The prevalence of corneal astigmatism in infants and young children who are members of a Native American tribe indicates that the mean amount of corneal astigmatism is higher than reported for non–Native American populations and increases from 1.43 D in 1-year-olds to nearly 2.00 D by school age.
Abstract
Purpose.
To describe the prevalence of corneal astigmatism in infants and young children who are members of a Native American tribe with a high prevalence of refractive astigmatism.
Methods.
The prevalence of corneal astigmatism was assessed by obtaining infant keratometer (IK4) measurements from 1235 Tohono O'odham children, aged 6 months to 8 years.
Results.
The prevalence of corneal astigmatism >2.00 D was lower in the 1- to <2-year-old age group when compared with all other age groups, except the 6- to <7-year-old group. The magnitude of mean corneal astigmatism was significantly lower in the 1- to <2-year age group than in the 5- to <6-, 6- to <7-, and 7- to <8-year age groups. Corneal astigmatism was with-the-rule (WTR) in 91.4% of astigmatic children (≥1.00 D).
Conclusions.
The prevalence and mean amount of corneal astigmatism were higher than reported in non–Native American populations. Mean astigmatism increased from 1.43 D in 1-year-olds to nearly 2.00 D by school age.
A high prevalence of astigmatism has been documented among preschool- and school-age members of several Native American tribes (Kershner RM, et al. IOVS 1984;25:ARVO Abstract 70),1–11 including the Tohono O'odham of southern Arizona.9–11 Other studies have documented that the astigmatism is primarily corneal (Kershner RM, et al. IOVS 1984;25:ARVO Abstract 217).5,10 However, no information has been published concerning the prevalence of corneal astigmatism in Native American children younger than 5 years nor are data available concerning any change in prevalence between infancy and school age.
The purpose of the present study was to examine the prevalence of corneal astigmatism in infants and young children who are members of the Tohono O'odham Nation, a Native American tribe with a high prevalence of astigmatism (Kershner RM, et al. IOVS 1984;25:ARVO Abstract 217)9,10 that is primarily with-the-rule (WTR)9,10 and corneal in origin (Kershner RM, et al. IOVS 1984;25:ARVO Abstract 217).10
Methods
Subjects
The subjects were children who were recruited between September 2005 and December 2008, at 6 months through 7 years of age, into a study of refractive error development. The children were recruited from the Women, Infants, and Children (WIC) clinics, the Head Start program, the community, and kindergarten and first grade classrooms on the Tohono O'odham reservation in southern Arizona. Data from the first study encounter for each child (ages 6 months through 7 years) were included in the analyses (n = 1502).
This research complied with the Declaration of Helsinki and was approved by the Tohono O'odham Nation and by the Institutional Review Board of the University of Arizona. Parents provided written informed consent before testing.
Infant Keratometer
The IK4 infant keratometer consists of a single-ring (200-mm-diameter) keratoscope with 12 infrared light-emitting diodes (LEDs) attached to a custom telecentric telephoto lens designed for use with a camcorder (Sony TRV460 Digital-8; Sony Electronics, Inc., San Diego, CA). The LEDs pose an insignificant hazard to the eye.12 The instrument incorporates infrared imaging to minimize ambient illumination artifacts and to improve the attractiveness of the central fixation target for the child. A telecentric design was used to minimize magnification variation for images within the depth of field and to improve the accuracy of corneal curvature measurements. Two appropriately spaced, infrared-coated, achromatic lenses, one of +50-mm focal length and one of –50-mm focal length, were used for the telephoto system, along with prototyping hardware from Edmund Industrial Optics (Barrington, NJ). The lenses add 70 mm to the length of the camcorder and serve to mount the ring keratoscope. Calibration constants specific to the keratometer and the imaging lens were determined and were verified periodically throughout the study interval, through measurement of a reference surface. The working distance of the IK4 is approximately 11.5 cm from the child's eye. Studies have shown good agreement between IK and Retinomax K+ (Nikon, Tokyo, Japan) keratometry measurements of young children (Miller JM, et al. IOVS 2005;46:ARVO E-Abstract 5625; Clifford-Donaldson CE, et al. IOVS 2007;48:ARVO E-Abstract 997).
Procedures
Video keratoscope images were obtained with the IK4 for each child's right eye (RE). The older children were asked to remain still and to fixate on the center green light in the display; the younger children sat on a parent's lap, and the parent and tester directed their attention toward the IK4. The tester looked through the monitor of the IK4's camcorder and aligned the reflected images of the circle of 12 infrared LEDs around the perimeter of the child's pupil. The tester moved the instrument forward or backward, so that the reflected ring of lights was in sharp focus. Short videos, approximately 15 to 30 seconds in length, were recorded.
Data Analysis
Custom image analysis software was written to score the IK4 image data. The software automatically scans captured video, analyzing each frame for corneal curvature, pupil size, alignment, and image motion. Calibration constants for the software were established by imaging two lenses with radii of curvature that cover the anticipated range expected for children. The lenses were plano-convex and had radii of 6.19 and 8.25 mm, (parts 45-693 and 45-694, respectively; Edmund Optics). Petroleum jelly was smeared on the flat side of the lenses to disrupt Purkinje reflections on their surfaces. For each frame, the software locates the position of the 12 LEDs reflected from the cornea. Each of the LED spots is analyzed to determine the quality of the frame. Elongated spots suggest image motion during acquisition, whereas large-diameter spots indicate that the keratometer is not properly focused for a given frame. Frames falling into these preceding categories are discarded, and the remaining images are reviewed manually for quality. For images judged to be stable and in focus, the positions of the LED spots are fitted by computer to an ellipse and scaled by a calibrated magnification factor to recover the keratometry values and orientation.
The keratometry and orientation values were transformed into J0 and J45 components,13 and the median J0 and median J45 were determined. The median J0 and J45 were transformed back into standard clinical notation for cylinder power and axis. The number of images used in determining the keratometry values was also recorded.
The axis was categorized as WTR if the plus cylinder axis was ≥60° and ≤120°, against-the-rule (ATR) if the plus cylinder axis was ≤30° or ≥150°, and oblique if the plus cylinder axis was >30° and <60° or >120° and <150°.
Results
Prevalence and Axis of Corneal Astigmatism
Subjects.
Data from 267 of the 1502 children were excluded from the analysis: 28 because of ocular abnormalities other than high refractive error and 238 because scorable IK4 images were not obtained. Of the latter 121 were excluded because the child did not cooperate during the measurement or because the video data quality was too poor to score (e.g., off center, out of focus), 107 due to technical/experimenter error (e.g., the tester failed to initiate recording before measurement), and 10 because the instrument was not functioning on the test day). In addition, the measurement from one child was an extreme outlier (−13 D) and was therefore excluded. Failure to obtain scorable IK4 images (n = 238) varied significantly across age (χ27 =107.19, P < 0.001), and occurred in 85 (23.5%) of 361 6-month to <1-year-olds, 75 (28.5%) of 263 1- to <2-year-olds, 34 (21.0%) of 162 2- to <3-year-olds, 19 (11.2%) of 170 3- to <4-year-olds, 15 (6.9%) of 217 4- to <5-year-olds, 3 (2.6%) of 115 5- to <6-year-olds, 5 (3.4%) of 149 6- to <7-year-olds, and 2 (3.1%) of 65 7- to <8-year-olds. After Bonferroni correction for multiple comparisons, the measurement success rate was significantly better in each of the oldest four age groups (ranging from 4 to <8 years) than in any of the youngest three age groups (ranging from 6 months to <3 years), and the success rate was significantly better in the 3- to < 4-year-old age group than in the 6-month to <1-year-old and 1- to <2-year-old groups. The mean age of the final sample of 1235 children was 3.35 years (SD 2.19; range, 0.50–7.97 years).
Prevalence of Corneal Astigmatism.
Table 1 shows the prevalence of corneal astigmatism in terms of cylinder magnitude (clinical notation) as a function of age group. The prevalence of astigmatism ≥1.00 D did not differ significantly across age group. Table 1 also shows prevalence of corneal astigmatism by sex. There was no significant relation between sex and prevalence of corneal astigmatism.
Table 1.
Prevalence of Right Eye Corneal Astigmatism by Age and by Sex
| Corneal Astigmatism (D) |
||||||
|---|---|---|---|---|---|---|
| <1.00 n (%) | 1 to <2 n (%) | 2 to <3 n (%) | 3 to <4 n (%) | ≥4.00 n (%) | ||
| Age, y | ||||||
| 0.5 to <1 | 269 | 53 (19.7) | 123 (45.7) | 74 (27.5) | 17 (6.3) | 2 (0.7) |
| 1 to <2 | 183 | 46 (25.1) | 92 (50.3) | 36 (19.7) | 9 (4.9) | — |
| 2 to <3 | 125 | 28 (22.4) | 56 (44.8) | 28 (22.4) | 9 (7.2) | 4 (3.2) |
| 3 to <4 | 149 | 34 (22.8) | 59 (39.6) | 39 (26.2) | 13 (8.7) | 4 (2.7) |
| 4 to <5 | 197 | 44 (22.3) | 84 (42.6) | 31 (15.7) | 29 (14.7) | 9 (4.6) |
| 5 to <6 | 108 | 21 (19.4) | 46 (42.6) | 23 (21.3) | 9 (8.3) | 9 (8.3) |
| 6 to <7 | 143 | 29 (20.3) | 63 (44.1) | 23 (16.1) | 16 (11.2) | 12 (8.4) |
| 7 to <8 | 61 | 13 (21.3) | 15 (24.6) | 21 (34.4) | 6 (9.8) | 6 (9.8) |
| Sex | ||||||
| Girls | 611 | 132 (21.6) | 269 (44.0) | 138 (22.6) | 46 (7.5) | 26 (4.3) |
| Boys | 624 | 136 (21.8) | 269 (43.1) | 137 (22.0) | 62 (9.9) | 20 (3.2) |
| Total | 1235 | 268 (21.7) | 538 (43.6) | 275 (22.3) | 108 (8.7) | 46 (3.7) |
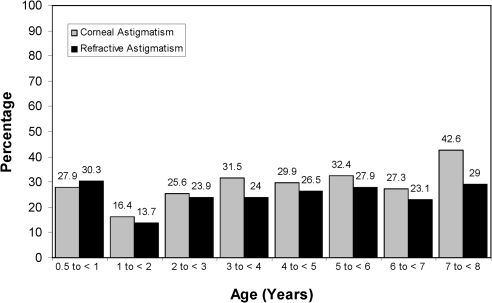
Figure 1 shows the prevalence of corneal astigmatism >2.00 D in each age group. Also shown in Figure 1 is the prevalence of refractive astigmatism >2.00 D from previously published data on this sample.14 The χ2 analysis indicated a significant difference across age in prevalence of corneal astigmatism >2.00 D (χ27 = 21.51, P < 0.001), and pairwise χ2 analyses showed a significant difference between prevalence of astigmatism >2.00 D in the 1- to <2-year age group when compared with all other age groups except the 6- to <7-year-old group (P < 0.05 before Bonferroni correction, with only the comparisons of the 1- to <2-year vs. 7- to <8-year age group comparison significant after correction). In addition, the prevalence in the 7- to <8-year age group was significantly greater than the prevalence in the <1-year, 1- to <2-year, 3- to <4-year, and 6- to <7-year age groups (P <0.05 before Bonferroni correction, with no comparisons significant after correction).
Figure 1.
Prevalence of right eye corneal astigmatism >2.00 D from the present study (n = 1235) and prevalence of right eye refractive astigmatism > 2.00 D (n = 1461) from a previous report on the same sample of subjects.14 Final sample size varies across studies due to differences in measurement success rate across instruments.
Table 2 shows mean and SD of amount of corneal astigmatism (in terms of J0, J45, and cylinder magnitude in clinical notation) as a function of age group. ANOVA indicated significant main effects of age group for measurements of J0 (P < 0.001) and for measurements of cylinder magnitude (P < 0.002), but no significant effect for J45. Post hoc analysis (with Bonferroni correction) of J0 data indicated that the <1-year and 1- to <2-year age groups had significantly lower mean J0 than the 4- to <5-, 5 to <6-, 6- to <7-, and 7- to <8-year age groups and that the 1- to <2-year age group also had lower mean astigmatism than the 3- to <4-year age group. Post hoc analyses (with Bonferroni correction) indicated that mean cylinder magnitude was significantly lower in the 1- to <2-year age group than in the 5- to <6-, 6- to <7-, and 7- to <8-year age groups.
Table 2.
Mean Corneal Astigmatism by Age
| Age (y) | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| J0* | |||||
| 0.5 to <1 | 269 | 0.59 | 0.52 | −1.42 | 1.85 |
| 1 to <2 | 183 | 0.52 | 0.44 | −0.72 | 1.66 |
| 2 to <3 | 125 | 0.69 | 0.53 | −0.88 | 2.48 |
| 3 to <4 | 149 | 0.73 | 0.49 | −0.27 | 2.02 |
| 4 to <5 | 197 | 0.78 | 0.56 | −0.13 | 2.42 |
| 5 to <6 | 108 | 0.82 | 0.56 | −0.06 | 2.20 |
| 6 to <7 | 143 | 0.78 | 0.64 | −0.43 | 3.29 |
| 7 to <8 | 61 | 0.85 | 0.63 | −0.41 | 2.42 |
| Total | 1235 | 0.69 | 0.55 | −1.42 | 3.29 |
| J45* | |||||
| 0.5 to <1 | 269 | 0.18 | 0.44 | −1.49 | 1.61 |
| 1 to <2 | 183 | 0.15 | 0.40 | −1.11 | 1.60 |
| 2 to <3 | 125 | 0.20 | 0.37 | −0.87 | 1.32 |
| 3 to <4 | 149 | 0.16 | 0.35 | −1.76 | 1.09 |
| 4 to <5 | 197 | 0.14 | 0.35 | −0.97 | 1.45 |
| 5 to <6 | 108 | 0.17 | 0.34 | −0.77 | 1.12 |
| 6 to <7 | 143 | 0.23 | 0.39 | −0.79 | 1.50 |
| 7 to <8 | 61 | 0.30 | 0.35 | −0.51 | 1.16 |
| Total | 1235 | 0.18 | 0.38 | −1.76 | 1.61 |
| Clinical Notation | |||||
| 0.5 to <1 | 269 | 1.62 | 0.83 | 0.25 | 4.50 |
| 1 to <2 | 183 | 1.43 | 0.74 | 0.00 | 3.75 |
| 2 to <3 | 125 | 1.66 | 0.99 | 0.25 | 5.00 |
| 3 to <4 | 149 | 1.67 | 0.95 | 0.00 | 4.50 |
| 4 to <5 | 197 | 1.75 | 1.10 | 0.00 | 5.00 |
| 5 to <6 | 108 | 1.82 | 1.08 | 0.25 | 4.50 |
| 6 to <7 | 143 | 1.82 | 1.23 | 0.00 | 6.50 |
| 7 to <8 | 61 | 1.98 | 1.19 | 0.25 | 4.75 |
| Total | 1235 | 1.68 | 1.00 | 0.00 | 6.50 |
Data are in expressed in diopters.
In vector notation, 0.50 D of astigmatism is equivalent to 1.00 D of astigmatism in clinical notation (e.g., 0.50 D J0 = 1.00 D × 90 in clinical notation).
To allow comparison with previous studies, corneal toricity was also calculated as difference between corneal power in the vertical meridian and the corneal power in the horizontal meridian. With this method, positive values represent WTR astigmatism, and negative values represent ATR astigmatism. Means (SDs) across age were 1.37 (1.20), 1.24 (1.04), 1.57 (1.12), 1.64 (1.01), 1.74 (1.11), 1.80 (1.11), 1.76 (1.31), 1.90 (1.30) for age groups <1 year through 7 to <8 years, respectively. ANOVA indicated significant main effects of age group (P < 0.001). Post hoc analysis (with Bonferroni correction) indicated that the <1-year and 1- to <2-year age groups had significantly lower mean toricity than the 4- to <5-, 5- to <6-, 6- to <7-, and 7- to <8-year age groups, and that the 1- to <2-year age group also had lower mean toricity than the 3- to <4-year age group.
Comparison of the mean corneal astigmatism across the sexes yielded no significant effect for J0 or for cylinder magnitude (clinical notation). However, the boys had significantly greater J45 than did the girls: 0.22 D (SD 0.38) vs. 0.13 D (SD 0.38) (t(1233) = 4.21; P > 0.001).
Axis of Corneal Astigmatism.
Table 3 shows the axis of astigmatism by age in the children with ≥1.00 D of corneal astigmatism. The axis was WTR in 91.4% of children, and χ2 analysis indicated a significant relation between age and WTR astigmatism (χ27 = 30.18; P < 0.001). Post hoc analyses indicated that WTR astigmatism was significantly less prevalent among children in the <1-year age group compared with each of the five older age groups ranging from 2 to < 3 years to 6 to < 7 years and significantly less prevalent in the 1- to <2-year age group than in the 4- to <5- and 5- to <6-year age groups before correction for multiple comparisons. After Bonferroni correction for multiple comparisons, only the <1-year versus 3- to <4-year and the <1-year versus 4- to <5-year comparisons remained significant.
Table 3.
Axis of Astigmatism in Children with ≥1.00 D of Corneal Astigmatism
| Age (y) | N | With-the-Rule n (%) | Against-the-Rule n (%) | Oblique n (%) |
|---|---|---|---|---|
| 0.5 to <1 | 216 | 180 (83.3) | 7 (3.2) | 29 (13.4) |
| 1 to <2 | 137 | 122 (89.1) | 3 (2.2) | 12 (8.8) |
| 2 to <3 | 97 | 93 (95.9) | 1 (1.0) | 3 (3.1) |
| 3 to <4 | 115 | 110 (95.7) | 1 (0.9) | 4 (3.5) |
| 4 to <5 | 153 | 146 (95.4) | — | 7 (4.6) |
| 5 to <6 | 87 | 84 (96.6) | — | 3 (3.4) |
| 6 to <7 | 114 | 105 (92.1) | 1 (0.9) | 8 (7.0) |
| 7 to <8 | 48 | 44 (91.7) | — | 4 (8.3) |
| Total | 967 | 884 (91.4) | 13 (1.3) | 70 (7.2) |
Plus cylinder axis ≥60° and ≤120° classified as with-the-rule, ≤30° or ≥150° as against- the-rule, and >30° and <60° or >120° and <150° as oblique.
Discussion
The results of the present study provide the first data on the prevalence and amount of corneal astigmatism in Native American infants and very young children who are members of a tribe with a high prevalence of refractive astigmatism. The prevalence of corneal astigmatism ≥1.00 D (78.3%) was extremely high across all age groups and did not vary with age. When high astigmatism was defined as >2.00 D, there was evidence of a decrease in prevalence in 1- to <2-year-olds compared with all but one of the other age groups. This finding mirrors our previous finding on the prevalence of refractive astigmatism in these children, which also showed a lower prevalence in the 1- to <2-year-olds, as illustrated in Figure 1.14 The apparent increase in prevalence of corneal astigmatism in the oldest age group was not observed in the refractive astigmatism data. The data showing a decrease in the prevalence of corneal astigmatism in 1- to <2-year-olds support the validity of the previous observation that the prevalence of refractive astigmatism decreases in the second year of life in this population, as the refractive and corneal astigmatism data were obtained independently (i.e., with different instruments; SureSight [Welch Allyn, Skaneateles, NY] versus IK4). Furthermore, the presence of this pattern in corneal astigmatism data suggests that the observed change with age in the refractive astigmatism data was due at least in part to a change in corneal astigmatism. This decrease in prevalence in the second year of life is similar to the pattern observed in longitudinal studies of Caucasian and Asian populations,15–23 in which highly astigmatic infants showed a decrease in magnitude of refractive astigmatism during the second year of life. In contrast, Tohono O'odham children showed a subsequent increase in prevalence after the second year of life. Longitudinal data will allow us to determine patterns of change in astigmatism over the course of early development and will allow us to determine the extent to which these patterns can be predicted in individual children.
The mean amount of corneal astigmatism and the mean amount of corneal astigmatism on the vertical–horizontal meridian (J0) were lower in infants and toddlers than in older subjects in our sample, with the mean amount of astigmatism ranging from 1.43 D (SD 0.74) at age 1 to <2 years to 1.98 D (SD 1.19) at age 7 to <8 years (Table 2). As is the case with refractive astigmatism in this population,14 axis of corneal astigmatism was overwhelmingly WTR, although less so in the youngest age groups.
Data from the present study confirm and extend to younger ages the results of previous studies that have shown a high prevalence of corneal astigmatism among children who are members of Native American tribes in which there is a high prevalence of refractive astigmatism (Table 4).2,6,27–29 The average power of corneal astigmatism in the Tohono O'odham infants (1.62 D) was well above the values of 0.8 to 1.0 D previously reported for white infants (Table 5),30 In addition, toricity (vertical–horizontal) in the Tohono O'odham infants and preschoolers was greater than was observed in a sample of white infants and preschoolers31; was greater in the Tohono O'odham school-age children than in African American, Hispanic, Asian, and white school-age children32; and was similar to previous findings in Tohono O'odham school-age children of the same age (Table 6).32 Although some previous studies of Caucasian and Native American children have reported a higher prevalence28 and higher amounts24,25,29 of corneal astigmatism in girls than in boys, we found no evidence of a difference in prevalence or in amount of astigmatism, either across all ages or within individual age groups, although the boys had a greater oblique-axis component (J45) than did the girls.
Table 4.
Percentage of Children with Corneal Astigmatism across Studies
| Study | Ethnicity | Technique | Boys vs. Girls | Age (y) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.5 to <1 | 1 to <2 | 2 to <3 | 3 to <4 | 4 to <5 | 5 to <6 | 6 to <7 | 7 to <8 | ||||
| Woodruff24* | White | B&L Keratometer | Higher amount in girls | — | — | 1% (84) | 3% (140) | 3% (148) | 8% (108) | 17% (60) | — |
| Huynh et al.25 | Asian and Caucasian | IOL master | No difference | — | — | — | — | — | 27.7% (1727) | ||
| Abraham and Volovick2†‡ | Federal BIA School-Navajo | Not stated | Not stated | — | — | — | — | — | 74.1% (78) | 60.6% (38) | 59.0% (68) |
| County School-Navajo | — | 66.6% (145) | 80.2% (133) | ||||||||
| Lai et al.26§ | Taiwanese | KR8100 | Not stated | 10.5% (190) | |||||||
| Garber27‖¶ | Native American Navajo | B&L Keratometer | No difference | — | — | — | — | — | 26.4% (110) | 30.8% (117) | — |
| Maples et al.28 | Native American Navajo | Marco Keratometer | Higher in girls | — | 73.4% (250) | — | |||||
| Wick and Crane6†# | Native American Sioux | B&L Keratometer | No difference in first graders | — | — | — | — | — | — | 59.7% (72) | — |
| Lyle et al.†29 | Saskatchewan Indians | B&L Keratometer | Not stated | — | — | — | — | — | — | — | 60.6% (33) |
| White | 14.6% (48) | ||||||||||
| Present study | Native American Tohono O'odham | IK4 | No difference | 80.3% (269) | 74.9% (183) | 77.6% (125) | 77.2% (149) | 77.7% (197) | 80.6% (108) | 79.7% (143) | 78.7% (61) |
Numbers represent percentage with corneal astigmatism ≥1.00 diopter (D) except where otherwise noted. Sample sizes indicated in parentheses. B&L Keratometer, Reichert, DePew, NY; IOLmaster, Carl Zeiss Meditec, Inc., Dublin, CA; KR8100, Topcon Medical Systems, Inc., Oakland, NJ; Marco Keratometer, Marco, Jacksonville, FL.
≥1.25 D.
>1.00 D.
Ages not given; grades Beginner, 1, and 2.
>1.50.
Ages not given; grades K and 1.
≥2.00 D.
Ages not given; grade 1.
Table 5.
Mean Amount of Corneal Astigmatism across Studies
| Study | Ethnicity | Technique | Boys vs. Girls | Age (y) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.5 to <1 | 1 to <2 | 2 to <3 | 3 to <4 | 4 to <5 | 5 to <6 | 6 to <7 | 7 to <8 | ||||
| Howland and Sayles30 | White | Photokeratometer | Not stated | ∼1.00* (44) | ∼0.50 (73) | ∼0.75 (26) | <0.50 (18) | — | — | ||
| Huynh et al.25 | Asian and Caucasian | IOL master | Higher in girls | — | — | — | — | — | 0.82 (1712) | ||
| Lai et al.26† | Taiwanese | KR8100 | Not stated | 1.08 (190) | |||||||
| Heard et al.5‡ | Native American Zuni | B&L Keratometer | Not stated | 2.35 (∼100) | |||||||
| Lyle et al.29 | Saskatchewan Indians | B&L Keratometer | Higher in girls | — | — | — | — | — | — | — | 1.56 (33) |
| White | 0.87 (48) | ||||||||||
| Present study§ | Native American Tohono O'odham | IK4 | No difference | 1.62 (269) | 1.43 (183) | 1.66 (125) | 1.67 (149) | 1.75 (197) | 1.82 (108) | 1.82 (143) | 1.98 (61) |
Data are expressed in diopters. Sample size indicated in parentheses. Manufacturers are listed in Table 4.
0 to 1 year.
>1.50 D.
Ages not given; grades K through 3.
≥2.00 D.
Table 6.
Corneal Toricity Means
| Study | Ethnicity | Technique | Age (y) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0.5 to <1 | 1 to <2 | 2 to <3 | 3 to <4 | 4 to <5 | 5 to <6 | 6 to <7 | 7 to <8 | |||
| Mutti et al.31 | White | Hand-held custom keratometer | ∼0.75D (243) | ∼0.75D (257) | ∼0.75D (220) | |||||
| African American | 0.99, 0.83 (118,107) | 0.93, 0.87 (64,66) | ||||||||
| Asian | 1.02, 0.94 (141,152) | 1.03, 1.15 (45,48) | ||||||||
| Twelker et al.32* | Hispanic | Alcon auto-keratometer | 0.97, 0.69 (136,116) | 1.00, 1.02 (158,130) | ||||||
| White | 0.51, 0.48 (446,389) | 0.58, 0.44 (31,160) | ||||||||
| Native American Tohono O'odham | 1.05, 1.52 (11,10) | 2.06, 2.09 (50,39) | ||||||||
| Present Study | Native American Tohono O'odham | IK4 | 1.37 (269) | 1.24 (183) | 1.57 (125) | 1.64 (149) | 1.74 (197) | 1.80 (108) | 1.76 (143) | 1.90 (61) |
Data are vertical-horizontal corneal power in diopters. Positive values represent with-the-rule astigmatism, and negative values represent against-the-rule astigmatism.
Sample sizes provided in parenthesis. Autokeratometer; Alcon, Fort Worth, TX.
Data provided are for girls, boys.
The present study has several strengths: (1) a large sample size, with prevalence analyses based on data from 1235 children 6 months to 7 years of age, (2) a high proportion of children in whom scorable IK4 images could be obtained (84.1%; 1264/1502), (3) the use of a community-based rather than a clinic-based sample, and (4) use of the same instrument to obtain measurements of corneal astigmatism across the entire age range tested. There are also several limitations in the present study. The first is that the portion of the sample comprising children aged 4 years and younger may not be representative of the population as a whole, since there are family income requirements for both the WIC and Head Start programs. In contrast, the older children in the sample are likely to be representative, since approximately 85% of kindergarten and first grade children on the reservation participated. A second limitation of the prevalence data is that we were unable to obtain scorable IK4 images on a greater percentage of children in the younger age groups. We do not know whether inclusion of data from children of higher income families or from children who were uncooperative during testing would have significantly influenced the prevalence values obtained for the youngest age groups.
In conclusion, the results showed a higher prevalence and higher mean amounts of corneal astigmatism in young members of a Native American tribe with a high prevalence of refractive astigmatism than has been reported among non–Native American populations. The results also revealed an increase in mean corneal astigmatism of approximately 0.50 D between infancy and early school age, against which there are no comparative data from Caucasian or Asian populations. Finally, corneal astigmatism data mirrored the findings in a previous study in which we observed a decrease in prevalence of refractive astigmatism during the second year of life and an increase thereafter. Longitudinal data from this population will allow us to better evaluate and understand the patterns of change in astigmatism observed in individual infants and children.
Acknowledgments
The authors thank the Tohono O'odham Nation, the Tohono O'odham Early Childhood Head Start Program, the Indian Oasis/Baboquivari School District, the Bureau of Indian Affairs Office of Indian Education Programs (BIA OIEP, Papago/Pima Agency), the San Xavier Mission School, the parents and children who participated in the study, and our NIH/NEI Data Monitoring and Oversight Committee: Robert Hardy, PhD, chair; Morgan Ashley; Donald Everett, MA; Jonathan Holmes, MD; Louis Johnson; Andrew Lorentine; and Karla Zadnik, OD, PhD.
Footnotes
Supported by Grant U10 EY13153 (EMH) from the National Eye Institute of the National Institutes of Health, Department of Health and Human Services; unrestricted funds granted to the Department of Ophthalmology and Vision Science from Research to Prevent Blindness (JMM); the Walt and Lilly Disney Award for Amblyopia Research from Research to Prevent Blindness (JMM); and a Career Development Award from Research to Prevent Blindness (EMH).
Disclosure: E.M. Harvey, None; V. Dobson, None; J.M. Miller, None; J. Schwiegerling, None; C.E. Clifford-Donaldson, None; T.K. Green, None; D.H. Messer, None
References
- 1. Levy WJ, Wall FJ. A study of the refractive state of a group of American Pueblo Indians. Rocky Mountain Med J. 1969;40–42 [PubMed] [Google Scholar]
- 2. Abraham JE, Volovick JB. Preliminary Navajo optometric study. J Am Optom Assoc. 1972;43:1257–1260 [Google Scholar]
- 3. Boniuk V. Refractive problems in native peoples (the Sioux Lookout Project). Can J Ophthalmol. 1973;8:229–233 [PubMed] [Google Scholar]
- 4. Hamilton JE. Vision anomalies of Indian school children: the Lame Deer study. J Am Optom Assoc. 1976;47:479–487 [PubMed] [Google Scholar]
- 5. Heard T, Reber N, Levi D, Allen D. The refractive status of Zuni Indian children. J Optom Physiol Opt. 1976;53:120–123 [DOI] [PubMed] [Google Scholar]
- 6. Wick B, Crane S. A vision profile of American Indian children. J Optom Physiol Opt. 1976;53:34–40 [DOI] [PubMed] [Google Scholar]
- 7. Mohindra I, Nagaraj S. Astigmatism in Zuni and Navajo Indians. Am J Optom Physiol Opt. 1977;54:121–124 [DOI] [PubMed] [Google Scholar]
- 8. Maples WC, Atchley JW, Hughes J. Refractive profile of Navajo children. J Behav Optom. 1996;7:59–64 [Google Scholar]
- 9. Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism, eyeglass wear, and poor visual acuity among Native American grade-school children. Optom Vis Sci. 2006;83:206–212 [DOI] [PubMed] [Google Scholar]
- 10. Dobson V, Miller JM, Harvey EM. Corneal and refractive astigmatism in a sample of 3- to 5-year-old children with a high prevalence of astigmatism. Optom Vis Sci. 1999;76:855–860 [DOI] [PubMed] [Google Scholar]
- 11. Miller JM, Dobson V, Harvey EM, Sherrill DL. Comparison of preschool vision screening methods in a population with a high prevalence of astigmatism. Invest Ophthalmol Vis Sci. 2001;42:917–924 [PubMed] [Google Scholar]
- 12. International Commission on Non-Ionizing Radiation Protection ICNIRP statement on light-emitting diodes (LEDS) and laser diodes: implications for hazard assessment. Health Physics. 2000;78(6):744–752 [DOI] [PubMed] [Google Scholar]
- 13. Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci. 1997;74:367–375 [DOI] [PubMed] [Google Scholar]
- 14. Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010;87:400–405 [DOI] [PubMed] [Google Scholar]
- 15. Ingram RM, Barr A. Changes in refraction between the ages of 1 and 3½ years. Br J Ophthalmol. 1979;63:339–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ingram RM, Traynar MJ, Walker C, Wilson JM. Screening for refractive errors at age 1 year: a pilot study. Br J Ophthalmol. 1979;63:243–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mohindra I, Held R. Refraction in humans from birth to five years. Doc Ophthalmol Proc Ser. 1981;28:19–27 [Google Scholar]
- 18. Gwiazda J, Scheiman M, Mohindra I, Held R. Astigmatism in children: changes in axis and amount from birth to six years. Invest Ophthalmol Vis Sci. 1984;25:88–92 [PubMed] [Google Scholar]
- 19. Edwards M. The refractive status of Hong Kong Chinese infants. Ophthal Physiol Opt. 1991;11:297–303 [PubMed] [Google Scholar]
- 20. Ehrlich DL, Braddick OJ, Atkinson J, Anker S, Weeks F, Hartley T, Wade J, Rudenski A. Infant emmetropization: longitudinal changes in refraction components from nine to twenty months of age. Optom Vis Sci. 1997;74:822–843 [DOI] [PubMed] [Google Scholar]
- 21. Atkinson J, Braddick O, French J. Infant astigmatism: its disappearance with age. Vision Res. 1980;20:891–893 [DOI] [PubMed] [Google Scholar]
- 22. Abrahamsson M, Fabian G, Sjöstrand J. Changes in astigmatism between the ages of 1 and 4 years: a longitudinal study. Br J Ophthalmol. 1988;72:145–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Atkinson J, Anker S, Bobier W, Braddick O, Durden K, Nardini M, Watson P. Normal emmetropization in infants with spectacle correction for hyperopia. Invest Ophthalmol Vis Sci. 2000;41:3726–3731 [PubMed] [Google Scholar]
- 24. Woodruff ME. Cross sectional studies of corneal and astigmatic characteristics of children between the twenty-fourth and seventy-second months of life. Am J Optom. 1971;48:650–659 [PubMed] [Google Scholar]
- 25. Huynh SC, Kifley A, Rose KA, Morgan I, Heller GZ, Mitchell P. Astigmatism and its components in 6-year-old children. Invest Ophthalmol Vis Sci. 2006;47:55–64 [DOI] [PubMed] [Google Scholar]
- 26. Lai YH, Hsu HT, Wang HZ, Change CH, Chang SJ. Astigmatism in preschool children in Taiwan. J AAPOS. 2010;14:150–154 [DOI] [PubMed] [Google Scholar]
- 27. Garber JM. High corneal astigmatism in Navajo school children and its effect on classroom performance. J Am Optom Assoc. 1981;52:583–586 [PubMed] [Google Scholar]
- 28. Maples WC, Herrmann M, Hughes J. Corneal astigmatism in preschool Native Americans. J Am Optom Assoc. 1997;68:87–94 [PubMed] [Google Scholar]
- 29. Lyle WM, Grosvenor T, Dean KC. Corneal astigmatism in Amerind children. Am J Optom Arch Am Acad Optom. 1972;49:517–524 [DOI] [PubMed] [Google Scholar]
- 30. Howland HC, Sayles N. Photokeratometric and photorefractive measurements of astigmatism in infants and young children. Vision Res. 1985;25:73–81 [DOI] [PubMed] [Google Scholar]
- 31. Mutti DO, Mitchell GL, Jones LA, et al. Refractive astigmatism and the toricity of ocular components in human infants. Optom Vis Sci. 2004;81:753–761 [DOI] [PubMed] [Google Scholar]
- 32. Twelker JD, Mitchell GL, Messer DH, et al. and the CLEERE Study Group Chidren's ocular components and age, gender, and ethnicity. Optom Vis Sci. 2009;86:918–935 [DOI] [PMC free article] [PubMed] [Google Scholar]