Abstract
Mycobacterial tuberculous tenosynovitis of the extensor tendon sheath is an extremely rare manifestation of extrapulmonary tuberculosis. The diagnosis may be easily delayed because of its non-specific clinical signs. We report a new case of tuberculous tenosynovitis of the extensor without concomitant pulmonary tuberculosis or documented immunodeficiency.
Background
Mycobacterial tuberculous tenosynovitis of the extensor tendon sheath is an extremely rare manifestation of extrapulmonary tuberculosis.1
Case presentation
A 46-year-old man without history of previous illness presented to our rheumatology department with a history of swelling of the left wrist which gradually increased in size and which appeared 5 months before the presentation. No history of wrist trauma was found. There was no associated history of fever, loss of weight, night sweats nor fatigue. Physical examination revealed a well looking man with a non-painful left wrist swelling located in front of the extensor tendon, measuring approximately 4×4 cm. Movements of the wrist were limited at the extension.
Investigations
Tuberculin skin test showed an induration of 18 mm. Laboratory examinations showed an erythrocyte sedimentation rate of 23 mm at the first hour and a C reactive protein <5 mg/dl. Tests for rheumatoid arthritis factor, hepatitis B and C viruses, HIV, brucella and Salmonella typhi were negative. The sputum test for Mycobacterium tuberculosis was negative on direct examinations and culture. Chest x-ray was normal.
Left wrist joint x-ray showed marked soft-tissue opacity and multiple lytic areas on the lower radius metaphysis (figure 1).
Figure 1.

Anteroposterior radiography of the wrists: multiple lytic areas on the lower radius metaphysis and marked opacity on the wrist (arrowheads).
MRI of the wrist showed, on dorsolateral aspect of the wrist, an expansile lesion surrounding extensor tendons on increased T2 signal, low signal intensity on T1 and marked heterogeneous enhancement after gadolinium injection (figure 2). A surgical synovectomy was performed and macroscopic findings revealed numerous white nodules that appeared like scattered grains of boiled rice. Histopathological examination of the biopsy specimen revealed granulomatous inflammation with caseous necrosis. The diagnosis of tuberculosis extensor tenosynovitis was then established.
Figure 2.
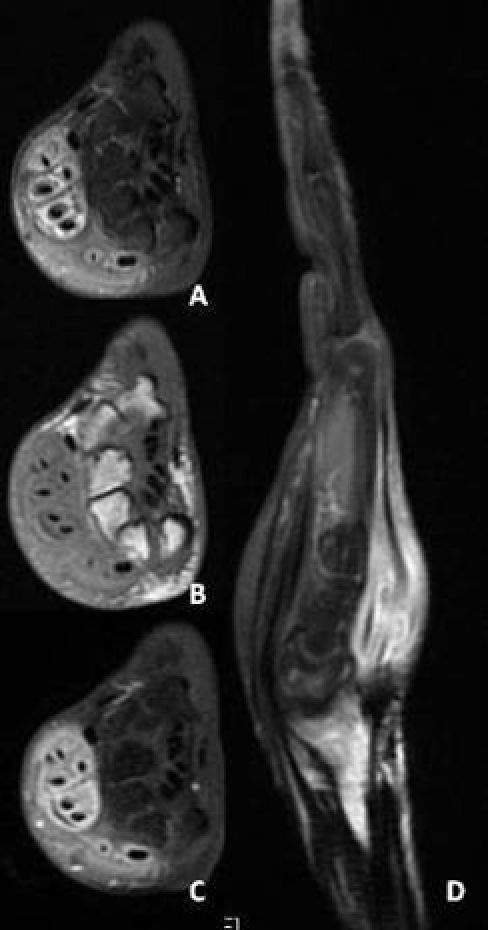
MRI of the wrist: dorsolateral aspect of the wrist showing an expansile lesion surrounding extensor tendons on increased T2 signal (A), low signal intensity on T1(B) and marked heterogeneous enhancement after gadolinium injection (D).
Differential diagnosis
Several diagnoses were discussed: De Quervain’s disease, granulomatous tophaceous gout, non-specific synovitis or rheumatoid arthritis.
Treatment
Treatment was initiated with four drugs (rifampicine, ethambutol, isoniazide and pyrazinamide) for 2 months followed by rifampicine and isoniazide for 10 months.
Outcome and follow-up
Tenosynovitis healed 6 months after initiation of antitubercular treatment.
Discussion
Tubercular tenosynovitis is rare and essentially affects the upper limbs. It targets selectively the wrist and the hand.2 The mechanism of infection can be haematogenous from a pleuropulmonary or genitourinary tuberculosis or direct inoculation from adjacent bone or joint infection. Common risk factors include previous trauma, corticosteroid injections, age higher than 60 years, low socioeconomic status, alcoholism and immunosupression.3 4 However, in our patient, no risk factors were found. The diagnosis can be easily delayed because of non-specificity of clinical signs. Patients may present with a painful swelling along the inflamed tendon, a carpel tunnel syndrome and a non-specific synovitis mimicking De Quervain’s disease or granulomatous tophaceous gout.5 6 Tendon rupture is rare but may occur when treatment is delayed. Laboratory findings are generally negative except the increasing of erythrocyte sedimentation rate and C reactive protein.7 Diagnosis is often established after culture of mycobacterium from surgical biopsies or tenosynovectomies because direct microscopic examinations are often negative, as in our patient. Molecular biology techniques can also be used to detect and identify the main species of mycobacteria. The most effective treatment includes surgical debridement with excision of the necrotic synovium, early postoperative mobilisation and the use of antituberculous drug. Medical treatment involves a combination of four drugs: rifampicine, isoniazide, pyrazimamide and ethambutol, during 2 months, followed by bitherapy. The recommended duration of treatment is generally between 9 and 12 months.8 The total duration of antituberculous therapy was 12 months in our patient with a favourable evolution. It is very important that patients recover a full range of motion as soon as possible.
Learning points.
-
▶
Tuberculous tenosynovitis of the extensor tendons should be kept in mind in patients with chronic or recurrent tenosynovitis of the extensor of the wrist.
-
▶
This diagnosis can be easily delayed because of non-specificity of clinical signs.
-
▶
Early excision of the infected tissues combined with antituberculous drug therapy gives good functional results.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Toyokawa N, Kokubu T, Fujioka H. Mycobacterial tuberculous tenosynovitis of the extensor tendon occurring after liver transplantation: a case report. Hand Surg 2008;13:37–40 [DOI] [PubMed] [Google Scholar]
- 2.Hristea A, Luka AI, Oancea I, et al. Isolated tuberculous tenosynovitis of the forearm in an immunocompetent patient. Chirurgia (Bucur) 2010;105:427–30 [PubMed] [Google Scholar]
- 3.Lall H, Nag SK, Jain VK, et al. Tuberculous extensor tenosynovitis of the wrist with extensor pollicis longus rupture: a case report. J Med Case Reports 2009;3:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le Meur A, Arvieux C, Guggenbuhl P, et al. Tenosynovitis of the wrist due to resistant Mycobacterium tuberculosis in a heart transplant patient. J Clin Microbiol 2005;43:988–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaovisidha S, Chen C, Ryu KN, et al. Tuberculous tenosynovitis and bursitis: imaging findings in 21 cases. Radiology 1996;201:507–13 [DOI] [PubMed] [Google Scholar]
- 6.Amine B, Benbouazza K, Bahiri R, et al. Multifocal tuberculous tenosynovitis. Joint Bone Spine 2006;73:474–5 [DOI] [PubMed] [Google Scholar]
- 7.Albornoz MA, Mezgarzedeh M, Neumann CH, et al. Granulomatous tenosynovitis: a rare musculoskeletal manifestation of tuberculosis. Clin Rheumatol 1998;17:166–9 [DOI] [PubMed] [Google Scholar]
- 8.Aboudola S, Sienko A, Carey RB, et al. Tuberculous tenosynovitis. Hum Pathol 2004;35:1044–6 [DOI] [PubMed] [Google Scholar]


