Abstract
Bracing is an established method of conservative treatment for adolescent idiopathic scoliosis and kyphosis. Compliance among adolescents is frequently inadequate due to the discomfort of wearing a brace, cosmetic issues, and fear on the part of patients and parents that bracing may reduce everyday physical activities. The aim of this prospective, controlled study was to objectify the impact of spinal bracing on daily step activity in patients receiving conservative treatment for adolescent idiopathic scoliosis (AIS) or adolescent kyphosis (AK). Forty-eight consecutive patients (mean age 13.4 ± 2.3 years), consisting of 38 AIS patients (33 girls, 5 boys) and 10 AK patients (6 girls, 4 boys) were included. Once the decision to carry out bracing had been taken and while the patients were waiting for the individual brace to be built, step activity was assessed without braces by means of step activity monitoring (SAM) for seven consecutive days. After 8 weeks of brace wearing, step activity was assessed during regular brace treatment, again for seven consecutive days. In addition, brace-wearing times were simultaneously recorded using temperature probes implanted in the braces to measure compliance. Before and during brace treatment, patients completed the Scoliosis Research Society (SRS-22) questionnaire. The SAM was worn for an average of 12.7 ± 1.5 h/day during the first measurement and 12.3 ± 1.9 h on average during the second measurement. The mean gait cycles (GCs) per day and per hour before treatment were 5,036 ± 1,465 and 395 ± 105, respectively. No significant reduction in step activity was found at the follow-up measurement during bracing, at 4,880 ± 1,529 GCs/day and 403 ± 144 GCs/h. Taking the 23-h recommended time for brace wearing as a basis (100%), patients wore the brace for 72.7 ± 27.6% of the prescribed time, indicating an acceptable level of compliance. Girls showed a higher compliance level (75.6 ± 25.6%) in comparison with boys (56.7 ± 31.9%), although the difference was not significant (P = 0.093). The SRS-22 total score showed no differences between the two measurements (2.57 ± 0.23 vs. 2.56 ± 0.28). Implementing a simultaneous and objective method of assessing step activity and brace-wearing times in everyday life proved to be feasible, and it expands the information available regarding the impact of bracing on patients’ quality of life. The results clearly show that brace treatment does not negatively interfere with daily step activity in AIS and AK patients. This is an important finding that should help reduce patients’ and parents’ worries concerning bracing.
Keywords: Step activity monitoring (SAM), Bracing, Compliance, Idiopathic adolescent scoliosis, Idiopathic adolescent kyphosis
Introduction
Basically, there are three treatment options for preventing curve progression in patients with adolescent idiopathic scoliosis (AIS) and adolescent kyphosis (AK), including therapeutic exercising, bracing, and surgery [26]. The appropriate choice depends on the type of curve and the severity of the deformity. Scoliosis bracing is an accepted treatment in skeletally immature, adolescent patients with Cobb curvatures ranging approximately between 20° and 40°–50° [4, 12]. The primary aim in conservative scoliosis management for adolescents is to prevent curvature progression and secondary health implications associated with the spinal deformity and ultimately to avoid the need for later surgery [11, 45].
AK (Scheuermann’s disease) is characterized by a flexible hyperkyphosis at the beginning of the disease, and during progression by a rigid thoracic or thoracolumbar hyperkyphosis, which is commonly seen in boys [1, 31]. With the exception of very progressive cases, the treatment is conservative with a brace and is aimed at stabilizing and correcting the deformity [33].
The efficacy of bracing in scoliosis as well as kyphosis is still being questioned [10, 18, 34], although it has become established as the most effective nonsurgical method of treatment for mild to moderate AIS and AK [16]. The success of conservative treatment by means of bracing largely depends on compliance on the part of the patients, and continuous wearing of the brace on a regular basis is therefore essential [13, 15, 34]. Reasons for nonadherence are various and include, among others, wearing discomfort, cosmetic aspects when the rather bulky brace is being worn, and in particular a fear of reduced trunk muscle strength and restrictions in everyday physical activities. Little is known about the effect of bracing on gait or step activity in everyday life outside laboratory conditions.
In view of the importance of regular physical activities in childhood and adolescence, on the one hand, and serious concerns on the part of patients and parents on the other, the aim of the present study was to objectively assess daily step activity in scoliosis and kyphosis patients receiving brace therapy. The technique of step activity monitoring by accelerometry was used, as this is the best available method for studying step activity in everyday life for a continuous and prolonged period.
The reliability and validity of step activity monitoring have been confirmed in several clinical investigations [2, 23]. In this study, step activity on seven consecutive days was correlated with brace-wearing times, which was objectively quantified by means of temperature sensors inside the brace. This method makes it possible to measure step activity during brace wearing, as well as nonadherence times, and it provides information about changes in activity behavior when the braces are discarded. This combination of long-term activity measurement in a nonlaboratory setting along with an objective assessment of brace-wearing compliance has not previously been reported in the literature.
The study hypothesis was that bracing reduces everyday physical activities. Therefore, the aim of this prospective, nonrandomized study was to assess the patients’ step activity before treatment and during brace wearing, in order to examine the effect of brace treatment on daily step activity. Subsequently, step activity during brace treatment was evaluated in relation to activities performed with the brace and activities without the brace, in order to determine whether patients become more active when they discard the brace.
Materials and methods
Approval for the study was obtained from the local Ethics Committee (registration no. 2007-497-f-S) and the parents and patients provided written informed consent to participation. Patients with an indication for conservative treatment by means of spinal braces were eligible to participate in this prospective, controlled study if they met the following inclusion criteria: (1) a diagnosis of thoracic or thoracolumbar AIS with Cobb angles of 20°–50°; or (2) a diagnosis of AK with a Stagnara angle(Th4–12) of 50°–70°, or a thoracolumbar kyphosis angle (Th10–L2) of more than 20°, or extraordinarily large vertebral defects (Schmorl’s nodes or similar defects) meaning an increased risk of kyphosis progression hence justifying brace treatment even if the Stagnara angle is below 50° or the thoracolumbar kyphosis angle is below 20°. Exclusion criteria were: (1) Cobb angles less than 20° or more than 50° in AIS, or Stagnara angles less than 50° or more than 70°; and (2) injury to or surgery in the lower extremity within 3 months before participation in the study. From a total of 70 consecutive patients who met the inclusion criteria and were asked to participate in the study, complete data records were obtained for 48 patients. Reasons for drop-outs were: loss of step activity monitors (SAM) on return shipment (n = 3); completion or continuation of treatment in another institution (n = 4); refusal due to weather conditions (n = 1); decision in favor of surgery (n = 1); loss of motivation to participate between the initial and follow-up measurements (n = 10); and inability of the patient to remove the temperature sensor from the brace (n = 3).
A pedometer-based uniaxial accelerometer was used to assess daily step activity (StepWatch™ 3.0 Activity Monitor, SAM, Orthocare Innovations, Oklahoma City, Oklahoma, USA) (Fig. 1). This piezoelectric device is an ankle-worn monitor for recording gait cycles (GCs; one GC = two steps) per day and per hour (GC/day divided by monitor-wearing time), and for movement intensities (e.g., the average number of GCs/min), with a storage capacity of several weeks. One-minute periods of data recording were used to assess step activity. Previous studies have documented the validity and reliability of this monitor in children and adolescents [21, 23]. The SAM was also used in a previous study to evaluate step activity in lumbar spine patients [36], justifying its application in spine patients. It carries out measurements without providing feedback to the patient, thus minimizing test bias. A monitoring period of 7 days is required in order to produce an acceptable estimate of daily step activity in children and adolescents and to account for significant differences in weekday and weekend activity [38].
Fig. 1.
TheStepWatch Activity Monitor (SAM)
The first measurement was performed before brace therapy was started. When the patients presented for the first time and an indication for bracing had been established, braces were constructed on an individual basis in the university’s specialized technical department. Production usually takes about 4–6 weeks. During this period, the first step activity measurement was performed for a period of seven consecutive days. The second measurement was initiated after 8 weeks of regular continuous brace wearing, when the patients presented at the outpatient clinic for the first check-up examination. Step activity and brace-wearing times were assessed simultaneously for a further seven consecutive days.
Daily step activity was evaluated using average GCs/day. Furthermore, average GCs/h were determined (GCs divided by monitor-wearing time). As compliance levels are assumed to vary widely between patients, step activity during brace wearing was evaluated separately from activities performed without the brace during the follow-up measurement. This method was intended to demonstrate whether patients discarded the brace in order to become more active, or whether their habitual step activity patterns in everyday life do not differ during brace wearing. Using 1-min periods for data recording made it possible to measure GCs/min and hence average movement intensities. This was carried out in order to compare the first and second measurements and also to compare average movement intensities for adherence and nonadherence periods during follow-up measurements. For this analysis, only those minutes including step activity were included (total GCs/day divided by total minutes above zero GCs/min). In addition, step activity above 40 GCs/min was also evaluated, as it indicates continuous walking [35].
Brace-wearing times were determined using a temperature sensor (Proges Plus, Willems, France) embedded in the Chêneau brace above the anterior superior iliac spine. The size of the Proges Plus Thermobutton is 1.6 × 0.6 cm. To measure brace-wearing times using the temperature sensors in everyday life, 3-min periods of data recording and a resolution of 0.5°C were used, allowing storage capacity of 17 consecutive days. Preliminary investigations showed that the Thermobutton reacts immediately to temperature changes and makes it possible to clearly distinguish brace-wearing times from nonadherence times [25]. We selected 28°C as a threshold temperature for distinguishing between brace-wearing and non-wearing times, in accordance with a previous study by Helfenstein et al. [13].
AIS patients were treated with a Chêneau brace and AK patients with a kyphosis brace (Fig. 2a–f). The Chêneau brace (or CTM brace = Chêneau–Toulouse–Münster brace) was developed by Dr. Chêneau 1981 in France and introduced to Germany by Dr. Matthias in Münster [30]. The brace acts on a three-point pressure principle to correct the deformity via rib hump and lumbar hump without limiting respiratory movements. The kyphosis brace was developed on the basis of the Milwaukee brace, however modified, in order to act on a three-point principle applying pressure from posterior to the kyphosis counteracting from anterior via chest and pelvis.
Fig. 2.
The Chêneau (scoliosis) brace (a–c) and the kyphosis brace (d–f) (developed on the basis of the Milwaukee brace)
Patients were instructed to wear the SAM during waking hours and to wear the brace for 23 h a day, corresponding to the best compliance level (23 h = 100%). Patients were allowed to and encouraged to perform sports and exercises during the time of brace treatment without any restrictions [17]. In addition, they had physiotherapy once a week on a regular basis [9, 43, 44]. Patients were allowed to discard the brace while exercising, swimming, and during personal hygiene activities.
The patients also completed the German version of the Scoliosis Research Society (SRS-22) questionnaire, which has recently been validated [29]. This evaluation was carried out at the same time as the step activity assessment, once before and once during brace treatment, in order to register changes in health-related quality of life. The SRS-22 questionnaire consists of five domains, covering function/activity (five questions), pain (five questions), self-image (five questions), mental health (five questions), and satisfaction with management (two questions). The higher the score in each domain, the higher the patient’s level of satisfaction.
Statistical analyses were performed using the PASW Statistics 18 package (SPSS Inc., Chicago, Illinois, USA) and included Kolmogorov–Smirnov testing, the t test for paired samples, and the Wilcoxon and Mann–Whitney U test for parametric and nonparametric tests, respectively. Descriptive statistical analyses included means, standard deviations, and 95% confidence intervals (CIs). Bland–Altman plots [3] were used to assess changes in step activity between the initial and follow-up measurements.
Results
A total of 38 AIS and 10 AK patients were included in the study. The 39 girls and 9 boys had mean ages of 12.9 ± 2.3 and 15.2 ± 1.0 years, respectively. Their anthropometric data are presented in Table 1.
Table 1.
Patients’ characteristics
| AIS (n = 38, 33 females, 5 males) Mean ± SD (95% CI) |
AK (n = 10, 6 females, 4 males) Mean ± SD (95% CI) |
|
|---|---|---|
| Age (at presentation) | 13.1 ± 2.4 (12.3/13.9) | 14.5 ± 1.1 (13.7/15.3) |
| Height (m) | 1.63 ± 0.1 (1.59/1.67) | 1.75 ± 0.1 (1.69/1.80) |
| Weight (kg) | 52.1 ± 13.7 (47.6/56.7) | 64.2 ± 13.6 (54.5/73.9) |
| BMI (kg/m2) | 19.4 ± 3.7 (18.1/20.6) | 20.9 ± 3.6 (18.4/23.5) |
AIS adolescent idiopathic scoliosis, AK adolescent kyphosis, BMI body mass index, CI confidence intervals, SD standard deviation
Five AIS patients had a double major curve, and 19 patients had a thoracic curve. A thoracolumbar curve was noted in 14 patients. The mean Cobb angle of the primary curves before brace treatment was 28.3° ± 8.9°, while secondary curves had a mean Cobb angle of 22.3° ± 12.7°. In AK patients, eight patients had a thoracic hyperkyphosis of 59.2° ± 8.3° (thoracolumbar kyphosis 5.4° ± 16.0°), one patient had a thoracolumbar hyperkyphosis of 42.9° (thoracic kyphosis of 44.0°) and one patient had a thoracolumbar hyperkyphosis of 13.0° (thoracic kyphosis of 35.0°) with severe thoracolumbar structural defects due to the Scheuermann’s disease and the necessity to prevent thoracolumbar kyphosis progression due to these large defects.
Figure 3 shows an example of the simultaneous objective assessment of step activity using accelerometry and brace-wearing times in everyday life. The patients wore the SAM during both measurements in similar proportions, for 12.7 ± 1.5 and 12.3 ± 1.9 h/day, respectively. The results of the SAM measurements are shown in Table 2. While the mean step activity per day decreased by 157 ± 1,412 GCs between the two measurements, step activity in relation to daily monitor-wearing time increased by 7.9 ± 107 GCs/h (Fig. 4). GCs/min were also slightly increased in the second SAM measurement, as was the percentage time spent in activities above 40 GCs/min, indicating continuous walking. However, daily step activity did not differ significantly for any of the evaluated parameters between the pretreatment and follow-up measurements.
Fig. 3.
Example illustrating a female adolescent idiopathic scoliosis patient, with simultaneous objective assessment of step activity (4,896 gait cycles) and compliance (84.3%, or 20.4 h of brace-wearing time) during 1 day. When the brace is taken off, the temperature drops below the threshold level of 28°C and immediately approximates to room temperature. Brace-wearing times can therefore clearly be distinguished from times when the brace is not worn
Table 2.
Changes in step activity among patients with adolescent idiopathic scoliosis (AIS) and adolescent kyphosis (AK) between the pretreatment and follow-up measurements
| Baseline, mean ± SD (95% CI) | During brace treatment, mean ± SD (95% CI) | P valuea | |
|---|---|---|---|
| GCs/day | 5,036 ± 1,465 (4,611/5,462) | 4,879 ± 1,529 (4,436/5,323) | n.s. |
| GCs/h | 395 ± 105 (365/426) | 403 ± 144 (362/445) | n.s. |
| GCs/min | 14.6 ± 2.4 (13.9/15.3) | 14.9 ± 2.4 (14.2/15.6) | n.s. |
| >40 GCs/min (%) | 2.2 ± 1.1 (1.9/2.6) | 2.3 ± 1.1 (1.9/2.60) | n.s. |
GC gait cycles, SD standard deviation, CI confidence intervals
at test for paired samples
Fig. 4.
A Bland–Altman plot indicating individual changes in daily step activity, measured by mean gait cycles (GCs) per hour between pretreatment (m1) and follow-up measurements (m2). The mean difference (m2 − m1) was +7.9 ± 106.9 GCs/h. A mark above the mean indicates greater step activity during the second measurement. The dashed lines represent means for differences ±2 SD
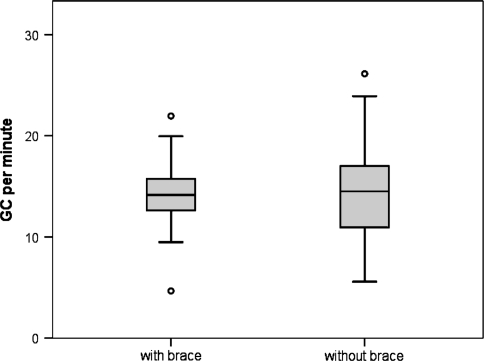
In the follow-up measurements, 33% (95% CI, 25.5/41.4) of the total GCs were performed without the brace, while 67% (95% CI, 58.6/74.5) were performed during brace wear. Figure 5 compares step activity patterns using GCs/min for activities during brace wearing and activities performed without the brace during the second measurement. No significant differences between the two conditions were observed.
Fig. 5.
Comparison of mean gait cycles (GCs) per minute during the follow-up measurements. GCs performed while wearing the brace: 14.5 ± 4.4 GCs/min (95% CI 13.2–15.8) and GCs performed without the brace: 14.2 ± 3.1 (95% CI 13.3–15.1). The difference was not significant (Mann–Whitney U test). The box plots represent the median, 25th and 75th percentiles, 1.5 interquartile range (IQR), and outliers
Female patients had an average of 4,986 ± 1,193 GCs/day during the pretreatment measurements and 4,901 ± 1,561 GCs/day during the follow-up measurements. GCs/h increased slightly from 394 ± 93–396 ± 133. During the follow-up measurements, movement intensities were nearly identical, at 14.1 ± 3.2 GCs/min during brace-wearing times and 14.2 ± 4.5 GC/min when the brace was discarded (not significant).
In the male patients, step activity decreased from 5,254 ± 2,405 to 4,786 ± 1,462 GCs/day, while GCs/h increased from 400 ± 154 to 433 ± 190. During the follow-up measurement, male patients had higher movement intensities when they discarded the brace (15.9 ± 4.0 GCs/min). However, the difference from brace-wearing times, with an average of 14.6 ± 2.5 GCs/min, was not significant.
Similar results were found when the two diagnostic groups were compared. Step activity decreased in AIS patients between the pretreatment and follow-up measurements from 5,069 ± 1,453 to 4,988 ± 1,528 GCs/day and increased from 397 ± 106 to 403 ± 137 GCs/h (neither difference significant). During the follow-up measurements, AIS patients had slightly, but not significantly, reduced movement intensities at 14.3 ± 2.8 GCs/min when wearing the brace in comparison with 14.7 ± 4.3 GCs/min at times when the brace was discarded.
In AK patients, a reduction in daily step activity from 4,913 ± 1,586 to 4,469 ± 1,539 GCs/day was observed, but an increase from 390 ± 106 to 403 ± 175 GCs/h. During the follow-up measurements, movement intensities were lower during brace-wearing times in comparison with periods when the AK patients discarded the brace (13.7 ± 4.1 vs. 14.0 ± 5.1). Again, none of these comparisons showed any statistically significant differences.
Overall, the mean brace-wearing time was 16 h and 43 min, corresponding to a compliance rate of 72.7 ± 27.6% relative to the 23 h of recommended wearing time (equivalent to 100%). Compliance levels were higher, but not significantly increased, in female patients (75.6 ± 25.6%) in comparison with males (56.7 ± 31.9%). No significant differences in compliance levels were observed between the AIS patient group (74.1 ± 27.2%) and AK patients (64.5 ± 28.9%).
The results of the SRS-22 questionnaire are summarized in Table 3. There were no significant differences in the total score between the two measurements (2.57 ± 0.23 vs. 2.56 ± 0.28). Only the score for satisfaction with management decreased significantly (P < 0.01) between the baseline (2.57 ± 0.32) and assessment during brace therapy (1.89 ± 0.84).
Table 3.
Pretreatment and follow-up mean scores from the SRS questionnaire for all patients
| Baseline, mean ± SD (95% CI) | During brace treatment, mean ± SD (95% CI) | P valuea | |
|---|---|---|---|
| Function | 3.17 ± 0.40 (3.05/3.30) | 3.37 ± 0.39 (3.25/3.49) | 0.004 |
| Pain | 1.95 ± 0.31 (1.86/2.05) | 2.02 ± 0.30 (1.93/2.11) | n.s. |
| Image | 2.54 ± 0.61 (2.34/2.73) | 2.74 ± 0.69 (2.53/2.95) | n.s. |
| Mental health | 2.80 ± 0.31 (2.70/2.90) | 2.78 ± 0.21 (2.71/2.84) | n.s. |
| Management | 2.35 ± 1.16 (1.95/2.67) | 1.89 ± 0.84 (1.64/2.14) | 0.005 |
| Total | 2.57 ± 0.32 (2.47/2.67) | 2.56 ± 0.28 (2.48/2.64) | n.s. |
SD standard deviation, CI confidence intervals
at test for paired samples
Three patients and their parents were not able to remove the temperature sensor from the brace, but no other technical problems were noted. Records from the SAM device and temperature probes were downloaded and synchronized without difficulties after the measurements, delivering data that can be easily processed.
Discussion
At the beginning of the investigation, the study hypothesis was that due to anxieties on the part of patients and parents, bracing reduces daily step activity. The results clearly show that this hypothesis is incorrect. This is an important argument in the field of conservative treatment for spinal deformities, and the evidence can be used in discussions with patients and parents both during, and in particular before, treatment with braces.
Physical activity
As regular PA is a prerequisite for health, well-being and quality of life in children and adolescents, the study evaluated the impact of spinal bracing on daily step activity in AIS and AK patients. The results show that bracing does not interfere with habitual step activities in everyday life.
None of the parameters investigated—i.e., overall step activity, expressed as GCs/day and GCs/h, nor average movement intensities, expressed as GCs/min, nor the percentage of step activity above 40 GCs/min—was significantly reduced in AIS and AK patients during brace treatment in comparison with the baseline measurements (Table 2). Movement intensities, expressed as average GCs/min with and without the brace in the follow-up measurements, did not differ significantly either (Fig. 5). A significant change in this parameter would have indicated altered activity behavior, with patients who discard the brace most probably becoming more active. However, the results show that this assumption could not be confirmed. Further analyses for subgroups—i.e., female compared with male patients and AIS patients compared with AK patients—also showed no significant differences in step activity.
Although brace treatment had no impact on habitual activities, the overall mean step activity before and during brace treatment, at 5,036 ± 1,465 and 4,879 ± 1,529 GCs/day, respectively, was lower in AIS and AK patients in comparison with the expected values for healthy peers, at 6,000–8,000 GCs/day in boys and 5,000–7,000 GCs/day in girls [39].
A recent study measured step activity using GCs per hour and per day with the SAM in 9- to 11-year-old schoolchildren [41]. Overall, step activity per day in the study was clearly decreased in AIS and AK patients at 5,036 ± 1,465 GCs and 4,879 ± 1,529 GCs in comparison with healthy school children at 8,336 ± 1,608 GCs/day. Step activity in the healthy children, at 657 ± 113 GCs/h, was clearly higher than in the AIS and AK patients included in the study, at 395 ± 105 and 403 ± 144 GCs/h, respectively.
Although it has to be taken into account that these control individuals (aged 9 and 11 years) were clearly younger than the patients in the present study (13.4 ± 2.3 years) and therefore likely to be more active in daily life, these studies indicate that step activity in AIS and AK patients is already reduced before brace treatment. The reasons for reduced daily activities are difficult to determine. During brace treatment, AIS and AK patients do not generally experience pain that might negatively influence their habitual activities. It can be assumed that modified gait in AIS patients, demonstrated in the laboratory setting [19, 46], which is accompanied by increased oxygen consumption [20], restricts everyday physical activities in adolescent patients.
Compliance
Conservative treatment using braces is currently a matter of controversy, as this treatment option largely depends on compliance on the part of the patients [32]. Objective checking of compliance using technical solutions, as in the present study, may be a way of addressing the difficulties that have been reported in the past with the subjective patient information given in interviews or questionnaires regarding brace-wearing times, as such methods are known to be biased and unreliable [8]. This objective checking is a relevant issue in the present study. Although the objective assessment of brace-wearing times using compliance monitors has been carried out in various studies [13, 27, 28, 32, 37], this is the first one that has combined compliance monitoring with an objective assessment of step activity in everyday life.
Evaluations of the effectiveness of treatment with orthopedic orthoses should be based on objective measurements of actual compliance [37, 42]. It may be a matter of opinion whether it is reasonable and justifiable to incorporate tools such as the Thermobutton into braces in everyday clinical practice. In the present authors’ view, this solution cannot be recommended for everyday clinical practice. Patients might feel wary, and the mutual trust needed for the confidential patient–doctor relationship might be negatively affected by the use of objective checking tools. However, such tools are extremely valuable for scientific studies.
The overall compliance rate in this study was 72.7 ± 27.6%, taking the 23-h recommended wearing time as a basis (100%). Compliance levels were thus higher than the 47–68% rates reported in previous studies [13, 22, 27] and comparable to those described by Takemitsu et al. at 75% [37], using compliance monitors. However, the average monitoring periods in these other studies ranged from 5 weeks to 17 months, considerably longer than the assessment periods in the present study. Due to the prolonged duration of monitoring, increased time periods for data recording were also used in these studies, ranging from 10 to 16 min and thus reducing the temporal resolution [22, 27, 37] (with the exception of the study conducted by Helfenstein et al. [13], which used 2-min periods). It is important to note that compliance monitoring in the present study was performed after 8 weeks of brace wearing for 7 consecutive days and thus at the beginning of conservative treatment. It is conceivable that adherence to wearing recommendations might decline over time, although the longitudinal results presented by Morton et al. [22] did not reveal such effects. Previous results showing lower compliance levels in male AIS patients in comparison with female ones [14] were confirmed in the present study, although the differences between the two groups were not significant. The mismatch might be attributable to the discrepancy in age between the two groups, as the female patients were on average 2.3 years younger than males, and compliance is known to correlate negatively with age [22, 27, 37].
SRS-22 questionnaire
With regard to quality of life, the results of the SRS-22 questionnaire show a significant increase in the domain of function/activity and a significant reduction in the domain of satisfaction with management. The scores presented—especially for satisfaction with management (2.25 ± 1.16 at baseline and 1.89 ± 0.84 during brace treatment) are clearly lower in comparison with other studies with scores of 3.8 ± 0.70 in 109 AIS patients after completion of treatment [5] and 3.55–4.03 in 46 AIS patients receiving brace treatment, depending on the size of the Cobb angles [7]. It is important to note that the scores reported in these publications were calculated in patients at an average of 24 and 27 months, respectively, after the start of brace treatment. The AIS and AK patients in the present study completed the SRS-22 questionnaire shortly after the diagnosis (baseline) and only 8 weeks after starting brace treatment. It is possible that satisfaction with management in the present study declined significantly because the patients are not yet familiar at this early stage of treatment with either the diagnosis or their braces, so that anxieties, uncertainty, and dissatisfaction may significantly affect the health-related quality of life in AIS and AK patients. However, the study by Bunge et al. [5] confirmed that in patients treated with braces, the score for satisfaction with management was significantly lower in comparison with patients treated with braces and surgery, or with surgery alone.
Feasibility
This study demonstrates that it is feasible to implement a simultaneous objective assessment of step activity and brace-wearing time in AIS and AK patients. No technical problems with regard to data processing were encountered. However, three patients experienced problems with removing the temperature probes from the brace. No restrictions caused by wearing the devices were reported, so that the patients’ everyday activities were not affected by the monitors. It can be concluded that the simultaneous application of the devices proved to be successful. This new method can therefore be recommended for future scientific studies evaluating step activity and compliance in adolescent spine patients.
Limitations
One possible limitation of this study concerns the assessment of physical activity in everyday life with the ankle-worn SAM. By definition, physical activity is defined as any bodily movement produced by skeletal muscles resulting in energy expenditure [6]. As the SAM is an ankle-worn device, it can only assess stepping, and activities with the upper extremity are ignored. In addition, no detailed information regarding energy expenditure is available. However, there are currently no methods capable of assessing every single aspect of daily step activity [24]. Step activity also accounts for approximately 80% of overall physical activity in everyday life [40]. With its demonstrated validity and reliability, this makes the SAM an appropriate tool for assessing physical activity in everyday life.
The compliance monitoring period in this study was also fairly short, so that only limited conclusions can be drawn regarding treatment adherence. However, the aim of the present study was to evaluate the impact of spinal bracing on daily step activity. The relatively long assessment period of 7 days using accelerometry is longer than that used in most comparable investigations on activity measurement, and the technique is an established method in the literature [25, 36, 38].
Conclusions
The results of this study indicate that bracing does not interfere with daily step activity in AIS and AK patients in relation to GCs per day or per hour, nor does it interfere with movement intensities, shown as GCs/min. However, overall step activity in these patients is already reduced before bracing therapy in comparison with healthy peers. Compliance levels in this study were slightly higher than those previously reported in the literature. The results also demonstrate the feasibility of this new approach, with simultaneous assessment of brace-wearing times and step activity in everyday life.
Acknowledgments
No financial support was provided by DePuy Spine.
Conflict of interest The authors hereby state that there were no financial conflicts of interest in relation to any of the companies mentioned in this paper.
Footnotes
C. Müller and K. Fuchs share authorship.
References
- 1.Arlet V, Schlenzka D. Scheuermann’s kyphosis: surgical management. Eur Spine J. 2005;14:817–827. doi: 10.1007/s00586-004-0750-0. [DOI] [PubMed] [Google Scholar]
- 2.Bjornson KF, Belza B, Kartin D, Logsdon R, McLaughlin JF. Ambulatory physical activity performance in youth with cerebral palsy and youth who are developing typically. Phys Ther. 2007;87:248–257. doi: 10.2522/ptj.20060157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 4.Bulthuis GJ, Veldhuizen AG, Nijenbanning G. Clinical effect of continuous corrective force delivery in the non-operative treatment of idiopathic scoliosis: a prospective cohort study of the TriaC-brace. Eur Spine J. 2008;17:231–239. doi: 10.1007/s00586-007-0513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bunge EM, Juttmann RE, Kleuver M, Biezen FC, Koning HJ, NESCIO group Health-related quality of life in patients with adolescent idiopathic scoliosis after treatment: short-term effects after brace or surgical treatment. Eur Spine J. 2007;16:83–89. doi: 10.1007/s00586-006-0097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung KM, Cheng EY, Chan SC, Yeung KW, Luk KD. Outcome assessment of bracing in adolescent idiopathic scoliosis by the use of the SRS-22 questionnaire. Int Orthop. 2007;31:507–511. doi: 10.1007/s00264-006-0209-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 9.Mauroy J, Weiss H, Aulisa A, Aulisa L, Brox J, Durmala J, Fusco C, Grivas T, Hermus J, Kotwicki T, Le Blay G, Lebel A, Marcotte L, Negrini S, Neuhaus L, Neuhaus T, Pizzetti P, Revzina L, Torres B, Loon P, Vasiliadis E, Villagrasa M, Werkman M, Wernicka M, Wong M, Zaina F. 7th SOSORT consensus paper: conservative treatment of idiopathic and Scheuermann’s kyphosis. Scoliosis. 2010;5:9. doi: 10.1186/1748-7161-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976) 2007;32:S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 11.Heary RF, Bono CM, Kumar S. Bracing for scoliosis. Neurosurgery. 2008;63:125–130. doi: 10.1227/01.NEU.0000320387.93907.97. [DOI] [PubMed] [Google Scholar]
- 12.Heary RF, Madhavan K. Genetics of scoliosis. Neurosurgery. 2008;63:222–227. doi: 10.1227/01.NEU.0000320384.93384.28. [DOI] [PubMed] [Google Scholar]
- 13.Helfenstein A, Lankes M, Ohlert K, Varoga D, Hahne HJ, Ulrich HW, Hassenpflug J. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine. 2006;31:339–344. doi: 10.1097/01.brs.0000197412.70050.0d. [DOI] [PubMed] [Google Scholar]
- 14.Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine. 2001;26:2001–2005. doi: 10.1097/00007632-200109150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Katz DE, Durrani AA. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2001;26:2354–2361. doi: 10.1097/00007632-200111010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Korovessis P, Zacharatos S, Koureas G, Megas P. Comparative multifactorial analysis of the effects of idiopathic adolescent scoliosis and Scheuermann kyphosis on the self-perceived health status of adolescents treated with brace. Eur Spine J. 2007;16:537–546. doi: 10.1007/s00586-006-0214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liljenqvist U, Witt KA, Bullmann V, Steinbeck J, Volker K. Recommendations on sport activities for patients with idiopathic scoliosis. Sportverletz Sportschaden. 2006;20:36–42. doi: 10.1055/s-2005-859029. [DOI] [PubMed] [Google Scholar]
- 18.Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine (Phila Pa 1976) 2007;32:S115–S119. doi: 10.1097/BRS.0b013e3181354501. [DOI] [PubMed] [Google Scholar]
- 19.Mahaudens P, Banse X, Mousny M, Detrembleur C. Gait in adolescent idiopathic scoliosis: kinematics and electromyographic analysis. Eur Spine J. 2009;18:512–521. doi: 10.1007/s00586-009-0899-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahaudens P, Detrembleur C, Mousny M, Banse X (2009) Gait in adolescent idiopathic scoliosis: energy cost analysis. Eur Spine J10.1007/s00586-009-1002-0 [DOI] [PMC free article] [PubMed]
- 21.McDonald CM, Widman L, Abresch RT, Walsh SA, Walsh DD. Utility of a step activity monitor for the measurement of daily ambulatory activity in children. Arch Phys Med Rehabil. 2005;86:793–801. doi: 10.1016/j.apmr.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Morton A, Riddle R, Buchanan R, Katz D, Birch J. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2008;28:336–341. doi: 10.1097/BPO.0b013e318168d154. [DOI] [PubMed] [Google Scholar]
- 23.Mudge S, Stott NS. Test-retest reliability of the StepWatch Activity Monitor outputs in individuals with chronic stroke. Clin Rehabil. 2008;22:871–877. doi: 10.1177/0269215508092822. [DOI] [PubMed] [Google Scholar]
- 24.Müller C, Winter C, Rosenbaum D. Current objective techniques for physical activity assessment in comparison with subjective methods. Dtsch Z Sportmed. 2010;61:11–18. [Google Scholar]
- 25.Müller C, Winter C, Klein D, Damaske K, Schmidt C, Schulte T, Bullmann V, Rosenbaum D. Objective assessment of brace wear times and physical activities in two patients with scoliosis. Biomed Tech (Berl) 2010;55:117–120. doi: 10.1515/BMT.2010.026. [DOI] [PubMed] [Google Scholar]
- 26.Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, Kotwicki T, Maruyama T, Romano M, Vasiliadis ES (2010) Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev (1):CD006850. 10.1002/14651858.CD006850.pub2 [DOI] [PubMed]
- 27.Nicholson GP, Ferguson-Pell MW, Smith K, Edgar M, Morley T. The objective measurement of spinal orthosis use for the treatment of adolescent idiopathic scoliosis. Spine. 2003;28:2243–2250. doi: 10.1097/01.BRS.0000085098.69522.52. [DOI] [PubMed] [Google Scholar]
- 28.Nicholson GP, Ferguson-Pell MW, Smith K, Edgar M, Morley T. Quantitative measurement of spinal brace use and compliance in the treatment of adolescent idiopathic scoliosis. Stud Health Technol Inform. 2002;91:372–377. [PubMed] [Google Scholar]
- 29.Niemeyer T, Schubert C, Halm HF, Herberts T, Leichtle C, Gesicki M. Validity and reliability of an adapted german version of scoliosis research society-22 questionnaire. Spine (Phila Pa 1976) 2009;34:818–821. doi: 10.1097/BRS.0b013e31819b33be. [DOI] [PubMed] [Google Scholar]
- 30.Pham VM, Herbaux B, Schill A, Thevenon A. Evaluation of the Cheneau brace in adolescent idiopathic scoliosis] Ann Readapt Med Phys. 2007;50:125–133. doi: 10.1016/j.annrmp.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 31.Poolman RW, Been HD, Ubags LH. Clinical outcome and radiographic results after operative treatment of Scheuermann’s disease. Eur Spine J. 2002;11:561–569. doi: 10.1007/s00586-002-0418-6. [DOI] [PubMed] [Google Scholar]
- 32.Rahman T, Bowen JR, Takemitsu M, Scott C. The association between brace compliance and outcome for patients with idiopathic scoliosis. J Pediatr Orthop. 2005;25:420–422. doi: 10.1097/01.bpo.0000161097.61586.bb. [DOI] [PubMed] [Google Scholar]
- 33.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976) 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 34.Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Jt Surg Am. 1997;79:664–674. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Sawamura C, Hornicek FJ, Gebhardt MC. Complications and risk factors for failure of rotationplasty: review of 25 patients. Clin Orthop Relat Res. 2008;466:1302–1308. doi: 10.1007/s11999-008-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schulte TL, Schubert T, Winter C, Brandes M, Hackenberg L, Wassmann H, Liem D, Rosenbaum D, Bullmann V. Step activity monitoring in lumbar stenosis patients undergoing decompressive surgery. Eur Spine J. 2010;19:1855–1864. doi: 10.1007/s00586-010-1324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Takemitsu M, Bowen JR, Rahman T, Glutting JJ, Scott CB. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine. 2004;29:2070–2074. doi: 10.1097/01.brs.0000138280.43663.7b. [DOI] [PubMed] [Google Scholar]
- 38.Trost SG. Objective measurement of physical activity in youth: current issues, future directions. Exerc Sport Sci Rev. 2001;29:32–36. doi: 10.1097/00003677-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Tudor-Locke C, McClain JJ, Hart TL, Sisson SB, Washington TL. Expected values for pedometer-determined physical activity in youth. Res Q Exerc Sport. 2009;80:164–174. doi: 10.1080/02701367.2009.10599550. [DOI] [PubMed] [Google Scholar]
- 40.Tudor-Locke CE, Myers AM. Methodological considerations for researchers and practitioners using pedometers to measure physical (ambulatory) activity. Res Q Exerc Sport. 2001;72:1–12. doi: 10.1080/02701367.2001.10608926. [DOI] [PubMed] [Google Scholar]
- 41.Uhlenbrock K, Thorwesten L, Sandhaus M, Fromme A, Brandes M, Rosenbaum D, Dieterich S, Völker K. Physical education and daily life activity of nine and eleven year-old pupils. Dtsch Z Sportmed. 2008;59:228–233. [Google Scholar]
- 42.Vandal S, Rivard CH, Bradet R. Measuring the compliance behavior of adolescents wearing orthopedic braces. Issues Compr Pediatr Nurs. 1999;22:59–73. doi: 10.1080/014608699265293. [DOI] [PubMed] [Google Scholar]
- 43.Weiss HR. Conservative treatment of idiopathic scoliosis with physical therapy and orthoses. Orthopade. 2003;32:146–156. doi: 10.1007/s00132-002-0430-x. [DOI] [PubMed] [Google Scholar]
- 44.Weiss HR. The Schroth scoliosis-specific back school—initial results of a prospective follow-up study] Z Orthop Ihre Grenzgeb. 1995;133:114–117. doi: 10.1055/s-2008-1039421. [DOI] [PubMed] [Google Scholar]
- 45.Weiss HR, Negrini S, Rigo M, Kotwicki T, Hawes MC, Grivas TB, Maruyama T, Landauer F, (SOSORT guideline committee) Indications for conservative management of scoliosis (guidelines) Scoliosis. 2006;1:5. doi: 10.1186/1748-7161-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong MS, Cheng CY, Ng BK, Lam TP, Sin SW, Lee-Shum LF, Chow HK, Tam YP. The effect of rigid versus flexible spinal orthosis on the gait pattern of patients with adolescent idiopathic scoliosis. Gait Posture. 2008;27:189–195. doi: 10.1016/j.gaitpost.2007.03.007. [DOI] [PubMed] [Google Scholar]