Abstract
Background
Concerns about the use of mastectomy and breast reconstruction for breast cancer have motivated interest in surgeon’s influence on the variation in receipt of these procedures.
Objectives
To evaluate the influence of surgeons on variations in the receipt of mastectomy and breast reconstruction for patients recently diagnosed with breast cancer.
Methods
Attending surgeons (n=419) of a population-based sample of breast cancer patients diagnosed in Detroit and Los Angeles during 6/05 − 2/07 (n=2290) were surveyed. Respondent surgeons (n=291) and patients (n=1780) were linked. Random-effects models examined the amount of variation due to surgeon for surgical treatment. Covariates included patient clinical and demographic factors and surgeon demographics, breast cancer specialization, patient management process measures, and attitudes about treatment.
Results
Surgeons explained a modest amount of the variation in receipt of mastectomy (4%) after controlling for patient clinical and sociodemographic factors but a greater amount for reconstruction (16%). Variation in treatment rates across surgeons for a common patient case was much wider for reconstruction (median 29%, 5th–95th percentile 9%–65%) than for mastectomy (median 18%, 5th–95th percentile, 8% and 35%). Surgeon factors did not explain between-surgeon variation in receipt of treatment. For reconstruction, one surgeon factor (tendency to discuss treatment plans with a plastic surgeon prior to surgery) explained a substantial amount of the between-surgeon variation (31%).
Conclusion
Surgeons have largely adopted a consistent approach to the initial surgery options. By contrast, the wider between-surgeon variation in receipt of breast reconstruction suggests more variation in how these decisions are made in clinical practice.
INTRODUCTION
The appropriateness of rates of mastectomy for treatment of breast cancer has been a contentious policy issue for over two decades. There are lingering concerns that surgeons are recommending overly-aggressive care, given persistently high rates of mastectomy and wide regional variation despite strong professional consensus favoring less invasive treatment.1–3 However, recent studies suggest that surgical treatment decisions are a result of a more complex interplay between surgeon recommendations and patient preferences.2,4,5 Breast reconstruction following mastectomy has also been a focus of policy concerns because low rates of use and sociodemographic disparities suggest potentially that there is underuse in some groups.6,7
These issues motivate interest in quantifying attending surgeon’s influence on the variation in receipt of surgical treatment for breast cancer. Surgeons have a primary role in decisions about breast cancer treatment options, including post-mastectomy reconstruction,2,7 and there are large differences in surgeon specialization and practice context.8 In prior work, we found that the individual surgeon explained a moderate amount of the variation in mastectomy rates (7.5%) and larger amount of the variation in reconstruction rates following mastectomy (15%) after controlling for patient clinical and demographic characteristics.9
The present study advances the research in a new, more recently-diagnosed, population-based cohort of patients by addressing two questions motivated by the prior findings.9 First, are there patient factors beyond those originally studied that might further explain surgeon variation in receipt of treatment? Some women, as part of their primary treatment, have a mastectomy that follows very soon after BCS which is clearly a different decision than the earlier initial decision for BCS vs. mastectomy. Additionally, some women have contraindications to BCS due to characteristics not readily available in the SEER data. Our earlier research could not evaluate whether the differential distribution of these attributes might contribute to the variation attributed to the surgeon. Finally, the earlier study oversampled patients with ductal carcinoma in situ (DCIS) cancer by design and, thus, may not have reflected the amount of surgeon variation seen in patients presenting with a population spectrum of breast cancer.
The second question is whether certain features of surgical practices, endorsed in a recent Institute of Medicine report and promoted by national organizations as key elements of quality cancer care,10–13 may explain some degree of the surgeon level variation.8 Since there are no existing measures of these constructs in delivery of cancer care, we developed and evaluated our own measures of patient management process factors, using the Chronic Care Model.8 A unique feature of the present study is our ability to evaluate the degree to which such practice factors contribute to surgeon variation in breast cancer treatments.
METHODS
Study Sample
Details of the patient study have been published elsewhere.14–17 We enrolled a population-based sample of 3133 women in the metropolitan areas of Los Angeles and Detroit, aged 20–79 years recently diagnosed with breast cancer during a period from June, 2005 through February, 2007. We excluded patients with Stage 4 breast cancer, those who died prior to the survey, those who could not complete a questionnaire in English or Spanish, and Asian women in Los Angeles (because of enrollment in other studies). Latinas (in Los Angeles) and African-Americans (in both Los Angeles and Detroit) were over-sampled. Eligible patients were identified from the Surveillance, Epidemiology and End Results (SEER) program registries of both regions. The Dillman survey method was employed to encourage survey response.18 Patients completed a survey approximately nine months after diagnosis (96.5% by mail and 3.5% by phone), and this information was merged to SEER clinical data. The response rate was 73.1% (n=2290) of whom 2268 patients (72.4%) had complete SEER data. The study was approved by the Institutional Review Boards of the University of Michigan, University of Southern California and Wayne State University.
An attending surgeon was identified for 98.9% of the patient sample using information from patient reports, pathology reports, and SEER. Surgeons were mailed a letter of introduction, a survey, and a $40 subject fee approximately 14 months after the start of patient survey. We used a modified version of the Dillman method to optimize response.18 We identified 419 surgeons, of whom 318 returned completed questionnaires (response rate 75.9%). The patient and surgeon records were merged to create an analytic dataset with 1780 respondent patients (56.8% of eligible patients) nested among 291 respondent surgeons (69.5% of eligible surgeons).
VARIABLES
Dependent Variables
We used two dependent variables derived from the patient survey: 1) the first surgical treatment (mastectomy vs. BCS with or without radiation) was determined by asking women what was the first surgery performed after biopsy; and 2) receipt of post-mastectomy reconstruction defined as women who responded that they received breast reconstruction before being surveyed (yes vs. no).
Patient-Related Independent Variables
Clinical variables (derived from SEER) included tumor size (< 1 cm, 1 to 2 cm, 2 to 5 cm,> 5 cm and missing); histologic grade (well-differentiated, moderately differentiated, poorly differentiated, undifferentiated, missing); and tumor behavior (DCIS vs. invasive) because this information is generally available to surgeons at the time of surgery consultation. Patient demographics included age (categorical), race/ethnicity (white, black, Latina, other), education (high school graduate or less vs. some college or more), marital status (married/partnered, not married) and SEER site. Patient report of a clinical contraindication to BCS (yes/no) was measured based on a list of reasons her surgeon recommended mastectomy (eg. the tumor was too large or too diffusely located in the breast or that the initial surgery did not get it all).2,19
Surgeon-Related Independent Variables
We evaluated three sets of independent variables related to surgeons: 1) demographics; 2) level of breast cancer practice specialization, and 3) patient management factors. Demographic factors included surgeon gender and number of years in practice after training (continuous). Level of breast cancer specialization was measured by surgeon report of the percentage of total practice devoted to breast cancer (<15%, 15%–49%, and ≥ 50%). To measure patient and practice management process factors, we developed five scales reflecting implementation of a coordinated cancer care model in a surgical practice. The distribution of these measures in surgical practices has been recently described.8 These are comprised of patient and practice management processes reported by the surgeons. Three of these five had a monotonic relationship with mastectomy and reconstruction in bivariate analyses, and were included in the analysis. These included first, a Multidisciplinary Communication scale based on three items for which surgeons indicated the share of their patients in the prior year for whom they discussed a treatment plan with a medical oncologist, radiation oncologist, or plastic surgeon prior to surgery. Second, an Availability of Clinical Information scale was based on three items where surgeons indicated the share of their patients in the prior year who came for a second opinion whom they: 1) had specimens that were collected by another; provider reviewed again by your pathologist; 2) had mammogram images that were taken at another institution reviewed again by your radiologist; 3) repeated mammogram images that were brought from another institution. And third, a Patient Decision and Care support scale was based on five items where surgeons indicated the share of their patients who: 1) attended a presentation about breast cancer organized by your practice; 2) viewed video about treatment issues made available through your practice; 3) were referred to website tailored to your practice; 4) attended a patient support group organized by your practice; or 5) talked to other patients arranged by your practice. We used a five-point Likert response category where surgeons indicated the share of their patients who received the particular practice process item (from none or very few to almost all). Scale scores were calculated by summing items and dividing the resulting score into three categories (low, moderate, high).
Additional Variables
For the mastectomy versus BCS model, we included a measure of surgeons’ attitudes toward recommending the two treatment options (mastectomy vs. BCS). Surgeons were given a scenario describing a 60-year-old, 3 cm grade 3 infiltrating ductal carcinoma (ER/PR and HER-2 negative) with no contraindications to the surgery options. They were asked which treatment they would recommend and how strongly. We categorized the responses into those who would recommend mastectomy vs BCS.
Analysis
The analytic dataset contained all respondents with complete information for all variables used in the analyses (except for tumor size and histologic grade where missing observations were 6.6% and 7.8% of the sample respectively, and were placed in a “missing” category). We had 1639 patient observations clustered within 277 surgeons (median 6 patients, range 1–34) for the mastectomy outcome and 597 patients who received reconstruction surgery following mastectomy clustered in 217 surgeons (median 3 patients, range 1 to 20). Bivariate comparisons with the excluded observations showed no significant differences in any of the analysis variables. We first generated descriptive statistics for all of the variables and examined patterns of missing variables. All of these estimates were weighted to account for the differential probability of selection.
We used multilevel logistic regression models to estimate the amount of variation at the surgeon and patient level, and to examine the relative contribution of both patient and surgeon variables in explaining that variation. The models for both outcomes included the design variables (site and race/ethnicity), other patient demographics (age, education, marital status), and breast cancer clinical characteristics. The design variables were included in all models to account for the differential probability of selection of subjects based on categories of race by SEER site (LA vs. Detroit) generated by our sampling strategy (described above). The clinical contraindication to BCS variables was tested next for the mastectomy model.
We then added the surgeon level variables. We first tested bivariate relationships. We then added all the variables that were significant at a 0.10 level in the dichotomous relationships to the model and eliminated them if the likelihood ratio test was not significant when comparing the nested models.
Finally, we tested for the presence of a cross-level interaction between individual surgeon and patient characteristics for geographic site, those variables with a large effect on the outcome, or those for which we hypothesized that the coefficient of that effect might vary across surgeons. For the mastectomy model, we tested the heterogeneity of the education and contraindication to BCS variable across surgeons by testing whether the coefficient was random at the surgeon level. For the reconstruction model, we tested the heterogeneity of the coefficient for education across individual surgeon.
For each model, we calculated several measures that describe the amount of surgeon variation in the rates of mastectomy and reconstruction. These include the proportion of variation explained by the patient covariates and the residual surgeon level variation quantified using the method described by Snijders.22 This method provides an estimate of the proportion of the variance on the log odds scale attributable to the latent variable representing differences in rates across surgeons as well as the variance explained by the included covariates. We also provide a graphical presentation of the direct variation in rates as a function of the surgeon effect. All analyses were conducted using Stata software for Windows (version 10.1; StataCorp LP, College Station, TX).
RESULTS
Treatment Receipt
Overall, one-quarter (439, 26.8%) of women in our sample received mastectomy as initial surgical treatment. An additional 152 (9.3%) received mastectomy after one or more attempts at lumpectomy, but are counted for this analysis as initially receiving BCS. About one-third of the women who ultimately received mastectomy (222 of 591, 37.6%) had received reconstruction at the time of the survey.
Patient Characteristics
Table 1 shows patient characteristics and the distribution of receipt of initial mastectomy and receipt of reconstruction after mastectomy by subgroups. One-quarter had tumors <1 cm; 31.1% had tumors between 1 and 2 cm; and 39.7% had tumors greater than 2 cms. About one-fifth had DCIS. Patient report of clinical contraindications to BCS was uncommon. One-fifth of patients were less than 50, and 21.2% were 65 and older. About half of women were white, 26.6% were black, and 25.3% were Latina. One third of patients were high school graduates or less. Over half were partnered. About half were from Los Angeles, and 46.1% were from Detroit.
Table 1.
Patient characteristics and receipt of treatment
| N1 | %1 | % Initial Mastectomy2 |
P3 | % Recon after Mastectomy2 |
P3 | |
|---|---|---|---|---|---|---|
| Tumor Size | <.001 | <.001 | ||||
| <10 mm | 372 | 22.7 | 15.9 | 48.3 | ||
| 10–19 mm | 509 | 31.1 | 19.1 | 36.5 | ||
| 20–39 mm | 440 | 26.9 | 27.9 | 27.9 | ||
| 40+mm | 210 | 12.8 | 47.9 | 34.3 | ||
| Missing | 108 | 6.6 | 34.0 | 39.9 | ||
| Histologic Grade | <.001 | .005 | ||||
| 1 | 272 | 16.6 | 14.4 | 45.6 | ||
| 2 | 587 | 35.8 | 24.3 | 34.7 | ||
| 3 | 592 | 36.1 | 30.5 | 32.5 | ||
| 4 | 60 | 3.7 | 22.7 | 44.6 | ||
| Missing | 128 | 7.8 | 28.9 | 33.9 | ||
| Tumor Behavior | <.001 | <.001 | ||||
| DCIS | 330 | 20.1 | 14.4 | 56.3 | ||
| Invasive | 1309 | 79.9 | 27.5 | 31.8 | ||
| Contraindications to BCS | <.001 | .161 | ||||
| No Contraindications | 1423 | 86.8 | 16.9 | 36.3 | ||
| Contraindications | 216 | 13.2 | 85.6 | 32.9 | ||
| Age Group | <.001 | <.001 | ||||
| <50 | 438 | 26.7 | 33.9 | 54.1 | ||
| 50–64 | 721 | 44.0 | 22.8 | 37.4 | ||
| ≥65 | 480 | 29.3 | 21.2 | 8.2 | ||
| Race | .239 | .038 | ||||
| Latina | 505 | 25.3 | 29.8 | 28.1 | ||
| Black | 436 | 26.6 | 24.5 | 33.1 | ||
| White | 749 | 45.7 | 23.8 | 38.4 | ||
| Other | 39 | 2.4 | 25.8 | 22.5 | ||
| Education | .525 | <.001 | ||||
| H.S. Grad or Less | 657 | 40.1 | 24.4 | 18.7 | ||
| Some College or More | 982 | 59.9 | 25.3 | 42.2 | ||
| Marital Status | .703 | <.001 | ||||
| Not Married | 728 | 44.4 | 25.3 | 25.7 | ||
| Married/Partner | 911 | 55.6 | 24.8 | 41.6 | ||
| SEER Site | .003 | <.001 | ||||
| LA | 884 | 53.9 | 23.9 | 32.0 | ||
| Detroit | 755 | 46.1 | 27.9 | 43.5 | ||
Values are expressed as number and unweighted percentages
Values are expressed as weighted percentages to account for the sampling design
P values test differences in distribution of receipt of treatment by subgroups
Surgeon Characteristics
Table 2 shows characteristics of the surgeon sample. One-fifth were female and the mean number of years in practice was 18.4 (SD,10.7); 61.7% were from Los Angeles and 38.3% were from Detroit. One-third devoted 15% or less of their practice to breast cancer and 16.8% devoted 50% or more. One-quarter indicated that their main practice affiliation was a cancer center, with 40.1% in a practice affiliated with an ACoS Cancer Program. One-third of surgeons scored low on the Multidisciplinary Communication scale (31.9%) and on the Availability of Clinical Information Scale. Two-thirds scored low on the Patient Decision Support scale. Only 14.9% of surgeons favored mastectomy in the treatment scenario.
Table 2.
Surgeon Characteristics
| N1 | %1 | |
|---|---|---|
| Surgeon Gender | ||
| Male | 227 | 81.9 |
| Female | 50 | 18.1 |
| Yrs in Practice (mn, s.d.) | 18.4 | (10.7) |
| SEER Site | ||
| LA | 171 | 61.7 |
| Detroit | 106 | 38.3 |
| Surgeon Specialization2 | ||
| <15 | 100 | 36.1 |
| 15–49 | 132 | 47.7 |
| ≥50 | 45 | 16.2 |
| Practice Setting | ||
| NCI Cancer Center | 79 | 28.5 |
| ACS Cancer Program | 111 | 40.1 |
| Neither | 87 | 31.4 |
| Multidisciplinary Comm | ||
| Low | 89 | 32.1 |
| Medium | 130 | 46.9 |
| High | 58 | 20.9 |
| Availability of Clinical Info | ||
| Low | 88 | 31.8 |
| Medium | 118 | 42.6 |
| High | 71 | 25.6 |
| Pt Decision Support | ||
| Low | 177 | 63.9 |
| Medium | 82 | 29.6 |
| High | 18 | 6.5 |
Values are expressed as number and unweighted percentages
% of total practice devoted to breast cancer
Independent Correlates of Mastectomy
Receipt of initial mastectomy was positively associated with larger tumor size, advanced histologic grade, invasive disease behavior, and report of clinical contraindication to BCS (all p values<.001). No patient sociodemographic variables or surgeon characteristics, including practice organizational factors and surgeon attitudes toward treatment, were significantly associated with receipt of mastectomy after controlling for clinical factors. There were no interactions between SEER site and other covariates.
Between-Surgeon Variation in Receipt of Mastectomy
Table 3 summarizes the multilevel model results for the mastectomy versus BCS outcome. Overall, the model explained 37% of the total variation in mastectomy rates with patient clinical factors and patient report of a clinical contraindication to BCS the primary explanatory variables (Column A). Seven percent of the variation in mastectomy versus BCS among women in our sample was attributed to individual surgeons after controlling for patients clinical and demographic factors (Column B). The proportion of variation unexplained at the surgeon level decreased to 4.0% when clinical contraindication to BCS was added to the model, indicating that including this variable reduced unexplained between-surgeon variation by 43% (column C). Surgeon variables added sequentially to the model did not further explain variance at the patient or surgeon level.
Table 3.
Random-effects model: Mastectomy versus Breast-conserving surgery1
| Variables | A2 Total Variation |
B3 Surgeon Variation |
C4 % of surgeon variation explained |
|---|---|---|---|
| Patient clinical and demographics | 14% | 7% | NA |
| Contraindication to BCS | 37% | 4% | 43% |
| Surgeon demographics | 37% | 4% | 0 |
| Surgeon practice factors | 38% | 4% | 0 |
| Surgeon attitudes about treatment | 38% | 4% | 0 |
N= 1639 patients and 277 surgeons
Column A: R2 results after inclusion of patient and surgeon variable sets
Column B: % total variation attributable to individual surgeons
Column C: % of between -surgeon variation explained after including variable sets
Independent Correlates of Breast Reconstruction
Receipt of breast reconstruction after mastectomy was positively associated with smaller tumor size, non-invasive disease, younger age, and higher education. Reconstruction was positively associated with more multidisciplinary communication (adjusted odds ratio 3.7 and 3.4 for high and moderate levels of communication vs lowest level, Wald test 8.7, p=.012). On further evaluation we determined that this association was entirely due to one item in the scale: share of patients for whom the surgeon respondent consulted with a plastic surgeon prior to surgery. When one variable constructed from this item (1/3 or more vs. none or few patients referred to plastic surgeon prior to surgery) was included in a model substituting for the scale, the adjusted odds ratio was 6.6 (95 CI 3.2, 13.9).
We evaluated whether there were significant interactions between patient and surgeon level variables. There were no interactions between SEER site and other covariates. We then focused on patient education, because the base model showed that patients with lowest education were less likely to receive reconstruction (aOR .45, 95%CI .25, .78), and it seemed plausible that this effect of education might be modified by different surgeon communication styles or abilities. Patients with low education were widely dispersed across surgeon: 217 of 277 surgeons in the dataset had one or more low-education patients in their panel, and 62 had four patients or more. There was no evidence that the effect of education on reconstruction varied across surgeon (likelihood ratio chi sq 0.0, p>.9)
Between-Surgeon Variation in Receipt of Reconstruction
In contrast to the results for mastectomy, the individual surgeon explained a substantial amount of the patient variation in receipt of breast reconstruction (Table 4). Overall, the model explained 45% of the total patient variation with contributions from both patient and surgeon factors (Column A). Sixteen percent of variation in receipt of reconstruction among women who were treated with mastectomy was attributable to individual surgeons after controlling for patient clinical and demographic variables (Column B). Surgeon practice factors explained 31% of the between-surgeon variation (Column C). The effect of surgeon practice factors on between-surgeon variation in reconstruction was due solely to one item in the multidisciplinary communication scale: surgeon’s share of new patients in their practice for whom the surgeon talked to a plastic surgeon prior to surgery. When this item was entered in a model (binary variable few or no patients vs. more) with only patient level variables, it accounted for 31% of the between-surgeon variation in reconstruction. No other surgeon practice variables contributed to between-surgeon variation in reconstruction.
Table 4.
Random-effects model: Breast Reconstruction (yes vs no)1
| Variables | A2 Total Variation |
B3 Surgeon Variation |
C4 % of surgeon variation explained |
|---|---|---|---|
| Patient clinical and demographics | 38% | 16% | NA |
| Surgeon demographics | 38% | 16% | 0 |
| Surgeon practice process factors | 45% | 11% | 31% |
N= 597 patients and 217 surgeons
Column A: R2 results after inclusion of patient and surgeon variable sets
Column B: % total variation attributable to individual surgeons
Column C: % of between-surgeon variation explained after including variable sets
The figure illustrates the surgeon effect directly on the scale of mastectomy and reconstruction rates. The figures show the estimated average surgeon rate of mastectomy and breast reconstruction for a typical patient in clinical practice across the different individual surgeons in the sample (indicated by the change in procedure rate moving from one end to the other of the surgeon distribution shown on the×axis). It also shows differences in procedure rates across important clusters of clinical characteristics described in the figure legend (shown by the difference in rates seen between curves on each graph). Thus, the magnitude of these absolute differences in use rates can be compared across surgeon and by key patient characteristics. For mastectomy, the graphs show that the magnitude of effect of having a clinical contraindication to breast conserving surgery dwarfs the differences in the propensity to do a mastectomy across surgeons. However, the effect, within an individual surgeon's practice, when comparing the mastectomy rates of a women with a smaller moderately differentiated tumor to one with a larger more poorly differentiated tumor, is similar in magintude to going from a surgeon with a low average rate of mastectomy to one with a high rate. For reconstruction, the differences in rate of reconstruction across surgeon (moving from left to right along the×axis) are for the most part larger than those within surgeon across clinical characteristics (moving across curves at any given x-axis location representing an individual surgeon).
Figure 1.
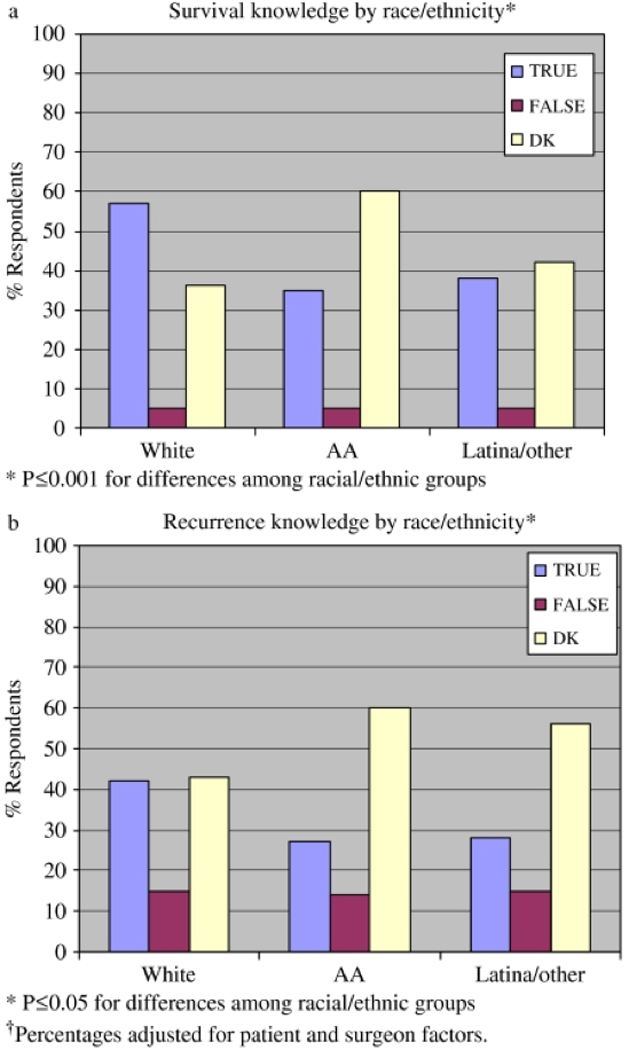
The figures show the estimated rate of mastectomy and breast reconstruction for a typical patient in the dataset across the different individual surgeons. The base case represents a 50–64 year old, white high school graduate with moderately differentiated early stage disease, with no clinical contraindication to BCS. Two other cases are shown in each graph. For mastectomy, a patient with a larger and higher stage is shown, as well as one with a contraindication to BCS. For reconstruction, a patient with larger and higher stage is also shown along with a patient with age>65. At the bottom of the graph are histograms showing the distribution of the surgeon effects observed for the study participants. These distributions illustrate the degree to which the observed surgeon effects are normally distributed, as well as the presence or absence of any outlier surgeons, and give a sense of the proportion of the population of surgeons that would be expected to have any given rate mastectomy or reconstruction. The magnitude of difference in rates across the distribution of surgeons can be compared to the magnitude of effect across the different levels of covariates illustrated with the different lines.
Comment
We performed a survey of patients recently diagnosed with breast cancer in the Los Angeles and Detroit metropolitan areas, and a companion survey of their attending surgeons to examine surgeon influences on variations in initial receipt of mastectomy and post-mastectomy reconstruction. We found that individual surgeon explained only a modest amount of the total variation in receipt of mastectomy (4%) after controlling for patient clinical and sociodemographic factors, but a much greater amount of total variation in reconstruction (16%). With regard to our first study question: more precise specification of receipt of treatment; better identification of women with contraindications to mastectomy; and inclusion of a more representative spectrum of breast cancer severity in our sample did not eliminate the surgeon level variation in rates of mastectomy and reconstruction that we had previously observed.9
Our second study question was whether practice organizational factors would explain some of the residual differences in mastectomy and reconstruction rates across surgeons. Our results suggest little association between mastectomy and these factors: Neither surgeon demographics (gender and years in practice), nor practice factors (breast cancer specialization and patient management process measures); nor attitudes about the treatment options measured using scenarios further explained between-surgeon variation in receipt of treatment. For reconstruction, one surgeon patient management process factor (share of the surgeons patients for whom the surgeon consulted with plastic surgeon prior to surgery) explained a substantial amount of the remaining between surgeon variation (31%).
Unique to the current analyses was the addition of surgeon patient management process factors to these models. These measures were developed based on the Chronic Care Model 8 which addresses basic elements for improving care in health systems including multidisciplinary care teams, and patient decision and care support.20,21 The model has been applied to research addressing the patterns of treatment and quality of care of patients with diabetes, heart disease, and depression. These types of factors have been highlighted by national organizations, including the IOM, as potential mechanisms for improving the quality of cancer care. Despite the interest in these management process factors, there have been no large studies that have incorporated these potentially important measures to evaluate patterns of treatment during the initial course of therapy. However, variables designed to measure most of the reasons that have been hypothesized as leading to practice variation (including surgeon experience, attitudes, and whether they practice in settings where there are opportunities for patient decision support and multidisciplinary input) did not further explain between-surgeon variation in treatment.
Strengths of the study included a large diverse sample of patients in two urban regions of the United States. We were able to link over 98% of respondent patients to an attending surgeon and nearly 75% of surgeons completed a survey. We collected a comprehensive set of surgeon level variables including demographics; level of specialization in breast cancer; and measures of surgeon patient management factors. However, our findings should be interpreted in the context of some limitations. The fact that our surveys were conducted in two large, urban geographic locations (Detroit and Los Angeles) limits the generalizability, particularly to more rural locations. We had limited power to detect small SES gradients in use of reconstruction because of the sample size and thus these results should be interpreted with some caution. Non-response and non-matching between some patients and surgeons may have also limited generalizability of our findings, particularly for surgeons with very low patient volumes. We were unable to account for the potential clustering of surgeons within practices or hospitals. However, the procedures we studied in this are commonly done by many general surgeons and one surgeon may practice at different hospital locations, lessening any potential impact of hospital-related clustering. We were also limited by the self-reported nature of some variables on both the patient and surgeon side.
Implications
Our findings have important implications for health policy. Lingering concerns about overtreatment with mastectomy at the hands of surgeons have diminished in response to recent research suggesting that surgeons’ recommendations for treatment are generally appropriate, and that patient preferences play an important role in decision-making.2,4 The very modest effect of individual surgeon on variation in mastectomy use observed in this study reinforces the notion that surgeons have largely adopted a uniform approach to the initial surgery options. Furthermore, between-surgeon variation in receipt of mastectomy was not attributable to surgeon demographics or patient management processes related to a more coordinated cancer care approach to treatment. While these practice management factors may be desirable for other reasons, they do not seem to explain differences in the surgical treatment options that women receive.
By contrast, the wide between-surgeon variation in receipt of breast reconstruction after mastectomy suggests that patients should be more cautious about how these decisions are made in clinical practice. In particular, the very strong effect of exposure to plastic surgeons prior to decisions about local therapy suggests that one possible result of multidisciplinary models of decision-making may be a much greater likelihood of receiving breast reconstruction after mastectomy. Prior literature suggests that patient satisfaction and quality of life related to breast reconstruction are high. But some patients who do not get it report lack of information or difficulties finding a surgeon who will perform it despite state laws that mandate insurance coverage.6,7 Our findings suggest that the treatment decision context and access to breast reconstruction vary across surgeon practices.
Our findings may inform interventions to reduce SES disparities in receipt of breast reconstruction after mastectomy. Similar to another study, we observed large socioeconomic disparities in the receipt of breast reconstruction after mastectomy. 6 A key question is whether the SES gradient in receipt of reconstruction varied across surgeon (reflecting a differential ability to bridge this disparity on the part of individual surgeons). We did not find any evidence of the heterogeneity of this effect. These findings suggest that interventions to reduce these disparities should be targeted broadly across the surgeon community.
Acknowledgments
Funding
This work was funded by grants R01 CA109696 and R01 CA088370 from the National Cancer Institute (NCI) to the University of Michigan. Dr. Katz was supported by an Established Investigator Award in Cancer Prevention, Control, Behavioral, and Population Sciences Research from the NCI (K05CA111340). The collection of Los Angeles County cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the NCI’s Surveillance, Epidemiology and End Results (SEER) Program under contract N01-PC-35139 awarded to the University of Southern California, contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The collection of metropolitan Detroit cancer incidence data was supported by the NCI SEER Program contract N01-PC-35145. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Footnotes
Additional Contributions: We acknowledge the outstanding work of our project staff: Barbara Salem, MS, MSW; Christina Jagielski, MPH; and Ashley Gay, BA (University of Michigan); Ain Boone, BA; Cathey Boyer, MSA; and Deborah Wilson BA (Wayne State University); and Alma Acosta, Mary Lo, MS, Norma Caldera, Marlene Caldera, and Maria Isabel Gaeta, (University of Southern California). We thank the American College of Surgeons Commission on Cancer (David Winchester, MD, and Connie Bura).
REFERENCES
- 1.Katz SJ, Hawley ST. From policy to patients and back: surgical treatment decision-making for patients with breast cancer. Hlth Affairs. 2007;26(3):761–769. doi: 10.1377/hlthaff.26.3.761. [DOI] [PubMed] [Google Scholar]
- 2.Morrow M, Jagsi R, Alderman AK, et al. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA. 2009;302(14):1551–1556. doi: 10.1001/jama.2009.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher ES, Wennenberg J. Health Care Quality, Geographic Variations, and the Challenge of Supply-Sensitive Care. Perspectives in Biology and Medicine. 2003;46(1):69–79. doi: 10.1353/pbm.2003.0004. [DOI] [PubMed] [Google Scholar]
- 4.Hawley ST, Griggs JJ, Hamilton AS, et al. Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. J Nat Cancer Inst. 2009;101(19):1337–1347. doi: 10.1093/jnci/djp271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz SJ, Lantz PM, Janz NK, et al. Patient involvement in surgical treatment decisions for breast cancer. Journal of Clinical Oncology. 2005;23(24):5526–5533. doi: 10.1200/JCO.2005.06.217. [DOI] [PubMed] [Google Scholar]
- 6.Alderman AK, Hawley ST, Janz NK, et al. Racial/ethnic disparities in the use of post-mastectomy breast reconstruction: results from a population-based study. J Clin Oncol. 2009 doi: 10.1200/JCO.2009.22.2455. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alderman AK, Hawley ST, Waljee JF, et al. Correlates of referral practices of general surgeons to plastic surgeons for mastectomy reconstruction. Cancer. 2007;109:1715–1720. doi: 10.1002/cncr.22598. [DOI] [PubMed] [Google Scholar]
- 8.Katz SJ, Morrow M, Hawley ST, et al. Coordinating cancer care: patient and practice management processes among surgeons who treat breast cancer. Medical Care. 2009 doi: 10.1097/MLR.0b013e3181bd49ca. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawley ST, Hofer TP, Janz NK, et al. Correlates of between-surgeon variation in breast cancer treatments. Medical Care. 2006;44(7):609–616. doi: 10.1097/01.mlr.0000215893.01968.f1. [DOI] [PubMed] [Google Scholar]
- 10.Hewitt M, Simone JV, editors. Ensuring Quality Cancer Care. Washington, DC: National Academy Press; 1999. Institute of Medicine Report NCPB, National Research Council) p. 97. [PubMed] [Google Scholar]
- 11.National Cancer Institute. [Accessed 2008];Quality of Care and Survivorship Issues. 2007 < http://ncccp.cancer.gov/Resources/QualityCare.htm>.
- 12.American Society of Clinical Oncology. [Accessed 2008 November, 2008];The Quality Oncology Practice Initiative. 2008 < http://qopi.asco.org>.
- 13.American College of Surgeons Commission on Cancer. National Quality Forum Endorsed Commission on Cancer Measures for Quality of Cancer Care for Breast and Colorectal Cancers. [Accessed 2008 November, 2008];2007 < http://www.facs.org/cancer/qualitymeasures.html>.
- 14.Hamilton AS, Hofer TP, Hawley ST, et al. Latinas and breast cancer outcomes: population-based sampling, ethnic identity and acculturation assessment. Cancer Epidemiology, Biomarkers, and Prevention. 2009;18(7):2022–2029. doi: 10.1158/1055-9965.EPI-09-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mujahid M, Janz NK, Hawley ST, et al. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Research and Treatment. 2009 doi: 10.1007/s10549-009-0389-y. 2009(Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in adequacy of information and support for women with breast cancer. Cancer. 2008;113(5):1058–1067. doi: 10.1002/cncr.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawley ST, Janz NK, Hamilton AS, et al. Latina patient perspectives about informed decision making for surgical breast cancer. Patient Educ Couns. 2008;73(2):363–370. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dillman DA. Mail and telephone surveys. New York: John Wiley and Sons, Inc.; 1978. [Google Scholar]
- 19.American College of Radiology. Practice guideline for the breast conservation therapy in the management of invasive breast carcinoma. J Am Coll Surg. 2007;205(2):362–376. doi: 10.1016/j.jamcollsurg.2007.02.057. [DOI] [PubMed] [Google Scholar]
- 20.Casalino LP. Disease management and the organization of physician practice. JAMA. 2005;293(4):485–488. doi: 10.1001/jama.293.4.485. [DOI] [PubMed] [Google Scholar]
- 21.Wagner EH, Austin BT, M VK. Organizing care for patients with chronic illness. 1996;74(4):511–544. [PubMed] [Google Scholar]
- 22.Snijders T, Bosker R. Multilevel analysis: an introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 23.Larsen K, Merlo J. Appropriate Assessment of Neighborhood Effects on Individual Health: Integrating Random and Fixed Effects in Multilevel Logistic Regression. Am J Epidemiol. 2005;161(1):81–88. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]


