene.24 Degenerating photoreceptors release massive amounts of intracellular material that can be immunogenic.25 In response to these new antigens generated locally, lymphocyte invasion of the eyes was frequently detected, and infiltration lasted for the entire course of photoreceptor degeneration (Figs. 1B–E). Immunohistochemical studies showed that most of these infiltrated cells in the mutant mice were macrophages and some were T cells (reactive with F4/80 and CD3 antibodies, respectively; Figs. 1F, 1G).
Figure 1.
Lymphocytes infiltrate a degenerating TAM tko retina. (A) Horizontal section through the middle of the eye showing TUNEL+ ONL cells (green) in the naive tko retina at the age of 4 weeks (the same TUNEL staining pattern is seen in the Mertk single-mutant eye). (B–E) H&E–stained sections through the retinas of 6-week-old WT mice (B) and 4- (C), 7- (D, or 12- (E) week-old naive tko mice. (F, G) Eye sections from 7-week-old tko mice immunostained with antibodies against F4/80 (F) or CD3 (G) to show macrophage and T cell infiltration, respectively. (H) Age-matched WT eye section shows negative staining with anti-CD3 antibody. V, vitreous humor; INL, inner nuclear layer; GCL, ganglion cell layer. Scale bars, 80 μm.
CD4 T Cells Are Constantly Activated in Naive tko Mice with Characteristics of Decreased Naive, Increased Memory, and Activated T Cell Phenotypes
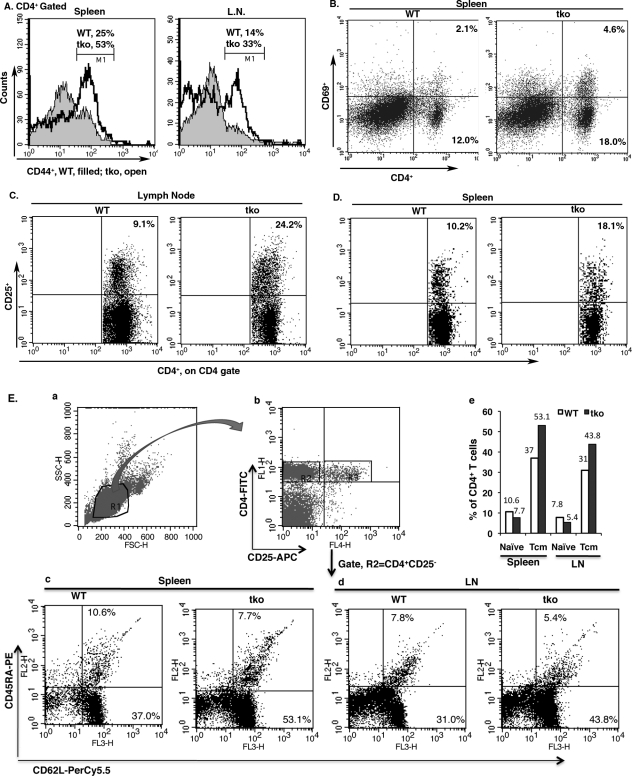
CD4 T cells play an important role in adaptive immune responses. Having engaged with self-antigen presented by major histocompatibility complex class II molecules on APCs and costimulatory receptors, naive CD4+ T cells become activated, as shown by the upregulation of three major surface markers—CD25, CD44, and CD69—which are commonly used for analysis of T cell activation. Therefore, we tested the activation status of the T cells in the tko mice. Consistent with our previous studies14 and the observed retinal infiltration of lymphocytes in the tko mice, we detected an activated phenotype of CD4 T cells in spleen and lymph nodes (inguinal, iliac, axillary, and submandibular) of young tko mice at approximately 4 to 5 weeks of age, with an increased frequency of CD4+CD44+ (Fig. 2A), CD4+CD69+ (Fig. 2B), and CD4+CD25+ T cells (Figs. 2C, 2D). On the other hand, the percentile of naive CD4 T cells, as identified by the CD4+CD25−CD62L+CD45RA+ phenotype,26 decreased in either spleen (Figs. 2Ec, 2Ee) or lymph nodes (Figs. 2Ed, 2Ee) of tko mice. Those results indicated that CD4+ T cells were overwhelmingly activated in the naive tko mice.
Figure 2.
CD4+ T cells are spontaneously activated in naive TAM tko mice. (A) Total lymphocytes from WT or tko spleens and lymph nodes were double-labeled with anti-CD4 and CD44 antibodies. The CD4+ cells (as shown in Supplementary Figure S1B, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.10-6700/-/DCSupplemental) were gated for further analysis of the CD44+ population. Histograms show the distributions and percentiles of the CD44high T cells from the CD4+-gated naive WT (solid) or tko (open) lymphocytes. The CD4 gate and no anti-CD44 controls are shown in Supplementary Figure S1B. (B) Dot plots show increased CD4+CD69+ double-positive cells in tko spleens (right, from WT 2.1% to tko 4.6%). (C, D) Dot plots show an increased CD4+CD25+ T cell population in the lymph nodes (C) and spleen (D) of tko mice, with the gate set on CD4+ T cells. The PE rat IgG2b k-isotype serves as a negative control for the PE-CD25 antibody, as shown in Supplementary Figures S1E–S1H (http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.10-6700/-/DCSupplemental). (A–D) Data are representative of those obtained from six mice in each genotype in three independent assays. (E) Young naive tko mice exhibited decreased naive and increased central memory T cells (Tcm). The pooled spleens and lymph nodes (inguinal, iliac, axillary, and submandibular) of three naive WT or tko female mice at ages of 4 to 5 weeks were prepared for single-cell suspension and stained with CD4-FITC, CD25-APC, CD62L-PerCp5.5, and CD45RA-PE antibodies. Viable lymphocytes were gated on FSC versus SSC dot plots (Ea) and were separated for the CD4+CD25− T cell population on CD4-FITC versus CD25-APC scattering dot plots (Eb). A second gate was then set on the CD4+CD25− T cell population for further analysis of CD62L and CD45RA subsets by CD62L-PerCy5.5 versus CD45RA-PE scattering dot plots (Ec, Ed). CD4+CD25−CD62L+CD45RA+ and CD4+CD25−CD62L+CD45RA− are naive (upper right) and central memory (Tcm, lower right) T cell subsets, respectively. The percentile numbers in the dot-plots are the average of two sets of independent assays (total, six mice) and are summarized in (Ee).
Rapid tissue (including photoreceptor) degeneration in tko mice occurs at approximately 3 weeks of age,13,20 and the newly released apoptotic materials may provoke naive CD4 T cells to differentiate into effectors, some of which can survive for a long period and become memory T cells. To determine whether increased memory T cells are present in tko mice, we analyzed the frequency of central memory T cells (Tcm) with a phenotypic CD4+CD25−CD62L+CD45RA− surface marker.26 The tko mice showed a higher frequency of the Tcm population in both spleen (Figs. 2Ec, 2Ee) and lymph node (Figs. 2Ed, 2Ee), suggesting that these mutant mice had previously been encountered with antigens.
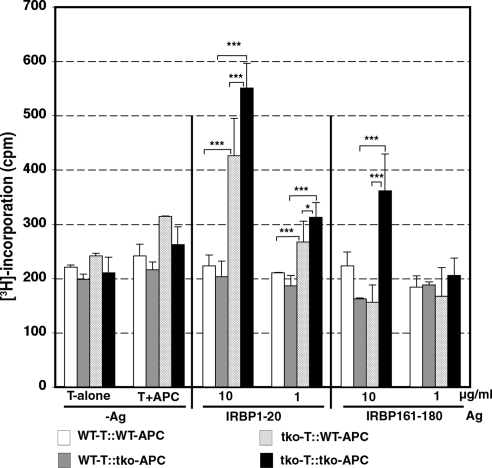
IRBP1–20–Specific T Cells Are Present in Naive tko Mice
Although we did not see massive T cell expansion and colonization in the naive tko retina, probably because of rapid loss of the entire outer nuclear layer (ONL) in which the photoreceptors are located, we indeed detected an increased frequency of memory CD4 T cells in tko peripheral lymph tissues (Fig. 2E). To determine whether the enhanced memory T cell population in tko mice contained retinal antigen-specific cells, we isolated T cells from the pooled spleens and lymph nodes of either WT or tko mice and tested their proliferation in response to two IRBP peptides, IRBP1–20 and IRBP161–180, presented by either WT or tko APCs. Unsurprisingly, neither WT nor mutant T cells proliferated in vitro in the absence of antigen (Fig. 3, left). However, the tko mouse T cells displayed antigen-specific responses to two antigens, and the responses were antigen dose dependent (Fig. 3, center and right, comparison between the 10- and 1-μg/mL groups). Consistent with the lower antigenicity of IRBP161–180 in the C56BL/6 strain, the response to this antigen was lower with T cells from these mice (Fig. 3, center and right, comparison between the IRBP1–20 and IRBP161–180 groups). Notably, tko T cells exhibited higher proliferation when cocultured with tko APCs (Fig 3, center and right, dark solid bars labeled tko-T::tko-APC) than those with the WT APCs (Fig. 3, center and right, light-dotted bars labeled tko-T::WT-APC). T cells from naive WT mice (negative control) showed no response to either antigen.
Figure 3.
IRBP-specific T cells are present in naive TAM tko mice. The T cells (4 × 104) used for each [3H]thymidine incorporation assay were isolated from pooled spleens and lymph nodes (inguinal, iliac, axillary, and submandibular) of three naive WT or tko female mice at ages of 6 to 8 weeks by the nylon wool column filtration method and were expanded for 72 hours on γ-irradiated syngeneic splenic APCs (1 × 105) in the medium containing no antigen (-Ag, left) or IRBP1–20 (center) or IRBP161–180 (right) at concentrations of 1 and 10 μg/mL. The WT T cells were cocultured with either WT APCs (WT-T::WT-APCs) or tko APCs (WT-T::tko-APCs), and the tko T cells were also plated on either WT APCs (tko-T::WT-APCs) or tko APCs (tko-T::tko-APCs). In the last 8 hours of coculture, 0.5 μCi methyl-[3H]-thymidine was added to each well. [3H]Thymidine incorporation into the responder T cells was measured as count per minute (cpm). The data shown are representative of those obtained in three independent experiments. Bars represent ±SD for n = 8 wells per group in each experiment. *P < 0.05, ***P < 0.001 by ANOVA Tukey's multiple comparison tests.
TAM tko Mice Are More Sensitive to IRBP1–20 Immunization
To determine whether TAM tko mice were more sensitive to immunization with retina-specific antigenic peptide, we immunized WT and tko mice with IRBP1–20, then isolated T cells and splenic APCs 2 to 3 weeks later and cocultured the T cells with the γ-irradiated APCs in a 96-well plate in the presence of either the immunizing peptide (IRBP1–20) or a control peptide (IRBP161–180). As shown in Figure 4A, although both WT and tko cells displayed a proliferative response to the immunizing peptide IRBP1–20 (Fig. 4A, center) but not to IRBP161–180 (Fig. 4A, right), tko cells displayed a threefold higher response than WT cells, and such response was antigen dose dependent (Fig. 4A, center). This higher proliferative response by the tko T cells plated on the tko APCs in the presence of the immunizing peptide was directly visualized by the formation of macroscopic colonies composed of the proliferating T cells in the presence of the immunizing peptide (IRBP1–20; Fig. 4C) but not the nonrelevant peptide (IRBP161–180; Fig. 4D). Although such proliferating T cell colonies were also formed in the coculture of WT T cells with WT APCs, these colonies displayed small sizes and unclear colony boundaries (Fig. 4B). These results suggest that TAM deficiency in APCs may lead to an overresponse of T cells to the antigens presented by the tko APCs.
Figure 4.
TAM tko mice produced increased T cells specific for immunizing the IRBP1–20 antigen. (A) The T cell–depleted syngeneic splenocytes, which served as APCs, were prepared as single-cell suspensions and γ-irradiated before plating on a 96-well plate (1 × 105 cells per well). Nylon wood–separated T cells (4 × 105 cells), prepared on day 14 after immunization from both WT and tko mice preimmunized with IRBP1–20 peptide in CFA, were plated in each well and cultured for 72 hours in the absence (-Ag) or presence of 0.01, 0.1, 1, and 10 μg/mL IRBP1–20 or the irrelevant IRBP161–180 peptide, as indicated. In the last 8 hours of coculture, 0.5 μCi methyl-[3H]-thymidine was added to each well. [3H]Thymidine incorporation into the responder T cells was measured as count per minute (cpm). (B–D) Images of colony formation by the WT T cells that had been isolated from IRBP1–20–immunized WT mice and expanded for 72 hours on γ-irradiated WT splenic APC feeders in the presence of IRBP1–20 (B) or by tko T cells that had been isolated from immunized tko mice and expanded in culture for 72 hours on the tko APCs in the presence of 10 μg/mL of either IRBP1–20 (C) or the irrelevant peptide, IRBP161–180 (D). Error bars represent ±SD for n = 8 wells per group. Data are representative of those obtained in four independent assays. ***P < 0.001 by one-way ANOVA.
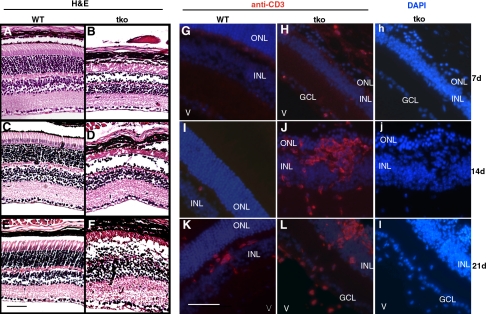
IRBP1–20 Immunization of tko Mice Induces Inflammation and T Cell Infiltration into the Retina
The WT C57BL/6 mice were less susceptible to uveitis induction than the B10RIII mice. In C57BL/6 mice, the minimum amount of uveitogenic IRBP1–20 peptide that causes EAU is approximately 300 μg per mouse.22 To test whether tko mice were more susceptible to the induction of uveitis, we immunized WT and tko mice with the low dose of 150 μg IRBP1–20 per mouse. Immunization invoked a massive infiltration of lymphocytes into the subretinal space within 7 days in tko mice (Fig. 5B) but not in WT mice (Fig 5A), and the severity of the inflammatory reaction increased at days 14 (Fig. 5D) and 21 (Fig. 5F) compared with WT controls (Figs. 5C, 5E, respectively). To identify the invasive cell types, we immunostained paraffin-embedded eye sections with anti-CD3 antibody and found that CD3+ T cells were clearly present in the tko retina by days 14 and 21 after immunization (Figs. 5J, 5L, respectively). In addition, although there was no clear sign of lymphocyte infiltration in the H&E-stained WT sections, CD3+ T cells were also visible in the WT retina at 21 days after immunization (Fig. 5K). However, the disorganization of the ONL normally seen in the B10-RIII mouse was not seen in any of the immunized mice at this dose of immunizing peptide, but it was seen in C57BL/6 mice day 14 after immunization using the dose of 500 μg per mouse; none of the tko or Mertk single-knockout mice survived for 48 hours at this dose; they died of hyperreactive immune responses.27
Figure 5.
IRBP1–20 immunization causes infiltration of CD3+ T cells into the tko retina. Eyes were isolated from WT and tko mice immunized with 250 μg/mouse IRBP1–20 in CFA at day 7 (top), 14 (center), or 21 (bottom) after immunization and were processed for paraffin embedding and sectioned at 8 μm. (A–F) Eye sections were stained with H&E. (G–L) Eye sections were immunostained with anti–CD3 antibody visualized by Cy-3–labeled secondary antibody. (h, j, l) Same sections as in (H), (J), and (L) showing nuclei stained blue with DAPI. V, vitreous humor; INL, inner nuclear layer; GCL, ganglion cell layer. Scale bars, 80 μM (the bar in E shows the scale in A–F, whereas that in K shows the scale in G–l).
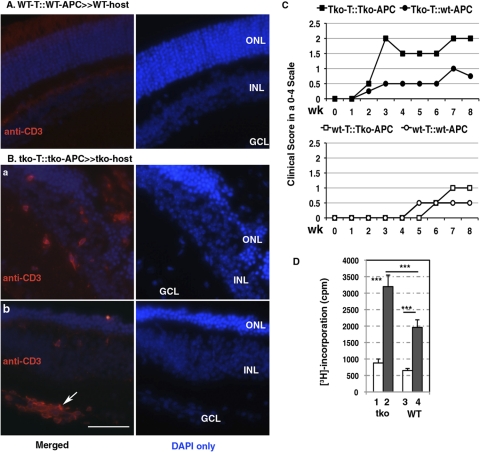
CD4+ T Cells from Immunized tko Mice Are More Effective at Inducing Host Immune Responses and tko Mice Are More Susceptible to Immunopathogenic Induction by Adoptive Transfer of IRPB-Specific T Cells
To test whether T cells from IRBP-immunized tko mice were more effective in inducing eye inflammation in host WT or tko mice and whether tko mice were more vulnerable to uveitogenic induction by transfer of IRBP-specific T cells from immunized WT or tko mice, we performed T cell transplantation experiments. We first immunized WT and tko mice with 150 μg IRPB1–20 in CFA, then isolated CD4+ and CD11c+ cells from pooled spleens and lymph nodes 14 days later and cocultured them at a ratio of 1:1 for 48 hours in the presence of IRPB1–20. A low dose of 1 × 106 purified and IRBP-primed CD4+ T cells per mouse were then injected via the tail veil into 6- to 8-week-old WT or tko mice. This number of transplanted cells per mouse has been shown not to induce uveitis in the WT C57BL/6 mice,22,23 and this was further confirmed in our present study because no CD3+ T cells were present in the WT host even 5 weeks after T cell transplantation (Fig. 6A). In contrast, CD3+ T cells were detected in the tko retina, especially in areas surrounding retinal blood vessels (Fig. 6Bb, arrow). As shown in Figure 6C, clinical scoring of uveitis by funduscopy performed from posttransplantation week 2 to week 8 showed that the transplanted tko T cells that had been cocultured with tko APCs induced EAU with scores of 0.5 to 2 in the tko host mice (Fig. 6C, top, labeled tko-T::tko-APC and indicated by solid squares) and that the transplanted tko T cells after coculture with WT APCs also induced EAU, but with less severity (Fig. 6C, top, labeled tko-T::WT-APC and indicated by solid circles). In contrast, the transplanted WT T cells that had been treated identically were not able to induce EAU in either WT or tko hosts within the first 5 weeks after cell transfer but were able to induce EAU over a longer time course, but only in tko recipients (Fig. 6C, bottom). Under the same experimental conditions, neither tko nor WT T cells induced EAU in any WT host. To examine whether IRBP1–20–specific T cells were present in the host mice after 5 weeks of transplantation and to compare transplanted CD4+ T cells prepared from IRBP1–20–immunized WT or tko mice, we performed an in vitro T cell proliferation assay. As shown in Figure 6D, the IRBP1–20–specific T cells from preimmunized WT or tko mice were present in the tko host at 5 weeks after transplantation; however, those prepared from preimmunized tko mice and in vitro–expanded tko APCs in the presence of immunizing-antigen before adoptive transfer were present in greater numbers (Fig. 6D, bar 2 vs. bar 4).
Figure 6.
Adoptive transfer of IRBP-primed CD4 T cells causes retinal inflammation and T cell colonization in the tko recipient eye. T cells used for adoptive transfer were isolated and purified by nylon wood column filtration from WT and tko mice preimmunized with 150 μg/mouse IRBP1–20 in CFA for 14 days and were expanded in culture with γ-irradiated splenic APCs in the presence of 10 μg/mL IRBP1–20 for 48 hours. CD4+ T cells (1 × 106 cells) from each combination of cocultures were purified using a negative selection mouse CD4+ T cell enrichment kit and injected into the tail veil of a WT or tko female recipient at approximately 6 to 8 weeks of age. (A, B) By 35 days after transfer, the recipient eyes were processed for paraffin embedding and sectioning at 8 μm. The T cells infiltrated into tko recipient (Ba, Bb) and wild-type (A) eyes were immunostained with anti-CD3 antibody and visualized with Cy3-labeled secondary antibody, and nuclei were stained blue using DAPI (right). Fluorescence images were captured by a color CCD camera connected to an inverted microscope. Note, the caption WT-T::WT-APC≫WT-host indicates that the WT T cells from the IRBP1–20–immunized mice were expanded in vitro on the WT APCs before they were transferred into a WT recipient host, whereas the tko-T::tko-APC≫tko-host represents that the tko T cells from immunized mice were expanded on the tko APCs in culture before they were transferred into a tko host. (C) Adoptive transfer of IRBP1–20–primed CD4+ T cells induces EAU in the tko but not in the WT host. Funduscopy was performed on both tko and WT recipients at the time points indicated. The funduscopic score is based on a 0 to 4 scale. Given that no WT recipient developed clear funduscopic defect, the plots in (C) only show data obtained from the tko hosts and present a single representative of three independent experiments. Note, legends, tko-T::tko-APC, tko-T::wt-APC and wt-T::wt-APC or wt-T::tko-APC indicate that either tko (tko-T) or WT (wt-T) T cells have been expanded for 48 hours on either tko (tko-APC) or WT (wt-APC) APCs in vitro, before adoptive transfer of the IRBP-primed CD4+ T cells. (D) T cell proliferation assay performed on T cells isolated from the tko recipient mice after adoptive transfer of IRBP1–20–primed CD4+ T cells. [3H]Thymidine (0.5 μCi/well) incorporation was performed for 8 hours on splenic and pooled lymph node T cells pre-cocultured with tko APCs in the presence of 10 μg/mL IRBP1–20 for 48 hours (bars 2 and 4) or the absence of the pre-coculture (bars 1 and 3). The label tko indicates that the T cells used in this [3H]thymidine incorporation assay were isolated from the tko hosts, previously injected with the tko T cells that had been primed in vitro with tko APCs. The label WT represents that the T cells for the incorporation assays were also isolated from the tko hosts, but those tko hosts had been previously transplanted with the WT T cells prepared originally from the IRBP1–20–immunized WT mice and further primed in vitro with WT APCs. Error bars represent the SD for n = 3. ***P < 0.001 by ANOVA multiple comparison test.
Discussion
TAM receptors, particularly the Mertk receptor, play an important role in the clearance of apoptotic cells or spent cell organelles.8 Inefficient removal of dead cells by phagocytes lacking TAM receptors results in the accumulation of apoptotic debris, a potent activator of innate and adaptive immune responses. Mertk regulates the phagocytic clearance of spent photoreceptor outer segments by RPE cells; failure to do so causes rapid photoreceptor cell death by apoptosis. The newly released self-antigens from apoptotic cells are presumably captured and processed by APCs and subsequently presented to and activate the naive T cells to become effector T helper cells. As a result, those tko mice have CD4 T cells that are more activated but less naive. In general, though most of the antigen-experienced T cells are eliminated by apoptosis, a small fraction can survive for a long period and become memory T cells. We indeed observed the presence of increased memory T cells in the naive tko mice. In addition, those naive tko mice produced antigen-specific CD4+ T cells, including IRBP-specific CD4+ T cells.
Consistent with the presence of memory T cells and the spontaneous development of IRBP-specific CD4+ T cells, tko mice were more susceptible to the induction of uveitis by IRBP immunization. Immunization of tko mice with IRBP1–20 induced more than three times as many antigen-specific CD4+ T cells than WT controls. In response to low-dose IRBP immunization, T cells in tko mice, but not WT mice, invaded and colonized the retina, as visualized by anti-CD3 antibody immunostaining. Increased IRBP-specific CD4+ T cells in naive or immunized tko mice and the overwhelming response to IRBP immunization by tko mice suggest that tko mice are more susceptible to IRBP immunization.
Given that the rapid photoreceptor degeneration in tko mice caused by the deficiency of Mertk began when mice were 3 weeks of age, those mice had undergone intense encounter with self-antigens, including IRBP released from apoptotic photoreceptors. It is conceivable that when antigen-specific memory T cells in tko mice re-encounter the same self-antigens, memory T cells are rapidly activated. Those memory T cells in tko mice may be responsible for hyperresponse to IRBP immunization. To avoid the participation of memory T cells generated from the encounter of apoptotic material during photoreceptor degeneration, the T cells were isolated from young naive tko mice at 3 weeks of age and were transferred into either WT or tko hosts. Those cells failed to induce uveitis in any hosts. It will be useful to deplete the memory T cells in adult mice before IRBP immunization to test whether those tko mice overreact to IRBP because of the antigen-specific memory T cells or because of the malfunctioning T cell response to immunization.
On the other hand, the APCs lacking TAM receptors may also contribute to hyperreactivity. TAM receptors are expressed in cells of the myeloid lineage, such as monocytes, DCs, and macrophages, and in natural killer (NK) cells, but not T and B cells.6 TAM receptors negatively control innate immune responses,28 and DCs lacking TAM receptors unrestrainedly release proinflammatory cytokines, including IL-6, interferons, and TNF-α,7 which can cause the systemic lupus erythematosus-like phenotypes seen in TAM tko mice.14 Systemic autoimmune disorders have been considered one of the major causes of uveitis, especially posterior uveitis, which affects the back of the uveal tract. To test the TAM tko environment affecting the susceptibility to EAU development, we induced EAU in WT or tko recipients by adoptive transfer of purified and in vitro IRBP–primed CD4+ T cells that had been prepared from the IRBP-immunized WT or tko mice at 6 to 8 weeks of age. To optimally observe differences between WT and tko hosts in the development of retinal inflammation, we transferred 1 million, a number lower than normally required for adoptive transfer of the disease in C57BL/6 mice, purified IRBP-specific CD4+ T cells into each recipient and tested for the induction of EAU. Although no EAU was found in WT recipients by funduscopy or anti-CD3 antibody immunostaining in three independent experiments, almost all tko recipients developed a clear clinical funduscopic score independently of the source of the transferred T cells. However, closer examination showed that the T cells isolated from tko mice preimmunized with IRBP peptide were more effective at causing clinical signs of inflammation. These studies indicate that the transferred tko T cells and the tko recipient itself both contribute to a vulnerable environment for the promotion of retinal autoimmune diseases. Whether the altered antigen presentation or cytokine expression profile in each single APC cell, or simply the increased total number of APCs in the tko mice, contributes to such hyperreactivity to IRBP induction must be further investigated.
Supplementary Material
Acknowledgments
The authors thank Douglas Dean for valuable discussion and Research to Prevent Blindness for general support.
Footnotes
Supported by National Institutes of Health Grants R01-EY018830 (Q-XLu), RR017702 (Q-XLu), R01-EY01989 (QLi), and RR018733 (QLi). Q-XLu is a 2010 RPB William and Mary Greve Special Scholar investigator.
Disclosure: F. Ye, None; Q. Li, None; Y. Ke, None; Qj. Lu, None; L. Han, None; H.J. Kaplan, None; H. Shao, None; Qx. Lu, None
References
- 1. Lai C, Gore M, Lemke G. Structure, expression, and activity of Tyro 3, a neural adhesion-related receptor tyrosine kinase. Oncogene. 1994;9:2567–2578 [PubMed] [Google Scholar]
- 2. Ohashi K, Mizuno K, Kuma K, Miyata T, Nakamura T. Cloning of the cDNA for a novel receptor tyrosine kinase, Sky, predominantly expressed in brain. Oncogene. 1994;9:699–705 [PubMed] [Google Scholar]
- 3. O'Bryan JP, Frye RA, Cogswell PC, et al. axl, a transforming gene isolated from primary human myeloid leukemia cells, encodes a novel receptor tyrosine kinase. Mol Cell Biol. 1991;11:5016–5031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Janssen JW, Schulz AS, Steenvoorden AC, et al. A novel putative tyrosine kinase receptor with oncogenic potential. Oncogene. 1991;6:2113–2120 [PubMed] [Google Scholar]
- 5. Jia R, Hanafusa H. The proto-oncogene of v-eyk (v-ryk) is a novel receptor-type protein tyrosine kinase with extracellular Ig/GN-III domains. J Biol Chem. 1994;269:1839–1844 [PubMed] [Google Scholar]
- 6. Graham DK, Dawson TL, Mullaney DL, Snodgrass HR, Earp HS. Cloning and mRNA expression analysis of a novel human protooncogene, c-mer. Cell Growth Differ. 1994;5:647–657 [PubMed] [Google Scholar]
- 7. Rothlin CV, Ghosh S, Zuniga EI, Oldstone MB, Lemke G. TAM receptors are pleiotropic inhibitors of the innate immune response. Cell. 2007;131:1124–1136 [DOI] [PubMed] [Google Scholar]
- 8. Scott RS, McMahon EJ, Pop SM, et al. Phagocytosis and clearance of apoptotic cells is mediated by MER. Nature. 2001;411:207–211 [DOI] [PubMed] [Google Scholar]
- 9. Stitt TN, Conn G, Gore M, et al. The anticoagulation factor protein S and its relative, Gas6, are ligands for the Tyro 3/Axl family of receptor tyrosine kinases. Cell. 1995;80:661–670 [DOI] [PubMed] [Google Scholar]
- 10. Schneider C, King RM, Philipson L. Genes specifically expressed at growth arrest of mammalian cells. Cell. 1988;54:787–793 [DOI] [PubMed] [Google Scholar]
- 11. Manfioletti G, Brancolini C, Avanzi G, Schneider C. The protein encoded by a growth arrest-specific gene (gas6) is a new member of the vitamin K-dependent proteins related to protein S, a negative coregulator in the blood coagulation cascade. Mol Cell Biol. 1993;13:4976–4985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dahlback B. Protein S and C4b-binding protein: components involved in the regulation of the protein C anticoagulant system. Thromb Haemost. 1991;66:49–61 [PubMed] [Google Scholar]
- 13. Prasad D, Rothlin CV, Burrola P, et al. TAM receptor function in the retinal pigment epithelium. Mol Cell Neurosci. 2006;33:96–108 [DOI] [PubMed] [Google Scholar]
- 14. Lu Q, Lemke G. Homeostatic regulation of the immune system by receptor tyrosine kinases of the Tyro 3 family. Science. 2001;293:306–311 [DOI] [PubMed] [Google Scholar]
- 15. Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California: the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111:491–500, discussion 500 [DOI] [PubMed] [Google Scholar]
- 16. Davies JB, Rao PK. Ocular manifestations of systemic lupus erythematosus. Curr Opin Ophthalmol. 2008;19:512–518 [DOI] [PubMed] [Google Scholar]
- 17. Shao H, Shi H, Kaplan HJ, Sun D. Chronic recurrent autoimmune uveitis with progressive photoreceptor damage induced in rats by transfer of IRBP-specific T cells. J Neuroimmunol. 2005;163:102–109 [DOI] [PubMed] [Google Scholar]
- 18. Caspi RR, Sun B, Agarwal RK, et al. T cell mechanisms in experimental autoimmune uveoretinitis: susceptibility is a function of the cytokine response profile. Eye (Lond). 1997;11(pt 2):209–212 [DOI] [PubMed] [Google Scholar]
- 19. Becker MD, Adamus G, Davey MP, Rosenbaum JT. The role of T cells in autoimmune uveitis. Ocul Immunol Inflamm. 2000;8:93–100 [PubMed] [Google Scholar]
- 20. Lu Q, Gore M, Zhang Q, et al. Tyro-3 family receptors are essential regulators of mammalian spermatogenesis. Nature. 1999;398:723–728 [DOI] [PubMed] [Google Scholar]
- 21. Ke Y, Sun D, Zhang P, Jiang G, Kaplan HJ, Shao H. Suppression of established experimental autoimmune uveitis by anti-LFA-1alpha Ab. Invest Ophthalmol Vis Sci. 2007;48:2667–2675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shao H, Liao T, Ke Y, Shi H, Kaplan HJ, Sun D. Severe chronic experimental autoimmune uveitis (EAU) of the C57BL/6 mouse induced by adoptive transfer of IRBP1–20-specific T cells. Exp Eye Res. 2006;82:323–331 [DOI] [PubMed] [Google Scholar]
- 23. Avichezer D, Silver PB, Chan CC, Wiggert B, Caspi RR. Identification of a new epitope of human IRBP that induces autoimmune uveoretinitis in mice of the H-2b haplotype. Invest Ophthalmol Vis Sci. 2000;41:127–131 [PubMed] [Google Scholar]
- 24. D'Cruz PM, Yasumura D, Weir J, et al. Mutation of the receptor tyrosine kinase gene Mertk in the retinal dystrophic RCS rat. Hum Mol Genet. 2000;9:645–651 [DOI] [PubMed] [Google Scholar]
- 25. Nagata S, Hanayama R, Kawane K. Autoimmunity and the clearance of dead cells. Cell. 2010;140:619–630 [DOI] [PubMed] [Google Scholar]
- 26. Yang L, Anderson DE, Baecher-Allan C, et al. IL-21 and TGF-beta are required for differentiation of human T(H)17 cells. Nature. 2008;454:350–352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Camenisch TD, Koller BH, Earp HS, Matsushima GK. A novel receptor tyrosine kinase, Mer, inhibits TNF-alpha production and lipopolysaccharide-induced endotoxic shock. J Immunol. 1999;162:3498–3503 [PubMed] [Google Scholar]
- 28. Lemke G, Lu Q. Macrophage regulation by Tyro 3 family receptors. Curr Opin Immunol. 2003;15:31–36 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.