Abstract
Selective fusion of thoracic and thoracolumbar/lumbar curves in adolescent idiopathic scoliosis is a concept critically debated in the literature. While some surgeons strongly believe that a more rigid and straighter spine provides predictably excellent outcomes, some surgeons recommend a mobile and less straight spine. This topic is a crucial part of surgical treatment of idiopathic scoliosis, particularly in young patients who will deal with the stress of the fusion mass at the proximal and distal junctions over many years. This study will review the literature on various aspects of selective fusion.
Keywords: Selective fusion, Adolescent idiopathic scoliosis, Spinal fusion, Selective thoracic fusion, Selective thoracolumbar/lumbar fusion, Spinal deformity
Introduction
The surgical treatment of adolescent idiopathic scoliosis (AIS) has made remarkable progress since the development of the Harrington rod in the late 1950s [1]. As new instrumentation was introduced over the next few decades, the ability to correct patients’ curves improved significantly. The technology has changed, but the goals of surgery for AIS remain the same: (1) halt curve progression and correct deformity, (2) maintain a balanced spine in the coronal and sagittal planes, (3) preserve as many mobile spinal segments as possible, and, (4) prevent surgical complications such as junctional kyphosis, adding-on, and revision surgery [2–11]. Since the publication of the landmark article by King et al. [12], some double major curves have been identified as containing a structural and a compensatory component. The King Type II curve is known as the “false double major” pattern, because the lumbar curve shows less magnitude and more flexibility on side-bending films which suggests that it is a compensatory curve present only to maintain coronal balance in the setting of a fixed thoracic curve. The King Type II curve was later reclassified by Lenke et al. [13–15] as Lenke 1C, 2C, 3C, and 4C curves. Controversy exists over the treatment of the compensatory lumbar curve in King Type II curves [15, 16]. Moe recommended selective fusion of the thoracic curve because the lumbar curve in a King Type II curve would undergo spontaneous correction following selective thoracic fusion [4, 12, 17–21]. Recent studies have shown that more flexible compensatory curves are able to correct spontaneously after fusion of the structural curve [3–5, 7, 10, 17, 18, 22–27]. As pedicle screws began to be used in the thoracic spine, studies showed superior curve correction with all pedicle screw constructs due to the three column fixation of pedicle screws and greater ability to translate and derotate the spine [5, 28]. Dobbs et al. [3] in 2006 found that pedicle screws allowed for better curve correction than hooks for selective thoracic fusion. The majority of spinal deformity surgeons believe that a balanced and mobile lumbar spine without progression of the lumbar curve is better than a straight and stiff lumbar spine. They feel comfortable with selective fusions for a more mobile and less corrected spine because it is also possible to extend the selective thoracic fusion to the lumbar spine in instances when the lumbar curve is progressing, although the rate of progression requiring fusion is very low in the current published literature. However, some advocated for long fusions including the major thoracic curve and compensatory lumbar curve from the upper thoracic spine to either L3 or L4 for better correction of both curves and also to diminish the risk of postoperative coronal decompensation, progression of lumbar curve, adding-on, junctional kyphosis, and eventual revision surgery. Selective fusion is a concept that has developed over this controversy and is defined in this review as isolated thoracic fusion with Lenke 1C, 2C, some 3C, and some 4C curves as well as isolated thoracolumbar/lumbar curves in Lenke 5C and some 6C curves.
One of the key features of the Lenke classification system is the ability for the classification to guide surgeons in treatment. Each Lenke curve type indicates which part of the spine should undergo fusions. In patients with Lenke Type 1C curves, only the thoracic curve should undergo fusion by classification. Yet many surgeons prefer to fuse both curves. One study showed that selective thoracic fusion was performed in 62% of patients with Lenke 1C curves [14]. This study found that both the thoracic and lumbar curves are fused in 38% of the Lenke 1C curves. This result is contradictory to the recommendations provided by the Lenke classification and thus the Lenke lumbar C modifier was termed a “rule breaker”. Another study by Newton et al. [29] showed that five AIS centers in the United States varied between 6 and 67% for selective thoracic fusions for Lenke 1C curves.
The difficulty now lies in determining which patients should undergo selective fusion and which vertebrae should be included in the fusion. There are many parameters that must be considered when evaluating a patient for selective fusion of either the main thoracic or thoracolumbar/lumbar curves including patient lifestyle and expectation as well as guidelines for selective fusion, fusion levels, amount of curve correction, and potential complications. The purpose of this study is to review the literature to determine the guidelines for selective fusion in adolescent idiopathic scoliosis.
Criteria of selective thoracic fusion
The goal of selective thoracic fusions in Lenke 1C, 2C, 3C, and 4C curves is to allow for as many mobile vertebral segments as possible while still achieving spontaneous correction of minor curves [10]. The King–Moe Type II curve is an s-shaped double curve pattern that comprised right thoracic and left lumbar curves which cross the midline (the apical vertebrae of each curve are past the midline) and the thoracic curve is equal to or larger and more rigid than the lumbar curve [12]. Moe recommended selective thoracic fusion if the lumbar curve is more flexible and smaller. Lenke and Bridwell [30] reported that the King–Moe definition of a Type II curve was not sufficient to recommend selective thoracic fusion and delineated more strict radiographic guidelines for selective thoracic fusion. Their criteria included relative apical vertebral translation, apical vertebral rotation, Cobb angle, and flexibility of the two curves as well as sagittal plane assessment of the thoracolumbar junction.
The most important factors to decide whether or not to perform selective thoracic fusion consist of patient lifestyle and clinical patient status including activity level, age, and preference to sports. Some patients such as professional dancers or athletes require more lumbar flexibility for their activity and thus require selective thoracic fusion if indicated [17, 22]. The patient and family need to understand the potential for lumbar curve progression, junctional problems, and revision surgery to extend the fusion. Physical examination such as Adams forward bending test is very important. Thoracic rotational prominence should be larger than the lumbar prominence with a scoliometer. Flexibility on thumb abduction testing is also important. If a patient is very flexible, a selective fusion may not be a good choice.
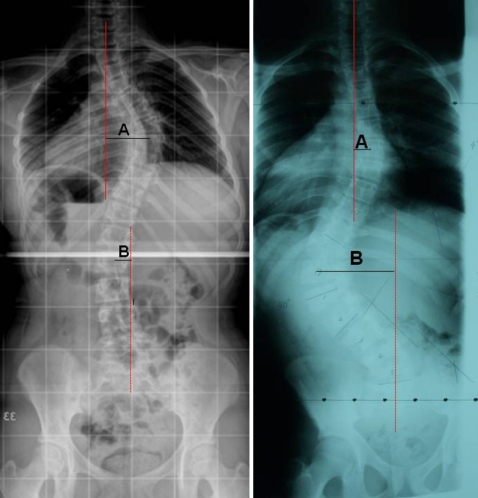
Radiographic criteria proposed by Lenke et al. are to be considered more when evaluating a patient for possible selective thoracic fusion. The thoracic apical vertebral translation (AVT) is the distance between the C-7 plumb line and the center of the apical vertebral body of the thoracic curve (Fig. 1). The thoracolumbar/lumbar AVT is the distance between the center of the apical vertebral body of the thoracolumbar/lumbar curve and the center sacral vertebral line. A ratio of thoracic AVT to thoracolumbar/lumbar AVT larger than 1.2 indicates a more translated (20% or more) thoracic curve that may be treated with selective thoracic fusion [10, 22, 31, 32]. The second factor that helps to determine if selective thoracic fusion is feasible is apical vertebral rotation (AVR). This is based on the Nash–Moe grading for vertebral rotation based on the radiographic pedicle appearance of the thoracic or thoracolumbar/lumbar apical vertebrae [33]. A ratio of thoracic AVR to thoracolumbar/lumbar AVR greater than 1.2 suggests that the thoracic curve is more rotated (20% or more) than the thoracolumbar/lumbar curve, and thus may undergo selective thoracic fusion [10, 22, 31, 32]. This radiographic rotation may be replaced by a scoliometric measurement mentioned above. The third factor is the magnitude of the curves on Cobb measurements. The thoracic Cobb angle must be larger (20% or more) than the thoracolumbar/lumbar Cobb angle by a suggested ratio of 1.2 [10, 22, 31, 32]. The lumbar curve which is non-structural with side bending to less than 25° and a sagittal kyphosis T10–L2 of less than 20° is a better candidate [13, 16]. A more flexible thoracolumbar/lumbar curve is one that will spontaneously correct upon selective fusion of the thoracic spine [22, 31]. However, Behensky et al. [34] showed relatively non-flexible thoracolumbar/lumbar curves with side bending to more than 25°, Lenke 3C curves, spontaneously correct. They found that of 21 patients in Lenke 3C curves who met 2 or 3 out of 3 of the above criteria had good postoperative coronal balance and outcomes. They did not perform selective fusion in patients with lumbar Cobb angles greater than 60°. Relative ratio of AVT is known to be the most important factor for good outcomes among the three radiographic parameters. Selective fusion of the thoracic spine is possible in Lenke 3C curves if AVT, AVR or Cobb ratio is larger [34]. A fourth variable to consider is the sagittal plane balance. The thoracolumbar junctional angle between T10 and L2 should be less than 10°. The sagittal disc angle below the instrumented vertebrae should be lordotic [15, 30]. Skeletal maturity is also important. Closure of the triradiate cartilage is very important in preventing postoperative progression of the lumbar spine and junctional decompensation [31].
Fig. 1.
The thoracic apical vertebral translation (A) is the distance between the center of the thoracic apical vertebra (A) and the C7 plumb line (solid line). The lumbar apical vertebral translation (B) is the distance between the center of the lumbar apical vertebra and central sacral vertical line (dashed line)
These various factors for selective fusion of thoracic curves are summarized in Table 1. The level of evidence for these recommendations are based on mostly level IV evidence case series studies that report outcomes after treatment as sited above. There are no studies that compare outcomes to controls nor are there randomized control trials.
Table 1.
Factors for selective fusion of thoracic curves
| Category | Criteria | Notes |
|---|---|---|
| Candidates | Lenke 1C, 2C, 3C, 4C | |
| Clinical parameters | Lifestyle and activity level | |
| Thoracic rotational prominence > lumbar prominence | ||
| Soft tissue flexibility: thumb abduction test | ||
| Radiographic parameters | ||
| Coronal plane ratio criteria |  |
Possible if AVT criteria only Better if 2 or 3 criteria met |
 |
||
 |
||
| Sagittal plane criteria | Thoracolumbar (T10–L2) kyphosis < 10° | |
| Sagittal disc angle below LIV—lordosis | ||
| Skeletal maturity | Triradiate cartilage—closed | |
| Additional criteria | TL/L side bender < 25° | Possible if TL/L side bender >25° if more criteria met |
| TL/L curve < 60° | ||
| CSL touches thoracic LEV or below | ||
AVT apical vertebral translation, AVR apical vertebral rotation, LIV lowest instrumented vertebra, TL/L thoracolumbar/lumbar, LEV lower end vertebrae
Determination of fusion levels for selective thoracic fusion
Once a patient is determined for selective fusion, the next step is to determine which levels need to be fused. Selection of the ideal lowest instrumented vertebrae (LIV) is crucial in preventing distal junctional problems such as adding-on or distal junctional kyphosis. Yet it is still important to retain as many mobile vertebral segments as possible. Goldstein [35] noted that the fusion should often be extended to the neutral vertebra to prevent future adding-on of the curve. King et al. [25] identified the stable and neutral vertebra as the appropriate area to end a fusion for false double major curve. The majority of studies have shown satisfactory outcomes when the LIV is at the stable and neutral vertebra [3, 5, 7, 17, 20, 36, 37]. One study showed a significantly increased risk of lumbar decompensation when the fusion did not end at the stable and neutral vertebra, and decompensation occurred at a rate of 22% [4].
There are some patients with Lenke 1C curves that have a significant pre-operative trunk shift toward the left side. This means that the stable vertebra by the center sacral line is located around the thoracic apex and ending the fusion construct around the thoracic apex would lead to poor outcomes. In this situation, Goldstein’s recommendation of ending the fusion at neutral or 1 vertebra distal to the neutral vertebra may be an option for selective thoracic fusion, not to extend the fusion to the lower lumbar spine and retain a mobile lumbar spine.
Other factors that contribute to LIV selection include the sagittal balance and patient skeletal maturity. A sagittal kyphosis at the thoracolumbar junction (T10–L2) of less than 20° and a lordotic disc angle below the LIV is important to prevent distal junctional kyphosis [10, 38]. Additionally, closure of the triradiate cartilage is important to prevent adding-on and distal junctional problems [36].
Selection of the uppermost instrumented vertebra (UIV) is also important for shoulder balance and proximal junctional kyphosis. The important pre-operative factors are standing shoulder balance (left high, level, and right high), structurality of the proximal thoracic curve, sagittal thoracic kyphosis at T2–T5, and instrumentation technique. If the left shoulder is high, then the UIV should be T2 in Lenke 2C curves or 2 vertebra proximal to the upper end vertebra in Lenke 1C curves [39]. Preservation of the thoracic kyphosis or an intra-operative increase of thoracic kyphosis is important to prevent proximal junctional kyphosis [40]. Surgical technique is also an important component to prevent junctional kyphosis. Distraction of the concave side of the curve rather than compression of convex side at the UIV is better to prevent proximal junctional kyphosis [41].
The amount of correction for selective thoracic fusion
Curve correction is another aspect of selective thoracic fusion that is frequently debated. Although spontaneous lumbar curve correction occurs consistently following a selective thoracic spinal fusion, the degree of correction is somewhat unpredictable. Previous studies have shown that over correction of the thoracic curve is related to progression of the lumbar curve below a selective thoracic fusion [42, 43] due to lack of compensatory lumbar curve correction [30, 44–49]. It has been hypothesized that the unfused lumbar compensatory curve cannot compensate for excessive correction of the main thoracic curve and this therefore results in coronal decompensation [8, 50, 51]. Richards et al. [8] reported less postoperative spontaneous correction of the lumbar curves than shown on pre-operative flexibility radiographs (27 compared to 70%, respectively) in King Type II curves with Cotrel–Dubousset instrumentation. The thoracic curve was corrected to 48% of pre-operative curve in this study, which may explain why the lumbar curve was unable to spontaneously correct more than 27%. Roye et al. [51] also reported significantly less correction of the lumbar curves than of the thoracic curves (38 compared to 50%, respectively). Lumbar curve magnitude or stiffness also correlates to decreased correction of the lumbar curve and lumbar curve decompensation [30, 52]. As a result of these and other studies, the pre-operative push-prone and supine lumbar radiographs were recommended as the best assessment of pre-operative flexibility imaging to predict the ideal amount of thoracic curve correction and expected spontaneous lumbar curve correction [53].
In contrast, several studies have shown spontaneous correction of the lumbar curve between 60 to 81%, which corresponded to the 61–83% correction of the thoracic curve [37, 54, 55]. They did not find a correlation between over correction of the thoracic curve and decreased spontaneous correction of the lumbar curve. One study states that newer intra-operative techniques using pedicle screws may have an enhanced capacity to control spontaneous correction of the lumbar spine which exceeds the pre-operative flexibility radiographic correction amount [37]. They have found up to 83% correction of the thoracic spine and 81% spontaneous correction of the lumbar spine when pre-operative flexibility imaging showed a spontaneous lumbar correction of 66%.
Thompson et al. [44] studied the influence of rod rotation for correction of the major curve on the secondary curve in computed tomography scans. They concluded that patients who underwent rod derotation techniques for selective fusion of the primary thoracic curve demonstrated decreased spontaneous correction of the secondary lumbar curve. This then led to a larger size of the secondary lumbar curve and later progression of this curve below their selective thoracic fusion. The rod derotation maneuver led to their reported 75% decompensation in King Type II curves. This is more common in those patients with larger and more deviated lumbar curves. However, Suk et al. [37] showed that the rod derotation maneuver did not lead decompensation.
Postoperative complications
Preservation of global coronal and sagittal balance is key to ensure good patient outcomes for all spinal deformity surgery, and coronal balance is at greater risk than sagittal balance in selective thoracic fusion. When the C7 plumb line is left of the curve pre-operatively, the coronal balance will increase to the left postoperatively since the spontaneous lumbar correction comes mostly from the proximal lumbar spine and not the distal lumbar spine [8].
Several studies examined the problem of postoperative coronal decompensation and found a prevalence of 4 to 41% [46, 51]. Poor outcomes are related with progression of the unfused lumbar curve below a selective fusion [42, 43], overcorrection of the thoracic curve [30, 44, 45], poor choice of fusion levels [42, 47, 56, 57], incorrect identification of curve patterns [30, 58], lumbar curve magnitude or stiffness [30, 52], and relative position and rotation of the apical vertebrae [30, 59]. In a study following patient outcomes with a minimum 5 years follow-up after selective thoracic fusion, the overall revision rate to accommodate worsening deformity was 6% (2/32 patients) [60]. In this study, 12 patients were considered marginal radiographic outcomes due to: 16% (5/32) with LIV more than 3 cm translation from the CSVL, 12.5% (4/32) with worsening lumbar AVT compared to pre-op, 3% (1/32) with worsening lumbar AVT compared to pre-op, 16% (5/32) with distal junctional kyphosis more than 10° increased from pre-op, and 6% (2/32) with lumbar Cobb angle more than 5° from pre-op. These results are consistent with previous reports in the literature [17, 36, 61].
Selective thoracolumbar/lumbar fusion
While the studies examining the selective fusion of thoracolumbar/lumbar curves are much fewer in number, it is no less feasible. The lack of literature on this topic may be due to the fact that extending a fusion from the lumbar spine to the thoracic spine does not lead to the same amount of motion loss as extending a fusion from the thoracic to the lumbar spine. Regardless, many of the same considerations as for selective thoracic fusion apply to selective thoracolumbar/lumbar fusions such as careful selection of fusion levels, correction amount, and potential complications. Lenke Type 5 and 6 curves are thoracolumbar/lumbar major curves with minor thoracic curves [13, 15, 16]. If the thoracic curve side bends to less than 25° and the T10–L2 kyphosis is less than 20°, it is classified as Lenke Type 5 curve and selective thoracolumbar/lumbar fusion is possible. However, even if the thoracic curve side bends to more than 25° and the T10–L2 kyphosis is more than 20° (Lenke Type 6), selective thoracolumbar/lumbar fusion is still possible if they meet the criteria.
In 2003, Sanders et al. [62] examined the criteria necessary for successful selective anterior fusion of thoracolumbar/lumbar curves. They followed 49 patients for 2 years after selective anterior thoracolumbar/lumbar fusion and determined that a thoracic curve of less than 40° was necessary for a satisfactory result. The best predictor of successful outcome was skeletal maturity as determined by the triradiate cartilage. Also predictive of a satisfactory outcome was thoracolumbar/lumbar to thoracic Cobb ratio of greater than 1.25, thoracolumbar/lumbar curve 55° or less, and/or a thoracic curve side-bending Cobb measurement of 20° or less. These factors for good outcomes after selective fusion of thoracolumbar/lumbar curves are shown in Table 2. Similar to the recommendations listed in Table 1, the studies for Table 2 are level 4 evidence based on case series reports.
Table 2.
Factors for selective fusion of thoracolumbar/lumbar curves
| Category | Criteria | Notes |
|---|---|---|
| Candidates | Lenke 5C, 6C | |
| Clinical parameters | Lifestyle and activity level | |
| Lumbar rotational prominence > thoracic prominence | ||
| Soft tissue flexibility: thumb abduction test | ||
| Radiographic parameters | ||
| Coronal plane ratio criteria |  |
Possible if AVT criteria only |
 |
Better if 2 or 3 criteria met | |
 | ||
| Sagittal plane criteria | Thoracolumbar (T10–L2) kyphosis < 10° | If UIV between T10 and L2 |
| Skeletal maturity | Triradiate cartilage—closed | |
| Additional criteria | Thoracic side bender < 25° | Possible if >25° if more criteria met |
| Thoracic curve < 40° | Possible if >40° if T10–L2 >20° if UIV ≥T10 | |
AVT apical vertebral translation, AVR apical vertebral rotation, UIV uppermost instrumented vertebra, TL/L thoracolumbar/lumbar
Schulte et al. [27] in 2006 studied the spontaneous vertebral derotation of secondary curves. They found a significant spontaneous derotation of lumbar curves after selective anterior thoracic fusion. Yet for selective anterior thoracolumbar/lumbar fusion, there was an increase in the rotation of the compensatory thoracic curve. A spontaneous thoracic correction of 36% was shown in this study. Li et al. [63] followed patients after selective lumbar fusion in Lenke 5C curves. They found an average of 57% lumbar curve correction and 26% thoracic curve correction with a minimum 2 year follow-up.
Conclusion
Selective fusion of thoracic or thoracolumbar/lumbar curves in C lumbar modifiers is a way to provide balanced curve correction while leaving the maximum number of mobile vertebral segments. The majority of studies demonstrated satisfactory outcomes based upon patient activity level, curve character such as curve magnitude, flexibility, rotation, translation and sagittal profile, and skeletal maturity. Poor patient selection, selection of the incorrect fusion levels, and inadequate correction can lead to progressive deformity, adding-on, shoulder imbalance, and worsening trunk rotation. Most of the literature on this subject comes from level 4 studies that are case series and higher level comparison studies would be beneficial to decision making. Further research is needed to evaluate the long-term outcomes of selective anterior or posterior instrumentation methods.
Conflict of interest
None.
Appendix: Case presentation
Case 1
N.P. is a 17-year-old female with idiopathic scoliosis. Pre-operative standing AP radiograph showed a right thoracic curve of 56° and a left thoracolumbar curve of 52° that bent down to 4° on side-bending films. The thoracic apical vertebral rotation was 2 and the lumbar apical vertebral rotation was 2. The thoracic apical vertebral translation was 37 mm and the lumbar apical vertebral translation was 32 mm. Pre-operative standing lateral radiograph showed thoracic kyphosis at T5–T12 7° and lumbar lordosis T12–S1 at 80°. Scoliometer measurement showed a thoracic angle of 14° and lumbar angle of 5°. She also has an L5/S1 grade 2 spondylolisthesis. She underwent selective thoracic fusion from T4–T11 and postoperative thoracic curve of 35° and lumbar curve of 29° (Fig. 2).
Fig. 2.
Selective thoracic fusion for Lenke 1CN curve
Case 2
T.F. is a 13-year-old boy with an idiopathic scoliosis. Pre-operative standing AP radiograph showed a right thoracic curve of 47° and a left thoracolumbar curve of 80°. The lumbar apical vertebral rotation at T13 was 40° and thoracic apical vertebral rotation at T7 was 5°, according to Perdriolle. The thoracic apical vertebral translation was 18 mm and the lumbar apical vertebral translation was 77 mm. The C7 plumb line was 44 mm toward the left side. Pre-operative standing lateral radiograph showed thoracic kyphosis at T5–T12 of 3°, thoracolumbar kyphosis at T10–L2 of 23°, and lumbar lordosis at T12–S1 of 42°. The left side bender of the thoracolumbar curve was 58° and the right side bender was 22°. He also had a left-side only synostosis of L5–S1. His curve is a 6C according to the Lenke classification system. He underwent posterior osteotomy at L5–S1 and selective posterior thoracolumbar instrumentation and fusion at T10–L3 and presented at 12 months follow-up with satisfactory frontal and sagittal spinal alignment (Fig. 3).
Fig. 3.
Selective thoracolumbar fusion for Lenke 6C curve
References
- 1.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Jt Surg Am. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 2.Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine. 1999;24:2607–2616. doi: 10.1097/00007632-199912150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine. 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 4.Lenke LG, Betz RR, Bridwell KH, Harms J, Clements DH, Lowe TG. Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine. 1999;24:1663–1672. doi: 10.1097/00007632-199908150-00007. [DOI] [PubMed] [Google Scholar]
- 5.Luk KDK, Don AS, Chong CS, Wong YW, Cheung KM. Selection of fusion levels in adolescent idiopathic scoliosis using fulcrum bending prediction: a prospective study. Spine. 2008;33:2192–2198. doi: 10.1097/BRS.0b013e31817bd86a. [DOI] [PubMed] [Google Scholar]
- 6.Nault M-L, Labelle H, Aubin C-E, Balazinski M. The use of fuzzy logic to select which curves need to be instrumented and fused in adolescent idiopathic scoliosis: a feasibility study. J Spinal Disord Tech. 2007;20:594–603. doi: 10.1097/BSD.0b013e318046eb30. [DOI] [PubMed] [Google Scholar]
- 7.Patel PN, Upasani VV, Bastrom TP, Marks MC, Pawelek JB, Betz RR, Lenke LG, Newton PO. Spontaneous lumbar curve correction in selective thoracic fusions of idiopathic scoliosis: a comparison of anterior and posterior approaches. Spine. 2008;33:1068–1073. doi: 10.1097/BRS.0b013e31816f6404. [DOI] [PubMed] [Google Scholar]
- 8.Richards BS. Lumbar curve response in type II idiopathic scoliosis after posterior instrumentation of the thoracic curve. Spine. 1992;17:S282–S286. doi: 10.1097/00007632-199208001-00012. [DOI] [PubMed] [Google Scholar]
- 9.Satake K, Lenke LG, Kim YJ, Bridwell KH, Blanke KM, Sides B, Steger-May K. Analysis of the lowest instrumented vertebra following anterior spinal fusion of thoracolumbar/lumbar adolescent idiopathic scoliosis: can we predict postoperative disc wedging? Spine. 2005;30:418–426. doi: 10.1097/01.brs.0000153342.89478.d2. [DOI] [PubMed] [Google Scholar]
- 10.Wang T, Xu J-G, Zeng B-F. Selective fusion in adolescent idiopathic scoliosis. Chin Med J. 2008;121:1456–1461. [PubMed] [Google Scholar]
- 11.Mok JM, Hu SS. Surgical strategies and choosing levels for spinal deformity: how high, how low, front and back. Neurosurg Clin N Am. 2007;18:329–337. doi: 10.1016/j.nec.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 12.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Jt Surg Am. 1983;65:1302–1313. [PubMed] [Google Scholar]
- 13.Lenke LG, Betz RR, Bridwell KH, Clements DH, Harms J, Lowe TG, Shufflebarger HL. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Jt Surg Am. 1998;80:1097–1106. doi: 10.2106/00004623-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Lenke LG, Betz RR, Clements D, Merola A, Haher T, Lowe T, Newton P, Bridwell KH, Blanke K. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment? Spine. 2002;27:604–611. doi: 10.1097/00007632-200203150-00008. [DOI] [PubMed] [Google Scholar]
- 15.Lenke LG, Edwards CC, 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine. 2003;28:S199–S207. doi: 10.1097/01.BRS.0000092216.16155.33. [DOI] [PubMed] [Google Scholar]
- 16.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 17.Edwards CC, 2nd, Lenke LG, Peelle M, Sides B, Rinella A, Bridwell KH. Selective thoracic fusion for adolescent idiopathic scoliosis with C modifier lumbar curves: 2- to 16-year radiographic and clinical results. Spine. 2004;29:536–546. doi: 10.1097/01.BRS.0000109992.22248.77. [DOI] [PubMed] [Google Scholar]
- 18.Ritzman TF, Upasani VV, Bastrom TP, Betz RR, Lonner BS, Newton PO. Comparison of compensatory curve spontaneous derotation after selective thoracic or lumbar fusions in adolescent idiopathic scoliosis. Spine. 2008;33:2643–2647. doi: 10.1097/BRS.0b013e3181891806. [DOI] [PubMed] [Google Scholar]
- 19.Frez R, Cheng JC, Wong EM. Longitudinal changes in trunkal balance after selective fusion of King II curves in adolescent idiopathic scoliosis. Spine. 2000;25:1352–1359. doi: 10.1097/00007632-200006010-00006. [DOI] [PubMed] [Google Scholar]
- 20.McCance SE, Winter RB, Lonstein JE. A King type II curve pattern treated with selective thoracic fusion: case report with 44-year follow-up. J Spinal Disord. 1999;12:262–265. [PubMed] [Google Scholar]
- 21.Yu B, Zhang JG, Qiu GX, Wang YP, Weng XS. Posterior selective thoracic fusion in adolescent idiopathic scoliosis. Chin Med Sci J. 2004;19:216–220. [PubMed] [Google Scholar]
- 22.Bridwell KH. Selection of instrumentation and fusion levels for scoliosis: where to start and where to stop. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:1–8. doi: 10.3171/spi.2004.1.1.0001. [DOI] [PubMed] [Google Scholar]
- 23.Jansen RC, Rhijn LW, Duinkerke E, Ooij A. Predictability of the spontaneous lumbar curve correction after selective thoracic fusion in idiopathic scoliosis. Eur Spine J. 2007;16:1335–1342. doi: 10.1007/s00586-007-0320-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuklo TR, Lenke LG, Won DS, Graham EJ, Sweet FA, Betz RR, Bridwell KH, Blanke KM. Spontaneous proximal thoracic curve correction after isolated fusion of the main thoracic curve in adolescent idiopathic scoliosis. Spine. 2001;26:1966–1975. doi: 10.1097/00007632-200109150-00006. [DOI] [PubMed] [Google Scholar]
- 25.King HA. Selection of fusion levels for posterior instrumentation and fusion in idiopathic scoliosis. Orthop Clin North Am. 1988;19:247–255. [PubMed] [Google Scholar]
- 26.Majd ME, Holt RT, Castro FP. Selection of fusion levels in scoliosis surgery. J Spinal Disord Tech. 2003;16:71–82. doi: 10.1097/00024720-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Schulte TL, Liljenqvist U, Hierholzer E, Bullmann V, Halm HF, Lauber S, Hackenberg L. Spontaneous correction and derotation of secondary curves after selective anterior fusion of idiopathic scoliosis. Spine. 2006;31:315–321. doi: 10.1097/01.brs.0000197409.03396.24. [DOI] [PubMed] [Google Scholar]
- 28.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 29.Newton PO, Faro FD, Lenke LG, Betz RR, Clements DH, Lowe TG, Haher TR, Merola AA, D’Andrea LP, Marks M, Wenger DR. Factors involved in the decision to perform a selective versus nonselective fusion of Lenke 1B and 1C (King–Moe II) curves in adolescent idiopathic scoliosis. Spine. 2003;28:S217–S223. doi: 10.1097/01.BRS.0000092461.11181.CD. [DOI] [PubMed] [Google Scholar]
- 30.Lenke LG, Bridwell KH, Baldus C, Blanke K. Preventing decompensation in King type II curves treated with Cotrel–Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine. 1992;17:S274–S281. doi: 10.1097/00007632-199208001-00011. [DOI] [PubMed] [Google Scholar]
- 31.Heary RF, Albert TJ (eds) (2007) Spinal deformities: the essentials. Thieme, New York and Stutgart
- 32.Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL. Cotrel–Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Jt Surg Am. 1992;74:1056–1067. [PubMed] [Google Scholar]
- 33.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Jt Surg Am. 1969;51:223–229. [PubMed] [Google Scholar]
- 34.Behensky H, Cole AA, Freeman BJC, Grevitt MP, Mehdian HS, Webb JK. Fixed lumbar apical vertebral rotation predicts spinal decompensation in Lenke type 3C adolescent idiopathic scoliosis after selective posterior thoracic correction and fusion. Eur Spine J. 2007;16:1570–1578. doi: 10.1007/s00586-007-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goldstein LA (1973) The surgical treatment of idiopathic scoliosis. Clin Orthop Relat Res 93 [DOI] [PubMed]
- 36.Kim YL, Lenke LG, Bridwell KH, Boachie-Adjei O, Clements J, Cho SK, Cha TD, Fischer CR (2010) Stable vertebra for surgical management of adolescent idiopathic scoliosis: how much stable is enough? Transactions of the SRS/IMAST
- 37.Suk S-I, Lee S-M, Chung E-R, Kim J-H, Kim S-S. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 38.Lowe TG, Lenke L, Betz R, Newton P, Clements D, Haher T, Crawford A, Letko L, Wilson LA (2006) Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention. Spine (Phila Pa 1976) 31:299–302. doi:10.1097/01.brs.0000197221.23109.fc [DOI] [PubMed]
- 39.Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine. 2005;30:2045–2050. doi: 10.1097/01.brs.0000179084.45839.ad. [DOI] [PubMed] [Google Scholar]
- 40.Kim YL, Lenke LG, Bridwell KH, Boachie-Adjei O, Hosogane N, Kim YB (2008) Significance of intraoperative thoracic kyphosis increase to prevent the proximal junctional kyphosis in adolescent idiopathic scoliosis following posterior segmental spinal instrumentation and fusion: a multicenter analysis of 518 cases. Transactions of the Scoliosis Research Society Annual Meeting
- 41.Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine. 2007;32:2731–2738. doi: 10.1097/BRS.0b013e31815a7ead. [DOI] [PubMed] [Google Scholar]
- 42.Bridwell KH, McAllister JW, Betz RR, Huss G, Clancy M, Schoenecker PL. Coronal decompensation produced by Cotrel–Dubousset “derotation” maneuver for idiopathic right thoracic scoliosis. Spine (Phila Pa 1976) 1991;16:769–777. doi: 10.1097/00007632-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 43.Kalen V, Conklin M. The behavior of the unfused lumbar curve following selective thoracic fusion for idiopathic scoliosis. Spine (Phila Pa 1976) 1990;15:271–274. doi: 10.1097/00007632-199004000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel–Dubousset instrumentation of idiopathic scoliosis. Spine. 1990;15:927–931. doi: 10.1097/00007632-199009000-00017. [DOI] [PubMed] [Google Scholar]
- 45.Arlet V, Marchesi D, Papin P, Aebi M. Decompensation following scoliosis surgery: treatment by decreasing the correction of the main thoracic curve or “letting the spine go”. Eur Spine J. 2000;9:156–160. doi: 10.1007/s005860050227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mason DE, Carango P. Spinal decompensation in Cotrel–Dubousset instrumentation. Spine (Phila Pa 1976) 1991;16:394–403. doi: 10.1097/00007632-199108001-00018. [DOI] [PubMed] [Google Scholar]
- 47.Moore MR, Baynham GC, Brown CW, Donaldson DH, Odom JA., Jr Analysis of factors related to truncal decompensation following Cotrel–Dubousset instrumentation. J Spinal Disord. 1991;4:188–192. doi: 10.1097/00002517-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 48.Sar C, Hamzaoglu A, Talu U et al (1995) Selection of fusion levels in surgical treatment of King type II curves. Orthop Trans 16:642 (abstract)
- 49.Lackum WH, Miller JP. Critical observations of the results in the operative treatment of scoliosis. J Bone Jt Surg Am. 1949;31A:102–106. [PubMed] [Google Scholar]
- 50.Richards BS, Birch JG, Herring JA, Johnston CE, Roach JW. Frontal plane and sagittal plane balance following Cotrel–Dubousset instrumentation for idiopathic scoliosis. Spine (Phila Pa 1976) 1989;14:733–737. doi: 10.1097/00007632-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 51.Roye DP, Jr, Farcy JP, Rickert JB, Godfried D. Results of spinal instrumentation of adolescent idiopathic scoliosis by King type. Spine (Phila Pa 1976) 1992;17:270–273. doi: 10.1097/00007632-199208001-00010. [DOI] [PubMed] [Google Scholar]
- 52.McCall RE, Bronson W. Criteria for selective fusion in idiopathic scoliosis using Cotrel–Dubousset instrumentation. J Pediatr Orthop. 1992;12:475–479. doi: 10.1097/01241398-199207000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Dobbs MB, Lenke LG, Walton T, Peelle M, Della Rocca G, Steger-May K, Bridwell KH. Can we predict the ultimate lumbar curve in adolescent idiopathic scoliosis patients undergoing a selective fusion with undercorrection of the thoracic curve? Spine (Phila Pa 1976) 2004;29:277–285. doi: 10.1097/01.BRS.0000106488.51299.75. [DOI] [PubMed] [Google Scholar]
- 54.Goshi K, Boachie-Adjei O, Moore C, Nishiyama M. Thoracic scoliosis fusion in adolescent and adult idiopathic scoliosis using posterior translational corrective techniques (Isola): is maximum correction of the thoracic curve detrimental to the unfused lumbar curve? Spine J. 2004;4:192–201. doi: 10.1016/j.spinee.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 55.Chang KW, Chang KI, Wu CM. Enhanced capacity for spontaneous correction of lumbar curve in the treatment of major thoracic-compensatory C modifier lumbar curve pattern in idiopathic scoliosis. Spine (Phila Pa 1976) 2007;32:3020–3029. doi: 10.1097/BRS.0b013e31815cdde3. [DOI] [PubMed] [Google Scholar]
- 56.Knapp DR, Jr, Price CT, Jones ET, Coonrad RW, Flynn JC. Choosing fusion levels in progressive thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1992;17:1159–1165. doi: 10.1097/00007632-199210000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Puno RM, Grossfeld SL, Johnson JR, Holt RT. Cotrel–Dubousset instrumentation in idiopathic scoliosis. Spine (Phila Pa 1976) 1992;17:258–262. doi: 10.1097/00007632-199208001-00008. [DOI] [PubMed] [Google Scholar]
- 58.King HA. Analysis and treatment of type II idiopathic scoliosis. Orthop Clin North Am. 1994;25:225–237. [PubMed] [Google Scholar]
- 59.Patwardhan AG, Rimkus A, Gavin TM, Bueche M, Meade KP, Bielski R, Ibrahim K. Geometric analysis of coronal decompensation in idiopathic scoliosis. Spine (Phila Pa 1976) 1996;21:1192–1200. doi: 10.1097/00007632-199605150-00011. [DOI] [PubMed] [Google Scholar]
- 60.Chang MS, Bridwell KH, Lenke LG, Cho W, Baldus CR, Auerbach JD, Crawford CH, O’Shaughnessy BA (2009) Predicting the outcome of selective thoracic fusion in false double major lumbar “C” cases with five to 15 year follow-up. Transactions of the Scoliosis Research Society Annual Meeting [DOI] [PubMed]
- 61.Lowe TG, Lenke L, Betz R, Newton P, Clements D, Haher T, Crawford A, Letko L, Wilson LA. Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention. Spine. 2006;31:299–302. doi: 10.1097/01.brs.0000197221.23109.fc. [DOI] [PubMed] [Google Scholar]
- 62.Sanders AE, Baumann R, Brown H, Johnston CE, 2nd, Lenke LG, Sink E. Selective anterior fusion of thoracolumbar/lumbar curves in adolescents: when can the associated thoracic curve be left unfused? Spine. 2003;28:706–713. doi: 10.1097/01.BRS.0000051925.88443.85. [DOI] [PubMed] [Google Scholar]
- 63.Li M, Ni J, Fang X, Liu H, Zhu X, He S, Gu S, Wang X. Comparison of selective anterior versus posterior screw instrumentation in Lenke 5C adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2009;34:1162–1166. doi: 10.1097/BRS.0b013e31819e2b16. [DOI] [PubMed] [Google Scholar]