Abstract
Background
The accuracy of screening for anal cancer precursors relative to screening for cervical cancer precursors has not been systematically examined. The aim of the current meta-analysis was to compare the relative accuracy of anal cytology to cervical cytology in discriminating between histopathologic high grade and lesser grades of dysplasia when the reference standard biopsy is obtained using colposcope magnification.
Methods and Findings
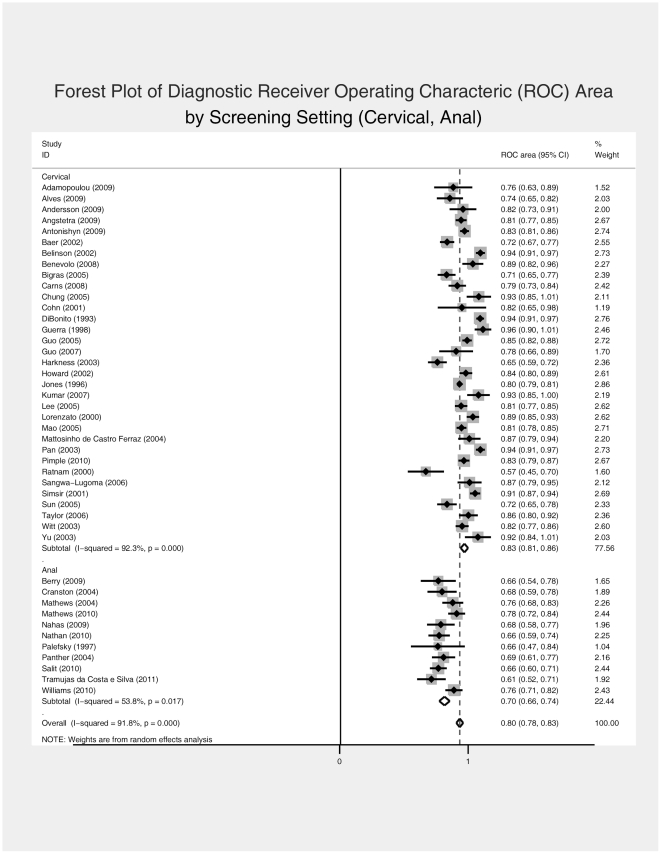
The outcome metric of discrimination was the receiver operating characteristic (ROC) curve area. Random effects meta-analysis of eligible studies was performed with examination of sources of heterogeneity that included QUADAS criteria and selected covariates, in meta-regression models. Thirty three cervical and eleven anal screening studies were found to be eligible. The primary meta-analytic comparison suggested that anal cytologic screening is somewhat less discriminating than cervical cytologic screening (ROC area [95% confidence interval (C.I.)]: 0.834 [0.809–0.859] vs. 0.700 [0.664–0.735] for cervical and anal screening, respectively). This finding was robust when examined in meta-regression models of covariates differentially distributed by screening setting (anal, cervical).
Conclusions
Anal cytologic screening is somewhat less discriminating than cervical cytologic screening. Heterogeneity of estimates within each screening setting suggests that other factors influence estimates of screening accuracy. Among these are sampling and interpretation errors involving both cytology and biopsy as well as operator skill and experience.
Introduction
The accuracy of screening procedures for anal cancer and its precursors relative to comparable procedures used in screening for cervical cancer and its precursors has not been systematically defined. The issue is of importance because invasive anal cancer rates are increasing among HIV-infected persons[1], [2] and because screening programs modeled on procedures used in cervical cancer screening are being increasingly implemented among persons at increased risk for anal cancer[3]. The primary objective of this study was to meta-analytically compare a summary operating characteristic of the performance of cervical and anal cytology testing in the detection of cervical and anal cancer and their precursors, when the reference standard biopsy is obtained at colposcopy or high resolution anoscopy (HRA), respectively.
Methods
Data Sources and Searches
Cervical
Data sources included: (1) MEDLINE from 2000 through 2010; (2) review of two previously published meta-analyses of cervical cytology accuracy.[4], [5] The MEDLINE search strategy included the following search terms in any field: cervical cytology AND sensitivity AND specificity AND cervical intraepithelial neoplasia AND year of publication 2000-2010. Searches were limited to English-language publications. Unpublished studies were ineligible for inclusion. Authors were not contacted to provide data in the eligible format if the published manuscript had incomplete data for analysis.
Anal
Data sources included: (1) MEDLINE from 1990 through 2010; (2) review of published systematic reviews [6]–[9]. Because the search algorithm comparable to that used for cervical publications yielded only 33 potentially relevant publications, the search strategy for anal publications was broadened. The MEDLINE search included the following search strategy in any field: (anal cancer OR anal dysplasia OR anal cytology OR anal intraepithelial neoplasia) AND screening AND ((sensitivity AND specificity) OR accuracy). Unpublished and non-English language publications were ineligible for inclusion. When a publication appeared to be eligible for inclusion but the data presented in the manuscript was incomplete, authors were contacted to request data in the required format (see below).
Study Selection
In establishing study inclusion and exclusion criteria we used the following definitions of index and reference tests. The index test was cytologic sampling of cervicovaginal or anal canal tissues using cytology swabs or brushes and processing of the samples using either traditional slide fixation or liquid cytologic media. The reference standard was defined as colposcope magnified and directed punch biopsy of the uterine cervix or anal canal, respectively. Operator visual impression without a biopsy could not be included as part of the definition of the reference standard result. Inclusion criteria included published reports: (1) of primary screening or follow up evaluation for previous cytologic abnormalities; (2) use of the Bethesda 1991 or 2001 Classification System (or equivalent); (3) reference standard diagnosis by cervical or anal punch biopsy obtained using colposcope magnification; the addition of endocervical curettage sampling was allowed for colposcopy studies; (4) average time interval between cytology and punch biopsy ≤3 months; (5) availability of extractable data in the format below (Table 1), where “cases” are defined as those with histopathologic evidence by punch biopsy (cervical or anal) of cervical or anal intraepithelial neoplasia 2 (CIN 2 or AIN 2) or greater and cytology diagnostic categories include negative (“no atypical or malignant cells”), atypical squamous cells of uncertain significance (ASCUS), atypical squamous cells can't rule out high grade (ASC-H), low grade squamous intraepithelial lesion (LSIL), and high grade intraepithelial lesion (HSIL):
Table 1. Data format extracted for each included study in the present meta-analysis.
| Cytology | ||||
| Biopsy | Negative | ASCUS | LSIL | ≥HSIL or ASC-H |
| ≥CIN 2 (AIN 2) | ||||
| <CIN 2 (AIN 2) | ||||
Exclusion criteria included: (1) reference standard established only by visual inspection at colposcopy or anoscopy without biopsy; (2) patients with normal colposcope magnified visual impression but no biopsy were classified as normal histology; (3) cervical cytology study sample explicitly included patients previously treated by conization or LLETZ (because of unavailability of comparable study populations for anal cytology studies).
Data Extraction
In abstracting cytology data from the included publications, the following conventions were followed: (1) inflammatory changes were categorized with the “negative” category; (2) AGUS was categorized with ASCUS; (3) HPV changes or koilocytes were classified under LSIL; (4) the category “≥HSIL” included ASC-H, HSIL, CIS, and invasive carcinoma.
The main outcome measure was the receiver operating characteristic (ROC) curve area estimated from the extracted 2 by 4 data tables, wherein the cytology diagnostic categories are treated as ordinal measures and the reference standard is binary. An ROC metric to summarize the ability of cervical (anal) cytology to discriminate between ≥CIN 2 (AIN 2) and < CIN 2 (AIN 2) histology has been previously used [10]–[12] and has the advantage of not being cut point dependent.
Each identified publication was reviewed by a single reviewer (WCM) and classified as ineligible or potentially eligible based on review of the title and abstract. When ineligibility was in doubt, full reports were reviewed for a final determination. Full reports of potentially eligible publications were then independently reviewed by two investigators. Final eligibility determination was based on consensus of the two reviewers. Decisions regarding final eligibility for inclusion were made without knowledge of the cytology ROC area, which is the primary outcome metric of the meta-analysis.
Validity Assessment: Study Quality and Covariate Rating
Eligible publications were reviewed using the QUADAS tool [13]–[15]. Further specification of quality and covariate review criteria was operationalized using the following additional questions:
Were patients undergoing the reference standard procedure (colposcopy or HRA directed punch biopsy) selected on the basis of prior screening cytology results? (Yes/No/Unclear)[verification bias]
What was the time interval between the test cytology and the reference standard procedure? (same day/ not same day but within 3 months/Unclear)[disease progression bias]
Was the reference standard result based only on punch biopsy interpretation? (punch biopsy only/composite of punch biopsy and colposcopy-HRA visual impression/mixture of punch biopsy and other histology/Unclear)[reference standard definition]
What cytology method was used? (Conventional/Thin Prep/Other liquid cytology/Unclear)
Were histologic and/or cytologic results reviewed for final classification by central adjudication or independent readers? (Yes/No/Unclear)
Did the study sample explicitly include HIV infected patients? (Yes/No/Unclear)
What was the study design? (Clinical Cohort/Case Control/Convenience sample of matched cytology and histology results/Clinical Trial/Other/Unclear)
What cytology classification system was used? (Bethesda 1991/Bethesda 2001/Other comparable/Other not comparable/Unclear)
The study quality review was separately scored by two co-authors (WCM and WA). Discordant ratings were resolved by consensus. Initial agreement (prior to consensus review) among reviewers was summarized using the prevalence and biased adjusted kappa statistic (PABAK)[16] implemented in WinPEPI version 11.4.[17]
Data Synthesis and Analysis
For each eligible and included study, the diagnostic ROC area was estimated from extracted 2 by 4 raw frequency tables using the roctab procedure in Stata version 11.2 (StataCorp, College Station, TX). Estimated ROC areas with their standard errors (s.e.) were then pooled using the random effects model of DerSimonian and Laird[18] as implanted in the Stata metan procedure. The primary analysis included all eligible studies. A secondary planned analysis was performed conditioning on two factors that may influence comparability of the two screening contexts: (1) the time interval between most recent cytology and biopsy; and (2) the operative method for obtaining the histology reference standard. For this secondary analysis, included studies were limited to those reporting both same day cytology and histology reference standard based exclusively on colposcope directed punch biopsy.
Heterogeneity of effects was evaluated using the I2-statistic[19] and further explored with funnel plots graphing ROC area against s.e.(ROC) to detect asymmetry suggesting bias. The Egger test was performed as a quantitative test of skewness in the funnel plot.[20] Finally, we performed random effects meta-regression as implemented using the Stata metareg procedure including as covariates those QUADAS and covariate measures that were differentially distributed across screening setting (p<0.20) in contingency table analysis. Covariates found to be associated with the ROC outcome (p<0.05) in metagression models jointly adjusted for screening setting (cervical, anal) were used as stratification factors to estimate the effect of screening setting (cervical, anal) within levels of the same covariates.
Results
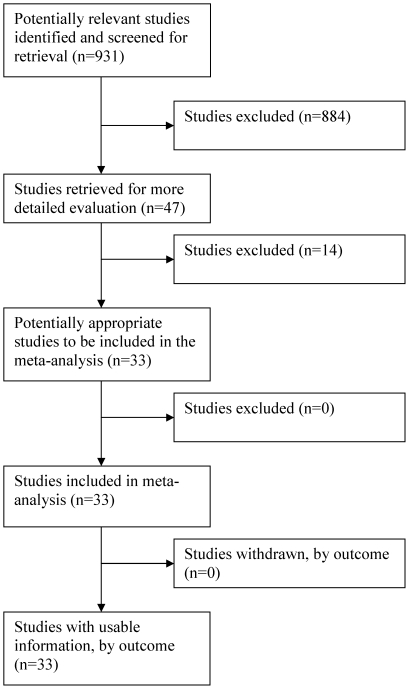
Trial Flow: Cervical Cytology-Biopsy Studies
From the MEDLINE search algorithm for cervical studies, 931 unduplicated publications were initially identified. Primary reasons for exclusion of 884 publications on initial screen included: (1) lack of relevance to the research question; (2) incomplete data for analysis evident by review of abstract; and (3) use of cytology system not comparable to Bethesda system. The remaining 47 publications were judged to be potentially eligible for study inclusion, and their manuscripts were independently reviewed for final determination of eligibility by two investigators (WCM and WA). Of these, 14 were excluded for the following reasons (more than one may apply to each study): (1) non-biopsied patients were classified as having normal histology if colposcopic appearance was normal (n = 4); (2) cytology-biopsy interval either not stated or exceeded average of 3 months (n = 8); (3) reported data aggregated across cytology categories (n = 2); (4) cytology classification not comparable to Bethesda system (n = 1); and (5) substantial missing data (31/52) with small sample size (n = 1). The thirty three remaining studies met eligibility criteria and were included (Figure 1).
Figure 1. Flow of Included Studies: Cervical Screening.
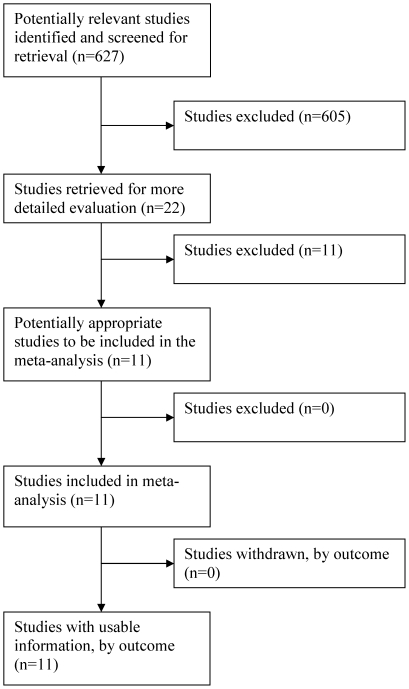
Trial Flow: Anal Cytology-Biopsy Studies
From the MEDLINE search strategy for anal publications, 627 unduplicated publications were initially identified. Of these, 605 were excluded on preliminary screen. Primary reasons for exclusion included: (1) lack of relevance to the research question; (2) lack of primary data (e.g. review articles); (3) incomplete data collected as evident from review of the abstract (e.g. investigators did not use colposcopic magnification or range of studied cytology results restricted). The remaining 22 studies were judged to be potentially eligible. Of the 22, 11 were excluded after detailed review and attempts to contact authors for clarification or data. Nine authors were emailed with requests to provide data in the required format. Of the 9, 4 responded and 1 was able to provide eligible data. Reasons for final exclusion of the 11 studies (more than one category may apply to each study) were: (1) incomplete data for analysis (n = 8); (2) cytology-biopsy interval either not stated or exceeded average of 3 months (n = 5); (3) HRA not performed in all reported cases (n = 2); and (4) cytology classification not comparable to Bethesda system (n = 1). The final number of included eligible studies was eleven (Figure 2).
Figure 2. Flow of Included Studies: Anal Screening.
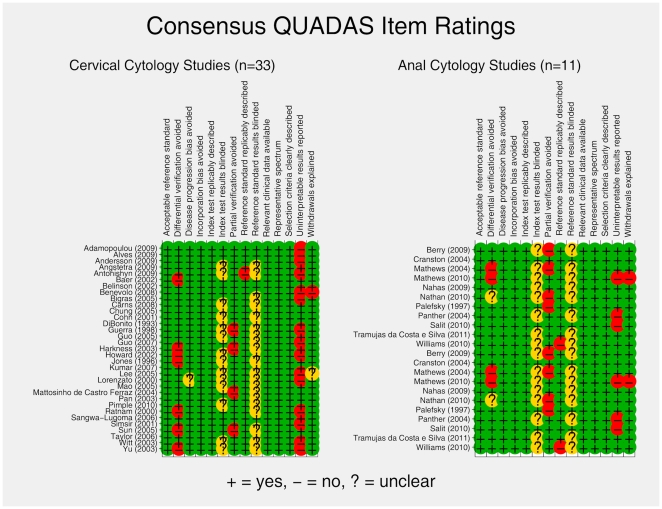
Study Characteristics: Study Quality and Covariate Review
PABAK agreement (median [range]) between the two primary study reviewers on QUADAS item scoring was 0.72 [0.44 – 0.94] and 0.73 [0 – 0.82], for cervical and anal cytology studies, respectively. PABAK was not estimable for those items for which reviewers uniformly chose a single rating option. Consensus QUADAS ratings by study category (cervical or anal) are presented in Figure 3. Reviewers judged that study participants were selected based on prior cytology screening results in 58% and 27% (p = 0.192) of cervical and anal cytology studies, respectively. There was no difference in the distribution of cytology-biopsy time intervals comparing cervical to anal studies, with 71% and 82% (p = 0.774) of studies reporting same day cytology and biopsy measures, respectively. With regard to the histological reference standard, 91% of anal studies reported exclusive use of HRA directed punch biopsy whereas 65% of the cervical studies reported exclusive use of colposcopically directed punch biopsy (p = 0.344). The most common additional histological reference standard component included in the cervical studies was endocervical curettage. There was no difference in reported cytological method between the two study types with 65% and 64% (p = 0.364) of cervical and anal studies reporting use of conventional cytology, respectively. Only 3% of cervical studies reported on HIV-infected participants, whereas 100% of anal studies included (not necessarily exclusively) HIV infected persons. By study design, 80% of the cervical studies were cohort designs in comparison 91% of anal studies; 12% and 9% of cervical and anal studies, respectively, were cross sectional studies involving matching of available cytology to biopsy results. The Bethesda 1991 cytology system was reported in 71% and 36% (p = 0.12) of cervical and anal studies, respectively. This difference reflects the more recent publication of HRA studies.
Figure 3. Consensus QUADAS ratings by study category (Cervical or Anal).
Quantitative Data Synthesis
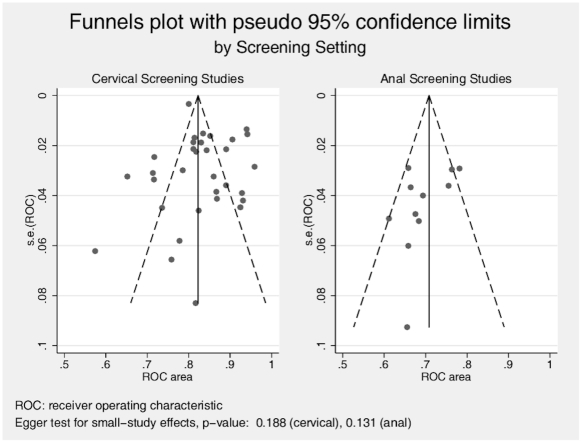
Table S1 presents the data extraction results and summary metric (cytology-biopsy ROC area) organized by study type (cervical and anal). The primary analysis (Figure 4) comparing the ability of cervical and anal cytology to discriminate between high grade and non-high grade histology by colposcope directed biopsy suggested superiority for cervical screening (ROC area [95% C.I.]: 0.834 [0.809 – 0.859] vs. 0.700 [0.664 – 0.735] for cervical and anal screening, respectively). While heterogeneity of effect was evident among studies for both screening contexts, it was greater among cervical screening studies (I2 statistic 92.3%, p<0.0001 for cervical studies and 53.8%, p = 0.017 for anal studies). This difference in heterogeneity across screening context is also evident in the funnel plots (Figure 5), which demonstrate that relatively more of the cervical screening studies fall outside the pseudo 95% confidence intervals than is observed for the anal screening studies. The relative symmetry of both funnel plots is supported by the non-significant Egger test for both.
Figure 4. Forest Plot of Diagnostic Receiver Operating Characteric (ROC) Area, by Screening Setting (Cervical, Anal).
Figure 5. Funnel plots with pseudo 95% confidence limits, by Screening Setting.
When the analysis was restricted to those studies reporting both concurrent (same day) cytology and biopsy and also reporting histology reference standard obtained exclusively using punch biopsy (excluding endocervical curettage), the difference between screening contexts was greater than that estimated for the unrestricted primary analysis (ROC area [95% C.I.]: 0.871 [0.844 – 0.899] vs. 0.690 [0.649 – 0.732] for cervical and anal screening, respectively).
The distributions of the following QUADAS items and covariates were differential (p<0.20) in contingency table analyses of study characteristics and screening setting: (1) QUADAS 5 (partial verification bias)[p = 0.071], (2) QUADAS 10 (index test blinded)[p = 0.082], (3) patients referred for biopsy on the basis of prior screening cytology [p = 0.087],(4) HIV-infected patients included in study [p<0.0001], and (5) the cytology classification system used [p = 0.092]. Each of these five characteristics was entered as a categorical indicator in separate random effects meta-regressions that included also screening setting (cervical, anal) to identify those that were explanatory of heterogeneity in estimated ROC outcome. Of these five study characteristics, only the item dealing with referral for colposcope directed biopsy conditional upon screening cytology results was significantly associated with estimates of ROC heterogeneity in random effects meta-regression models (Table 2, Model 3). It is also evident in Table 2 that, with the exception of Model 4 (HIV+ patients included), the estimated effect of screening setting remained statistically significant and in all models consistent with the overall effect screening setting favoring cervical screening over anal screening. Regarding Model 4, it should be noted that only 1 of 32 cervical screening studies explicitly included HIV infected patients whereas all 11 of the anal screening studies included HIV infected patients. So the effect of screening setting was strongly confounded with the HIV covariate.
Table 2. Meta-Regression Estimates of Joint Effects of Screening Setting and Selected Covariates (n = 44 studies).
| Model | Covariate | b[covariate] | s.e.[covariate | p[covariate] | b[screening setting3] | s.e.[screening setting] | p[screening setting] |
| 1 | QUADAS 51 [reference = yes] | -- | |||||
| QUADAS 5 = no | -0.028 | 0.034 | 0.419 | -0.132 | 0.03 | <0.0001 | |
| 2 | QUADAS 102 [reference: yes] | -- | |||||
| QUADAS 10 = unclear | 0.2 | 0.025 | 0.445 | -0.143 | 0.03 | <0.0001 | |
| 3 | Conditional referral for biopsy [reference: yes] | 0.045 | |||||
| no | 0.061 | 0.026 | 0.023 | -0.153 | 0.028 | <0.0001 | |
| unclear | 0.061 | 0.035 | 0.085 | ||||
| 4 | HIV+ patients included [reference: yes] | -- | |||||
| no | 0.016 | 0.112 | 0.885 | -0.121 | 0.114 | 0.296 | |
| 5 | Cytology Classification System [reference: Bethesda 1991] | -- | 0.836 | ||||
| Bethesda 2001 | -0.01 | 0.029 | 0.726 | -0.131 | 0.032 | <0.0001 | |
| Other comparable | -0.032 | 0.059 | 0.588 |
1. QUADAS 5. Partial verification avoided.
2. QUADAS 10. Index test results blinded.
3. Screening setting: anal. Reference: cervical.
Because Model 3 (referral for biopsy conditional upon screening cytology results) suggested that conditional referral was associated with at least part of the observed effect heterogeneity in the primary meta analytic result, we re-estimated the screening setting effects for each of the three rating options for conditional referral (yes, no, unclear). The estimated pooled ROC effects for screening setting restricting eligibility to those studies for which the conditional referral item was rated “yes” were: 0.797 (95% CI: 0.771–0.822) for cervical screening (n = 19 studies) and 0.749 (0.699–0.798) for anal screening (n = 3 studies), with associated I2 heterogeneity estimates of 86.3% and 37.3%, respectively. The corresponding pooled ROC effect estimates restricting eligibility to studies for which the conditional referral item was rates “no” were: 0.898 (0.865–0.931) for cervical screening (n = 10 studies) and 0.657 (0.621–0.694) for anal screening (n = 6 studies), with associated I2 estimates of 74.9% and 0%, respectively. Finally for the conditional referral rating of “unclear” for which there were only 4 eligible cervical and 2 eligible anal studies, the corresponding pooled ROC estimates were 0.868 (0.785–0.951) and 0.716 (0.618–0.813) with I2 estimates of 91.8% and 77.5%, respectively. Thus, in these exploratory analyses based on meta-regression results, non-overlapping ROC confidence intervals were observed only for the conditional referral category of “no” while the subgroup study sample size was considerably reduced for each restricted comparison.
Discussion
To our knowledge, this study is the first attempt to systematically compare the relative accuracy of anal and cervical screening for cancer precursors. In the primary meta-analysis of 33 cervical and 11 anal screening studies, we found that anal cytologic screening appeared to be somewhat less discriminating than cervical cytologic screening for detecting high grade histopathologic lesions (≥CIN 2 or AIN 2): (1) when the index of discrimination is defined as area under the receiver operating characteristic (ROC) curve; (2) when the reference standard biopsy is obtained using colposcope magnification; and (3) when the interval between cytology and biopsy is less than or equal to 3 months. This conclusion was robust when restricting study eligibility by requiring that cytology and histology be ascertained on the same day using only punch biopsy to obtain the reference standard diagnosis. Although there was considerable heterogeneity among both cervical and anal screening studies (more so among cervical studies), we found that the primary result was confirmed in meta-regression models controlling for those study quality indicators and covariates that were differentially associated with screening setting (cervical, anal).
A number of factors may account for or contribute to the primary meta-analytic finding. First is the possibility that the currently used screening procedures for anal cancer and its precursors are intrinsically less accurate than the comparable procedures for cervical screening. Cytology is obtained blindly in anal screening and under direct visualization in cervical screening. In addition, obtaining the reference standard biopsy is more challenging in the anal canal because of the collapsing nature of the organ such that lesions may be obscured by tissue folds not adequately retracted [21].
However before concluding intrinsic inferiority of anal screening, sources of bias in the conduct of the meta-analysis must be examined. First, our study selection procedures differed by screening setting as discussed in the Methods section. We used expanded MEDLINE search terms to initially identify potentially eligible anal screening studies because of the low yield when applying the terms used to identify cervical screening studies. Second, we contacted authors for clarifying information and for formatted data for the potentially eligible anal studies but not for the cervical studies. Third, the response rate from contacted authors of anal screening studies was low. Fourth, we excluded studies (both cervical and anal) that examined other metrics of cytology screening performance (sensitivity, specificity, predictive value) when data inadequate to estimate our ROC metric were either not published or not made available upon data request (in the case of anal studies). We do not know whether these procedural decisions resulted in biased study selection and estimation of effects. However we required that decisions regarding study selection were made prior to estimating study ROC outcomes. Furthermore, examination of the funnel plot symmetry and non-significant Egger tests provide some support for a conclusion that selection of publications was not seriously biased.
The sample size (n = 21,616) of one cervical screening study, Jones (1996), far exceeded the sample sizes of all other included studies and would have dominated the analysis using a fixed effect weighting procedure. The median [range] sample sizes for the anal and cervical studies were 169 [75, 401] and 448 [54, 21616]. We chose random effects meta-analysis in order to allow estimation of the true effect to vary between studies and to give relatively greater weight to smaller studies.[22] The primary meta-analytic result was concordant for both random and fixed effect models; the pooled fixed effect ROC estimates (95% CI) for anal and cervical screening studies were 0.708 (0.685–0.731) and 0.823 (0.818–0.828), respectively.
Although a few of the included studies addressed the issue of verification bias, the raw data abstracted from all included studies was unadjusted for verification bias. The study raters judged that 58% of included cervical screening studies and 27% of anal studies were subject to potential verification bias in that referral for colposcopy or HRA was conditional upon screening cytology results. Although conditional referral was identified in meta-regression analysis as significantly associated with ROC heterogeneity (Table 2, Model 3), controlling for it did not alter the primary meta-analytic result.
If one accepts our meta-analytic ROC estimates as valid, what conclusions can be drawn regarding screening for anal cancer precursors? First, we believe that the finding of somewhat less discriminatory ability for anal cytology than for cervical cytology does not diminish the rationale for anal cancer screening. The rationale has been argued cogently with an accumulating evidence base[7], [23] on the basis of accepted criteria for public health screening[24], albeit with considerable uncertainty regarding the efficacy of treatments for anal cancer precursors identified through screening and also regarding screening logistics (who to screen, how to screen, how often to screen).[8] Second, experience with performing anal cytology and HRA is much more limited and recent than comparable experience screening for cervical cancer and its precursors. It is known that operator experience makes a difference [25] and HRA investigators and practitioners are still learning to optimize techniques.[26], [27] Heterogeneity of ROC estimates may in part reflect operator experience and skill such that the ceiling for accuracy of combined screening with cytology, HRA, and biopsy components may not yet have been achieved. Third, studies of accuracy of both cervical and anal screening procedures should take into account the fact that the reference standard of punch biopsy is itself an imperfect reference standard subject to sampling and interpretation error[28] just as is the case for cytological screening.[21] Fourth, a recent cost-effectiveness analysis of screening for anal cancer precursors in HIV-infected men having sex with men concluded that direct use of HRA was the most cost-effective strategy for detecting AIN 2/3 that high risk population.[29] It is our view, however, that because that conclusion assumed that HRA directed biopsy was itself a perfect reference standard and did not take into account the potential value of repeated cytological examination combined with digital rectal examination, our finding of somewhat less discriminating performance of anal cytology in comparison with cervical cytology does not of itself support a recommendation to eliminate prior cytology screening as a component of screening for anal cancer precursors in high risk populations. In conclusion, we believe that our results better define the relative accuracy of screening for anal cancer precursors and contribute to ongoing policy discussions regarding formulation of guidelines regarding anal cancer screening in populations at risk.
Supporting Information
Extracted Study Data and Outcome Metrics, by Study Type Cytology-Biopsy Joint Cell Frequencies.
(DOCX)
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported in part by the Clinical Investigation Core of the University of California San Diego Center for AIDS Research [AI036214], the CFAR Network of Integrated Clinical Systems (CNICS) [R24 AI067039-01A1], and the Pacific AIDS Education and Training Center (PAETC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Piketty C, Selinger-Leneman H, Grabar S, Duvivier C, Bonmarchand M, et al. Marked increase in the incidence of invasive anal cancer among HIV-infected patients despite treatment with combination antiretroviral therapy. AIDS. 2008;22:1203–1211. doi: 10.1097/QAD.0b013e3283023f78. [DOI] [PubMed] [Google Scholar]
- 2.D'Souza G, Wiley DJ, Li X, Chmiel JS, Margolick JB, et al. Incidence and epidemiology of anal cancer in the multicenter AIDS cohort study. Journal of acquired immune deficiency syndromes. 2008;48:491–499. doi: 10.1097/QAI.0b013e31817aebfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palefsky J. San Francisco: University of California San Francisco; 2011. Anal Cancer Info. pp. List of HRA providers. [Google Scholar]
- 4.Fahey MT, Irwig L, Macaskill P. Meta-analysis of Pap test accuracy. American journal of epidemiology. 1995;141:680–689. doi: 10.1093/oxfordjournals.aje.a117485. [DOI] [PubMed] [Google Scholar]
- 5.Nanda K, McCrory DC, Myers ER, Bastian LA, Hasselblad V, et al. Accuracy of the Papanicolaou test in screening for and follow-up of cervical cytologic abnormalities: a systematic review. Annals of internal medicine. 2000;132:810–819. doi: 10.7326/0003-4819-132-10-200005160-00009. [DOI] [PubMed] [Google Scholar]
- 6.Bean SM, Chhieng DC. Anal-rectal cytology: a review. Diagnostic cytopathology. 2010;38:538–546. doi: 10.1002/dc.21242. [DOI] [PubMed] [Google Scholar]
- 7.Chiao EY, Giordano TP, Palefsky JM, Tyring S, El Serag H. Screening HIV-infected individuals for anal cancer precursor lesions: a systematic review. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2006;43:223–233. doi: 10.1086/505219. [DOI] [PubMed] [Google Scholar]
- 8.Fox P. Anal cancer screening in men who have sex with men. Current opinion in HIV and AIDS. 2009;4:64–67. doi: 10.1097/coh.0b013e32831a6fe0. [DOI] [PubMed] [Google Scholar]
- 9.Oon SF, Hanly A, Winter DC. Pap smears for men: a vision of the future? Irish journal of medical science. 2010;179:459–462. doi: 10.1007/s11845-009-0340-6. [DOI] [PubMed] [Google Scholar]
- 10.Davey E, Irwig L, Macaskill P, Clarke J, Thurloe J, et al. Does providing previous results change the accuracy of cervical cytology? Acta Cytol. 2009;53:644–652. doi: 10.1159/000325405. [DOI] [PubMed] [Google Scholar]
- 11.Cohn JA, Gagnon S, Spence MR, Harrison DD, Kluzak TR, et al. The role of human papillomavirus deoxyribonucleic acid assay and repeated cervical cytologic examination in the detection of cervical intraepithelial neoplasia among human immunodeficiency virus-infected women. Cervical Disease Study Group of the American Foundation for AIDS Research Community Based Clinical Trials Network. Am J Obstet Gynecol. 2001;184:322–330. doi: 10.1067/mob.2001.109938. [DOI] [PubMed] [Google Scholar]
- 12.Taoka H, Yamamoto Y, Sakurai N, Fukuda M, Asakawa Y, et al. Comparison of conventional and liquid-based cytology, and human papillomavirus testing using SurePath preparation in Japan. Human cell : official journal of Human Cell Research Society. 2010;23:126–133. doi: 10.1111/j.1749-0774.2010.00093.x. [DOI] [PubMed] [Google Scholar]
- 13.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC medical research methodology. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, et al. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC medical research methodology. 2006;6:9. doi: 10.1186/1471-2288-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dwamena BA. Ann Arbor, Michigan: Division of Nuclear Medicine, Department of Radiology, University of Michigan Medical School; 2010. quadas: A program for graphical depiction of study quality assessment for diagnostic test accuracy reviews. [Google Scholar]
- 16.Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. Journal of clinical epidemiology. 1993;46:423–429. doi: 10.1016/0895-4356(93)90018-v. [DOI] [PubMed] [Google Scholar]
- 17.Abramson JH. WINPEPI updated: computer programs for epidemiologists, and their teaching potential. Epidemiologic Perspectives & Innovations. 2011;8 doi: 10.1186/1742-5573-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mathews WC, Cachay ER, Caperna J, Sitapati A, Cosman B, et al. Estimating the accuracy of anal cytology in the presence of an imperfect reference standard. PloS one. 2010;5:e12284. doi: 10.1371/journal.pone.0012284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, et al. metan: fixed- and random-effects meta-analysis. The Stata Journal. 2008;8:3–28. [Google Scholar]
- 23.Darragh TM, Winkler B. Anal cancer and cervical cancer screening: key differences. Cancer cytopathology. 2011;119:5–19. doi: 10.1002/cncy.20126. [DOI] [PubMed] [Google Scholar]
- 24.Andermann A, Blancquaert I, Beauchamp S, Dery V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bulletin of the World Health Organization. 2008;86:317–319. doi: 10.2471/BLT.07.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathews C, Caperna J, Cachay ER, Cosman B. Early impact and performance characteristics of an established anal dysplasia screening program: program evaluation considerations. The open AIDS journal. 2007;1:11–20. doi: 10.2174/1874613600701010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jay N, Berry JM, Hogeboom CJ, Holly EA, Darragh TM, et al. Colposcopic appearance of anal squamous intraepithelial lesions: relationship to histopathology. Diseases of the colon and rectum. 1997;40:919–928. doi: 10.1007/BF02051199. [DOI] [PubMed] [Google Scholar]
- 27.Berry JM, Palefsky J. Invited Commentary. Dis Colon Rectum. 2009;52:1860–1863. doi: 10.1097/01.dcr.0000361970.30352.e0. [DOI] [PubMed] [Google Scholar]
- 28.Lytwyn A, Salit IE, Raboud J, Chapman W, Darragh T, et al. Interobserver agreement in the interpretation of anal intraepithelial neoplasia. Cancer. 2005;103:1447–1456. doi: 10.1002/cncr.20927. [DOI] [PubMed] [Google Scholar]
- 29.Lam JM, Hoch JS, Tinmouth J, Sano M, Raboud J, et al. Cost-effectiveness of screening for anal precancers in HIV-positive men. AIDS. 2011;25:635–642. doi: 10.1097/QAD.0b013e3283434594. [DOI] [PubMed] [Google Scholar]
- 30.Adamopoulou M, Kalkani E, Charvalos E, Avgoustidis D, Haidopoulos D, et al. Comparison of cytology, colposcopy, HPV typing and biomarker analysis in cervical neoplasia. Anticancer Res. 2009;29:3401–3409. [PubMed] [Google Scholar]
- 31.Alves RR, Rabelo-Santos SH, Ribeiro AA, Carneiro MA, Ximenes Y, et al. Usefulness of repeat cytology at the time of first colposcopy. Diagn Cytopathol. 2009;37:68–73. doi: 10.1002/dc.20976. [DOI] [PubMed] [Google Scholar]
- 32.Andersson S, Sowjanya P, Wangsa D, Hjerpe A, Johansson B, et al. Detection of genomic amplification of the human telomerase gene TERC, a potential marker for triage of women with HPV-positive, abnormal Pap smears. Am J Pathol. 2009;175:1831–1847. doi: 10.2353/ajpath.2009.090122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angstetra D, Tait T, Tan J, Symonds I. Should liquid-based cytology be performed prior to colposcopy? A comparison of the accuracy, unsatisfactory rates and cost in a tertiary referral setting. Aust N Z J Obstet Gynaecol. 2009;49:681–684. doi: 10.1111/j.1479-828X.2009.01095.x. [DOI] [PubMed] [Google Scholar]
- 34.Antonishyn NA, Horsman GB, Kelln RA, Severini A. Human papillomavirus typing and viral gene expression analysis for the triage of women with abnormal results from papanicolaou test smears to colposcopy. Arch Pathol Lab Med. 2009;133:1577–1586. doi: 10.5858/133.10.1577. [DOI] [PubMed] [Google Scholar]
- 35.Baer A, Kiviat NB, Kulasingam S, Mao C, Kuypers J, et al. Liquid-based Papanicolaou smears without a transformation zone component: should clinicians worry? Obstet Gynecol. 2002;99:1053–1059. doi: 10.1016/s0029-7844(02)01998-1. [DOI] [PubMed] [Google Scholar]
- 36.Belinson JL, Pan QJ, Biscotti C, Wu LY, Pretorius RG, et al. Primary screening with liquid-based cytology in an unscreened population in rural China, with an emphasis on reprocessing unsatisfactory samples. Acta Cytol. 2002;46:470–474. doi: 10.1159/000326863. [DOI] [PubMed] [Google Scholar]
- 37.Benevolo M, Vocaturo A, Mottolese M, Mariani L, Vocaturo G, et al. Clinical role of p16INK4a expression in liquid-based cervical cytology: correlation with HPV testing and histologic diagnosis. Am J Clin Pathol. 2008;129:606–612. doi: 10.1309/BEPQXTCQD61RGFMJ. [DOI] [PubMed] [Google Scholar]
- 38.Bigras G, de Marval F. The probability for a Pap test to be abnormal is directly proportional to HPV viral load: results from a Swiss study comparing HPV testing and liquid-based cytology to detect cervical cancer precursors in 13,842 women. Br J Cancer. 2005;93:575–581. doi: 10.1038/sj.bjc.6602728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carns B, Fadare O. Papanicolaou test in the detection of high-grade cervical lesions: a re-evaluation based on cytohistologic non-correlation rates in 356 concurrently obtained samples. Int J Clin Exp Pathol. 2008;1:285–290. [PMC free article] [PubMed] [Google Scholar]
- 40.Chung JH, Park EJ, Choi YD, Kim HS, Lee YJ, et al. Efficacy assessment of CellSlide in liquid-based gynecologic cytology. Gynecol Oncol. 2005;99:597–602. doi: 10.1016/j.ygyno.2005.06.059. [DOI] [PubMed] [Google Scholar]
- 41.DiBonito L, Falconieri G, Tomasic G, Colautti I, Bonifacio D, et al. Cervical cytopathology. An evaluation of its accuracy based on cytohistologic comparison. Cancer. 1993;72:3002–3006. doi: 10.1002/1097-0142(19931115)72:10<3002::aid-cncr2820721023>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 42.Guerra B, De Simone P, Gabrielli S, Falco P, Montanari G, et al. Combined cytology and colposcopy to screen for cervical cancer in pregnancy. J Reprod Med. 1998;43:647–653. [PubMed] [Google Scholar]
- 43.Guo M, Hu L, Martin L, Liu S, Baliga M, et al. Accuracy of liquid-based Pap tests: comparison of concurrent liquid-based tests and cervical biopsies on 782 women with previously abnormal Pap smears. Acta Cytol. 2005;49:132–138. doi: 10.1159/000326120. [DOI] [PubMed] [Google Scholar]
- 44.Guo M, Patel SJ, Chovanec M, Jan YJ, Tarco E, et al. A human papillomavirus testing system in women with abnormal Pap results: a comparison study with follow-up biopsies. Acta Cytol. 2007;51:749–754. doi: 10.1159/000325838. [DOI] [PubMed] [Google Scholar]
- 45.Harkness CB, Theofrastous JP, Ibrahim SN, Galvin SL, Lawrence HC. Papanicolaou and thin-layer cervical cytology with colposcopic biopsy control. A comparison. J Reprod Med. 2003;48:681–686. [PubMed] [Google Scholar]
- 46.Howard M, Sellors J, Kaczorowski J. Optimizing the hybrid capture II human papillomavirus test to detect cervical intraepithelial neoplasia. Obstet Gynecol. 2002;100:972–980. doi: 10.1016/s0029-7844(02)02315-3. [DOI] [PubMed] [Google Scholar]
- 47.Jones BA, Novis DA. Cervical biopsy-cytology correlation. A College of American Pathologists Q-Probes study of 22 439 correlations in 348 laboratories. Arch Pathol Lab Med. 1996;120:523–531. [PubMed] [Google Scholar]
- 48.Kumar K, Iyer VK, Bhatla N, Kriplani A, Verma K. Comparative evaluation of smear cytology & hybrid capture II for the diagnosis of cervical cancer. Indian J Med Res. 2007;126:39–44. [PubMed] [Google Scholar]
- 49.Lee GY, Kim SM, Rim SY, Choi HS, Park CS, et al. Human papillomavirus (HPV) genotyping by HPV DNA chip in cervical cancer and precancerous lesions. Int J Gynecol Cancer. 2005;15:81–87. doi: 10.1111/j.1048-891x.2005.14417.x. [DOI] [PubMed] [Google Scholar]
- 50.Lorenzato F, Ho L, Terry G, Singer A, Santos LC, et al. The use of human papillomavirus typing in detection of cervical neoplasia in Recife (Brazil). Int J Gynecol Cancer. 2000;10:143–150. doi: 10.1046/j.1525-1438.2000.00007.x. [DOI] [PubMed] [Google Scholar]
- 51.Mao C, Balasubramanian A, Koutsky LA. Should liquid-based cytology be repeated at the time of colposcopy? J Low Genit Tract Dis. 2005;9:82–88. doi: 10.1097/00128360-200504000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Mattosinho de Castro Ferraz Mda G, Nicolau SM, Stavale JN, Focchi J, Castelo A, et al. Cervical biopsy-based comparison of a new liquid-based thin-layer preparation with conventional Pap smears. Diagn Cytopathol. 2004;30:220–226. doi: 10.1002/dc.10409. [DOI] [PubMed] [Google Scholar]
- 53.Pan Q, Belinson JL, Li L, Pretorius RG, Qiao YL, et al. A thin-layer, liquid-based pap test for mass screening in an area of China with a high incidence of cervical carcinoma. A cross-sectional, comparative study. Acta Cytol. 2003;47:45–50. doi: 10.1159/000326474. [DOI] [PubMed] [Google Scholar]
- 54.Pimple SA, Amin G, Goswami S, Shastri SS. Evaluation of colposcopy vs cytology as secondary test to triage women found positive on visual inspection test. Indian J Cancer. 2010;47:308–313. doi: 10.4103/0019-509X.64726. [DOI] [PubMed] [Google Scholar]
- 55.Ratnam S, Franco EL, Ferenczy A. Human papillomavirus testing for primary screening of cervical cancer precursors. Cancer Epidemiol Biomarkers Prev. 2000;9:945–951. [PubMed] [Google Scholar]
- 56.Sangwa-Lugoma G, Mahmud S, Nasr SH, Liaras J, Kayembe PK, et al. Visual inspection as a cervical cancer screening method in a primary health care setting in Africa. Int J Cancer. 2006;119:1389–1395. doi: 10.1002/ijc.21972. [DOI] [PubMed] [Google Scholar]
- 57.Simsir A, Ioffe OB, Bourquin P, Brooks SE, Henry M. Repeat cervical cytology at the time of colposcopy. Is there an added benefit? Acta Cytol. 2001;45:23–27. doi: 10.1159/000327183. [DOI] [PubMed] [Google Scholar]
- 58.Sun XR, Wang J, Garner D, Palcic B. Detection of cervical cancer and high grade neoplastic lesions by a combination of liquid-based sampling preparation and DNA measurements using automated image cytometry. Cell Oncol. 2005;27:33–41. doi: 10.1155/2005/981612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, et al. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118:957–962. doi: 10.1002/ijc.21434. [DOI] [PubMed] [Google Scholar]
- 60.Witt A, Hudelist G, Gregor H, Kucera E, Walchetseder C, et al. The detection of HPV DNA improves the recognition of cervical intraepithelial lesions. Arch Gynecol Obstet. 2003;268:29–34. doi: 10.1007/s00404-002-0320-9. [DOI] [PubMed] [Google Scholar]
- 61.Yu BK, Kuo BI, Yen MS, Twu NF, Lai CR, et al. Improved early detection of cervical intraepithelial lesions by combination of conventional Pap smear and speculoscopy. Eur J Gynaecol Oncol. 2003;24:495–499. [PubMed] [Google Scholar]
- 62.Berry JM, Palefsky JM, Jay N, Cheng SC, Darragh TM, et al. Performance characteristics of anal cytology and human papillomavirus testing in patients with high-resolution anoscopy-guided biopsy of high-grade anal intraepithelial neoplasia. Diseases of the colon and rectum. 2009;52:239–247. doi: 10.1007/DCR.0b013e31819793d9. [DOI] [PubMed] [Google Scholar]
- 63.Cranston RD, Darragh TM, Holly EA, Jay N, Berry JM, et al. Self-collected versus clinician-collected anal cytology specimens to diagnose anal intraepithelial neoplasia in HIV-positive men. Journal of acquired immune deficiency syndromes. 2004;36:915–920. doi: 10.1097/00126334-200408010-00004. [DOI] [PubMed] [Google Scholar]
- 64.Mathews WC, Sitapati A, Caperna JC, Barber RE, Tugend A, et al. Measurement characteristics of anal cytology, histopathology, and high-resolution anoscopic visual impression in an anal dysplasia screening program. Journal of acquired immune deficiency syndromes. 2004;37:1610–1615. doi: 10.1097/00126334-200412150-00014. [DOI] [PubMed] [Google Scholar]
- 65.Nahas CS, da Silva Filho EV, Segurado AA, Genevcius RF, Gerhard R, et al. Screening anal dysplasia in HIV-infected patients: is there an agreement between anal pap smear and high-resolution anoscopy-guided biopsy? Diseases of the colon and rectum. 2009;52:1854–1860. doi: 10.1007/DCR.0b013e3181b98f36. [DOI] [PubMed] [Google Scholar]
- 66.Nathan M, Singh N, Garrett N, Hickey N, Prevost T, et al. Performance of anal cytology in a clinical setting when measured against histology and high-resolution anoscopy findings. AIDS. 2010;24:373–379. doi: 10.1097/QAD.0b013e328333ab8e. [DOI] [PubMed] [Google Scholar]
- 67.Palefsky JM, Holly EA, Hogeboom CJ, Berry JM, Jay N, et al. Anal cytology as a screening tool for anal squamous intraepithelial lesions. Journal of acquired immune deficiency syndromes and human retrovirology : official publication of the International Retrovirology Association. 1997;14:415–422. doi: 10.1097/00042560-199704150-00004. [DOI] [PubMed] [Google Scholar]
- 68.Panther LA, Wagner K, Proper J, Fugelso DK, Chatis PA, et al. High resolution anoscopy findings for men who have sex with men: inaccuracy of anal cytology as a predictor of histologic high-grade anal intraepithelial neoplasia and the impact of HIV serostatus. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2004;38:1490–1492. doi: 10.1086/383574. [DOI] [PubMed] [Google Scholar]
- 69.Salit IE, Lytwyn A, Raboud J, Sano M, Chong S, et al. The role of cytology (Pap tests) and human papillomavirus testing in anal cancer screening. AIDS. 2010;24:1307–1313. doi: 10.1097/QAD.0b013e328339e592. [DOI] [PubMed] [Google Scholar]
- 70.Tramujas da Costa ESI, Coelho Ribeiro M, Santos Gimenez F, Dutra Ferreira JR, Galvao RS, et al. Performance of p16INK4a immunocytochemistry as a marker of anal squamous intraepithelial lesions. Cancer cytopathology. 2011 doi: 10.1002/cncy.20143. [DOI] [PubMed] [Google Scholar]
- 71.Williams VM, Metcalf C, French MA, McCloskey JC. Audit of paired anal cytology and histopathology outcomes in patients referred to a public sexual health clinic. Sexual health. 2010;7:346–351. doi: 10.1071/SH09118. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Extracted Study Data and Outcome Metrics, by Study Type Cytology-Biopsy Joint Cell Frequencies.
(DOCX)