The authors describe the screening of 55 families of European, Tunisian, and Arab descent for mutations in 15 BBS and 5 additional ciliopathy genes. The spectrum of mutations is described with a discussion of possible third-allele effects.
Abstract
Purpose.
Bardet-Biedl syndrome (BBS) is genetically heterogeneous with 15 BBS genes currently identified, accounting for approximately 70% of cases. The aim of our study was to define further the spectrum of BBS mutations in a cohort of 44 European-derived American, 8 Tunisian, 1 Arabic, and 2 Pakistani families (55 families in total) with BBS.
Methods.
A total of 142 exons of the first 12 BBS-causing genes were screened by dideoxy sequencing. Cases in which no mutations were found were then screened for BBS13, BBS14, BBS15, RPGRIP1L, CC2D2A, NPHP3, TMEM67, and INPP5E.
Results.
Forty-three mutations, including 8 frameshift mutations, 10 nonsense mutations, 4 splice site mutations, 1 deletion, and 20 potentially or probably pathogenic missense variations, were identified in 46 of the 55 families studied (84%). Of these, 21 (2 frameshift mutations, 4 nonsense mutations, 4 splice site mutations, 1 deletion, and 10 missense variations) were novel. The molecular genetic findings raised the possibility of triallelic inheritance in 7 Caucasian families, 1 Arabian family, and 1 Tunisian patient. No mutations were detected for BBS4, BBS11, BBS13, BBS14, BBS15, RPGRIP1L, CC2D2A, NPHP3, TMEM67, or INPP5E.
Conclusions.
This mutational analysis extends the spectrum of known BBS mutations. Identification of 21 novel mutations highlights the genetic heterogeneity of this disorder. Differences in European and Tunisian patients, including the high frequency of the M390R mutation in Europeans, emphasize the population specificity of BBS mutations with potential diagnostic implications. The existence of some BBS cases without mutations in any currently identified BBS genes suggests further genetic heterogeneity.
Bardet-Biedl syndrome (BBS; MIM 209900) is a genetically heterogeneous autosomal recessive disorder characterized by progressive retinal degeneration, truncal obesity, cognitive impairment, polydactyly, hypogonadism, and renal anomalies.1–6 Among the nonconsanguineous populations of Northern Europe and America, the prevalence ranges from 1 in 100,000 in North America7 to 1 in 160,000 in Switzerland.8 BBS incidence increases within populations of high consanguinity or those that are geographically isolated.4,9,10 To date, 15 genes (BBS112, Meckel syndrome 1 [MKS1, BBS13], centrosomal protein 290 kDa/nephronophthisis 6 [CEP290/NPHP6, BBS14], and C2ORF86 [BBS15]) have been implicated in BBS.11,12 Mutations in these genes account only for approximately 70% of BBS patients, suggesting that there are additional genes to be found for BBS.13BBS1 and BBS10 are major pathogenic genes in European populations, each accounting for at least 20% of cases in most series.14,15 However, most other genes are rare contributors. For example, there is only a single documented family with mutations in each of BBS11 (TRIM32), BBS13 (MKS1), BBS14 (CEP290), and BBS15 (C2ORF86).12,16,17 A number of recent publications have expanded the spectrum of known BBS mutations,18–21 and suggested that mutations in some genes, including BBS13 and TMEM67/MKS3, can modify the expression of BBS phenotypes in patients who have mutations in other genes.
BBS is also characterized by profound interfamilial and intrafamilial clinical variability, which is possibly explained in part by the presence of second-site modifiers. In some families, three mutated alleles in two BBS genes have been implicated (triallelic inheritance). BBS1, BBS2, BBS3, BBS4, BBS5, BBS6, BBS7, BBS8, and BBS10 have been implicated in triallelic inheritance of BBS,22–25 but the specific contribution of each allele is difficult to ascertain. Moreover, it has been suggested that there might be a connection between triallelism and the phenotypic severity of the disease.26 However, some studies have not identified a complex inheritance mode in this syndrome.27,28
In this study, we analyzed 55 families for known BBS genes (BBS1-BBS15) and identified 43 mutations in 46 families, 21 of which are novel. We also identified 7 Caucasian, 1 Arabic, and 1 Tunisian family in whom the molecular genetic findings raised the possibility of triallelic inheritance involving BBS1, BBS2, BBS3, BBS6, BBS7, BBS8, BBS9, BBS10, or BBS12. Although some sequence variations were identified in additional genes, no homozygous potential mutations were identified in previously unidentified BBS genes.
Materials and Methods
Appropriate informed consent was obtained from all participants in the study, in accord with the tenets of the Declaration of Helsinki. This study was approved by the Massachusetts Eye and Ear Infirmary and Harvard Medical School Institutional Review Boards, the ethics review board of Charles Nicolle Hospital, Tunis, and the CNS Institutional Review Board at the National Institutes of Health.
Study Subjects
We studied 70 persons with Bardet-Biedl syndrome (BBS) from 55 unrelated families including 8 recruited in Tunisia, 2 recruited in Pakistan, and 44 of European and 1 of Arabian descent recruited in the United States. In this study, the 8 BBS families recruited from Tunisia did not overlap with participants from a previous study.28 Among the 55 families, 44 were sporadic cases and the remaining had at least 2 affected members. BBS was diagnosed on the basis of the established criterion that 4 primary features or 3 primary plus 2 secondary features are necessary to make the diagnosis.29 The control group consisted of 96 persons of European origin, 96 persons of Tunisian origin, and 96 persons of Pakistani origin.
Mutation Screening
We carried out a mutation screen of the first 12 identified BBS (BBS1-BBS12) genes in 55 families (for a total of 70 patients) collected from the United States, Tunisia, and Pakistan. For BBS1 to BBS12, all genes were screened in all cases. Cases in which no mutations were found in BBS1 to BBS12 were then screened for mutations in BBS13 (MKS1), BBS14 (CEP290, NPHP6), and BBS15 (C2ORF86) as well as in RPGRIP1L, CC2D2A, NPHP3, TMEM67, and INPP5E because they have been implicated in other ciliopathies. Genomic DNA was isolated from blood leukocytes using standard protocols.30 Coding regions and exon-intron boundaries of the 20 genes were amplified by PCR using standard methods. Amplifications were carried out as previously described,28 and the PCR products were analyzed on 2% agarose gels and purified by vacuum filtration manifold plate (Millipore, Billerica, MA). The PCR primers for each exon were used for bidirectional sequencing using a reaction mix (BigDye Terminator Ready; Applied Biosystems, Foster City, CA) according to the manufacturer's instructions. Sequencing was performed on a gene analyzer (ABI PRISM 3130xl Genetic Analyzer; Applied Biosystems), and sequence traces were analyzed (MutationSurveyor [Soft Genetics Inc., State College, PA] and the SeqMan program of DNASTAR Software [DNASTAR Inc., Madison, WI]).
Criteria to Determine the Pathogenicity of New BBS Mutations
A mutation was considered novel if it was not present in the Human Mutation Database (http://www.hgmd.cf.ac.uk/ac) or the National Center for Biotechnology Information dbSNP database (http://www.ncbi.nlm.nih.gov/projects/SNP/index.html) and not published. A sequence variation was considered pathogenic when it segregated with the disease in the family and, when parental origin could be determined, double heterozygous mutations acted in trans; it was not present in 96 randomly selected controls from the ethnically matched population; it altered a well-conserved amino acid, preferably in a conserved region (http://www.ebi.ac.uk/Tools/clustalw2/index.html); and it was judged significant in a computational test for novel mutations. The neural network splice site scoring program (http://www.fruitfly.org/seq_tools/splice.html) was used to evaluate the effect of mutations affecting splice sites. Splice site scores were calculated with Splice site Score Calculation software (http://rulai.cshl.edu/new_alt_exon_db2/HTML/score.html). PolyPhen analysis (http://genetics.bwh.harvard.edu/pph/) was used to predict whether missense variations could impact the protein structure and function. The prediction is based on the position-specific independent counts score derived from a combination of available structural information and multiple sequence alignments of observations. PolyPhen scores >2.0 indicate the variant is probably damaging to protein function; scores from 1.5 to 2.0 indicate the variant is possibly damaging; and scores <1.5 indicate the variant is Likely benign. In the present study, both “probably damaging” and “possibly damaging” changes were classified as suspected pathogenic mutations.
Results
General Overview of BBS Mutations
Mutations were detected in 46 (of 55; 84%) families, and no mutations were detected for the remaining 9 (of 55; 16%) families. We identified 43 different mutations in the 46 families, including 39 families from the United States, including 1 of Saudi Arabian derivation, 5 from Tunisia, and 2 from Pakistan. Of the 43 different mutations, 21 were novel (Fig. 1, Table 113–15,24–26,28,31–34), confirming the genetic heterogeneity of BBS. Seven Caucasian, 1 Arabian, and 1 Tunisian family (20% of families with mutations detected) carry 3 mutations in 2 different genes, raising the possibility of triallelic inheritance (Table 1). Thirty-seven families (83% of patients with mutations detected) carry only 2 mutations in the same gene (Table 1): 15 for BBS1 (13 homozygotes and 2 compound heterozygotes), 4 for BBS2 (3 homozygotes and 1 compound heterozygote), 2 homozygotes for BBS3, 2 homozygotes for BBS5, 3 homozygotes for BBS7, 11 for BBS10 (5 homozygotes and 6 compound heterozygotes), and 1 compound heterozygote for BBS12 (C4ORF24). None of the novel mutations or third-allele mutations was observed in 192 ethnically matched control chromosomes, and none is recorded in the dbSNP database.
Figure 1.
The 21 novel BBS mutations identified in this study. Three novel mutations were identified in BBS1: a heterozygous c.518+1G>A allele, a homozygous c.1473+4A>G allele, and a heterozygous R512H allele. Two novel mutations were identified in BBS2: a heterozygous R275X allele and a heterozygous c.1659+3A>G allele. A novel homozygous deletion was identified in BBS3: c.123+1118del53985. Two novel mutations were identified in BBS5: a homozygous L50R allele and a homozygous c.619-1G>C allele. One novel mutation was identified in BBS6: a heterozygous R309H allele. Three novel mutations were identified in BBS8: a heterozygous K95R allele, a heterozygous M135I allele, and a heterozygous F337L allele. One novel mutation was identified in BBS9: a heterozygous Q132H allele. Six novel mutations were identified in BBS10: a homozygous L533fsX22 allele, a homozygous A323V allele, a heterozygous L445I allele, a homozygous E499X allele, a heterozygousT516RfsX7 allele, and a heterozygous V602L allele. Two novel mutations were identified in BBS12: a heterozygous W520X allele and a heterozygous R675X allele. Sequence tracings of novel mutations identified in this study compared to normal sequences from controls.
Table 1.
Mutations Identified in this Series of 46 Families (43 Mutations Found)
| Family | Ethnic Origin | Gene | Exon | Nucleotide Change | Predicted Amino Acid Change | State | Report/Date |
|---|---|---|---|---|---|---|---|
| K550 | Caucasian | BBS1 | 16 | c.1645G>T | p.E549X | Homozygous | Ref. 14/2002 |
| BBS2 | 13 | c.1659+3A>G† | splice mutation | Heterozygous | This study | ||
| 057015 | Tunisian* | BBS1 | 14 | c.1473+4A>G† | splice mutation | Homozygous | This study |
| BBS8 | 11 | c.1011C>G† | p.F337L | Heterozygous | This study | ||
| J118 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Heterozygous | Ref. 27/2003 |
| BBS1 | 16 | c.1645G>T | p.E549X | Heterozygous | Ref. 14/2002 | ||
| BBS9 | 5 | c.396G>C† | p.Q132H | Heterozygous | This study | ||
| 5360 | Caucasian | BBS10 | 2 | c.1598_1601delTAAC† | p.L533fsX22 | Homozygous | This study |
| BBS12 | 1 | c.355G>A | p.G119S | Heterozygous | Ref. 34/2010 | ||
| D257 | Caucasian | BBS10 | 2 | c.1090del A | p.N364TfsX5 | Homozygous | Ref. 40/2007 |
| BBS6 | 3 | c.926G>A† | p.R309H | Heterozygous | This study | ||
| E729 | Caucasian | BBS2 | 2 | c.311A>C | p.D104A | Heterozygous | Ref. 25/2001 |
| BBS2 | 15 | c.1895G>C | p.R632P | Heterozygous | Ref. 26/2009 | ||
| BBS10 | 2 | c.1333C>A† | p.L445I | Heterozygous | This study | ||
| E059 | Arabic | BBS3 | 3 | c.92C>T | p.T31M | Homozygous | Ref. 41/2004 |
| BBS8 | 5 | c.405G>A† | p.M135I | Heterozygous | This study | ||
| 9409 | Caucasian | BBS7 | 7 | c.632C>T | p.T211I | Homozygous | Ref. 42/2003 |
| BBS8 | 5 | c.284A>G† | p.K95R | Heterozygous | This study | ||
| E521 | Caucasian | BBS12 | 1 | c.2023C>T† | p.R675X | Heterozygous | This study |
| BBS12 | 1 | c.476C>T | p.P159L | Heterozygous | Ref. 13/2007 | ||
| BBS1 | 15 | c.1535G>A† | p.R512H | Heterozygous | This study | ||
| 7367 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 7833 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 0775 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 7881 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 6579 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 1502 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 9390 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 5943 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 9437 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 2532 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 3163 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| F248 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| 057016 | Tunisian* | BBS1 | 12 | c.1169T>G | p.M390R | Homozygous | Ref. 14/2002 |
| D597 | Caucasian | BBS1 | 6 | c.518+1G>A† | splice mutation | Heterozygous | This study |
| BBS1 | 12 | c.1169T>G | p.M390R | Heterozygous | Ref. 27/2003 | ||
| 7348 | Caucasian | BBS1 | 12 | c.1169T>G | p.M390R | Heterozygous | Ref. 27/2003 |
| BBS1 | 16 | c.1645G>T | p.E549X | Heterozygous | Ref. 14/2002 | ||
| 1087 | Caucasian | BBS10 | 2 | c.272 insertion T | p.C91LfsX5 | Homozygous | Ref. 15/2006 |
| E084 | Caucasian | BBS10 | 2 | c.272 insertion T | p.C91LfsX5 | Homozygous | Ref. 15/2006 |
| Q119 | Caucasian | BBS10 | 2 | c.272 insertion T | p.P.C91LfsX5 | Homozygous | Ref. 15/2006 |
| 9407 | Caucasian | BBS10 | 2 | c.1495G>T† | p.E499X | Homozygous | This study |
| F931 | Caucasian | BBS10 | 2 | c.968C>T† | p.A323V | Homozygous | This study |
| 5111 | Caucasian | BBS10 | 2 | c.272 insertion T | p.C91LfsX5 | Heterozygous | Ref. 15/2006 |
| BBS10 | 2 | c.907_910delAGTC | p.S303RfsX3 | Heterozygous | Ref. 15/2006 | ||
| 9438 | Caucasian | BBS10 | 2 | c.272 insertion T | p.C91LfsX5 | Heterozygous | Ref. 15/2006 |
| BBS10 | 2 | c.907_910delAGTC | p.S303RfsX3 | Heterozygous | Ref. 15/2006 | ||
| F699 | Caucasian | BBS10 | 2 | c.272 insertion T | p.C91LfsX5 | Heterozygous | Ref. 15/2006 |
| BBS10 | 2 | c.1677C>A | p.Y559X | Heterozygous | Ref. 34/2010 | ||
| 2834 | Caucasian | BBS10 | 2 | c.687delT† | p.P229fsX8 | Heterozygous | Ref. 15/2006 |
| BBS10 | 2 | c.907_910delAGTC | p.S303RfsX3 | Heterozygous | Ref. 15/2006 | ||
| E352 | Caucasian | BBS10 | 1 | c.145C>T | p.R49W | Heterozygous | Ref. 15/2006 |
| BBS10 | 2 | c.1804G>C† | p.V602L | Heterozygous | This study | ||
| 9398 | Caucasian | BBS10 | 1 | c.164T>C | p.L55P | Heterozygous | Ref. 34/2010 |
| BBS10 | 2 | c.1543_1546dupGATA† | p.T516RfsX7 | Heterozygous | This study | ||
| E325 | Caucasian | BBS2 | 2 | c.311A>C | p.D104A | Heterozygous | Ref. 25/2001 |
| BBS2 | 8 | c.823C>T† | p.R275X | Heterozygous | This study | ||
| 057012 | Tunisian* | BBS2 | 5 | c.565C>T | p.R189X | Homozygous | Ref. 28/2006 |
| M-679 | Caucasian | BBS2 | 8 | c.823C>T | p.R275X | Homozygous | Ref. 25/2001 |
| PK01 | Pakistani* | BBS2 | 11 | c.1658C>T | p.R413X | Homozygous | Ref. 24/2003 |
| M-002 | Caucasian | BBS5 | 8 | c.619–1G>C† | splice mutation | Homozygous | This study |
| 057010 | Tunisian* | BBS5 | 3 | c.149T>G† | p.L50R | Homozygous | This study |
| J585 | Caucasian | BBS7 | 7 | c.710_713delAGAG | p.K237fsX60 | Homozygous | Ref. 42/2003 |
| B-489 | Caucasian | BBS7 | 7 | c.632C>T | p.T211I | Homozygous | Ref. 42/2003 |
| J183 | Caucasian | BBS7 | 7 | c.632C>T | p.T211I | Homozygous | Ref. 42/2003 |
| 057013 | Tunisian* | BBS12 | 1 | 1560G>A† | p.W520X | Heterozygous | This study |
| BBS12 | 1 | c.355G>A | p.G119S | Heterozygous | Ref. 34/2010 | ||
| 061049 | Pakistani* | BBS3 | 3 | c.123+1118del53985† | Homozygous | This study |
DNA samples from the Tunisian and Pakistani families were obtained through the National Eye Institute; all others were obtained through the Berman-Gund Laboratory, Harvard Medical School, Massachusetts Eye and Ear Infirmary.
Novel mutations.
BBS1 Mutations
BBS1 mutations were present in 19 of the 46 families with identified mutations and represented the primary pathogenic locus in 18 families (33%) and a possible third mutant allele in 1 family (Fig. 1, Table 1). In 15 families (13 homozygotes and 2 compound heterozygotes), only 2 mutations were identified in the BBS1 gene (Table 1). Eighteen affected members of 12 Caucasian families and 1 Tunisian family were homozygous for the M390R allele, predicted to be pathogenic with a PolyPhen score of 2.7. The proband of family D597 is a compound heterozygote for M390R and c.518+1G>A, which was not found in controls and showed calculated splice site scores of 11.0 for the normal splice site and 0.2 for the variant site, suggesting that it affects splicing. The proband of family 7348 was a compound heterozygote for the M390R and E549X alleles. All affected members carrying the M390R mutation shared a common SNP haplotype across the BBS1 gene (Supplementary Table S1, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7554/-/DCSupplemental).
Possible triallelic inheritance with involvement of mutations at two distinct loci was seen in 3 European-American families (K550, J118, and E521) and 1 Tunisian family (057015) (Table 1), including the proband of family 057015, who was heterozygous for the F337L allele in BBS8 and homozygous for the c.1473+4A>G BBS1 allele, which showed a reduction from 7.3 for the natural splice site to 4.3 for the variant site, indicating that this alteration might affect splicing.
BBS2 Mutations
BBS2 mutations were identified in 6 of the 46 families; they were the primary pathogenic mutations in 5 families (9%) and a potential triallelic contributor in 1 family. Two were novel (Fig. 1, Table 1). The proband of family E325 was a compound heterozygote for R275X and D104A and had a score of 2.44 when analyzed with PolyPhen, suggesting pathogenicity.
Possible triallelic inheritance with involvement of mutations at two distinct loci was suspected in two European-derived families (E729 and K550) (Table 1). The proband of family E729 was a compound heterozygote for the D104A and R632P (PolyPhen scores of 2.44 and 2.7, respectively) alleles and also carried a heterozygous L445I allele in BBS10. The proband of family K550 was heterozygous for the c.1659+3A>G BBS2 allele (decreasing the splice site score from 0.52 to 0, consistent with loss of the donor site) and also carried a homozygous E549X allele in BBS1, the principal “pathogenic” mutation.
BBS3 Mutations
BBS3 mutations were found in 2 of the 46 families (4%), including a consanguineous Pakistani family (061049) in which affected members were homozygous for a novel 54-kb deletion beginning in intron 3, c.123+1118del 53,985, and extending beyond the end of the gene. In an Arabian family (E059), affected members were homozygous for a previously reported T31M allele in BBS3, predicted to be pathogenic (PolyPhen score 2.78). One member of this family also had a heterozygous M135I allele in BBS8 predicted to be benign with a PolyPhen score of 1.09.
BBS5 Mutations
Novel BBS5 mutations were found in 2 of the 46 families (4%), including a homozygous c.619–1G>C allele in European family M-002, decreasing the splice site score from 5.6 to −5.4 (Fig. 1, Table 1). Tunisian family 057010 showed a homozygous L50R (probably pathogenic) sequence change with a PolyPhen score of 2.17. Both mutations reported here affected the highly conserved DM16 domains,35 supporting their pathogenicity.
BBS6 Mutations
A novel heterozygous sequence change was present in a single family of European origin (D257), which showed the R309H BBS6 allele and carried a homozygous N364TfsX5 allele in BBS10 as well (Table 1), suggesting the possibility of triallelic inheritance. However, the R309H residue was not highly conserved during evolution (Fig. 2), and PolyPhen analysis predicts R309H to be benign (Table 2), indicating that its pathogenic potential is low.
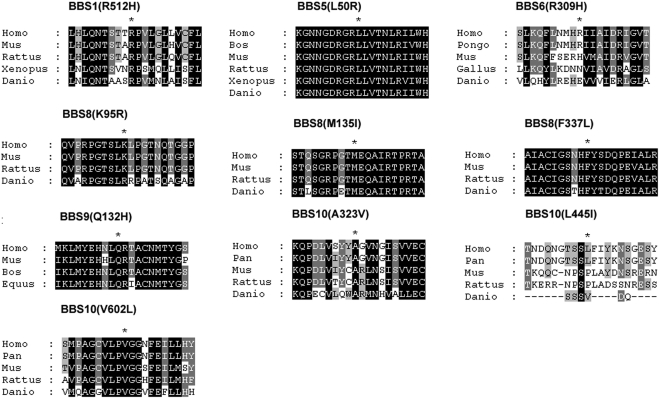
Figure 2.
Amino acid sequence conservation around residues affected by novel missense mutations in BBS1, BBS5, BBS6, BBS8, BBS9, and BBS10 identified in this study. Asterisk: position of the missense mutation. The sequences of BBS proteins or predicted translation products from several species have been compared and aligned. The relevant amino acids are in bold, and they are underlined when different from Homo sapiens reference; other identities are represented by a gray background. Homo, H. sapiens; Mus, Mus musculus; Rattus, Rattus norvegicus; Xenopus, Xenopus (silurana) tropicalis; Danio, Danio rerio; Bos, Bos taurus; Pongo, Pongo abelii; Gallus, gallus; Pan, Pan troglodytes; Equus, Equus caballus.
Table 2.
Evaluation of Novel BBS Missense Variants
| Gene-Exon | Predicted Amino Acid Change | Nucleotide Change | State | Third Mutated Allele | Con-served | Computational Prediction |
Present in Controls | Report | |
|---|---|---|---|---|---|---|---|---|---|
| PolyPhen Prediction | Remark | ||||||||
| BBS1-EX15 | R512H | c.1535G>A | Heter | No | Yes | Possibly damaging | Pathogenic | No | This study |
| BBS10-EX2 | A323V | c.968C>T | Homo | No | Yes | Likely benign | Neutral | No | This study |
| BBS10-EX2 | L445I | c.1333C>A | Heter | Yes | No | Likely benign | Neutral | No | This study |
| BBS10-EX2 | V602L | c.1804G>C | Heter | No | Yes | Likely benign | Neutral | No | This study |
| BBS5-EX3 | L50R | c.149T>G | Homo | No | Yes | Probably damaging | Pathogenic | No | This study |
| BBS6-EX3 | R309H | c.926G>A | Heter | Yes | No | Likely benign | Neutral | No | This study |
| BBS8_EX5 | K95R | c.284A>G | Heter | Yes | No | Likely benign | Neutral | No | This study |
| BBS8_EX5 | M135I | c.405G>A | Heter | Yes | Yes | Likely benign | Neutral | No | This study |
| BBS8-EX11 | F337L | c.1011C>G | Heter | Yes | Yes | Probably damaging | Pathogenic | No | This study |
| BBS9-EX5 | Q132H | c.396G>C | Heter | Yes | Yes | Possibly damaging | Pathogenic | No | This study |
Heter, heterozygous; Homo, homozygous.
BBS7 Mutations
Previously described BBS7 mutations were present in 4 of the 46 families (7%), all of European origin. Possible triallelic inheritance is suspected in 1 family (9409; Table 1), in which 2 affected family members are homozygous for theT211I BBS7allele and heterozygous for the K95R sequence change in BBS8. However, the K95R residue was not highly conserved during evolution (Fig. 2), and PolyPhen analysis predicts K95R to be benign with a score of 0.15 (Table 2).
BBS8 Mutations
Novel heterozygous BBS8 sequence changes were identified in 3 of the 46 families (6%; M135I in E059, K95R in Arabian family 9409, and F337L in Tunisian family 057015), all of which may be compatible with triallelic inheritance. The M135I residue is highly conserved during evolution, but PolyPhen predicts M135I to be benign with a score of 1.09 (Fig. 2, Table 2). In contrast, the F337L residue is highly conserved during evolution (Fig. 2), and PolyPhen analysis indicates that F337L is expected to be pathogenic with a score of 2.43 (Table 2).
BBS9 Mutations
A novel heterozygous BBS9 sequence change was present in 1 European-derived family (J118), possibly consistent with triallelic inheritance. The Q132H residue is highly conserved during evolution (Fig. 2), and PolyPhen analysis predicts that Q132H would be expected to be pathogenic with a score of 1.92 (Table 2).
BBS10 Mutations
BBS10 mutations were present in 14 of the 46 families, all European derived, with 2 pathogenic alleles present in 11 (20%), 2 changes of uncertain significance in 2 more (4%), and a single heterozygous change in 1 family. Six are novel (Fig. 1, Table 1). The proband of family F931was homozygous for the A323V allele, which is highly conserved during evolution, but it is a conservative change that PolyPhen analysis predicts to be benign, (Fig. 2, Table 2). Similarly, the proband of family E352 was a compound heterozygote for the R49W (previously reported15 with a probably damaging PolyPhen score of 2.46) and V602L alleles. Although the V602L residue is highly conserved during evolution, PolyPhen analysis predicts V602L to be benign. The proband of family 9398 was a compound heterozygote for the T516RfsX7 and L55P alleles. The L55P residue is highly conserved during evolution (Fig. 2), with a probably damaging PolyPhen score of 2.07 (Table 2).
Possible triallelic inheritance was found in probands of 3 families: 5360, which, in addition to homozygous L533fsX22, carries a heterozygous G119S allele in BBS12; D257 is homozygous for the N364TfsX5BBS10 allele with a heterozygous R309H allele in BBS6; and E729; Table 1). The proband of family E729 was heterozygous for the L445I BBS10 allele and also was a compound heterozygote for the D104A and R632P alleles in BBS2, the principal pathogenic mutations. The L445I residue is not highly conserved during evolution (Fig. 2), and PolyPhen predicts L445I to be benign (Table 2), suggesting low pathogenic potential.
BBS12 (C4ORF24) Mutations
BBS12 mutations (4 different alleles) were present in three families, including 2 families of European and 1 of Tunisian origin (Table 1). Possible triallelic inheritance was found in probands of 2 European-derived families. E521 carries a compound heterozygote for the previously reported13P159L and R675X alleles and a heterozygous R512H allele in BBS1. The proband of family 5360 is homozygous L533fsX22 allele in BBS10 and heterozygous for theBBS12 G119S allele, which is highly conserved during evolution (Fig. 2) and gives a probably damaging PolyPhen score (Table 2).
BBS4, BBS11 (TRIM32), BBS13, BBS14, BBS15 (C2ORF86), RPGRIP1L, CC2D2A, NPHP3, TMEM67, and INPP5E Mutations
No mutations were detected for BBS4, BBS11 (TRIM32), BBS13, BBS14, BBS15 (C2ORF86), RPGRIP1L, CC2D2A, NPHP3, TMEM67, or INPP5E in any of the 55 families studied.
Discussion
In agreement with previous studies in which mutations were identified in 70% to 75% of BBS families,19–21,36,37 in our study, mutations were identified in 38 of 45 patients of European ethnic origin (84%) and 5 of 8 Tunisian families (62.5%), giving an overall detection rate of 73%.
Our results are consistent with previous reports that BBS1 and BBS10 mutations are frequent, contributing 30% and 21% in previous studies15,22,23 (Supplementary Fig. S1, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7554/-/DCSupplemental). In this series BBS1 mutations contributed to disease in35% (19/55) of the patients, representing the primary pathogenic locus in 18 families (33%). Overall, these data support the previous observation that BBS1 and BBS10 are responsible for most of the disease in Europeans. In contrast, BBS2 and BBS8 are prime candidates in Tunisian-derived patients, in whom no BBS10 mutations were identified.
Examination of the distribution of BBS mutations in European and Tunisian individuals shows a number of differences (Supplementary Fig. S2, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7554/-/DCSupplemental). In agreement with previous reports, in which p.M390R has been reported to cause 18% to 32% of BBS cases,22,27 16 of 55 (29%) of families with BBS were found to carry the M390R mutation (13 as homozygous alleles and 3 as heterozygous alleles), making it the most common mutation found. It accounts for 24 of 32 (75%) BBS1 alleles identified in Europeans, in which the M390R mutation is considered to be an ancient mutation, as suggested by haplotype analysis. The M390R mutation has been described exclusively in European-derived patients of French descent.27 Interestingly, although 1 Tunisian patient in this study carries this mutation, he shares a common BBS1 SNP haplotype with the European patients. The geographic position of Tunisia in North Africa has ensured an eventful population history in which Phoenicians, Romans, Vandals, Byzantines, Arabs, Ottomans, and French have controlled or colonized the region at different historical times.28 Taken together with the haplotype data, this suggests that this Tunisian patient might be of French descent, consistent with the absence of the M390R mutation in most non-European populations. BBS2 and BBS8 are the most common genes implicated in Tunisians, and R189X is the only BBS2 mutation seen in Tunisians. Finally, though the Tunisian data set is relatively small, it is notable for the complete absence of BBS10 mutations, the second most common gene affected in Europeans after BBS1.
BBS is inherited primarily as an autosomal recessive trait. However, in some patients, 3 mutations across 2 BBS genes appear to interact to modify the onset or severity, or both, of the phenotype.22–25Seven Caucasian families, 1 Arabian family, and 1 Tunisian family (15% of patients with mutations detected) were found to carry 3 mutations in the 2 different genes, termed triallelic inheritance (Supplementary Fig. S3, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7554/-/DCSupplemental). We found only a single, heterozygous mutation in BBS1 in 3 families, in BBS10 in 2 families, and in BBS2, BBS3, BBS7, and BBS12 in single families (Table 1). Although these data are compatible with a potential epistatic interaction, in which the effects of the primary gene are modified by a specific allele at a second gene, they might also represent the presence of undetected second mutations or the random occurrence of sequence variants in these genes.
Interestingly, 8 of the 9 third variant alleles were novel, except for BBS12 p.G119S, which was reported recently as a third allele variant by Billingsley et al.31 (Table 1, Supplementary Fig. S3, http://www.iovs.org/lookup/suppl/doi:10.1167/iovs.11-7554/-/DCSupplemental), and 2 of them involve genes that, to our knowledge, have not previously been reported to be involved in triallelic inheritance of BBS (BBS9 and BBS12). Given that most of these sequence changes are missense variants, the possibility that some are benign cannot be excluded, even though they were not identified in 96 healthy persons. Of the 8 missense variants, 4 (R512H in BBS1, F337L in BBS8, Q132H in BBS9, and G119S in BBS12) were estimated to be pathogenic changes, whereas the remaining four (R309H in BBS6, K95R in BBS8, M135I in BBS8, and L445I in BBS10) were estimated to be neutral by the PolyPhen program (Table 2). Five, including all those predicted to be pathogenic by PolyPhen analysis, involve residues that are highly conserved during evolution (Fig. 2). Thus, alternative explanations must be considered, including that the third allele detected in each of the families is a benign polymorphism or that the third allele is not causal in these patients but might exert a more subtle modifying effect. These observations are compatible with the previous suggestion that the severity of the disease phenotype and the clinical symptoms may vary as a result of the interaction of mutations in different BBS genes.22,23 However, the absence of these variants in 96 ethnically matched control subjects does not provide sufficient statistical power to demonstrate a causal relationship to BBS; functional analysis will be required to provide a definitive answer to this question.
Recent studies provide insight into how the BBS proteins mediate ciliary function in mammalian cells. Seven evolutionarily conserved BBS proteins (BBS1, 2, 4, 5, 7, 8, and 9) form a stable complex, the BBSome, mediating vesicular transport to the cilium.38 The BBSome is transported to the basal body through interactions between the BBS4 subunit of the BBSome and PCM-1 of the centriolar satellite. Inside the cilium, BBS7 and TTC8 may be involved in vesicular transport pathways, including functioning as an IFT cohesion factor.38 The ability of each BBS locus to contribute alleles that can modify the effect of mutations in other BBS genes suggests a common pathway and potentially the existence of a macromolecular complex under the “poison” hypothesis, stating the presence of mutant subunits in a heterodimer or multisubunit complex prevents proper functioning of the entire assembly.39 Although BBS6, BBS10, and BBS12 are not components of the BBSome, mutations in these genes also lead to similar phenotypes. Seo et al.40 demonstrated that chaperonin-like BBS proteins (BBS6, BBS10, and BBS12) are required for BBSome assembly.
In addition to BBS, a number of related syndromes result from ciliary dysfunction, including BBS14 mutated in nephronophthisis, Joubert syndrome, and BBS and Meckel-Gruber syndrome.17,41,42 Although this provided a rationale for screening families without identified mutations in known BBS genes for mutations in these genes, no mutations were found in our patients.
In summary, we have identified 43 mutations in 55 families affected with BBS, including 21 novel mutations. We found evidence compatible with triallelic inheritance in affected persons from 9 families. This mutational analysis has expanded the already extensive categorization of BBS mutations and contributed to our understanding of both the population genetics of BBS and to the molecular pathology of the genes implicated in these diseases, as well as suggesting distinct optimal sequential mutational analysis in Tunisian and European patients for diagnostic purposes. The identification of many novel mutations unique to individuals highlights the genetic heterogeneity of the disorder, and the existence of some BBS cases without identified mutations in known BBS genes suggests further genetic heterogeneity.
Supplementary Material
Acknowledgments
The authors thank all the patients and their families for their contribution to this work.
Footnotes
Supported in part by a Center Grant from the Foundation Fighting Blindness (ELB).
Disclosure: J. Chen, None; N. Smaoui, None; M.B.H. Hammer, None; X. Jiao, None; S.A. Riazuddin, None; S. Harper, None; N. Katsanis, None; S. Riazuddin, None; H. Chaabouni, None; E.L. Berson, None; J.F. Hejtmancik, None
References
- 1. Laurence JZ, Moon RC. Four cases of “retinitis pigmentosa” occurring in the same family and accompanied by general imperfection of development. Ophthal Rev. 1866;2:32–41 [DOI] [PubMed] [Google Scholar]
- 2. Bardet G. Sur un syndrome d'obesite infantile avec polydactylie et retinite pigmentaire (contribution a l'etude des formes cliniques de l'obesite hypophysaire). 1920 [Google Scholar]
- 3. Biedl A. Ein Geschwisterpaar mit adiposo-genitaler Dystrophie. Dtsch. Med Wschr. 1922;48:1630–1630 [Google Scholar]
- 4. Moore SJ, Green JS, Fan Y, et al. Clinical and genetic epidemiology of Bardet-Biedl syndrome in Newfoundland: a 22-year prospective, population-based, cohort study. Am J Med Genet A. 2005;132:352–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rizzo JF, III, Berson EL, Lessell S. Retinal and neurologic findings in the Laurence-Moon-Bardet-Biedl phenotype. Ophthalmology. 1986;93:1452–1456 [DOI] [PubMed] [Google Scholar]
- 6. Bell J. Anomalies and diseases of the eye. In: Pearson K. (ed), Treasury of Human Inheritance: Dulau and Cow Ltd; 1909 [Google Scholar]
- 7. Croft JB, Swift M. Obesity, hypertension, and renal disease in relatives of Bardet-Biedl syndrome sibs. Am J Med Genet. 1990;36:37–42 [DOI] [PubMed] [Google Scholar]
- 8. Klein D, Ammann F. The syndrome of Laurence-Moon-Bardet-Biedl and allied diseases in Switzerland: clinical, genetic and epidemiological studies. J Neurol Sci. 1969;9:479–513 [DOI] [PubMed] [Google Scholar]
- 9. Farag TI, Teebi AS. Bardet-Biedl and Laurence-Moon syndromes in a mixed Arab population. Clin Genet. 1988;33:78–82 [DOI] [PubMed] [Google Scholar]
- 10. Farag TI, Teebi AS. High incidence of Bardet Biedl syndrome among the Bedouin. Clin Genet. 1989;36:463–464 [DOI] [PubMed] [Google Scholar]
- 11. Zaghloul NA, Katsanis N. Mechanistic insights into Bardet-Biedl syndrome, a model ciliopathy. J Clin Invest. 2009;119:428–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim SK, Shindo A, Park TJ, et al. Planar cell polarity acts through septins to control collective cell movement and ciliogenesis. Science. 2010;329, 1337–1340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stoetzel C, Muller J, Laurier V, et al. Identification of a novel BBS gene (BBS12) highlights the major role of a vertebrate-specific branch of chaperonin-related proteins in Bardet-Biedl syndrome. Am J Hum Genet. 2007;80:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mykytyn K, Nishimura DY, Searby CC, et al. Identification of the gene (BBS1) most commonly involved in Bardet-Biedl syndrome, a complex human obesity syndrome. Nat Genet. 2002;31:435–438 [DOI] [PubMed] [Google Scholar]
- 15. Stoetzel C, Laurier V, Davis EE, et al. BBS10 encodes a vertebrate-specific chaperonin-like protein and is a major BBS locus. Nat Genet. 2006;38:521–524 [DOI] [PubMed] [Google Scholar]
- 16. Chiang AP, Beck JS, Yen HJ, et al. Homozygosity mapping with SNP arrays identifies TRIM32, an E3 ubiquitin ligase, as a Bardet-Biedl syndrome gene (BBS11). Proc Natl Acad Sci U S A. 2006;103:6287–6292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leitch CC, Zaghloul NA, Davis EE, et al. Hypomorphic mutations in syndromic encephalocele genes are associated with Bardet-Biedl syndrome. Nat Genet. 2008;40:443–448 [DOI] [PubMed] [Google Scholar]
- 18. Abu Safieh L, Aldahmesh M, Shamseldin H, et al. Clinical and molecular characterization of Bardet-Biedl syndrome in consanguineous populations: the power of homozygosity mapping. J Med Genet. 2009;47:236–241 [DOI] [PubMed] [Google Scholar]
- 19. Muller J, Stoetzel C, Vincent MC, et al. Identification of 28 novel mutations in the Bardet-Biedl syndrome genes: the burden of private mutations in an extensively heterogeneous disease. Hum Genet. 2010;127:583–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hjortshoj TD, Gronskov K, Philp AR, et al. Bardet-Biedl syndrome in Denmark—report of 13 novel sequence variations in six genes. Hum Mutat. 2010;31:429–436 [DOI] [PubMed] [Google Scholar]
- 21. Harville HM, Held S, az-Font A, et al. Identification of 11 novel mutations in 8 BBS genes by high-resolution homozygosity mapping. J Med Genet. 2009;47:262–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Badano JL, Kim JC, Hoskins BE, et al. Heterozygous mutations in BBS1, BBS2 and BBS6 have a potential epistatic effect on Bardet-Biedl patients with two mutations at a second BBS locus. Hum Mol Genet. 2003;12:1651–1659 [DOI] [PubMed] [Google Scholar]
- 23. Beales PL, Badano JL, Ross AJ, et al. Genetic interaction of BBS1 mutations with alleles at other BBS loci can result in non-Mendelian Bardet-Biedl syndrome. Am J Hum Genet. 2003;72:1187–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fauser S, Munz M, Besch D. Further support for digenic inheritance in Bardet-Biedl syndrome. J Med Genet. 2003;40:e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Katsanis N, Ansley SJ, Badano JL, et al. Triallelic inheritance in Bardet-Biedl syndrome, a Mendelian recessive disorder. Science. 2001;293:2256–2259 [DOI] [PubMed] [Google Scholar]
- 26. Bin J, Madhavan J, Ferrini W, Mok CA, Billingsley G, Heon E. BBS7 and TTC8 (BBS8) mutations play a minor role in the mutational load of Bardet-Biedl syndrome in a multiethnic population. Hum Mutat. 2009;30:E737–E746 [DOI] [PubMed] [Google Scholar]
- 27. Mykytyn K, Nishimura DY, Searby CC, et al. Evaluation of complex inheritance involving the most common Bardet-Biedl syndrome locus (BBS1). Am J Hum Genet. 2003;72:429–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Smaoui N, Chaabouni M, Sergeev YV, et al. Screening of the eight BBS genes in Tunisian families: no evidence of triallelism. Invest Ophthalmol Vis Sci. 2006;47:3487–3495 [DOI] [PubMed] [Google Scholar]
- 29. Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet-Biedl syndrome: results of a population survey. J Med Genet. 1999;36:437–446 [PMC free article] [PubMed] [Google Scholar]
- 30. Smith RJH, Holcomb JD, Daiger SP, et al. Exclusion of Usher syndrome gene from much of chromosome 4. Cytogenet Cell Genet. 1989;50:102–106 [DOI] [PubMed] [Google Scholar]
- 31. Billingsley G, Bin J, Fieggen KJ, et al. Mutations in chaperonin-like BBS genes are a major contributor to disease development in a multiethnic Bardet-Biedl syndrome patient population. J Med Genet. 2010;47:453–463 [DOI] [PubMed] [Google Scholar]
- 32. White DR, Ganesh A, Nishimura D, et al. Autozygosity mapping of Bardet-Biedl syndrome to 12q21.2 and confirmation of FLJ23560 as BBS10. Eur J Hum Genet. 2007;15:173–178 [DOI] [PubMed] [Google Scholar]
- 33. Fan Y, Esmail MA, Ansley SJ, et al. Mutations in a member of the Ras superfamily of small GTP-binding proteins causes Bardet-Biedl syndrome. Nat Genet. 2004;36:989–993 [DOI] [PubMed] [Google Scholar]
- 34. Badano JL, Ansley SJ, Leitch CC, Lewis RA, Lupski JR, Katsanis N. Identification of a novel Bardet-Biedl syndrome protein, BBS7, that shares structural features with BBS1 and BBS2. Am J Hum Genet. 2003;72:650–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Li JB, Gerdes JM, Haycraft CJ, et al. Comparative genomics identifies a flagellar and basal body proteome that includes the BBS5 human disease gene. Cell. 2004;117:541–552 [DOI] [PubMed] [Google Scholar]
- 36. Sapp JC, Nishimura D, Johnston JJ, et al. Recurrence risks for Bardet-Biedl syndrome: Implications of locus heterogeneity. Genet Med. 2010;12:623–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Janssen S, Ramaswami G, Davis EE, et al. Mutation analysis in Bardet-Biedl syndrome by DNA pooling and massively parallel resequencing in 105 individuals. Hum. Genet. 2011;129:79–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nachury MV, Loktev AV, Zhang Q, et al. A core complex of BBS proteins cooperates with the GTPase Rab8 to promote ciliary membrane biogenesis. Cell. 2007;129:1201–1213 [DOI] [PubMed] [Google Scholar]
- 39. Badano JL, Katsanis N. Beyond Mendel: an evolving view of human genetic disease transmission. Nat Rev Genet. 2002;3:779–789 [DOI] [PubMed] [Google Scholar]
- 40. Seo S, Baye LM, Schulz NP, et al. BBS6, BBS10, and BBS12 form a complex with CCT/TRiC family chaperonins and mediate BBSome assembly. Proc Natl Acad Sci U S A. 2010;107:1488–1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sayer JA, Otto EA, O'Toole JF, et al. The centrosomal protein nephrocystin-6 is mutated in Joubert syndrome and activates transcription factor ATF4. Nat Genet. 2006;38:674–681 [DOI] [PubMed] [Google Scholar]
- 42. Baala L, Audollent S, Martinovic J, et al. Pleiotropic effects of CEP290 (NPHP6) mutations extend to Meckel syndrome. Am J Hum Genet. 2007;81:170–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.