In this article, the authors show that hyperoxia treatment prevents pathologic neovascularization and promotes physiological vascular repair in ischemic retinopathy.
Abstract
Purpose.
To investigate the therapeutic use and mechanisms of action of normobaric hyperoxia to promote revascularization and to prevent neovascularization in a mouse model of oxygen-induced ischemic retinopathy.
Methods.
Hyperoxia treatment (HT, 40%–75% oxygen) was initiated on postnatal day (P) 14 during the pre-proliferative phase of ischemic retinopathy. Immunohistochemistry, ELISA, and quantitative PCR were used to assess effects on retinal vascular repair and pathologic angiogenesis in relation to glial cell injury, VEGF protein, and mRNA levels of key mediators of pathologic angiogenesis. Effects of intravitreal injections of VEGF and the VEGF inhibitor VEGFR1/Fc fusion protein were also studied.
Results.
Administration of HT during the ischemic pre-proliferative phase of retinopathy effectively accelerated the process of revascularization while preventing the development of vitreous neovascularization. HT enhanced the formation of specialized endothelial tip cells at the edges of the repairing capillary networks and blocked the overexpression of several molecular mediators of angiogenesis, inflammation, and extracellular proteolysis. HT markedly reduced the reactive expression of GFAP in Müller cells and improved the morphology of astrocytes in the avascular region of the retina. Exogenous VEGF administered into the vitreous on P14 was not sufficient to cause vitreous neovascularization in the HT mice. Injection of the VEGF antagonist VEGFR1/Fc blocked both pathologic and physiological angiogenesis and did not rescue astrocytes.
Conclusions.
HT may be clinically useful to facilitate vascular repair while blocking neovascularization in the pre-proliferative stage of ischemic retinopathy by correcting a broad range of biochemical and cellular abnormalities.
Ischemic retinopathy is the leading cause of blindness in persons younger than 60 in the United States. It is a complication of diabetes, retinal vein occlusion, and retinopathy of prematurity, with loss of vision occurring as a result of retinal hypoxia, increased vascular permeability, and pathologic neovascularization (NV). Considerable scientific and clinical investigation have focused on identifying the molecular mediators involved in initiating pathologic angiogenesis in the retina and developing effective inhibitors. Anti-VEGF agents are now in widespread use in the treatment of patients with subretinal neovascularization associated with age-related macular degeneration and are being investigated in clinical trials in diabetic retinopathy.1 Several antiangiogenic agents are in clinical use to manage a wide variety of conditions involving pathologic angiogenesis and vascular permeability in the eye.1 Several issues, however, detract from the potential clinical value of these agents.
Whereas angiogenic inhibitors are effective in reversing vascular permeability and eliminating NV, this therapy does not address the issue of retinal ischemia or promote the normal vascular repair that is essential to ending tissue hypoxia and maintaining normal function. In fact, an inhibitor's lack of antiangiogenic selectivity might adversely impact the process of physiological vascular repair.2,3 Similarly, suppression of VEGF-mediated cell survival pathways in hypoxic neurons might inhibit neuronal survival and function.4 In addition, antiangiogenic therapy is not indicated at the pre-proliferative stage of ischemic retinopathy, a time when metabolic support of the retina and repair of the damaged capillary beds are most critical. Delivery of antiangiogenic agents by intravitreal injection also carries a risk for vision-threatening endophthalmitis and uveitis.5,6
The therapeutic use of oxygen has been extensively studied in wound healing,7,8 especially in clinical situations in which tissue perfusion is compromised by arterial insufficiency,9 diabetes,10,11 or previous radiation treatment for neoplasia.12 Numerous studies support the use of hyperbaric oxygen as adjunctive treatment for nonhealing lower extremity wounds in patients with diabetes,10,11 compromised tissue flaps and grafts,13 and radiation-induced ischemic osteonecrosis.14 Experiments in various animal models of ischemia have suggested that supplemental oxygen can improve the rate of wound healing and reduce apoptosis in the affected tissue.8,15 In addition to supporting oxidative phosphorylation, oxygen plays a critical role in redox signaling for cytokines, including VEGF and PDGF, and in cell motility, integrin function, and leukocyte recruitment.7,8,16
The therapeutic effects of oxygen supplementation in ischemic retinopathy have not been well characterized. However, it has been shown that hyperbaric oxygen treatment reduces breakdown of the blood-retinal barrier in streptozotocin-induced diabetic rats.17 In humans, small case series have suggested that normobaric supplemental oxygen can reduce vascular permeability and retinal thickness in diabetic macular edema18 and central retinal vein occlusion.19,20 Oxygen supplementation immediately after vaso-obliteration but before the onset of retinal hypoxia was also shown to reduce the severity of vitreous NV and to attenuate the degeneration of astrocytes in oxygen-induced retinopathy (OIR) models.21–23 These clinical and scientific studies support the potential value of oxygen therapy as a primary or adjunctive treatment for vision-threatening ischemic retinopathies.24
In the present study, we investigated the therapeutic benefit of oxygen supplement during the ischemic pre-proliferative phase of ischemic retinopathy in an OIR mouse model. Unlike other studies that start treatment of ischemic retinopathy before the onset of hypoxia, we initiated hyperoxia treatment (HT) after a period of retinal ischemia, when the multiple signs of ischemic retinopathy—such as no perfusion in the central retina, tortuous and dilated vessels,25 and upregulation of many angiogenic and inflammatory genes in the retina—are evident. This delay was chosen to determine the potential clinical use of HT in the pre-proliferative stage of ischemic retinopathy because most patients with ischemic retinopathy seek evaluation before NV has developed. We show that normobaric HT after a period of retinal ischemia selectively blocks the development of pathologic NV while it simultaneously accelerates the process of physiologic revascularization. Mechanistically, we further demonstrate the beneficial effect of HT may be attributed to its pleiotropic effect by correcting a broad range of biochemical and cellular abnormalities. Our data strongly support the potential of hyperoxia as an effective primary or adjunctive therapy for pre-proliferative ischemic retinopathy.
Methods
Treatment of Animals
All procedures with animals were performed in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research and were approved by the institutional animal care and use committee (Animal Welfare Assurance no. A3307-01). OIR was induced by exposing C57BL/6J mice to 75% oxygen from postnatal day (P) 7 to P12, followed by a return to room air until P17 or P20 (OIR groups). To investigate the effect of HT, OIR mice were maintained in room air from P12 to P14 and were then returned to 75% or 40% oxygen for various times (HT groups). Age-matched mice kept in room air served as room air control. Nutritional status is known to alter retinal neovascularization during OIR, and hyperoxia and return to room air can stress mice, which affects feeding. Thus, handling of the pups was kept to a minimum in experiments. The dams and pups were monitored closely during experiments, and surrogate dams were introduced if signs of stress were observed. On P14, pups were weighed; the weight range was 4.5 to 4.8 g. At the end of the experiment, the mice were killed, and one eye from each mouse was fixed in 4% paraformaldehyde for morphology studies. The contralateral retina was dissected, frozen in liquid nitrogen, and used for the measurement of mRNA by quantitative RT- PCR. All mice were weighed before kill, and there were no significant differences in body weight between the OIR and HT groups (Table 1).
Table 1.
Mouse Body Weights by Postnatal Day and Group
| P17 |
P20 |
||||
|---|---|---|---|---|---|
| OIR (n = 17) | HT (75% O2) (n = 17) | OIR (n = 9) | HT (75% O2) (n = 9) | HT (40% O2) (n = 6) | |
| Body weight, g | 5.1 ± 0.1 | 5.3 ± 0.2 | 5.9 ± 0.1 | 5.8 ± 0.1 | 6.3 ± 0.3 |
n, number of mice.
Intravitreal Injection
Mice were anesthetized by intraperitoneal injection of anesthetic (tribromoethanol; Avertin; 625 mg/kg). Intravitreal injections were performed by delivering 1 μL PBS containing 2 μg VEGFR1/Fc fusion protein or mouse VEGF (R&D Systems, Minneapolis, MN) or vehicle only with a 36-gauge needle mounted to a 10-μL Hamilton syringe. The tip of the needle was inserted under the guidance of a dissecting microscope (Wild M650; Leica, Bannockburn, IL) through the dorsal limbus of the eye. Injections were performed slowly throughout a period of 2 minutes.
Immunostaining on Wholemount Retinas
Retinas were carefully dissected, blocked, and permeabilized in PBS containing 10% goat serum and 1% Triton-X-100 for 30 minutes. Then retinas were incubated with Alex 594–labeled isolectin B4 (Griffonia simplicifolia; Invitrogen, Carlsbad, CA) and polyclonal rabbit anti-mouse glial fibrillary acidic protein (GFAP) (1:200; Dako, Carpinteria, CA) overnight at 4°C with gentle rocking. After washing in PBS, retinas were incubated with Alex 488–conjugated goat anti–rabbit antibody at 1:400 (Invitrogen) for 4 hours at 4°C. Retinas were washed with PBS, mounted on microscope slides in mounting medium (Vectashield; Vector Laboratories, Burlingame, CA), and examined by fluorescence microscopy (Axiophot; Carl Zeiss, Thornwood, NY) and by confocal microscopy (Zeiss 510; Carl Zeiss). Areas of vaso-obliteration and vitreoretinal neovascular tufts were quantified by using ImageJ software (developed by Wayne Rasband, National Institutes of Health, Bethesda, MD; available at http://rsb.info.nih.gov/ij/index.html) as reported.26
Immunostaining on Retinal Sections
After eyes were fixed in 4% paraformaldehyde, retinas were carefully dissected, equilibrated in 30% sucrose, embedded in optimal cutting temperature compound frozen in liquid nitrogen, and cut into 10-μm sections. Retinal sections were permeabilized with PBS containing 1% Triton X-100 for 30 minutes at room temperature and blocked with 3% normal goat serum for 30 minutes. Sections were incubated overnight at 4°C with rabbit polyclonal anti–GFAP antibody. After washing in PBS, sections were incubated with Alexa 488–conjugated goat anti–rabbit antibody at 1:500 (Invitrogen) for 1 hour at room temperature, washed with PBS, covered in mounting medium containing DAPI (Vector Laboratories) under a coverslip, and examined by fluorescence microscopy (Carl Zeiss).
RT-PCR Assay
Total RNA was isolated using a kit (RNA 4PCR kit; Applied Biosystems, Austin, TX) according to the manufacturer's instructions. Total RNA was reverse transcribed with reverse transcriptase (M-MLV; Invitrogen) to generate cDNA. Quantitative PCR was performed (StepOne PCR system; Applied Biosystems) with Power SYBR Green.27 The fold difference in various transcripts was calculated by the CT method using 18S as the internal control. After PCR, a melting curve was constructed in the range of 60°C to 95°C to evaluate the specificity of the amplification products. Primer sequences for mouse transcripts are shown in Table 2.
Table 2.
Primers Used for q-PCR
| Gene Name | Forward Primer | Reverse Primer |
|---|---|---|
| VEGF | TACCTCCACCATGCCAAGTG | TCATGGGACTTCTGCTCTCCTT |
| FGF-2 | TGGTATGTGGCACTGAAACGA | TCCAGGTCCCGTTTTGGAT |
| PDGF-A | GCTGCACTGGCTGTTGTAACA | GGTGGTGGACCCGTGAAG |
| Ang2 | ACACCGAGAAGATGGCAGTGT | CTCCCGAAGCCCTCTTTGTA |
| EPO | CCCCCACGCCTCATCTG | TGCCTCCTTGGCCTCTAAGA |
| IGFBP-3 | AGGTTGTCCCCAGCACACA | TTGGCATGGAGTGGATGGA |
| TNF-α | GGTCCCCAAAGGGATGAGAA | TGAGGGTCTGGGCCATAGAA |
| MCP-1 | GGCTCAGCCAGATGCAGTTAA | CCTACTCATTGGGATCATCTTGCT |
| ICAM-1 | CAGTCCGCTGTGCTTTGAGA | CGGAAACGAATACACGGTGAT |
| iNOS | GGCAGCCTGTGAGACCTTTG | TGCATTGGAAGTGAAGCGTTT |
| uPAR | CCACAGCGAAAAGACCAACA | TGTCAGGCTGATGATCATGGA |
| PAI-I | CGACACCCTCAGCATGTTCA | CGGAGAGGTGCACATCTTTCT |
| GFAP | CCAGCTTCGAGCCAAGGA | GAAGCTCCGCCTGGTAGACA |
ELISA
Mouse eyeballs (or retinas) were lysed by sonication with RIPA lysis buffer (50 mM Tris-HCl, pH 7.4, 150 mM NaCl, 0.25% deoxycholic acid, 1% NP-40, 1 mM EDTA) supplemented with protease inhibitors. The lysate was cleared of debris by centrifugation, and the supernatant was used for ELISA with a mouse VEGF ELISA kit (R&D Systems). Protein concentration in the lysates was determined by a BCA assay (Pierce Biotechnology, Rockford, IL). VEGF concentration was normalized to total protein in the lysate and then calculated as fold increase relative to the control.
Statistical Analysis
The results are expressed as mean ± SEM. Group differences were evaluated by using one-way ANOVA followed by post hoc Student's t-test. Results were considered significant at P < 0.05.
Results
HT Accelerates Retinal Revascularization in Pre-Proliferative Ischemic Retinopathy and Prevents NV
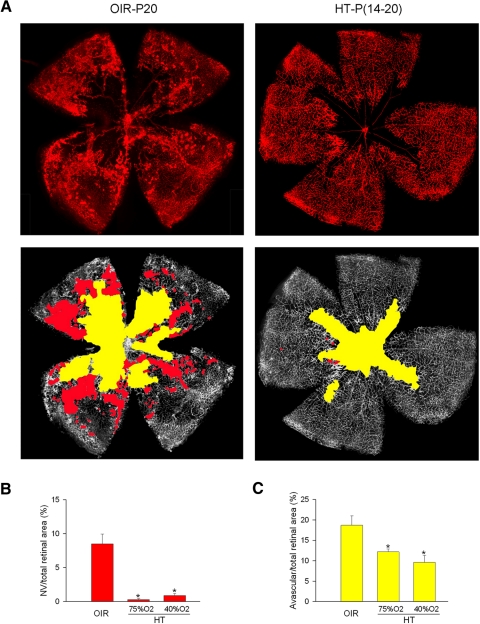
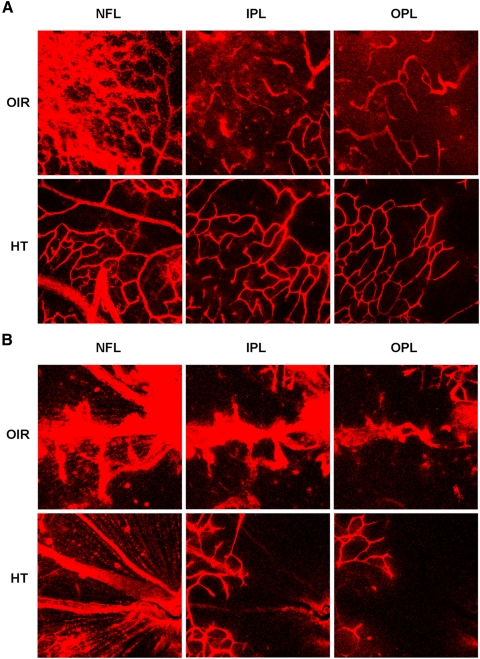
Studies were performed in the mouse model of ischemic retinopathy (OIR) in which obliteration of the immature retinal vessels is induced by exposure to 75% oxygen from P7 through P12. Immediately on return to room air, the avascular central retina becomes hypoxic, leading to the upregulation of many angiogenic and inflammatory genes.28 However, vitreous NV is not initiated until P15, which is 3 days after the onset of retinal hypoxia.25,29 This model has been widely used for studies of mechanisms and strategies for the blockade of pathologic NV,2,25,30–36 but very little is known about the mechanisms of vascular repair. Given that most patients with ischemic retinopathy present for evaluation before the development of NV, we initiated HT after a period of retinal ischemia to determine its potential clinical use in the pre-proliferative stage of ischemic retinopathy. Our data (Fig. 1) show that the HT prevented vitreous NV and accelerated revascularization of the central retina compared with room air ischemic controls. These effects were highly significant by P20, at which time retinal NV was reduced by 96% and the avascular area was reduced by 35%. Confocal microscopy of lectin-labeled capillaries (Fig. 2) showed that vascular recovery in hyperoxia was enhanced in both the deep and the superficial plexuses. Supplemental oxygen was effective in promoting revascularization and blocking NV at concentrations as low as 40%. There was no statistical difference between 75% and 40% oxygen supplements (Fig. 1). Retinas analyzed at P17, after 3 days of rescue hyperoxia, showed a reduction of NV by 98%, though improved revascularization was not yet evident (Supplementary Fig. S1, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7666/-/DCSupplemental).
Figure 1.
HT reduces NV tufts formation and accelerates retina revascularization in OIR. OIR mice were treated with hyperoxia (75% or 40% oxygen; HT) or were maintained in room air (OIR) from P14 to P20. (A) Retinas from OIR mice treated with 75% oxygen were whole flatmounted at P20. Representative images are shown. Original magnification, ×5. (B) NV areas (red) and (C) avascular areas (yellow) were quantified (n = 6–9 retinas from 6–9 mice). *P < 0.05 compared with OIR.
Figure 2.
HT accelerates revascularization of deep layers. OIR mice were treated with hyperoxia (75% oxygen; HT) or were maintained in room air (OIR) from P14 to P20. Retinas were whole flatmounted at P20. Retinal vasculature in nerve fiber layer (NFL), inner plexiform layer (INL), and outer plexiform layer (OPL) was visualized by confocal microscopy. Representative images are shown (n = 9 retinas from 9 mice). Original magnification, ×20. (A) Vessels in the peripheral retina. (B) Vessels in the central retina.
HT Increases the Formation of Endothelial Tip Cells
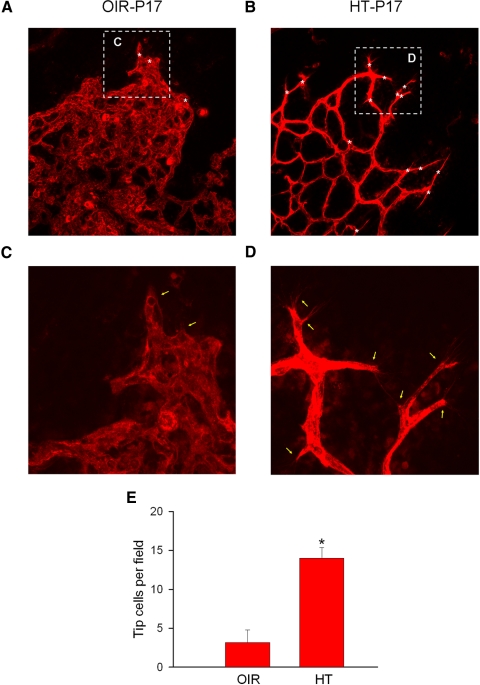
To examine potential cellular mechanisms underlying the beneficial effects of HT, the formation of endothelial tip cells was analyzed at P17 after 3 days of HT. Endothelial tip cells are critical for the development of new capillaries. They are characterized by the presence of specialized apical filopodia that mediate directional migration. Their migration is thought to be guided in part by receptor-mediated responses to cytokine gradients and by interactions with astrocytes, extracellular matrix, and cell surface adhesion molecules. In OIR, these cells were notably sparse at the junction of the vascular and avascular retina on P17 (Fig. 3). In areas lacking endothelial tip cells, the capillaries were poorly developed, and pathologic extension of vessels into the vitreous was present. On the other hand, in mice treated with hyperoxia beginning on P14, the density and distribution of endothelial tips cells was increased 3.4-fold compared with untreated controls (Fig. 3E), indicating that cellular and molecular factors critical to a normal angiogenic response were rescued.
Figure 3.
HT increases tip cells in OIR. OIR mice were treated with hyperoxia (75% oxygen; HT) or were maintained in room air (OIR) from P14 to P17. Retinas were whole flatmounted at P17. Representative images of retinal tip cells (white asterisk) and filopodia (yellow arrow) are shown. (A, B) OIR and HT. Original magnification, ×20. (C, D) High-magnification image from top of A and B. Original magnification, ×40. (E) Quantification of numbers of tip cells (n = 3 retinas from 3 mice). *P < 0.05 compared with OIR.
HT Rescues Astrocytes
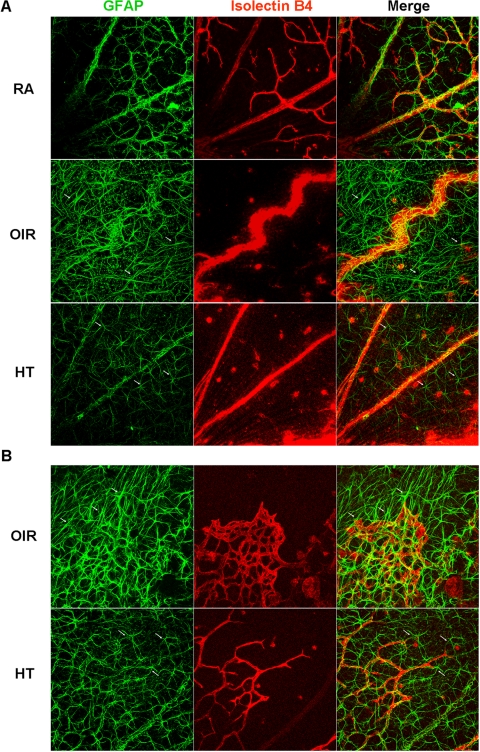
Astrocytes form the vascular template that guides physiological angiogenesis during retinal development.37,38 Aberrant astrocyte function, such as overactive CK2 or hypoxia-induced astrocyte degeneration, is involved in ischemia-induced vitreous neovascularization.22,39,40 OIR retinas analyzed on P17 showed extensive alterations in astrocyte morphology and distribution. The density of astrocytes in the central retina was increased, and many showed a spindle-shaped morphology with extensive overlapping (Fig. 4A). In mice treated with HT, astrocytes in the central retina formed a better network than those with OIR and retained their normal stellate/dendritic morphology (Fig. 4A). Their distribution was also more uniform and lacked the irregular overlap and variations in density seen with OIR. The transition zone between the vascular and avascular retina was also a transition zone for astrocyte morphology and distribution (Fig. 4B) in both OIR and hyperoxia-treated eyes. In areas with a capillary plexus, astrocytes were evenly distributed and were arranged in a reticular configuration, mirroring the capillaries. In HT-treated eyes, the density of capillaries was reduced compared with OIR eyes, though the capillaries that were present conformed to the template of underlying astrocytes. The formation of an astrocyte plexus slightly preceded the leading edge of developing capillaries, similar to the pattern described for developmental angiogenesis in the neonatal mouse retina.37
Figure 4.
HT improves the status of astrocyte network and morphology. OIR mice were treated with hyperoxia (75% oxygen; HT) or were maintained in room air (OIR) from P14 to P17. Mice maintained in room air (RA) from P1 to P17 are control. Retinal flatmounts were stained with isolectin B4 (red) and anti-GFAP (green). Representative confocal images are shown (n = 9 retinas from 9 mice). (arrows) Examples of astrocytes with different morphology in OIR (spindle-shaped) and HT (stellate). The punctate staining for GFAP in the flatmounts represents cross-sections of Müller cells expressing GFAP. Original magnification, ×20. (A) Central retina. (B) Revascularization area.
HT Reduces GFAP Expression in Müller Cells
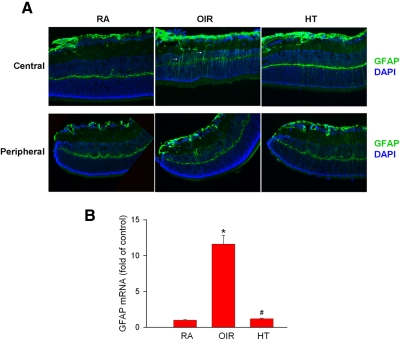
Müller cells are activated and involved in the development of pathologic angiogenesis.41,42 The reaction of Müller cells was determined by immunolabeling GFAP, a marker for Müller cell activation.39,43 Under normoxic conditions, GFAP-containing intermediate filaments are robustly expressed in processes associated with the superficial and deep vessels (Fig. 5A). OIR induces the activation of Müller cells in the central retina during the ischemic phase, as indicated by their robust expression of GFAP-containing filaments throughout their processes. Activation is minimal in peripheral areas of the retina, where capillary perfusion is preserved. Although GFAP expression in the nerve fiber layer is not changed, its expression in the Müller cell body in the central retina is suppressed by HT (Fig. 5A) compared with OIR. Quantitative PCR analysis of whole retina on P17 demonstrates that ischemia-induced expression of GFAP mRNA (11.6 ± 1.2-fold of control) is completely blocked by HT (1.2 ± 0.1-fold of control) (Fig. 5B). The expected lag between decreased mRNA expression and turnover of intermediate filament proteins would explain the residual GFAP immunolabeling seen on P17 in the HT retinas in spite of mRNA levels having already returned to normal.
Figure 5.
HT reduces GFAP expression. OIR mice were treated with hyperoxia (75% oxygen; HT) or were maintained in room air (OIR) from P14 to P17. Mice maintained in room air (RA) from P1 to P17 are control. (A) Retinal frozen sections were stained with anti-GFAP (green) and DAPI (blue). Arrows: Müller cell processes expressing GFAP. Representative fluorescence microscopy images of central and peripheral retinas (n = 3 retinas from 3 mice). Original magnification, ×20. (B) GFAP mRNA in retinas was quantified by q-PCR and normalized to RA control (n = 6–9 retinas from 6–9 mice). *P < 0.05 compared with RA. #P < 0.05 compared with OIR.
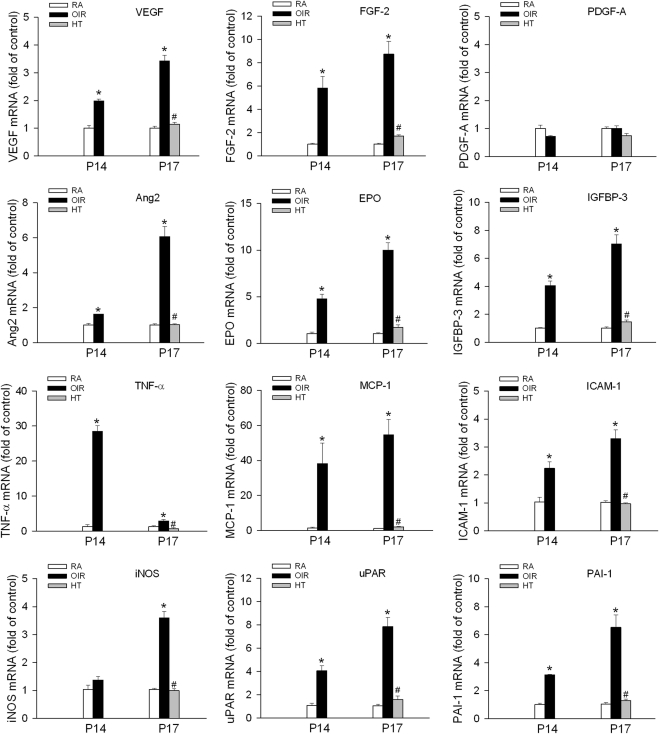
HT Normalizes Molecular Mediators of Angiogenesis and Inflammation
To investigate the molecular mechanisms underlying the beneficial effect of HT, the expression of known mediators of NV, including angiogenic factors (VEGF, FGF-2, PDGF-A, angiopoietin 2, erythropoietin, IGFBP-3), inflammatory molecules (TNF-α, ICAM-1, MCP-1, iNOS), and extracellular proteolytic molecules (urokinase plasminogen activator receptor [uPAR], PAI-1), were determined by quantitative PCR. As expected, the expression of these molecules is significantly increased by 0.4- to 54-fold after 2 or 5 days of OIR (Fig. 6). However, HT completely normalized the expression of each of these genes to the levels seen in the controls (non-OIR, room air). The observed downregulation of hypoxia-responsive genes, including VEGF and erythropoietin (EPO, suggests that HT decreases HIF-1α expression to normoxic levels. The downregulation of iNOS, ICAM-1, and MCP-1 suggests that supplemental oxygen also exerts a potent anti-inflammatory effect. Interestingly, PDGF-A, which is normally expressed by retinal ganglion cells and is known to play a prominent role in astrocyte recruitment and vascular patterning during retinal development,37 was not affected by either OIR or HT.
Figure 6.
HT normalizes the expression of angiogenic, inflammatory, and proteolytic molecules in OIR. OIR mice were treated with hyperoxia (75% oxygen; HT) or were maintained in room air (OIR) from P14 to P17. Mice maintained in room air (RA) from P1 to P17 are control. mRNA levels of specified molecules in retinas were quantified by q-PCR and normalized to RA control (n = 6–9 retinas from 6–9 mice). *P < 0.05 compared with RA. #P < 0.05 compared with OIR.
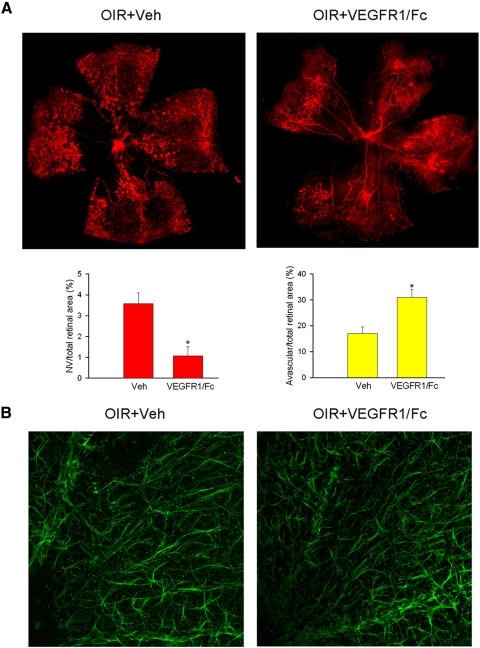
Intravitreal Injection of a VEGF Antagonist Blocks Pathologic and Physiological Angiogenesis
In addition to the increase in VEGF mRNA shown by quantitative PCR, analysis of VEGF protein in the retina also revealed close to a 3.2-fold increase that was decreased to the level of room air control by HT (1.2 ± 0.1-fold of control; Supplementary Fig. S2, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7666/-/DCSupplemental). To compare the relative efficacy of HT with anti-VEGF therapy, VEGFR-1/Fc (VEGF trap) was administered by intravitreal injection on P14 in OIR mice. VEGF blockade potently suppressed vitreous NV by 79% but also blocked retinal revascularization and increased the avascular area by 82% (Fig. 7A). It also induced further regression of the primary vascular plexus and thus reduced vascular density in the peripheral retina. These findings confirm the essential role of VEGF in normal retinal angiogenesis and in the formation of pathologic vessels in the vitreous. In contrast with the improved astrocyte morphology observed with HT (Fig. 4), alterations in astrocyte morphology and distribution found in VEGF antagonist-treated eyes were similar to those in vehicle-treated OIR eyes (Fig. 7B).
Figure 7.
Blocking VEGF inhibits NV and revascularization in OIR but does not prevent the disruption of the astrocyte network. OIR mice were intravitreally injected with PBS (Veh) or VEGF blocker (VEGFR1/Fc, 2 μg/eye) at P14. Retinal vasculature (isolectin B4, red) and astrocyte network (GFAP, green) were analyzed at P17 in flatmount. (A) Representative images of retinal flatmount and quantification of NV and avascular areas (n = 4 retinas from 4 mice). *P < 0.05 compared with Veh. Original magnification, ×5. (B) Representative confocal images of astrocyte in the central retina are shown (n = 4 retinas from 4 mice). Original magnification, ×20.
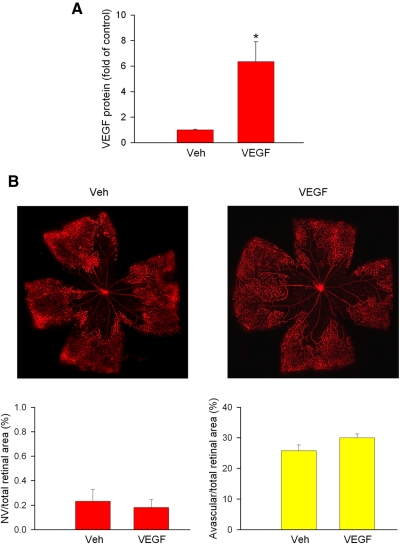
Intravitreal VEGF Does Not Cause Pathologic NV in Hyperoxia-Treated Eyes
HT effectively blocks the upregulation of VEGF in eyes made ischemic by OIR (Supplementary Fig. S2, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7666/-/DCSupplemental). To test whether blockade of VEGF expression is the critical mechanism by which hyperoxia prevents vitreous NV, we administered exogenous VEGF intravitreally on P14 in mice receiving HT. Our results showed that HT continued to prevent NV in spite of a 5.3-fold elevated level of VEGF protein (Fig. 8), suggesting that VEGF is necessary but not sufficient for the development of extraretinal NV. Exogenous VEGF did not alter the rate of revascularization compared with hyperoxia alone.
Figure 8.
VEGF supplement does not induce NV in hyperoxia-treated OIR mice. OIR mice were intravitreally injected with PBS (Veh) or VEGF (2 μg/eye) at P14 and then were treated with hyperoxia (75% oxygen) from P14 to P17. (A) VEGF levels in the ocular of P17 mice were determined by ELISA and normalized to vehicle control (n = 3 eyes from 3 mice). (B) Retinal vasculature (isolectin B4, red) at P17 in flatmount and quantification of NV and avascular areas were shown (n = 6 retinas from 6 mice). Original magnification, ×5.
Discussion
Ischemic retinopathy is characterized by a period of retinal ischemia (pre-proliferative stage) caused by vessel regression or occlusion, followed by pathologic retinal NV (proliferative stage). It is at the pre-proliferative stage of ischemic retinopathy that many patients first present to the ophthalmologist. Few therapeutic options exist at that point, and clinical observation for progression to NV is typically recommended. In this study, we determined the effects of supplying oxygen during the pre-proliferative stage of ischemic retinopathy. We demonstrate that HT with a range of oxygen concentrations after a period of retinal ischemia prevents the development of NV as effectively as supplying oxygen before the onset of retinal hypoxia21,23 in pre-proliferative ischemic retinopathy. Moreover, HT promoted the recovery and repair of damaged capillary beds within the retina, thus offering the possibility of significantly improving visual outcomes compared with current antiangiogenic or retinal ablative interventions. This study, together with previous studies showing similar beneficial effects when oxygen is supplied immediately after vessel regression but before retinal ischemia,21,23 indicates a broad therapeutic time window for HT in the pre-proliferative stage of ischemic retinopathy. The noninvasive and nondestructive nature of this intervention makes it particularly appealing for clinical use.
Thus far, only limited investigation of oxygen therapy in human ischemic retinopathy has been reported. Its use in human retinopathy of prematurity is limited by the clinical challenges of tightly controlling blood oxygenation in neonates whose conditions are unstable and by the potential for inducing oxygen-related pulmonary complications in the premature infant.44–46 In spite of these limitations, a randomized trial of supplemental oxygen did demonstrate a notable trend toward producing better retinal outcomes in infants with pre-threshold ROP.44 Oxygen therapy has also been evaluated in a small case series of patients with chronic diabetic macular edema18 and was found to cause significant and prolonged reduction in central macular thickness and improved visual function. We are not aware of any trials evaluating oxygen therapy in patients with diabetic retinopathy with significant ischemia (pre-proliferative or proliferative); however, case reports have been published19,20 in which hyperbaric oxygen therapy has been successfully used in central retinal vein occlusion with good visual outcomes.
Because hypoxia is thought to be a driving force behind angiogenesis, it is surprising that hyperoxia promotes retinal vascular recovery. This observation suggests that key physiological differences exist between the control of reparative angiogenesis and developmental angiogenesis in the retina. Although we did not directly measure tissue oxygen levels in the retina, the fact that VEGF and EPO mRNA expression were reduced to normoxic control levels by hyperoxia indicates that relief of cellular hypoxia was biologically significant. These data suggest that the expansion and survival of capillary networks during retinal revascularization is neither sensitive to high levels of inspired oxygen nor critically related to hypoxia-driven expression of VEGF or EPO, as has been shown for capillaries involved in developmental angiogenesis.33,47 Although it has been reported that oxygen-induced vaso-obliteration is significantly reduced in the retinas of transgenic mice that overexpress PDGF-α or IGFBP-3 and is enhanced in mice lacking IGFBP-3,48–50 our analysis showed that PDGF-α expression in hyperoxia-treated eyes was not significantly different from PDGF-α expression in ischemic controls and that IGFBP-3 levels were reduced by hyperoxia to those of room air control mice, suggesting protection from hyperoxia during vascular repair is mediated by other factors. Clinically, these data indicate that the use of therapeutic oxygen is not likely to adversely affect retinal revascularization in pre-proliferative ischemic retinopathy used outside the early developmental window seen in premature infants.
One cellular mechanism that may explain the improved vascular recovery in HT-treated eyes is the emergence of increased numbers of endothelial tip cells. It has been shown that these cells, which are critical to angiogenesis, depend on a physiological gradient of VEGF acting through the KDR/flk-1 receptor.51 Such gradients may be disrupted in severely ischemic tissue. The presence of appropriately directed endothelial tip cells in HT retinas indicates active, directional endothelial cell migration,51,52 implying physiological rather than pathologic regulation of angiogenesis. Conversely, the relative paucity of tip cells in non–HT-treated eyes suggests a disruption of normal signaling and cell-cell interactions involved in revascularization.
HT-induced rescue of astrocytes may also be crucial because the migration of endothelial tip cells is thought to be mediated in part by their interaction with cell adhesion molecules such as R-cadherin, expressed on the surfaces of astrocytes.38 Our immunohistochemical analysis of GFAP expression indicates that HT decreases the activation of Müller glia and improves the status of the astrocyte network in the avascular areas, facilitating the formation of a template over which proliferating intraretinal capillaries can form. Appropriate astrocyte-endothelial cell interactions would not only promote repair of the superficial vascular plexus but would also serve to limit pathologic extension of the vessels into the vitreous,53–55 thereby maintaining proper vascular compartmentalization.
To identify critical molecular mediators involved in HT, we performed RT-PCR analysis of several genes known to play key roles in pathologic NV. These included angiogenic cytokines, inflammatory mediators, and extracellular proteolytic molecules involved in cell migration. Interestingly, HT normalized the expression of each of these genes, demonstrating its pleiotropic effect in ischemic retinopathy. Although it is not possible to determine from this analysis which of these many factors might have been most critical, it is reasonable to assume that all might have had important and potentially interdependent contributions. Supporting this notion, whereas administration of a VEGF antagonist was sufficient to block pathologic NV in normoxic eyes subjected to OIR, exogenously administered intravitreal VEGF did not promote pathologic NV in eyes treated with hyperoxia. Selective suppression of pathologic NV in the presence of elevated VEGF expression has also been achieved consistently in the rodent model of OIR by the pharmacologic inhibition of retinal iNOS,35,56 TNF-α,34 or the angiotensin type 1 receptor57 or by the activation of peroxisome proliferator-activated receptor gamma.58 In this regard, the pleiotropic effect of HT makes it an appealing therapeutic approach for ischemic retinopathy, particularly because it does not aversely affect vascular repair, as seen with VEGF blockade. However, it is also expected that the beneficial role of HT will be transient unless such treatment is maintained until physiological vascular repair is complete. Further investigation is needed to establish the relevant dose-response relationship of HT and to better define the key molecular and cellular mechanisms involved in tip cell formation, glial rescue, and vascular repair during such treatment.
Supplementary Material
Footnotes
Supported by the Georgia Health Sciences University Vision Discovery Institute (SEB, RBC); National Eye Institute Grants R01 EY04618 (RBC) and R01 EY11766 (RBC, RWC); Veterans Administration MRA (RBC); National Heart, Lung, and Blood Institute Grant R01 HL70215 (RWC); American Heart Association Grant 11SDG4960005; and Juvenile Diabetes Research Foundation Grant JDRF 10-2009-575 (WZ).
Disclosure: W. Zhang, None; H. Yokota, None; Z. Xu, None; S.P. Narayanan, None; L. Yancey, None; A. Yoshida, None; D.M. Marcus, None; R.W. Caldwell, None; R.B. Caldwell, None; S.E. Brooks, None
References
- 1. Tolentino MJ. Current molecular understanding and future treatment strategies for pathologic ocular neovascularization. Curr Mol Med. 2009;9:973–981 [DOI] [PubMed] [Google Scholar]
- 2. Ishida S, Usui T, Yamashiro K, et al. VEGF164-mediated inflammation is required for pathological, but not physiological, ischemia-induced retinal neovascularization. J Exp Med. 2003;198:483–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McLeod DS, Taomoto M, Cao J, Zhu Z, Witte L, Lutty GA. Localization of VEGF receptor-2 (KDR/Flk-1) and effects of blocking it in oxygen-induced retinopathy. Invest Ophthalmol Vis Sci. 2002;43:474–482 [PubMed] [Google Scholar]
- 4. Nishijima K, Ng YS, Zhong L, et al. Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol. 2007;171:53–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ness T, Feltgen N, Agostini H, Bohringer D, Lubrich B. Toxic vitreitis outbreak after intravitreal injection. Retina. 30:332–338 [DOI] [PubMed] [Google Scholar]
- 6. Pilli S, Kotsolis A, Spaide RF, et al. Endophthalmitis associated with intravitreal anti-vascular endothelial growth factor therapy injections in an office setting. Am J Ophthalmol. 2008;145:879–882 [DOI] [PubMed] [Google Scholar]
- 7. Sen CK. Wound healing essentials: let there be oxygen. Wound Repair Regen. 2009;17:1–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang Q, Chang Q, Cox RA, Gong X, Gould LJ. Hyperbaric oxygen attenuates apoptosis and decreases inflammation in an ischemic wound model. J Invest Dermatol. 2008;128:2102–2112 [DOI] [PubMed] [Google Scholar]
- 9. Knighton DR, Silver IA, Hunt TK. Regulation of wound-healing angiogenesis-effect of oxygen gradients and inspired oxygen concentration. Surgery. 1981;90:262–270 [PubMed] [Google Scholar]
- 10. Abidia A, Laden G, Kuhan G, et al. The role of hyperbaric oxygen therapy in ischaemic diabetic lower extremity ulcers: a double-blind randomised-controlled trial. Eur J Vasc Endovasc Surg. 2003;25:513–518 [DOI] [PubMed] [Google Scholar]
- 11. Faglia E, Favales F, Aldeghi A, et al. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer: a randomized study. Diabetes Care. 1996;19:1338–1343 [DOI] [PubMed] [Google Scholar]
- 12. Chong KT, Hampson NB, Corman JM. Early hyperbaric oxygen therapy improves outcome for radiation-induced hemorrhagic cystitis. Urology. 2005;65:649–653 [DOI] [PubMed] [Google Scholar]
- 13. Monies-Chass I, Hashmonai M, Hoere D, Kaufman T, Steiner E, Schramek A. Hyperbaric oxygen treatment as an adjuvant to reconstructive vascular surgery in trauma. Injury. 1977;8:274–277 [DOI] [PubMed] [Google Scholar]
- 14. Feldmeier JJ, Hampson NB. A systematic review of the literature reporting the application of hyperbaric oxygen prevention and treatment of delayed radiation injuries: an evidence based approach. Undersea Hyperb Med. 2002;29:4–30 [PubMed] [Google Scholar]
- 15. Gordillo GM, Sen CK. Revisiting the essential role of oxygen in wound healing. Am J Surg. 2003;186:259–263 [DOI] [PubMed] [Google Scholar]
- 16. Sen CK, Roy S. Redox signals in wound healing. Biochim Biophys Acta. 2008;1780:1348–1361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chang YH, Chen PL, Tai MC, Chen CH, Lu DW, Chen JT. Hyperbaric oxygen therapy ameliorates the blood-retinal barrier breakdown in diabetic retinopathy. Clin Exp Ophthalmol. 2006;34:584–589 [DOI] [PubMed] [Google Scholar]
- 18. Nguyen QD, Shah SM, Van Anden E, Sung JU, Vitale S, Campochiaro PA. Supplemental oxygen improves diabetic macular edema: a pilot study. Invest Ophthalmol Vis Sci. 2004;45:617–624 [DOI] [PubMed] [Google Scholar]
- 19. Roy M, Bartow W, Ambrus J, Fauci A, Collier B, Titus J. Retinal leakage in retinal vein occlusion: reduction after hyperbaric oxygen. Ophthalmologica. 1989;198:78–83 [DOI] [PubMed] [Google Scholar]
- 20. Wright JK, Franklin B, Zant E. Clinical case report: treatment of a central retinal vein occlusion with hyperbaric oxygen. Undersea Hyperb Med. 2007;34:315–319 [PubMed] [Google Scholar]
- 21. Chan-Ling T, Gock B, Stone J. Supplemental oxygen therapy: basis for noninvasive treatment of retinopathy of prematurity. Invest Ophthalmol Vis Sci. 1995;36:1215–1230 [PubMed] [Google Scholar]
- 22. Chan-Ling T, Stone J. Degeneration of astrocytes in feline retinopathy of prematurity causes failure of the blood-retinal barrier. Invest Ophthalmol Vis Sci. 1992;33:2148–2159 [PubMed] [Google Scholar]
- 23. Gu X, Samuel S, El-Shabrawey M, et al. Effects of sustained hyperoxia on revascularization in experimental retinopathy of prematurity. Invest Ophthalmol Vis Sci. 2002;43:496–502 [PubMed] [Google Scholar]
- 24. Oguz H, Sobaci G. The use of hyperbaric oxygen therapy in ophthalmology. Surv Ophthalmol. 2008;53:112–120 [DOI] [PubMed] [Google Scholar]
- 25. Smith LE, Wesolowski E, McLellan A, et al. Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci. 1994;35:101–111 [PubMed] [Google Scholar]
- 26. Stahl A, Connor KM, Sapieha P, et al. Computer-aided quantification of retinal neovascularization. Angiogenesis. 2009;12:297–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang W, Rojas M, Lilly B, et al. NAD(P)H oxidase-dependent regulation of CCL2 production during retinal inflammation. Invest Ophthalmol Vis Sci. 2009;50:3033–3040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ishikawa K, Yoshida S, Kadota K, et al. Gene expression profile of hyperoxic and hypoxic retinas in a mouse model of oxygen-induced retinopathy. Invest Ophthalmol Vis Sci. 51:4307–4319 [DOI] [PubMed] [Google Scholar]
- 29. Skoura A, Sanchez T, Claffey K, Mandala SM, Proia RL, Hla T. Essential role of sphingosine 1-phosphate receptor 2 in pathological angiogenesis of the mouse retina. J Clin Invest. 2007;117:2506–2516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ritter MR, Banin E, Moreno SK, Aguilar E, Dorrell MI, Friedlander M. Myeloid progenitors differentiate into microglia and promote vascular repair in a model of ischemic retinopathy. J Clin Invest. 2006;116:3266–3276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Connor KM, SanGiovanni JP, Lofqvist C, et al. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat Med. 2007;13:868–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kubota Y, Hirashima M, Kishi K, Stewart CL, Suda T. Leukemia inhibitory factor regulates microvessel density by modulating oxygen-dependent VEGF expression in mice. J Clin Invest. 2008;118:2393–2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen J, Connor KM, Aderman CM, Smith LE. Erythropoietin deficiency decreases vascular stability in mice. J Clin Invest. 2008;118:526–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gardiner TA, Gibson DS, de Gooyer TE, de la Cruz VF, McDonald DM, Stitt AW. Inhibition of tumor necrosis factor-alpha improves physiological angiogenesis and reduces pathological neovascularization in ischemic retinopathy. Am J Pathol. 2005;166:637–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sennlaub F, Courtois Y, Goureau O. Inducible nitric oxide synthase mediates the change from retinal to vitreal neovascularization in ischemic retinopathy. J Clin Invest. 2001;107:717–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zamora DO, Davies MH, Planck SR, Rosenbaum JT, Powers MR. Soluble forms of EphrinB2 and EphB4 reduce retinal neovascularization in a model of proliferative retinopathy. Invest Ophthalmol Vis Sci. 2005;46:2175–2182 [DOI] [PubMed] [Google Scholar]
- 37. Fruttiger M, Calver AR, Kruger WH, et al. PDGF mediates a neuron-astrocyte interaction in the developing retina. Neuron. 1996;17:1117–1131 [DOI] [PubMed] [Google Scholar]
- 38. Dorrell MI, Aguilar E, Friedlander M. Retinal vascular development is mediated by endothelial filopodia, a preexisting astrocytic template and specific R-cadherin adhesion. Invest Ophthalmol Vis Sci. 2002;43:3500–3510 [PubMed] [Google Scholar]
- 39. Kramerov AA, Saghizadeh M, Pan H, et al. Expression of protein kinase CK2 in astroglial cells of normal and neovascularized retina. Am J Pathol. 2006;168:1722–1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ljubimov AV, Caballero S, Aoki AM, Pinna LA, Grant MB, Castellon R. Involvement of protein kinase CK2 in angiogenesis and retinal neovascularization. Invest Ophthalmol Vis Sci. 2004;45:4583–4591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bai Y, Ma JX, Guo J, et al. Müller cell-derived VEGF is a significant contributor to retinal neovascularization. J Pathol. 2009;219:446–454 [DOI] [PubMed] [Google Scholar]
- 42. Pierce EA, Avery RL, Foley ED, Aiello LP, Smith LE. Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc Natl Acad Sci U S A. 1995;92:905–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kirsch M, Trautmann N, Ernst M, Hofmann HD. Involvement of gp130-associated cytokine signaling in Müller cell activation following optic nerve lesion. Glia. 58:768–779 [DOI] [PubMed] [Google Scholar]
- 44. Supplemental Therapeutic Oxygen for Prethreshold Retinopathy Of Prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics. 2000;105:295–310 [DOI] [PubMed] [Google Scholar]
- 45. McGregor ML, Bremer DL, Cole C, et al. Retinopathy of prematurity outcome in infants with prethreshold retinopathy of prematurity and oxygen saturation >94% in room air: the high oxygen percentage in retinopathy of prematurity study. Pediatrics. 2002;110:540–544 [DOI] [PubMed] [Google Scholar]
- 46. Lloyd J, Askie L, Smith J, Tarnow-Mordi W. Supplemental oxygen for the treatment of prethreshold retinopathy of prematurity. Cochrane Database Syst Rev. 2003;CD003482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alon T, Hemo I, Itin A, Pe'er J, Stone J, Keshet E. Vascular endothelial growth factor acts as a survival factor for newly formed retinal vessels and has implications for retinopathy of prematurity. Nat Med. 1995;1:1024–1028 [DOI] [PubMed] [Google Scholar]
- 48. Yamada H, Yamada E, Ando A, et al. Platelet-derived growth factor-A-induced retinal gliosis protects against ischemic retinopathy. Am J Pathol. 2000;156:477–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lofqvist C, Chen J, Connor KM, et al. IGFBP3 suppresses retinopathy through suppression of oxygen-induced vessel loss and promotion of vascular regrowth. Proc Natl Acad Sci U S A. 2007;104:10589–10594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kielczewski JL, Jarajapu YP, McFarland EL, et al. Insulin-like growth factor binding protein-3 mediates vascular repair by enhancing nitric oxide generation. Circ Res. 2009;105:897–905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gerhardt H, Golding M, Fruttiger M, et al. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J Cell Biol. 2003;161:1163–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gerhardt H. VEGF and endothelial guidance in angiogenic sprouting. Organogenesis. 2008;4:241–246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dorrell MI, Aguilar E, Jacobson R, et al. Maintaining retinal astrocytes normalizes revascularization and prevents vascular pathology associated with oxygen-induced retinopathy. Glia. 58:43–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Stone J, Chan-Ling T, Pe'er J, Itin A, Gnessin H, Keshet E. Roles of vascular endothelial growth factor and astrocyte degeneration in the genesis of retinopathy of prematurity. Invest Ophthalmol Vis Sci. 1996;37:290–299 [PubMed] [Google Scholar]
- 55. Zhang Y, Stone J. Role of astrocytes in the control of developing retinal vessels. Invest Ophthalmol Vis Sci. 1997;38:1653–1666 [PubMed] [Google Scholar]
- 56. Banin E, Dorrell MI, Aguilar E, et al. T2-TrpRS inhibits preretinal neovascularization and enhances physiological vascular regrowth in OIR as assessed by a new method of quantification. Invest Ophthalmol Vis Sci. 2006;47:2125–2134 [DOI] [PubMed] [Google Scholar]
- 57. Downie LE, Pianta MJ, Vingrys AJ, Wilkinson-Berka JL, Fletcher EL. AT1 receptor inhibition prevents astrocyte degeneration and restores vascular growth in oxygen-induced retinopathy. Glia. 2008;56:1076–1090 [DOI] [PubMed] [Google Scholar]
- 58. Murata T, Hata Y, Ishibashi T, et al. Response of experimental retinal neovascularization to thiazolidinediones. Arch Ophthalmol. 2001;119:709–717 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.