Abstract
Objective
To examine whether health status and obesity prevalence differ by race or ethnicity and health care workforce category.
Methods
Data representing US health care workers aged 20 to 64 between 1982 and 2004 were retrieved from the Integrated Health Interview Series. Trends, as well as disparities, in health status and obesity are examined by workforce category using logistic regression.
Results
Self-reported health status of health care workers has declined over time and the prevalence of obesity is rising. Moreover, there is a clear social gradient across workforce categories, which is widening over time. Within workforce categories, there are significant racial disparities in health status and prevalence of obesity.
Conclusions
Health of health care workers needs to be taken into account when setting policies intended to increase access to health care and create a healthy diverse workforce.
Substantial health disparities have been documented for the general US population, with numerous studies showing racial or ethnic disparities in health status, health behaviors, and mortality.1–7 Yet there is a dearth of research on health disparities among health care providers. One recent study calculated morbidity rankings for over 200 occupations. The authors found that several of the more prestigious health professions (eg, physicians, dentists, pharmacists) were among the lowest in morbidity ranking, whereas nurse aids and licensed practical nurses were among the 10 highest morbidity rankings.8 However, little is known about racial disparities in health within the health care workforce. Given the importance of the health care workforce to a healthy population, there may be additional cause for concern if health disparities among health care workers mirror that of the general population.
Changes in technology, increasingly complicated disease management, and an aging population have all contributed to a significant growth in the demand for health care services.9–11 This rapid and persistent rise in the demand for health services has outpaced the supply of health care workers, leading to a significant health care workforce shortage. Moreover, these unfilled positions have resulted in an increase in the current health care workers’ workload. For example, Bhargavan and Sunshine12 found that the average radiologist’s annual clinical workload has increased by around 13% from 1995–1996 to 1998–1999. Other studies have found that the increased workload for health care workers generates burnout and stress, which in turn may harm the health and well-being of health care workers.13,14
Frontline health care workers face a wide range of hazards on their job, including stress, needle stick injuries, and back injuries.15–18 Providing medical care often includes continuous care for patients. Thus, many health care workers are required to have rotating shift work in their jobs, which has been associated with specific disorders such as peptic ulcer disease, coronary heart disease, and compromised pregnancy outcome.19 Kawachi et al20 found that nurses who worked rotating night shifts for as few as 6 years had an increased risk of coronary heart disease. Likewise, Schernhammer et al21,22 found modest increases in colorectal cancer and breast cancer to be associated with nurses who worked rotating night shifts.
Studies of the health care work-force have focused on demand and supply of health professionals, while research examining disparities in the health of health care workers and the implications for workforce diversity and workforce shortage is limited. To address the gap in the literature on health disparities among health care workers, we used 23 years of data from a nationally representative US sample to analyze the health of health care workers. Our primary objective was to examine whether the health of health care providers had changed over time. Secondarily, we assessed health disparities among health care providers by examining the extent to which self-reported health status and prevalence of obesity differ across health care professions and by race or ethnicity.
Materials and Methods
Data Source and Sample
We used cross-sectional survey data for adults aged 20 to 64 who reported employment in a health care profession to examine health disparities among health care workers. Our data were retrieved from the Integrated Health Interview Series (IHIS), a cross-sectional time series of harmonized National Health Interview Survey (NHIS) data.23 All variables except occupation were retrieved from IHIS. The occupation variable was obtained from the original NHIS public use files and linked with the IHIS variables using the unique person identifiers available in the original NHIS files. The sample for our study was adults between the ages of 20 and 64 years employed in health care professions in the United States between 1982 and 2004. We excluded respondents who did not report their occupation, who were other than Asian, Black, Hispanic, or White, or who had incomplete data on height and weight. The final unweighted sample size was 49,216 persons.
Measures
The outcomes of interest were self-reported excellent health status and obesity. Self-reported health status was consistently measured on a five-point scale, which we dichotomized into “excellent” (excellent) and “non excellent” (very good, good, fair, poor, or missing). To define obesity, we calculated body mass index (BMI) from subjects’ self-reported height and weight using the formula (weight (lb)/[height (in)]2 × 703).24 According to the Center for Disease Control and Prevention, obesity is defined as a BMI greater than 30. Using the BMI calculation, we created a dichotomous indicator variable to classify subjects as obese or nonobese.
Health care workforce categories were defined based on respondents’ main occupation during the week before interview, which had been recoded consistent with the Standard occupational classification system. There were two occupation recode variables in the NHIS representing a detailed recode (available 1982–1994) and a simple recode (available 1982–2004). For example, occupations in the detailed recode included separate codes for physician, pharmacist, dentist, nurse, and occupational therapist. The simple recode for health care occupations represented broad categories of health diagnosing professions, health assessing and treating occupations, health technologists and technicians, and health service workers. Because the detailed codes were not available for all years in our study, we recoded the detailed categories into these broad categories for use in analysis. Health diagnosing professions included physicians, dentists, optometrists, and podiatrists; health assessing and treating occupations consist of registered nurses, pharmacists, dietitians, and therapists; health technologists and technicians include clinical laboratory technologists and technicians, dental hygienists, health record technologists and technicians, radiological technicians, and licensed practical nurses; and health service workers are dental assistants, health aides, nursing aides, orderlies, and attendants. Detailed standard occupational classification code and corresponding health occupations are in Table 1.
TABLE 1.
Standard Occupational Classification (SOC) Code and Corresponding Health Occupations
| Occupation Title | 1990 SOC Code | Occupation |
|---|---|---|
| Health diagnosing occupations | 084 | Physicians |
| 085 | Dentists | |
| 086 | Veterinarians | |
| 087 | Optometrists | |
| 088 | Podiatrists | |
| 089 | Health diagnosing practitioners, n.e.c. | |
| Health assessing and treating occupations | 095 | Registered nurses |
| 096 | Pharmacists | |
| 097 | Dietitians | |
| 098 | Respiratory therapists | |
| 099 | Occupational therapists | |
| 103 | Physical therapists | |
| 104 | Speech therapists | |
| 105 | Therapists, n.e.c. | |
| 106 | Physicians’ assistants | |
| Health technologists and technicians | 203 | Clinical laboratory technologists and technicians |
| 204 | Dental hygienists | |
| 205 | Health record technologists and technicians | |
| 206 | Radiologic technicians | |
| 207 | Licensed practical nurses | |
| 208 | Health technologists and technicians, n.e.c. | |
| Health service | 445 | Dental assistants |
| 446 | Health aides, except nursing | |
| 447 | Nursing aides, orderlies, and attendants |
N.e.c. indicates not elsewhere classified.
Additional covariates were defined as follows. Race was a set of indicator variables for self-reported Asian, non-Hispanic Black, Hispanic, and non-Hispanic White. Age is categorized in three groups as 20 to 34 years, 35 to 49 years and 50 to 64 years. Educational attainment was classified as a college degree or not. Marital status was defined as married or not.
Analytic Methods
Our analytic approach consisted of three steps. First, we examined the extent to which the four health care worker categories differed in background characteristics potentially associated with health status using cross tabulations and design-based F-tests to account for the complex sample design. We then examined the overall relationship between health care workforce category and each of the two health status indicator variables (excellent health and obesity) using logistic regression models adjusted for race, age, gender, marital status, education, and year to determine whether occupational status was associated with health. To visually examine the trends in the health of health care providers over time, we interacted year with health care worker category (allowing the trends to vary by category) and produced graphs of the predicted probabilities of the outcome for each group over time. Finally, we stratified by occupational category to examine whether racial disparities in health exist within each of the health care workforce categories. For each occupational class, we estimated adjusted odds ratios for each race group with separate logistic regression models for the two health indicators adjusted for age, gender, marital status, education, and year. We then interacted year with race group and graphed the predicted probabilities for race groups within each health care workforce category.
Analyses were conducted using Stata statistical software (SE version 9.2), which produces unbiased estimates from data collected through complex sampling designs.25,26 The survey commands available in Stata properly account for the unequal probabilities of selection and the stratified or clustered sampling design of the NHIS data. Variance estimates were produced using Taylor series linearization.
Results
Sample Characteristics
Table 2 presents characteristics of the study population as a whole and by health care workforce category. Among all US health care workers aged 20 to 64 between 1982 and 2004, the majority are women (79%), White (75%), married (65%), and college educated (72%). Over one-third of all health care workers are classified in health assessing and treating occupations (38%) and nearly one-third of health care workers are classified as health services workers (29%).
TABLE 2.
Characteristics of US Health Professionals Aged 20 to 64 yr by Health Care Worker Category, 1982–2004
| Total | Health Diagnosing | Health Assessing | Health Technician | Health Service | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. population (Millions) | 154.6 | 18.0 | 58.6 | 33.0 | 45.0 | ||||||
| No. observations | 49,216 | 5430 | 18,106 | 10,421 | 15,259 | ||||||
| Rate (%) | SE (%) | Rate (%) | SE (%) | Rate (%) | SE (%) | Rate (%) | SE (%) | Rate (%) | SE (%) | P value | |
| Age | |||||||||||
| 20–34 yr old | 40 | 0.31 | 29 | 0.91 | 36 | 0.47 | 44 | 0.65 | 45 | 0.50 | 30.001 |
| 35–49 yr old | 41 | 0.29 | 48 | 0.90 | 45 | 0.49 | 41 | 0.60 | 35 | 0.48 | |
| 50–64 yr old | 19 | 0.23 | 23 | 0.74 | 19 | 0.38 | 15 | 0.47 | 20 | 0.42 | |
| Gender | |||||||||||
| Male | 21 | 0.27 | 77 | 0.70 | 13 | 0.32 | 19 | 0.54 | 10 | 0.34 | 30.001 |
| Female | 79 | 0.27 | 23 | 0.70 | 87 | 0.32 | 81 | 0.54 | 90 | 0.34 | |
| Race | |||||||||||
| Asian | 4 | 0.14 | 7 | 0.50 | 4 | 0.22 | 4 | 0.27 | 2 | 0.19 | 30.001 |
| Black | 15 | 0.34 | 4 | 0.36 | 9 | 0.31 | 14 | 0.48 | 28 | 0.68 | |
| Hispanic | 6 | 0.18 | 5 | 0.40 | 4 | 0.18 | 7 | 0.30 | 10 | 0.36 | |
| White | 75 | 0.40 | 84 | 0.70 | 83 | 0.43 | 75 | 0.62 | 60 | 0.72 | |
| Marital status | |||||||||||
| Married | 65 | 0.33 | 80 | 0.67 | 70 | 0.49 | 63 | 0.66 | 54 | 0.58 | 30.001 |
| Not married | 35 | 0.33 | 20 | 0.67 | 30 | 0.49 | 37 | 0.66 | 46 | 0.58 | |
| Education | |||||||||||
| College degree | 72 | 0.34 | 98 | 0.18 | 92 | 0.24 | 73 | 0.54 | 35 | 0.56 | 30.001 |
| No college degree | 28 | 0.34 | 2 | 0.18 | 8 | 0.24 | 27 | 0.54 | 65 | 0.56 | |
| Health status | |||||||||||
| Excellent | 42 | 0.33 | 67 | 0.82 | 46 | 0.49 | 39 | 0.62 | 28 | 0.47 | 30.001 |
| Non-excellent | 58 | 0.33 | 33 | 0.82 | 54 | 0.49 | 61 | 0.62 | 72 | 0.47 | |
| BMI | |||||||||||
| Underweight | 3 | 0.08 | 1 | 0.18 | 3 | 0.14 | 3 | 0.18 | 3 | 0.16 | 30.001 |
| Healthy weight | 52 | 0.32 | 55 | 0.85 | 58 | 0.48 | 52 | 0.64 | 44 | 0.58 | |
| Overweight | 28 | 0.27 | 36 | 0.85 | 25 | 0.41 | 28 | 0.61 | 28 | 0.47 | |
| Obese | 17 | 0.27 | 8 | 0.49 | 14 | 0.38 | 17 | 0.48 | 25 | 0.50 | |
| Occupation | |||||||||||
| Health diagnosing | 12 | 0.23 | |||||||||
| Health assessing | 38 | 0.32 | |||||||||
| Health technician | 21 | 0.25 | |||||||||
| Health services | 29 | 0.33 | |||||||||
There is a clear social gradient across health care workforce categories (see Table 2) with the highest status category (health diagnosing professions) being predominantly older, male, married, and college educated. Health care workers in health assessing and treating, health technician, and health services categories are mostly women (87%, 81%, and 90%, respectively). In contrast, women are less likely to work in health diagnosing occupations (23%). Differences in racial composition are also evident across the four categories of health care workers (P < 0.001). For example, Blacks make up 15% of the health care workforce, but they are underrepresented in health diagnosing professions (4%) and overrepresented in health service work (28%).
Health disparities are also apparent among health care workers. Overall, 42% of health care workers report excellent health. Across health care worker categories, 67% of those in health diagnosing professions report excellent health compared to 46% of those in health assessing professions, 39% of health technicians, and only 28% of health service workers (P < 0.001). In terms of obesity, overall 17% of health care workers are obese. Yet, the prevalence of obesity among health services workers is nearly three times higher compared with health diagnosing occupations (25% vs 8%, respectively; P < 0.001).
Self-Reported Health Status
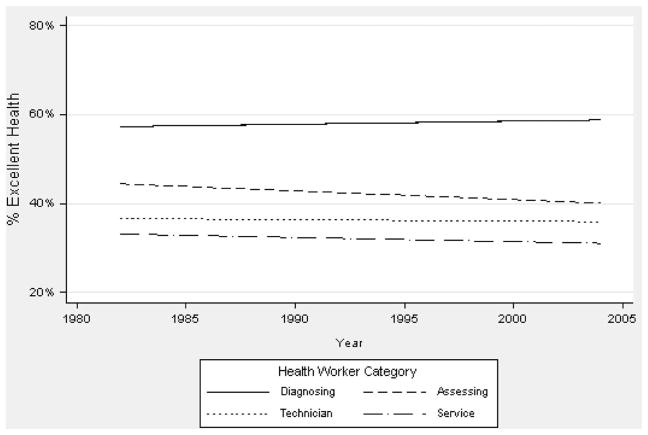
Table 3 presents the results of a series of logistic regression models estimating the odds of reporting excellent health among US health care workers. Model 1 indicates that after adjusting for age, sex, race, marital status, education, obesity, and year, people working in health assessing (OR = 0.52; 95% CI = 0.48 to 0.57), health technician (OR = 0.41; 95% CI = 0.37 to 0.45), and health services (OR = 0.34; 95% CI = 0.31 to 0.37) occupations, are significantly less likely to report excellent health than those working in health diagnosing professions. The overall proportion of workers reporting excellent health has declined over time (P = 0.043). Figure 1 graphically depicts the trend in self-reported excellent for health care worker categories over time.
TABLE 3.
Odds of Reporting Excellent Health by Workforce Category Among US Health Care Workers Aged 20 to 64 yr, 1982–2004
| Model 1: All OR (95% CI) |
Model 2: Health Diagnosing OR (95% CI) |
Model 3: Health Assessing OR (95% CI) |
Model 4: Health Technician OR (95% CI) |
Model 5: Health Service OR (95% CI) |
|
|---|---|---|---|---|---|
| Category of health workers | |||||
| Health diagnosing | 1.00 | ||||
| Health assessing | 0.52 (0.48–0.57)*** | ||||
| Health technician | 0.41 (0.37–0.45)*** | ||||
| Health service | 0.34 (0.31–0.37)*** | ||||
| Race/ethnicity | |||||
| Asian | 0.78 (0.69–0.89)*** | 0.62 (0.48–0.81)*** | 0.71 (0.59–0.85)*** | 0.84 (0.61–1.16) | 1.27 (0.94–1.71) |
| Black | 0.78 (0.72–0.84)*** | 0.65 (0.46–0.91)* | 0.65 (0.57–0.74)*** | 0.68 (0.59–0.78)*** | 0.96 (0.86–1.08) |
| Hispanic | 0.89 (0.81–0.98)* | 0.90 (0.67–1.19) | 0.81 (0.67–0.97)** | 0.97 (0.79–1.18) | 0.95 (0.82–1.11) |
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Obesity | |||||
| Obese | 0.43 (0.40–0.47)*** | 0.35 (0.26–0.47)*** | 0.38 (0.33–0.43)*** | 0.44 (0.38–0.52)*** | 0.52 (0.46–0.59)*** |
| Not obese | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Gender | |||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Male | 1.36 (1.27–1.46)*** | 1.60 (1.32–1.94)*** | 1.34 (1.18–1.51)*** | 1.32 (1.15–1.51)*** | 1.27 (1.10–1.46)*** |
| Age | |||||
| 20–34 yr old | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 35–49 yr old | 0.78 (0.74–0.82)*** | 0.65 (0.55–0.79)*** | 0.84 (0.78–0.91)*** | 0.77 (0.69–0.86)*** | 0.72 (0.66–0.80)*** |
| 50–64 yr old | 0.50 (0.47–0.54)*** | 0.43 (0.35–0.53)*** | 0.51 (0.46–0.57)*** | 0.49 (0.41–0.58)*** | 0.52 (0.46–0.60)*** |
| Marital status | |||||
| Married | 1.03 (0.98–1.09) | 1.11 (0.92–1.32) | 1.03 (0.95–1.12) | 1.04 (0.93–1.18) | 1.00 (0.90–1.10) |
| Not married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Education | |||||
| College degree | 1.56 (1.46–1.66)*** | 2.49 (1.53–4.04)*** | 1.54 (1.37–1.74)*** | 1.52 (1.35–1.71)*** | 1.56 (1.41–1.72)*** |
| No college degree | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Year | 1.00 (0.99–1.00)* | 1.01 (0.99–1.02) | 0.99 (0.99–1.00)* | 1.00 (0.99–1.01) | 0.99 (0.99–1.00) |
| Observations | 49,216 | 5,430 | 18,106 | 10,421 | 15,259 |
P < 0.05,
P < 0.01,
P < 0.001.
Fig. 1.
Predicted probability of self-reported excellent health by workforce category over time among US workers aged 20 to 64 years, 1982–2004.
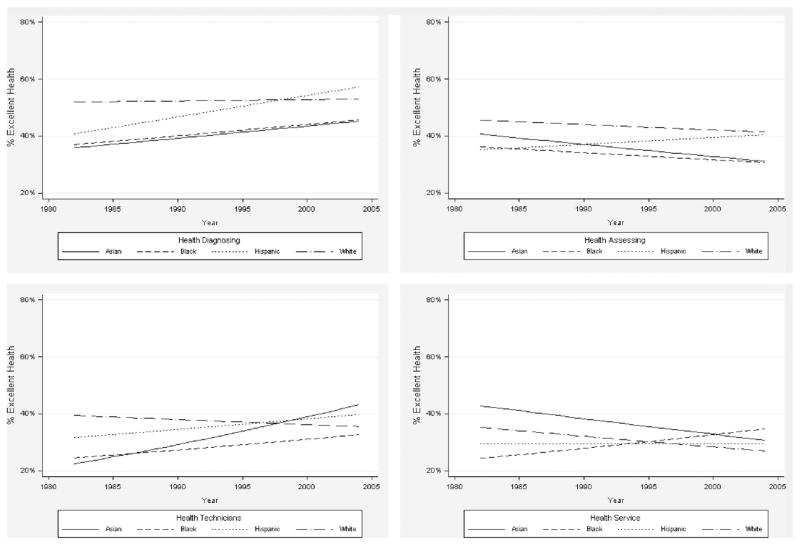
When stratifying by workforce category, there are significant racial disparities, which differ by work-force category. Among the health diagnosing professions (model 2), only Asians (OR = 0.62; 95% CI = 0.48 to 0.81) and Blacks (OR = 0.65; 95% CI = 0.46 to 0.91) are significantly less likely to report excellent health than Whites, whereas Hispanics are not significantly different. Asians (OR = 0.71; 95% CI = 0.59 to 0.85), Blacks (OR = 0.65; 95% CI = 0.57 to 0.74), and Hispanics (OR = 0.81; 95% CI = 0.67 to 0.97) are less likely to report excellent health than Whites among the health assessing professions (model 3). Only Blacks (OR = 0.68; 95% CI = 0.59 to 0.78) are significantly different from Whites in reporting excellent health among health technicians (model 4). However, there are no significant differences in reporting excellent health by race among health service workers (model 5). Figure 2 presents the predicted probabilities of reporting excellent health by race within each health care workforce category over time.
Fig. 2.
Predicted probability of reporting excellent health by race within health care workforce categories among US health care workers aged 20 to 64 years, 1982–2004.
Obesity
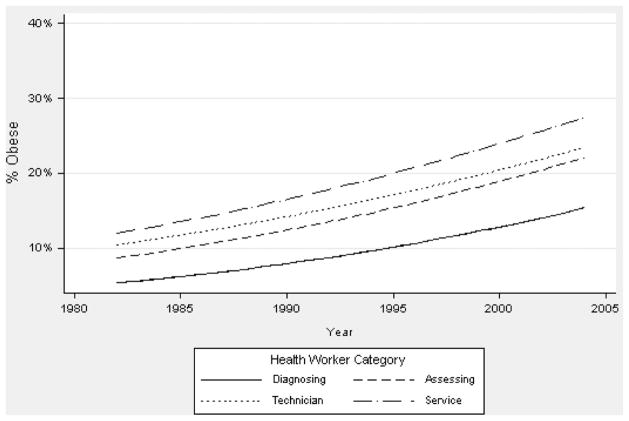
Table 4 presents the results of a series of logistic regression models estimating the odds of obesity among US health care workers. Model 6 indicates that after adjusting for age, sex, race, marital status, health status, education, and year people working in health assessing (OR = 1.60; 95% CI = 1.35 to 1.90), health technician (OR = 1.82; 95% CI = 1.53 to 2.16), and health services (OR = 2.20; 95% CI = 1.84 to 2.63) occupations are more likely to be obese than people working in health diagnosing professions. The probability of obesity among all workers has increased significantly over time (OR = 1.05; 95% CI = 1.04 to 1.05). Figure 3 graphically depicts the trend in obesity by showing predicted probabilities of obesity for health care worker categories over time.
TABLE 4.
Odds of Obesity by Workforce Category Among US Health Care Workers Aged 20 to 64 yr, 1982–2004
| Model 6: All OR (95% CI) |
Model 7: Health Diagnosing OR (95% CI) |
Model 8: Health Assessing OR (95% CI) |
Model 9: Health Technician OR (95% CI) |
Model 10: Health Service OR (95% CI) |
|
|---|---|---|---|---|---|
| Category of health workers | |||||
| Health diagnosing | 1.00 | ||||
| Health assessing | 1.60 (1.35–1.90)*** | ||||
| Health technician | 1.82 (1.53–2.16)*** | ||||
| Health service | 2.20 (1.84–2.63)*** | ||||
| Race/ethnicity | |||||
| Asian | 0.32 (0.23–0.47)*** | 0.22 (0.08–0.56)*** | 0.40 (0.24–0.67)*** | 0.16 (0.09–0.30)*** | 0.39 (0.19–0.80)*** |
| Black | 1.88 (1.72–2.04)*** | 0.65 (0.31–1.33) | 1.88 (1.61–2.20)*** | 1.54 (1.30–1.82)*** | 2.11 (1.88–2.38)*** |
| Hispanic | 1.18 (1.06–1.33)*** | 1.24 (0.70–2.20) | 0.98 (0.76–1.27) | 1.50 (1.20–1.88)*** | 1.16 (1.00–1.35)* |
| White | 1.00 | ||||
| Health status | |||||
| Excellent health | 0.43 (0.40–0.47)*** | 0.35 (0.26–0.47)*** | 0.38 (0.33–0.43)*** | 0.45 (0.38–0.52)*** | 0.52 (0.46–0.59)*** |
| Not excellent health | 1.00 | ||||
| Gender | |||||
| Female | 1.00 | ||||
| Male | 0.96 (0.86–1.06) | 1.34 (0.92–1.96) | 1.17 (0.97–1.41) | 0.87 (0.72–1.05) | 0.73 (0.60–0.90)*** |
| Age | |||||
| 20–34 yr old | 1.00 | ||||
| 35–49 yr old | 1.57 (1.46–1.69)*** | 1.16 (0.78–1.73) | 1.70 (1.48–1.95)*** | 1.61 (1.38–1.86)*** | 1.50 (1.33–1.68)*** |
| 50–64 yr old | 1.71 (1.56–1.87)*** | 0.96 (0.61–1.52) | 1.98 (1.67–2.35)*** | 1.71 (1.41–2.08)*** | 1.59 (1.39–1.83)*** |
| Marital status | |||||
| Married | 0.88 (0.82–0.94)*** | 0.97 (0.69–1.36) | 0.74 (0.66–0.84)*** | 0.84 (0.73–0.96)* | 1.02 (0.92–1.12) |
| Not married | 1.00 | ||||
| Education | |||||
| College degree | 0.82 (0.75–0.89)*** | 2.39 (0.82–7.02) | 0.80 (0.67–0.95)* | 0.74 (0.64–0.86)*** | 0.88 (0.79–0.99)* |
| No college degree | 1.00 | ||||
| Year | 1.05 (1.04–1.05)*** | 1.06 (1.03–1.08)*** | 1.05 (1.04–1.06)*** | 1.05 (1.03–1.06)*** | 1.05 (1.04–1.06)*** |
| Observations | 49,216 | 5430 | 18,106 | 10,421 | 15,259 |
P < 0.05,
P < 0.01,
P < 0.001.
Fig. 3.
Predicted probability of obesity by workforce category over time among US workers aged 20 to 64 years, 1982–2004.
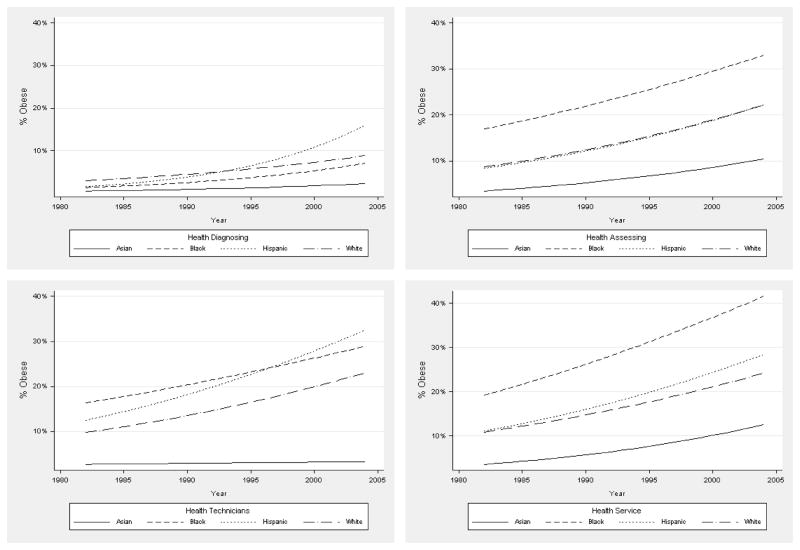
After stratifying by workforce category, racial disparities are evident within all four categories of health care workers, especially for health technicians (model 9) and health service workers (model 10). For example, in the health technician group, Asians (OR = 0.16; 95% CI = 0.09 to 0.30) are significantly less likely to be obese than Whites. However, Blacks (OR = 1.54; 95% CI = 1.30 to 1.82) and Hispanics (OR = 1.50; 95% CI = 1.20 to 1.88) are significantly more likely to be obese when compared with Whites. Among the health diagnosing professions, there are few significant differences in the odds of obesity by race (model 7). Specifically, only Asians are significantly different than Whites, having 0.22 the odds of being obese (95% CI = 0.08 to 0.56). Figure 4 presents the predicted probabilities of obesity by race group within each health care workforce category over time.
Fig. 4.
Predicted probability of obesity by race within health care workforce categories among US health care workers aged 20 to 64 years, 1982–2004.
Discussion
Our study examines the trend in two indicators of health as well as disparities in health among health care workers by examining self-reported health status and obesity across categories of health care professions and by race or ethnicity within health care worker categories over time. The analyses of health care workers from 1982 to 2004 provide several important findings.
First, the results indicate that the health of health care workers has declined from 1982 to 2004. For example, the self-reported excellent health status of health care workers has declined over the decades. Among health care workers, those employed in health diagnosing professions appear to have better health than other health care workers. One reason may be that socioeconomic status (SES) among those employed in health diagnosing professions is typically higher than for those employed in other health care work-force categories. Studies have shown that SES is associated with health and that people with lower SES tend to have lower health status.27 Additionally, the BMI index among health care workers in all workforce categories has increased over time, which is consistent with the findings of Caban et al28 who report that rates of obesity are rising among US workers regardless of race from 1986 to 2002. A number of studies have shown that nurses, aides, and orderlies are at high risk of injury, illness, and job-related burnout.29–31 Our study is consistent with these other studies in showing that those employed in health technician and heath service occupations are significantly less likely to report excellent health and are more likely to be obese.
Second, our findings indicate that health disparities by race or ethnicity do exist among health care workers. Overall, Black, Hispanic, and Asian health care workers are less likely to report excellent health than White health care workers. In terms of obesity, only Asian health workers are less likely to be obese than White workers across the health care work-force categories. In contrast, Black and Hispanic health care workers are more likely to be obese than their White counterparts in the categories of health technician and health services. Our findings are similar to previous studies that have shown a significant association between obesity and race or ethnicity.32,33 Moreover, Hertz et al34 studied the impact of obesity on work limitations and cardiovascular risk factors among US workers and found obese workers have the highest prevalence of work limitations, hypertension, dyslipidemia, type 2 diabetes, and the metabolic syndrome.
Finally, previous studies focus on physicians, dentists, and nurses who are among the health diagnosing and health assessing professions. Few studies have examined the health of health technicians and health services professions which are lower SES and more likely to have lower health status. Therefore, including the full spectrum of the health care workforce may help researchers better elucidate the context of health disparities among health care workers. Furthermore, additional research on health care utilization, health insurance coverage, and health conditions among these workers is needed if we are to understand and ultimately improve the health status of health care workers who can then provide better health care to reach Healthy People 2010 goals for the nation.
There are several study limitations that should be noted. First, excellent health status in the NHIS is based on self-report and responses may be culturally specific. Previous research has shown that Asians and Hispanics are less likely to provide strongly positive responses than Non-Hispanic Whites, although Asians and Hispanics tend to be younger and healthier.35 Differential reporting by race or ethnicity may explain some of the disparity in self-reported health status, although it is not clear that this would have changed over time. In addition, height and weight (for calculating BMI) are also both based on self-reports. Height is often overreported, whereas weight is often underreported which could result in an underestimate of obesity. However, epidemiologic evidence indicates a high correlation between self-reports and clinician measured BMI for Whites, Blacks, and Mexican-American adults.36 Second, sample sizes for some race groups within health care worker categories are small, thus limiting power to detect significant differences. Specifically, there are very few Blacks and Hispanics in the health diagnosing professions. Third, differences over time may be due to compositional differences in the population, which are likely not fully accounted for with the covariates included. Finally, health care workforce categories in our analyses are broadly defined and health status within each category may be quite heterogeneous. For example, the morbidity rankings of Lee et al8 indicate that among the health assessing and treating occupations, nurses have a relatively high morbidity ranking, whereas dietitians and pharmacists have relatively low rankings. Thus, our use of the coarsened health care work-force categories may be masking important health disparities within each category.
Conclusion
Self-reported health status of health care workers has declined over time and the prevalence of obesity is rising. Moreover, disparities in indicators of health exist, and in some cases have widened over time, among health care workers both across and within workforce categories. Providing quality health care requires a healthy health care work-force. Therefore, it is important to identify health differentials within the health care workforce to develop appropriate public health or occupational health interventions. Because health professionals from racial or ethnic minority and socioeconomically disadvantaged backgrounds are more likely to serve socially disadvantaged populations, the health status of health care workers needs to be taken into account when setting policies and implementing programs intended to increase access to health care and create a healthy diverse workforce. A diverse, well-trained, and healthy health care workforce may be key to improving the overall health status of the nation.
Acknowledgments
This project was supported by Grant Number R01HD046697 From the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
References
- 1.Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for the health status indicators: United States, 1990–98. Healthy People 2000 Stat Notes. 2002;23:1–16. [PubMed] [Google Scholar]
- 2.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17:477–486. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayala C, Greenlund K, Croft J, et al. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057. [DOI] [PubMed] [Google Scholar]
- 4.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57:36–54. doi: 10.1177/1077558700057001S03. [DOI] [PubMed] [Google Scholar]
- 6.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health. 2004;90:1923–1925. doi: 10.2105/ajph.90.12.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117:e868–e877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 8.Lee DJ, Fleming LE, Gomez-Marin O, et al. Morbidity ranking of U.S. workers employed in 206 occupations: the National Health Interview Survey (NHIS) 1986–1994. J Occup Environ Med. 2006;48:117–134. doi: 10.1097/01.jom.0000199520.23232.26. [DOI] [PubMed] [Google Scholar]
- 9.Schumacher EJ. Technology, skills, and health care labor markets. J Labor Res. 2002;23:397–415. [Google Scholar]
- 10.Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238:170–177. doi: 10.1097/01.SLA.0000081085.98792.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Escarce JJ, Chen W, Schwartz JS. Falling cholecystectomy thresholds since the introduction of laparoscopic cholecystectomy. JAMA. 1995;273:1581–1585. [PubMed] [Google Scholar]
- 12.Bhargavan M, Sunshine JH. Workload of radiologists in the united states in 2002–2003 and trends since 1991–1992. Radiology. 2005;236:920–931. doi: 10.1148/radiol.2363041316. [DOI] [PubMed] [Google Scholar]
- 13.Taub S, Morin K, Goldrich MS, Ray P, Benjamin R. Physician health and wellness. Occup Med (Lond) 2006;56:77–82. doi: 10.1093/occmed/kqj025. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 15.Porta C, Handelman E, McGovern P. Needlestick injuries among health care workers. A literature review. AAOHN J. 1999;47:237–244. [PubMed] [Google Scholar]
- 16.Yassi A, Cooper JE, Tate RB, et al. A randomized controlled trial to prevent patient lift and transfer injuries of health care workers. Spine. 2001;26:1739–1746. doi: 10.1097/00007632-200108150-00002. [DOI] [PubMed] [Google Scholar]
- 17.Yassi A, Khokhar J, Tate R, Cooper J, Snow C, Vallentyne S. The epidemiology of back injuries in nurses at a large Canadian tertiary care hospital: implications for prevention. Occup Med (Lond) 1995;45:215–220. doi: 10.1093/occmed/45.4.215. [DOI] [PubMed] [Google Scholar]
- 18.Baldwin PJ, Dodd M, Wrate RM. Young doctors’ health. II. Health and health behaviour. Soc Sci Med. 1997;45:41–44. doi: 10.1016/s0277-9536(96)00307-3. [DOI] [PubMed] [Google Scholar]
- 19.Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53:103–108. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- 20.Kawachi I, Colditz GA, Stampfer MJ, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92:3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- 21.Schernhammer ES, Laden F, Speizer FE, et al. Rotating night shifts and risk of breast cancer in women participating in the nurses’ health study. J Natl Cancer Inst. 2001;93:1563–1568. doi: 10.1093/jnci/93.20.1563. [DOI] [PubMed] [Google Scholar]
- 22.Schernhammer ES, Laden F, Speizer FE, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95:825–828. doi: 10.1093/jnci/95.11.825. [DOI] [PubMed] [Google Scholar]
- 23.Minnesota Population Center and State Health Access Data Assistance Center. Integrated Health Interview Survey: Version 1.0. Minneapolis: University of Minnesota; 2006. Available at: http://www.ihis.us/ [Google Scholar]
- 24.CDC. [Accessed July 9, 2007];About BMI for Adults. Available at: http://www.cdc.gov/nccdphp/dnpa/bmi/adult_BMI/about_adult_BMI.htm.
- 25.StataCorp. Stata Statistical Software; Release 9.0. College Station, TX: StataCorp LP; 2005. [Google Scholar]
- 26.StataCorp. Survey Data Reference Manual. College Station, TX: Stata Press; 2005. [Google Scholar]
- 27.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 28.Caban AJ, Lee DJ, Fleming LE, et al. Obesity in U.S. workers: the national health interview survey, 1986 to 2002. Am J Public Health. 2005;95:1614–1622. doi: 10.2105/AJPH.2004.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engel C. Health services industry: still a job machine? Mon Labor Rev. 1999;122:3–14. [Google Scholar]
- 30.Landsbergis PA. Occupational stress among health care workers: a test of the job demands—control model. J Organ Behav. 1988;9:217–239. [Google Scholar]
- 31.Engkvist IL, Hjelm EW, Hagberg M, Menckel E, Ekenvall L. Risk indicators for reported over-exertion back injuries among female nursing personnel. Epidemiology. 2000;11:519–522. doi: 10.1097/00001648-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Carroll MD, Gurtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 33.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 34.Hertz RP, Unger AN, McDonald M, Lustik MB, Biddulph-Krentar J. The impact of obesity on work limitations and cardiovascular risk factors in the U.S. work-force. J Occup Environ Med. 2004;46:1196–1203. [PubMed] [Google Scholar]
- 35.Kandula NR, Lauderdale DS, Baker DW. Differences in self-reported health among Asians, Latinos, and non-Hispanic whites: the role of language and nativity. Ann Epidemiol. 2007;17:191–198. doi: 10.1016/j.annepidem.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 36.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring) 2007;15:188–196. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]