Abstract
The authors present a case of spontaneous adrenal haemorrhage, in a 28-year-old woman at 36 weeks of a twin pregnancy. Initial symptom was sudden onset chest pain which soon migrated to abdomen, accompanied by hypovolaemic shock and fetal bradycardia. Subsequent caesarean section for suspected placental abruption and resuscitation with nine units of blood, 10 of cryoprecipitate, four of fresh frozen plasma and two of platelets, in order to treat anaemia of Hgb of 3.6 g/dl and disseminated intravascular coagulation, failed to stabilise the woman. A CT scan of abdomen and pelvis then revealed a 15×17×17 cm retroperitoneal haematoma, secondary to right adrenal haemorrhage. Management was with laparotomy drainage and packing of the retroperitoneal haematoma along with the use of activated factor VII. Adrenal haemorrhage in pregnancy is an extremely rare, acute, life-threatening condition, presenting with non-specific symptoms.
Background
Adrenal haemorrhage has been reported in 0.3%–1.8% of unselected cases in autopsy studies, and its overall mortality is 15%.1 2 The incidence in pregnancy is unknown. Non-specific presentation can lead to diagnostic confusion and catastrophic delays. Diagnosis is usually made by abdominal CT, intraoperatively, rarely clinical, and on autopsy.
Our personal experience from the case indicates that awareness of the condition’s presentation and course is the only way to raise the suspicion of it, in the acute clinical setting. By sharing this case, we aim not only to provide knowledge, but to give an insight of how this condition can rapidly evolve.
Case presentation
A 28-year-old primigravida, at 36+3 weeks gestation of an uncomplicated monochorionic diamniotic pregnancy, presented with acute onset right-sided chest pain. The patient was afebrile, pulse rate was 107 beats per min (bpm), blood pressure (BP), 122/77 mm Hg, tachypnoic of 20 breaths per min with oxygen saturation 99% on air. The fetal heart rate was normal for both of the twins.
Clinical examination of respiratory and cardiovascular systems was normal. The abdomen and uterus found soft, non-tender and no vaginal bleeding or discharge was present. Previous medical history was unremarkable, and no history of recent trauma or febrile illness mentioned. Regular antenatal follow-up was uneventful, and an ultrasound scan for fetal growth and umbilical artery Doppler study 3 days earlier, were normal.
Suspicion of pulmonary embolism, lead to initial investigation with an ECG, which revealed sinus tachycardia of 120 bpm and arterial blood gases showed Ph 7.548, PO2 16.5kPa, PCO2 2.55Kpa, base excess-3.9 meq/l and haemoglobin of 11.5 g/dl. With the pain migrating to the right flank and without further chest symptoms, obstetric input was sought.
During the obstetric review, right abdominal flank tenderness along with the complaint of dysouria suggested upper urinary tract pathology, and urinalysis with microscopy was requested.
At 90 min from presentation, an episode of orthostatic hypotension, BP of 68/47 mm Hg and pulse rate at 135 bpm, accompanied by fetal bradycardia of 85 bpm for the second twin. Although maternal BP recovered after resuscitation with 500 ml of colloid intravenous infusion, fetal bradycardia for both twins this time persisted and deteriorated to 55 bpm.
An emergency caesarean section under general anaesthetic was then performed for suspected concealed placenta abruption. Intraoperative findings of a bluish uterine surface, blood filled uterine cavity with separated placentas and uterine atony, supported the clinical suspicion of placental abruption, though no obvious retroplacental clot was identified.
Twin one weighed 2300 g, had apgar scores of 1 at 1 min, 3 at 5 min and 6 at 10 min, while the cord blood gases showed pH arterial 6.605, pH venous 6.746 and base excess of,-2.8 meq/l. Twin two weighed 2500 g and had apgar scores of 1 at 1 min, 3 at 5 min and 4 at 10 min, while the cord blood gases were not recorded. Both twins admitted to neonatal intensive care unit for further resuscitation.
Uterine tone recovered after massage and 20 units of intravenous syntocinon and 500 mcg of intramuscular ergometrine. Adequate haemostasis ensured before closure, and the estimated blood loss reached 2.5 l. Intraoperative haemoglobin estimate via haemacue was 5.2 mg/dl and immediate transfusion with two units of O negative blood commenced.
The preoperative blood count results then became available and revealed haemoglobin of 3.6 g/dl, platelets 44×109199/l, activated partial thromboplastin time (APTT) 51.9 s and fibrinogen 0.9 g/l. Liver and renal function tests were normal.
At 3 h from initial presentation, the patient transferred to labour ward high dependency unit with the diagnosis of disseminated intravascular coagulation (DIC). Further joint management by haematologist, anaesthetist and obstetrician included transfusion of a total of nine units of blood, 10 units of cryoprecipitate, four units of fresh frozen plasma and two units of platelets.
At 6 h from presentation and despite blood products and fluid resuscitation, the patient was persistently tachycardic of 120 bpm, and had right upper quadrant pain. Examination revealed tenderness of the right upper quadrant and a palpable mass considered to be liver edge, two finger breadths below the costal margin. In view of the recent suspected abruption and subsequent DIC, a subcapsular hepatic haematoma was suspected and urgent CT of the abdomen and pelvis requested.
Prior to imaging, patient stabilised at intensive care unit with further two units of blood. DIC had been corrected with fibrinogen levels at 2 g/l, APTT 30.6 s, prothrombin time 8.9 s and platelet count at 64×109/l.
Investigations
A CT scan of the abdomen and pelvis revealed a 15×17×17 cm retroperitoneal haematoma extending from the right kidney to the liver, secondary to right adrenal haemorrhage (figure 1A–D). The radiologist suggested adrenal artery embolisation, but such facility was not available onsite, and hence patient was unstable for transfer, a decision for laparotomy made, and activated factor VII was given preoperatively.
Figure 1.
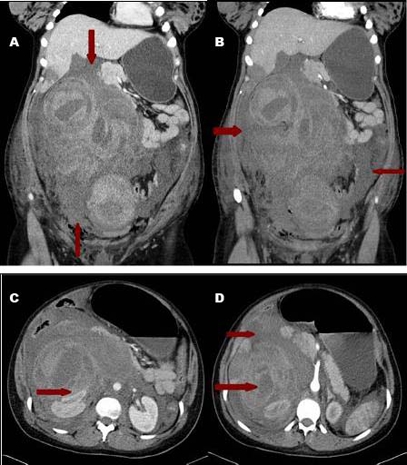
(A) Right suprarenal gland. (B) Right retro-peritoneal haematoma. (C, D) Extent of retro-peritoneal haematoma.
Placental histology confirmed prominent peri-villous fibrin deposition of questionable significance, without presence of haemosiderin or thrombi.
Differential diagnosis
During the course of the case, symptoms and signs constantly changed and the differentials considered were pulmonary embolism, upper urinary tract pathology, placental abruption, subcapsular liver haematoma and finally adrenal haemorrhage.
Treatment
At 14 h from presentation, exploration with midline laparotomy and drainage of a massive right-sided retroperitoneal haematoma took place. The right adrenal gland was fragmented with no active arterial bleeding but venous ooze. The retroperitoneal space was packed. Further, activated factor VII was given and the patient transferred to ICU where she stayed intubated for the next 72 h.
Activated factor VII, transfusion of blood and dexamethazone were given before the laparotomy and pack removal from retroperitoneal space, 3 days later.
Outcome and follow-up
Patient was discharged on day 13 and both of the neonates were discharged in good health.
Discussion
The sequence of events is unclear. The mechanism we suggest is that triggering event was that of the spontaneous right adrenal haemorrhage due to adrenal vascular rupture. The endothelial injury along with the local activation of coagulation, consumed platelets and coagulation factors in the retroperitoneal haemorrhage. The placental separation was the result and not the cause of the severe consumptive coagulopathy, hence there was no histological evidence of placental thrombus.
Another possibility is that of a pre-existing adrenal artery aneurism that ruptured in pregnancy, since more than 50% of aneurisms in young women rupture during pregnancy or puerperium.3
Spontaneous adrenal haemorrhage is found in approximately 11% of all adrenal haemorrhages and is usually unilateral, and presents with sudden onset abdominal, flank pain.2
Causes of adrenal haemorrhage include mainly sepsis, DIC, lupus anticoagulant and antiphospholipid antibodies, postoperative period, trauma and anticoagulation.
Pregnancy related conditions that could increase the risk for mostly bilateral adrenal rupture are pre-eclampsia, spontaneous abortion, antepartum or postpartum haemorrhage. Uncomplicated pregnancy is rarely associated with non-traumatic, unilateral adrenal haemorrhage.4
A mechanism for spontaneous rupture could be explained by the unique blood supply of the adrenal gland. The adrenal gland is supplied by three arteries which divide into 50 to 60 branches, the capillary plexus of which drain into medullary sinusoids which forms the single central adrenal vein. The flow to peripheral adrenal vein is turbulent. In pregnancy there is an increase of adrenocorticotropic hormone and subsequently adrenal volume and vascular supply, as well as a hypercoagulative status.
The increased and turbulent adrenal blood flow, hypercoagulative state and slowed venous return to vena cava due to increased pressure from the gravid uterus, may all predispose to spontaneous adrenal vein thrombosis and subsequent adrenal rupture and haemorrhage.5
Learning points.
-
▶
Although the clinical presentation has no specific diagnostic characteristics, one should consider spontaneous adrenal haemorrhage in patients who presents with upper abdominal or flank pain and signs of shock.
-
▶
Management is multidisciplinary, diagnosis is established with CT abdomen, and optimum therapeutic approach is that of adrenal artery embolisation.6
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Arnold G, Richer AG, Lepore JJ. Suprarenal hemorrhage in pregnancy; report of a case with a review of the literature. N Engl J Med 1949;240:1040–3 [DOI] [PubMed] [Google Scholar]
- 2.Tritos NA. Adrenal Hemorrhage. E Medicine 2007. http://emedicine.medscape.com/article/126806-overview (accessed 13 July 2011). [Google Scholar]
- 3.Nolte JE, Rutherford RB, Nawaz S, et al. Arterial dissections associated with pregnancy. J Vasc Surg 1995;21:515–20 [DOI] [PubMed] [Google Scholar]
- 4.Vella A, Nippoldt TB, Morris JC., 3rd Adrenal hemorrhage: a 25-year experience at the Mayo Clinic. Mayo Clin Proc 2001;76:161–8 [DOI] [PubMed] [Google Scholar]
- 5.Gavrilova-Jordan L, Edmister WB, Farrell MA, et al. Spontaneous adrenal haemorrhage during pregnancy: a review of the literature and a case report. Obstet Gynecol Surv 2005;60:191–5 [DOI] [PubMed] [Google Scholar]
- 6.Christie J, Batool I, Moss J, et al. Adrenal artery rupture in pregnancy. BJOG 2004;111:185–7 [DOI] [PubMed] [Google Scholar]


