Abstract
The goal of surgical treatment for adolescent idiopathic scoliosis (AIS) is to achieve a solid fusion in a balanced spine. While many previous studies analyzed coronal balance, there is a paucity of studies that comment on postoperative trunk shift, which has shown to have impact on clinical outcome. The purpose of this retrospective, multicenter data analysis was to analyze the incidence of postoperative trunk shift in patients with surgical treatment for AIS. We conducted a retrospective, multicenter data analysis of 1,555 patients with AIS. Patients with a Lenke type 1 or 2 curve pattern and a minimum follow-up of 24 months after surgery were included. A >2 cm deviation of the trunk in relation to the pelvis was considered positive trunk shift. A subanalysis was performed to identify potential risk factors for trunk shift. 273 patients meeting the inclusion criteria were analyzed. While the preoperative prevalence of trunk shift was surgically reduced from 29.3 to 13.6%, 24 patients (8.8%) with postoperative trunk shift had not had preoperative trunk shift, and the trunk shift was considered iatrogenic. Undercorrection of the lumbar curve was identified as potential risk factor, whereas thoracic correction, coronal balance, angulation and translation of the lowest instrumented vertebra did not seem to influence postoperative trunk shift. Iatrogenic postoperative trunk shift has an incidence of 8.8% in the surgical treatment of AIS.
Keywords: Adolescent idiopathic scoliosis, Trunk shift, Balance, Lenke type 1 and 2 curve, Lumbar curve correction
Introduction
The goal of surgical treatment for adolescent idiopathic scoliosis (AIS) is to achieve a solid spinal fusion that is balanced in both the coronal and sagittal planes. Sagittal balance, also referred to as the sagittal vertical axis, can be quantified by the distance between the lateral C7 plumb line (C7P) and either the center or posterior edge of the sacrum. The spinopelvic relation can also be assessed as an additional means to evaluate the “global” sagittal balance. Coronal balance may be quantified by the distance between the coronal C7P and the central sacral vertical line (CSVL). However, it has been demonstrated that a patient may be “balanced” in the coronal plane, with the head centered over the pelvis, but may still manifest a significant trunk imbalance. This specified deformity was initially described by Floman in 1982 [1]. Trunk imbalance has been shown to negatively affect pelvic obliquity, function, and self-image in patients with scoliosis [1, 2].
Numerous studies have used the C7P–CSVL distance as an outcome tool for coronal balance after surgical treatment for AIS [3–7], but there is a paucity of data commenting on the postoperative trunk balance and/or trunk shift in AIS. The purpose of this study is to analyze postoperative trunk balance in AIS patients with a Lenke type 1 or 2 curve from a prospective multicenter database. We will also attempt to identify any potential risk factors for postoperative imbalance or trunk shift in this patient population.
Materials and methods
An analysis of a prospectively collected multicenter database of 1,555 patients with AIS was performed. All patients within the database with a Lenke type 1 or 2 curve pattern and minimum 2-year postoperative clinical and radiographic follow-up were selected for inclusion in the study. In total, 273 patients from this database met the aforementioned criteria.
Examination of each patient’s preoperative and 2-year postoperative standing full length 36-inch posteroanterior (PA) radiographs was performed. Trunk shift was measured using a horizontal line drawn through the apical vertebra, with two subsequent marks drawn at the respective end of the left trunk (a), and the right trunk (b). A perpendicular line was then drawn at the midpoint of marks (a) and (b), which was deemed the vertical trunk reference line (VTRL) (Fig. 1). Trunk shift was, therefore, defined as a greater than 2-cm difference between the VTRL and the CSVL.
Fig. 1.
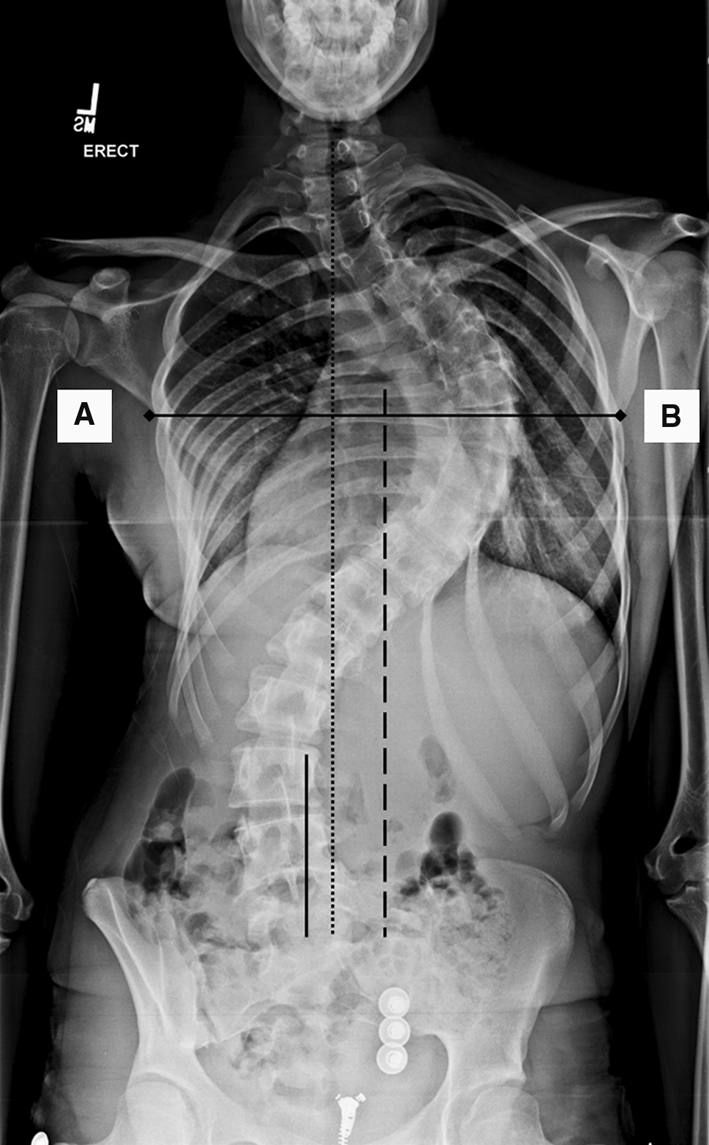
Schematic description for measuring trunk shift. A horizontal line is drawn through the apex of the thoracic curve. The endpoints of this line represent the truncal margin (A, B). The bisecting perpendicular line represents the vertical trunk reference line (VTRL, dashed). Trunk shift is defined as a distance greater than 2 cm between the VTRL and the center sacral vertical line (CSVL). The VTRL differs from the C7 plumb line (C7P, dotted) that is used to measure coronal balance (distance between CSVL and C7P)
Analysis of variance (ANOVA) was used to compare preoperative and 2-year radiographic data between patients with and without postoperative trunk shift in order to identify potential risk factors. These included pre-existing trunk shift, preoperative thoracic and lumbar curve magnitude, curve flexibility, coronal balance (distance between C7P and CSVL), shoulder height (measured with the T1 rib angle and the soft tissue shadow) level, angulation and translation of the lowest instrumented vertebra as well as thoracic and lumbar rotation (measured with the scoliometer). Spearman’s correlation and logistic regression analyses were used to confirm correlation of identified variables associated with postoperative trunk shift. Significance was achieved at p < 0.05.
Results
Of the 273 patients included in this study, 222 were Lenke type 1 (81%) and 51 were Lenke type 2 curves (19%). 224 patients were female (82%) and 49 were male (18%). The average age at surgery was 14.5 years (range 10–21 years). Preoperative trunk shift was identified in 80 patients (29.3%), while 37 patients (13.6%) were found to have trunk shift 2 years postoperatively. Twenty-four of the 37 patients (65%) who had postoperative trunk shift had no preoperative trunk shift, and this decompensation was considered iatrogenic (Table 1). At 2-year follow-up, the percent correction of the thoracic curve was similar in both groups (trunk shift = 61%, No trunk shift = 65%, p = 0.18). Patients with trunk shift demonstrated increased shoulder imbalance (5.5° vs. 3.8°, p = 0.04) and less correction of the lumbar curve than patients with no trunk shift (49 vs. 60%, p = 0.009). Logistic regression analysis did not confirm the findings for shoulder balance (r = 0.09, p = 0.14), but found a significant correlation between percentage of lumbar curve correction and the presence of postoperative trunk shift (r = 0.14, p = 0.02). None of the other analyzed parameters was found to be a significant risk factor for postoperative trunk shift. A selection of the analyzed parameters is given in Table 2.
Table 1.
Relation of preoperative to postoperative trunk shift
| Frequency | Percent | |
|---|---|---|
| No shift pre or post | 169 | 61.9 |
| No shift pre, yes post | 24 | 8.8 |
| Yes pre, no post | 67 | 24.5 |
| Yes pre, yes post | 13 | 4.8 |
| Total | 273 | 100 |
Table 2.
Comparison of potential risk factors between both groups
| T1 rib angle (°) | Correction lumbar (%) | Correction thoracic (%) | Coronal balance (cm) | LIV angulation (°) | LIV translation (cm) | |
|---|---|---|---|---|---|---|
| TS (n = 37) | 5.46 (SD 4.35) | 49% (SD 24) | 61% (SD 0.19) | 1.3 (SD 1.1) | 17.0 (SD 13.4) | 0.42 (SD 1.88) |
| No TS (n = 236) | 3.79 (SD 4.56) | 60% (SD 22) | 65% (SD 0.15) | 1.4 (SD 1.1) | 17.8 (SD 13.1) | 0.57 (SD 1.57) |
| p value | 0.04 | 0.009 | 0.18 | 0.77 | 0.72 | 0.62 |
Discussion
We identified a 29.3% prevalence of preoperative trunk shift in a prospectively collected database of 273 AIS surgical patients with Lenke type 1 or 2 curves. Two years postoperatively, the prevalence of trunk shift was 13.6%. Analysis of this subset of 37 patients with postoperative trunk shift revealed 24 patients who had a balanced trunk prior to surgery. This represents 65% of all patients with postoperative trunk shift (8.8% of total patient population) whose trunk imbalance was iatrogenic.
Few authors have addressed true trunk shift in AIS [1, 5]. Additionally, these studies are limited by a small and/or heterogeneous patient population. Instead, coronal balance is frequently used as outcome tool for coronal plane correction [3–5, 7]. However, a spine can be balanced by compensation with a trunk that is significantly shifted away from the center of the vertical axis, for example by adding-on above the instrumentation. This deformity has been shown to be significant according to Floman et al. [1] who observed a relation of trunk shift and pelvic obliquity as well as trunk shift and back pain. Additionally, Asher et al. [2] noted that clinical trunk deformity directly influenced the perception of function and self-image in patients with AIS. Therefore, an iatrogenic trunk shift incidence of 8.8% can be considered unfavorable and has to be recognized to further improve the surgical treatment of AIS.
In this study, the majority of parameters including the thoracic curve correction and coronal balance, as well as the angulation and translation of the LIV, were not found to have a statistically significant impact on postoperative trunk shift. The statistically significant difference that was observed for the T1 rib angle was not confirmed by logistic regression analysis. Undercorrection of the lumbar curve relative to the thoracic curve was the only identifiable predisposing factor to the development of postoperative trunk shift. Using the term “lumbar undercorrection” is clearly debatable, since the lumbar spine is not instrumented in selective thoracic fusion and corrects spontaneously. While some can argue that there is “spontaneous undercorrection” of the uninstrumented lumbar spine, others may prefer the expression “thoracic overcorrection.” The conclusion that has to be drawn would be that the surgeons really can do harm by achieving a perfect thoracic correction and, therefore, should aim for less. Furthermore, thoracic overcorrection (% of thoracic correction divided by % of lumbar correction) was one of the analyzed parameters. While potentially showing a trend, the difference was not statistically significant (p = 0.1).
In our opinion, the real challenge lies in identifying the ideal candidate for selective thoracic fusion. The average undercorrection of the lumbar curve that was seen in patients with postoperative trunk shift may be due to a number of patients in whom the compensatory curve did not sufficiently correct after selective thoracic fusion. Although shoulder balance was initially found to be significantly different between patients with and without trunk shift, logistic regression analysis did not confirm the findings and correlation between shoulder balance and trunk shift was not significant. However, it cannot be excluded that an existing postoperative shoulder imbalance was masked by a positional trunk shift in order to level the shoulders.
The influence of the lumbar curve on postoperative imbalance has been previously described. Undercorrection of the lumbar curve has been identified as a risk factor for postoperative decompensation in some patients undergoing selective thoracic fusion [3, 8]. Further, distal adding on after fusing “too short” has been described by Suk et al. [5] as a cause for postoperative trunk shift. A risk analysis performed by Behenksy et al. [7] found a correlation between coronal plane decompensation and lumbar apical vertebral rotation and flexibility measured on preoperative bending radiographs. Patwardhan et al. [9] concluded after their geometrical study that the postoperative lumbar curve magnitude should not exceed twice the amount of the postoperative thoracic curve magnitude to maintain coronal balance. However, these studies only assess coronal balance by measuring the C7P–CSVL distance and do not specifically assess trunk balance.
Richards et al. performed a radiographic study of patients with AIS and found a correlation between trunk shift and coronal balance. However, their findings were only reliable in patients with marked coronal imbalance, which does not happen to be the case for the majority of patients with AIS [6]. Although Luk et al. [10] measured postoperative trunk shift in patients with Lenke type 1 curves, the authors did not further analyze their data in regard to prevalence, incidence, or risk factors for postoperative decompensation.
Modern instrumentation systems and surgical techniques allow for substantial corrective forces to be applied to the spine. Nowadays, many surgeons take advantage of this and aim for nearly complete curve correction, potentially leaving the lumbar curve relatively undercorrected. As mentioned before, rather than being explained by thoracic “overcorrection,” this phenomenon may be due to misidentifying ideal candidates for selective thoracic fusion.
One limitation of our study is that we did not differentiate between surgical approaches or instrumentation. Further, we were only able to provide radiographic short-term (two-year) follow-up data and did not correlate our findings to clinical outcome. However, this is the first study that analyzes the prevalence and potential risk factors for trunk shift in a large AIS patient population with Lenke type 1 and 2 curve patterns.
Conclusion
Postoperative trunk shift is not uncommon after surgery for AIS, occurring is 13.6% of patients in this series, of which 65% were iatrogenic. Coronal imbalance does not correlate with trunk shift. Undercorrection of the lumbar curve predisposes to the development of postoperative trunk shift.
Acknowledgments
This study was supported by a research grant from the DePuy-Spine Harms Study Group and aided by a grant from the Orthopaedic Research and Education Foundation. IRB approval for the study was obtained locally from each contributing institution’s review board.
Conflict of interest The author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Floman Y, Penny JN, Micheli LJ, Riseborough EJ, Hall JE. Osteotomy of the fusion mass in scoliosis. J Bone Joint Surg Am. 1982;64:1307–1316. [PubMed] [Google Scholar]
- 2.Asher M, Lai SM, Burton D, Manna B. The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients’ health-related quality of life questionnaire responses. Spine (Phila Pa 1976) 2004;29:861–868. doi: 10.1097/00007632-200404150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Puno RM, An KC, Puno RL. Treatment recommendations for idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:2102–2115. doi: 10.1097/01.BRS.0000088480.08179.35. [DOI] [PubMed] [Google Scholar]
- 4.Satake K, Lenke LG, Kim YJ, et al. Analysis of the lowest instrumented vertebra following anterior spinal fusion of thoracolumbar/lumbar adolescent idiopathic scoliosis: can we predict postoperative disc wedging? Spine (Phila Pa 1976) 2005;30:418–426. doi: 10.1097/01.brs.0000153342.89478.d2. [DOI] [PubMed] [Google Scholar]
- 5.Suk S-I, Lee S-M, Chung E-R, et al. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:484–491. doi: 10.1097/01.BRS.0000048653.75549.40. [DOI] [PubMed] [Google Scholar]
- 6.Richards BS, Scaduto A, Vanderhave K, Browne R. Assessment of trunk balance in thoracic scoliosis. Spine (Phila Pa 1976) 2005;30:1621–1626. doi: 10.1097/01.brs.0000170298.89145.b4. [DOI] [PubMed] [Google Scholar]
- 7.Behensky H, Cole AA, Freeman BJ, et al. Fixed lumbar apical vertebral rotation predicts spinal decompensation in Lenke type 3C adolescent idiopathic scoliosis after selective posterior thoracic correction and fusion. Eur Spine J. 2007;16:1570–1578. doi: 10.1007/s00586-007-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dobbs MB, Lenke LG, Walton T, et al. Can we predict the ultimate lumbar curve in adolescent idiopathic scoliosis patients undergoing a selective fusion with undercorrection of the thoracic curve? Spine (Phila Pa 1976) 2004;29:277–285. doi: 10.1097/01.BRS.0000106488.51299.75. [DOI] [PubMed] [Google Scholar]
- 9.Patwardhan AG, Rimkus A, Gavin TM, et al. Geometric analysis of coronal decompensation in idiopathic scoliosis. Spine (Phila Pa 1976) 1996;21:1192–1200. doi: 10.1097/00007632-199605150-00011. [DOI] [PubMed] [Google Scholar]
- 10.Luk KD, Don AS, Chong CS. Selection of fusion levels in adolescent idiopathic scoliosis using fulcrum bending prediction: a prospective study. Spine (Phila Pa 1976) 2008;33:2192–2198. doi: 10.1097/BRS.0b013e31817bd86a. [DOI] [PubMed] [Google Scholar]


