Abstract
Objectives. To describe primary care management of knee pain, in relation to National Institute for Health and Clinical Excellence (NICE) OA guidelines, and examine variation in management by patient characteristics.
Methods. Subjects were 755 adults aged ≥50 years who responded to baseline and 3-year surveys and had consulted primary care for knee pain. Medical records (1997–2006) were searched. Associations of having interventions from the outer circle (adjunctive treatments or Step 3) of the NICE guidelines with self-reported socio-demographic and knee-specific factors were determined.
Results. Eighty per cent had received a Step 3 intervention. Thirty-eight per cent had been referred to secondary care, and 10% had received a knee replacement. Forty-three per cent had been prescribed an opioid and 41% an NSAID. Severe knee pain or disability at baseline and follow-up was the main association with receiving a Step 3 intervention [adjusted odds ratio (OR) 2.26; 95% CI 1.38, 3.70] and with referral (OR 2.57; 95% CI 1.72, 3.83). Older patients were less likely to be referred. Although non-significant, those of higher social class, in more affluent areas, older age or overweight or obese, appeared more likely to receive a knee replacement. Fifty per cent of those reporting severe knee pain or disability in both surveys had not been referred to secondary care.
Conclusion. Most of the older adults who consult primary care with knee pain receive at least one Step 3 intervention from the OA guidelines. Inequalities in the management and referral of knee problems in primary care were generally not observed, although there were some trends towards differences in likelihood of total knee replacement.
Keywords: Inequalities, Knee osteoarthritis, Knee pain, Referral, Primary care, Socio-economic factors, Medical records, Access to care
Introduction
People from lower socio-economic backgrounds have a higher prevalence of morbidity including arthritis [1], and may have more need for care. Inequality in access occurs when non-need variables (e.g. social class) affect the use of health care, and when individuals with the same needs (e.g. pain levels) consume different amounts of care [2]. Equity in access to services for musculoskeletal pain is highlighted in US, European and UK publications. These recommend that evidence-based interventions should be available to all who need them [3], health disparities in OA treatment should be identified and that current practice is reviewed in light of treatment guidelines [4]. Specifically, primary care should review referral procedures for ease of access to secondary care and rehabilitation services and referral to specialist services should be timely and appropriate [5].
OA is the most common form of arthritis. By 2020, OA is predicted to be the fourth largest cause of disability [6]. The knee is the most commonly affected joint, and is particularly important because of its contribution to disability. People with OA require a continuum of health services and access to high-quality, effective and timely advice [5, 7] and a model for assessment and management of OA in primary care exists [8]. This model outlines treatments in the order in which they should be considered. It has an inner circle (or Step 1) of core treatments to be considered for everyone (including exercise, advice and weight loss), paracetamol and topical NSAIDs are outlined in the second circle (or Step 2) for consideration alongside the core treatments. The outer circle of adjunctive treatments (or Step 3) is to be considered when further treatment is needed (e.g. prescriptions for Cox-2 inhibitors and opioids, and referral for surgery).
Few studies have investigated whether socio-economic factors influence initial General Practitioner (GP) consultation for knee pain. Findings overall suggest little effect [9–13]. In contrast, studies have reported disparities in the provision of joint replacement surgery [14–18]. This pattern, where people with lower socio-economic status report equal or increased access to primary care services but encounter barriers at later treatment stages is reported for access to care for cardiovascular problems and cancer [19]. Studying primary care management may help to understand this conundrum. We have studied management and referral for knee pain to explore if and where unequal opportunities for care develop in the pathway before knee replacement surgery.
Primary care management for OA has been studied to a limited extent using self-reported data [20–22]. These suggest an under utilization of core treatments for OA. The few studies investigating relationships with referral to secondary care for joint pain have tended to be small in size, have relied on self-reported data (which may be subject to recall bias), had low response rates or have not assessed the role of socio-economic factors [9, 21, 23–25]. There were two aims to our study (i) To describe management of knee pain in primary care alongside Step 3 of National Institute for Health and Clinical Excellence (NICE) guidelines for the management of OA in primary care [8]. We have focussed on Step 3 as these should be comprehensibly recorded in medical records. (ii) To examine variation in management by socio-economic and deprivation characteristics, and by self-reported severity of knee pain. We wanted to explore if inequalities observed previously for total joint replacement also existed in more conservative management options or whether management appears more driven by severity of pain.
Patients and methods
We linked self-reported survey data with 10-year primary and secondary care NHS medical records. The study was set within a larger study of knee pain [11, 26, 27]. Everyone aged ≥50 years registered at three general practices in North Staffordshire, UK, were sent a questionnaire in 2000. Those who responded and still registered with the practices were sent a follow-up questionnaire 3 years later. Both questionnaires included the knee pain screening tool (KNEST) [28] to identify knee pain and related health-care use in the past 12 months. Subjects were also asked whether they consented to viewing of their medical records. North Staffordshire Local Research Ethics Committee approved the study.
Identification of participants
Subjects were selected who: (i) responded to both baseline and follow-up surveys; (ii) consented to medical record review; (iii) reported knee pain on the follow-up survey; (iv) either self-reported a GP consultation for knee pain at baseline or follow-up, or had a recorded GP consultation for knee pain between 1997 and 2004; and (v) were still alive and registered at the practice at the end of 2006.
We defined a recorded GP consultation as an entry in the general practice computerized database in the study period. The practices undergo a cycle of assessment, feedback and training in the use of computerized morbidity Read coding [29]. Read codes are a commonly used morbidity coding system in the UK [30]. GPs can add information about a consultation (free text) alongside the code. Read-coded information and consultation text for consultations were searched to identify all consultations which had an allocated knee-related Read code or a musculoskeletal-related knee disorder mentioned in the text of the consultation.
Medical record review
While evidence of GP consultation was assessed for the period 1997–2004, the review of medical records for management were for the period 1997–2006. This period enabled a reasonable length of time for a course of management in primary care to be undertaken for all primary care consulters including those who had first consulted recently. Two searches of medical records for that period were made:
all selected participants had their complete GP records manually searched at their practice for information relating to all management of their knee pain including prescribed medication at the time of a consultation for knee pain, referral to secondary care or physiotherapy, surgery, injections, X-rays and OA or RA diagnoses; and
following the search of the primary care records, all those who had evidence of referral to secondary care for knee pain had their notes at the local hospital, including the local orthopaedic service, and the letters database at the local rheumatology service searched for contacts relating to the knee.
The manual searches were conducted by three research nurses and a health services researcher using a standardized protocol and an electronic data collection sheet. Reliability of data extraction was tested initially on 31 sets of GP records. Once all data had been extracted, the reason for medication and other management was linked to the NICE OA guidelines algorithm by an experienced GP (M.P.).
Survey self-report measures
Respondents who reported knee pain on the surveys completed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [31]. Severe knee pain or disability was defined as reporting severe or extreme on at least one item on the pain scale or severe or extreme difficulty on at least one item on the physical function scale. Subjects who did not report any severe or extreme problem and answered at least 4 of the 5 pain items and 14 of the 17 physical function items were rated non-severe. Persistent knee pain was defined as reporting knee pain in both the baseline and 3-year surveys. Persistent severe knee pain or disability was defined as reporting severe knee pain or disability in both surveys. We did not use the WOMAC stiffness scale. Also included was the Hospital Anxiety and Depression scale (HADS) [32]. Subjects scoring above the upper tertile of scores on the anxiety scale or depression scale were rated as being most anxious or depressed.
A body manikin for shading pain that has occurred in the past 4 weeks was used to determine pain elsewhere (hip, lower back, foot/ankle, hand or neck). Self-reported height and weight at baseline were used to determine BMI. A BMI of >25 was defined as overweight and ≥30 as obese. Demographic variables included co-habiting status, further education after leaving school, and household social-economic class based on current or last job [33].
Area deprivation was determined using the index of multiple deprivation (IMD) 2004 for England [34]. The index is based geographically at the lower level super output area (SOA) of which there are 32 482 in England with a mean population of 1500. The IMD has an overall score, based on a weighted combination of seven domains: income; employment; health; education, skills and training; barriers to housing and services; crime; and living environment. The SOAs from which the people in this study were drawn were categorized into three groups: the least deprived 20%, the most deprived 20% and the mid 60% [34, 35].
Statistical analysis
The proportion of primary care consulters having each management option within Step 3 of the guidelines were determined first with 95% CIs. Rates were adjusted using direct age and gender standardization to the England and Wales population.
The outcome measures for assessment of social inequalities were: (i) any intervention from Step 3 during the 10-year period; (ii) referral to rheumatology or orthopaedics; and (iii) evidence of a total knee replacement (TKR). Unadjusted associations between independent variables and each outcome were assessed and factors with a P < 0.05, or an odds ratio (OR) >1.30 or <0.77 [11, 36] were taken forward alongside age and gender into the multivariable analysis using logistic regression.
Results
Participants
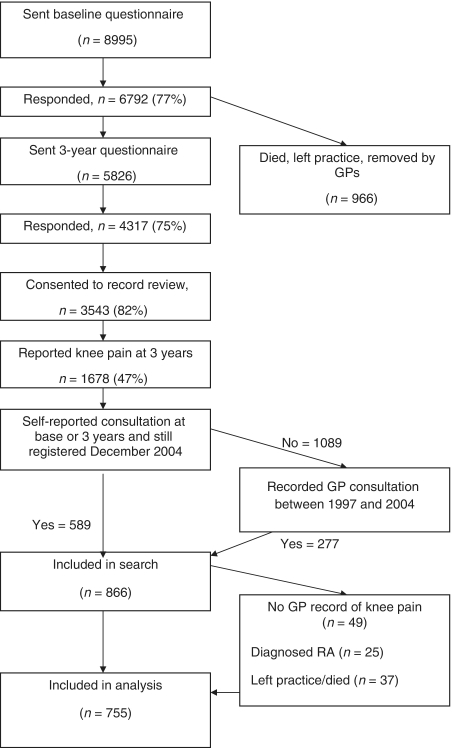
The flowchart of participants through the study is shown in Fig. 1. Response at baseline was slightly higher in females (79%) than males (75%, P < 0.001) and responders were slightly older than non-responders (mean difference 1.5 years, 95% CI 1.0, 2.0). At follow-up survey, those who responded and consented to medical record review were no different to non-responders and non-consenters by gender or age, but were slightly more likely to report knee pain at baseline (48 vs 45%, P = 0.03).
Fig. 1.
Flowchart detailing course of participants in the study.
A total 1678 people self-reported knee pain in the follow-up survey and consented to record review. Of those, 755 (45%) had an identified primary care consultation for knee pain and were included in the analysis (Fig. 1). Four hundred and fifty-one (60%) were females and the mean (s.d.) age was 67.5 (9.06) years. Six hundred and eleven (83%) also reported knee pain at baseline (persistent knee pain). Two hundred and sixty-eight (35%) reported severe pain at both time points (persistent severe knee pain). An OA diagnosis was recorded for 375 (50%) patients. Standardized rates of primary care consultation between 1997 and 2004 were 59% in those with knee pain, 66% in those reporting with persistent knee pain and 79% in those reporting persistent severe knee pain or disability.
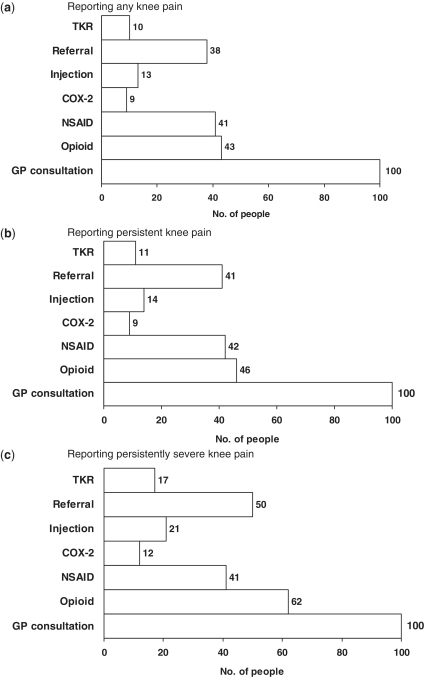
Ten-year management of knee pain
The use of interventions for those consulting primary care is shown in Table 1 with standardized rates in Fig. 2. The standardized rates are essentially unchanged from the unstandardized rates. For every 100 people consulting for knee pain, 80 had at least one intervention from Step 3 of the NICE guidelines. Of these, 43 had an opioid prescription, 41 an NSAID, 9 received a Cox-2 inhibitor, 38 were referred to secondary care and 10 received a TKR during the 10-year period (26% of those who had a referral record). Of those with a TKR, 29 (38%) had the replacement before the follow-up survey.
Table 1.
Recorded management
| Recorded management | n | % (95% CI) |
|---|---|---|
| Patients reviewed | 755 | |
| Management from Step 3 of NICE guidelines | 607 | 80 (77, 83) |
| Referral (orthopaedic or rheumatology) | 290 | 38 (35, 42) |
| Injection | 105 | 14 (12, 17) |
| Opioid prescribeda | 328 | 43 (40, 47) |
| NSAID prescribeda | 309 | 41 (37, 44) |
| Cox-2 inhibitor prescribeda | 71 | 9 (8, 12) |
| Capsaicin prescribeda | 23 | 3 (2, 5) |
| TKRb | 76 | 10 (8, 12) |
| In those without TKR (n = 679) | ||
| Referral (orthopaedic or rheumatology) | 214 | 31 (28, 35) |
| Referral (physiotherapy) | 247 | 36 (33, 40) |
| X-ray performed | 320 | 47 (43, 51) |
aAt time of a consultation for knee problem. bOn waiting list or performed.
Fig. 2.
Health-care management in 100 older adults consulting primary care with knee pain.
The figures are similar but slightly higher when restricting the analysis to just those with persistent knee pain (whether severe or not). In those with persistent severe knee pain or disability, 87 out of every 100 consulters received a Step 3 intervention, 62 were prescribed opioids, 50 were referred and 17 had a TKR. However, rates of NSAID use did not differ between those with persistent severe knee pain or disability and those with non-severe pain or disability (P = 0.34).
Associations with receiving a Step 3 intervention
Due to the similarity in the use of interventions of those with persistent knee pain to the entire group, we concentrated on severity as our measure of knee pain. There were elevated, although non-significant, relationships with two socio-economic factors: not going on to further education (adjusted OR 1.55; 95% CI 0.90, 2.69), and living in the most deprived areas (adjusted OR 1.46; 95% CI 0.64, 3.37) (Table 2). However, the only significant association with management at the highest level of the NICE guidelines was reporting severe knee pain or disability at baseline and follow-up (adjusted OR 2.26; 95% CI 1.38, 3.70 compared with not reporting severe pain or disability in either survey).
Table 2.
Associations with an intervention from NICE guidelines for OA Step 3
| Patient characteristics | Total | Step 3 management, n (%) | OR (95% CI) | ORa (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Male | 304 | 236 (78) | 1.00 | 1.00 |
| Female | 451 | 371 (82) | 1.34 (0.93, 1.92) | 1.21 (0.83, 1.78) |
| Ageb, years | ||||
| 53–64 | 310 | 242 (71) | 1.00 | 1.00 |
| 65–74 | 265 | 217 (82) | 1.27 (0.84, 1.92) | 1.24 (0.81, 1.92) |
| ≥75 | 180 | 148 (82) | 1.30 (0.81, 2.07) | 1.18 (0.70, 1.97) |
| Practice | ||||
| A | 281 | 224 (80) | 1.00 | – |
| B | 240 | 191 (80) | 0.99 (0.65, 1.52) | |
| C | 234 | 192 (82) | 1.16 (0.75, 1.81) | |
| Further education | ||||
| Yes | 86 | 61 (71) | 1.00 | 1.00 |
| No | 644 | 527 (82) | 1.85 (1.11, 3.06) | 1.55 (0.90, 2.69) |
| Unknown | 25 | 19 (76) | 1.30 (0.46, 3.63) | 1.06 (0.34, 3.32) |
| Cohabiting | ||||
| Yes | 555 | 441 (79) | 1.00 | – |
| No | 192 | 159 (83) | 1.25 (0.81, 1.91) | |
| Socio-economic class | ||||
| Managerial/professional | 225 | 178 (79) | 1.00 | – |
| Intermediate | 166 | 133 (80) | 1.11 (0.65, 1.75) | |
| Routine/manual | 321 | 261 (81) | 1.15 (0.75, 1.76) | |
| Unknown | 43 | 35 (81) | 1.16 (0.50, 2.66) | |
| Area deprivationc | ||||
| Least | 219 | 174 (79) | 1.00 | 1.00 |
| Mid | 468 | 373 (80) | 1.02 (0.68, 1.51) | 0.90 (0.59, 1.38) |
| Most | 68 | 60 (88) | 1.94 (0.87, 4.35) | 1.46 (0.64, 3.37) |
| BMId | ||||
| Normal/underweight | 161 | 122 (76) | 1.00 | 1.00 |
| Overweight | 345 | 275 (80) | 1.26 (0.80, 1.96) | 1.10 (0.69, 1.76) |
| Obese | 244 | 206 (84) | 1.73 (1.05, 2.86) | 1.38 (0.81, 2.33) |
| Anxious or depressede | ||||
| No | 338 | 265 (78) | 1.00 | – |
| Yes | 416 | 341 (82) | 1.25 (0.87, 1.80) | |
| Pain elsewheref,g | ||||
| No | 114 | 86 (75) | 1.00 | 1.00 |
| Baseline or follow-up | 219 | 177 (81) | 1.37 (0.80, 2.36) | 1.21 (0.68, 2.14) |
| Both baseline and follow-up | 422 | 344 (82) | 1.44 (0.88, 2.35) | 1.07 (0.63, 1.82) |
| Unilateral knee paine,g | 271 | 205 (76) | 1.00 | 1.00 |
| Bilateral knee pain | 474 | 395 (83) | 1.61 (1.11, 2.33) | 1.35 (0.91, 2.00) |
| Non-severe knee pain | 281 | 202 (72) | 1.00 | 1.00 |
| Severe baseline or follow-up | 206 | 169 (82) | 1.79 (1.15, 2.78) | 1.57 (0.98, 2.49) |
| Severe baseline and follow-up | 268 | 236 (88) | 2.88 (1.84, 4.53) | 2.26 (1.38, 3.70) |
Numbers may not add to 755 due to missing data. aAdjusted for other presented variables; bat follow-up survey; cbased on SOA, divided into 20% of SOAs least deprived and 20% of SOAs most deprived; dbased on the largest BMI recorded at baseline and follow-up survey; eat baseline or follow-up survey; fhip, low back, foot/ankle, hand, neck; gself-report.
Associations with referral to orthopaedics or rheumatology
Those aged ≥75 years were less likely to be referred to secondary care (adjusted OR 0.63; 95% CI 0.41, 0.95) (Table 3). However, there appeared little influence of other socio-economic variables in the decision to refer. The strongest associations with referral were reporting severe knee pain or disability at both baseline and follow-up (adjusted OR 2.57; 95% CI 1.72, 3.83 compared with not reporting severe pain or disability at either time point) and reporting severe knee pain or disability in one but not both surveys (adjusted OR 1.68; 95% CI 1.12, 2.52).
Table 3.
Associations with referral to rheumatology or orthopaedics
| Patient characteristics | Total | Referral, n (%) | OR (95% CI) | ORa (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Male | 304 | 106 (35) | 1.00 | 1.00 |
| Female | 451 | 184 (41) | 1.29 (0.95, 1.74) | 1.21 (0.88, 1.66) |
| Ageb, years | ||||
| 53–64 | 310 | 122 (39) | 1.00 | 1.00 |
| 65–74 | 265 | 105 (40) | 1.01 (0.72, 1.41) | 0.96 (0.67, 1,36) |
| ≥75 | 180 | 63 (35) | 0.83 (0.57, 1.22) | 0.63 (0.41, 0.95) |
| Practice | ||||
| A | 281 | 99 (35) | 1.00 | – |
| B | 240 | 97 (40) | 1.25 (0.87, 1.78) | |
| C | 234 | 94 (40) | 1.23 (0.86, 1.77) | |
| Further education | ||||
| Yes | 86 | 34 (40) | 1.00 | – |
| No | 644 | 249 (39) | 0.96 (0.61, 1.53) | |
| Unknown | 25 | 7 (28) | 0.60 (0.23, 1.58) | |
| Cohabiting | ||||
| Yes | 555 | 214 (39) | 1.00 | – |
| No | 192 | 73 (38) | 0.98 (0.70, 1.37) | |
| Socio-economic class | ||||
| Managerial/professional | 225 | 93 (41) | 1.00 | – |
| Intermediate | 166 | 60 (36) | 0.80 (0.53, 1.21) | |
| Routine/manual | 321 | 121 (38) | 0.86 (0.61, 1.22) | |
| Unknown | 43 | 16 (37) | 0.84 (0.43, 1.65) | |
| Area deprivationc | ||||
| Least | 219 | 76 (35) | 1.00 | – |
| Mid | 468 | 190 (41) | 1.29 (0.92, 1.80) | |
| Most | 68 | 24 (35) | 1.03 (0.58, 1.82) | |
| BMId | ||||
| Normal/underweight | 161 | 56 (35) | 1.00 | 1.00 |
| Overweight | 345 | 132 (38) | 1.16 (0.79, 1.72) | 1.01 (0.67, 1.52) |
| Obese | 244 | 100 (41) | 1.30 (0.86, 1.97) | 0.91 (0.59, 1.41) |
| Anxious or depressede | ||||
| No | 338 | 107 (32) | 1.00 | 1.00 |
| Yes | 416 | 183 (44) | 1.70 (1.26, 2.29) | 1.38 (1.00, 1.91) |
| Pain elsewheref,g | ||||
| No | 114 | 40 (35) | 1.00 | – |
| Baseline or follow-up | 219 | 81 (37) | 1.09 (0.68, 1,74) | |
| Both baseline and follow-up | 422 | 169 (40) | 1.24 (0.80, 1.90) | |
| Unilateral knee paine,g | 271 | 89 (33) | 1.00 | 1.00 |
| Bilateral knee pain | 474 | 197 (42) | 1.45 (1.06, 1.99) | 1.16 (0.83, 1.62) |
| Non-severe knee pain | 281 | 75 (27) | 1.00 | 1.00 |
| Severe baseline or follow-up | 206 | 79 (38) | 1.71 (1.16, 2.51) | 1.68 (1.12, 2.52) |
| Severe baseline and follow-up | 268 | 136 (51) | 2.83 (1.98, 4.04) | 2.57 (1.72, 3.83) |
Numbers may not add to 755 due to missing data. aAdjusted for other presented variables; bat follow-up survey; cbased on SOA, divided into 20% of SOAs least deprived and 20% of SOAs most deprived; dbased on largest BMI recorded at baseline and follow-up survey; eat baseline or follow-up survey; fhip, low back, foot/ankle, hand, neck; gself-report.
Association with TKR
Reporting severe knee pain or disability at both time points (adjusted OR 7.08; 95% CI 3.22, 15.58) was strongly related to a record of TKR, as was reporting severe knee pain or disability at one time point (adjusted OR 3.99; 95% CI 1.76, 9.04) (Table 4). Although non-significant, there was suggestion with elevated ORs that those of higher social class, living in more affluent areas, of older age or overweight or obese, were more likely to receive a replacement.
Table 4.
Associations with knee replacement
| Patient characteristics | Total | TKR, n (%) | OR (95% CI) | ORa (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Male | 304 | 26 (9) | 1.00 | 1.00 |
| Female | 451 | 50 (11) | 1.33 (0.81, 2.19) | 1.21 (0.71, 2.07) |
| Ageb, years | ||||
| 53–64 | 310 | 21 (7) | 1.00 | 1.00 |
| 65–74 | 265 | 27 (10) | 1.56 (0.86, 2.83) | 1.43 (0.76, 2.68) |
| ≥75 | 180 | 28 (16) | 2.54 (1.39, 4.61) | 1.84 (0.95, 3.56) |
| Practice | ||||
| A | 281 | 34 (12) | 1.00 | 1.00 |
| B | 240 | 22 (9) | 0.73 (0.42, 1.29) | 0.70 (0.38, 1.27) |
| C | 234 | 20 (9) | 0.68 (0.38, 1.21) | 0.65 (0.33, 1.27) |
| Further education | ||||
| Yes | 86 | 8 (9) | 1.00 | – |
| No | 644 | 66 (10) | 1.11 (0.52, 2.41) | |
| Unknown | 25 | 2 (8) | 0.85 (0.17, 4.27) | |
| Cohabiting | ||||
| Yes | 555 | 58 (10) | 1.00 | – |
| No | 192 | 18 (9) | 0.89 (0.51, 1.55) | |
| Socio-economic class | ||||
| Managerial/professional | 225 | 24 (11) | 1.00 | 1.00 |
| Intermediate | 166 | 11 (7) | 0.59 (0.28, 1.25) | 0.48 (0.22, 1.07) |
| Routine/manual | 321 | 35 (11) | 1.02 (0.59, 1.78) | 0.84 (0.46, 1.55) |
| Unknown | 43 | 6 (14) | 1.36 (0.52, 3.55) | 0.80 (0.28, 2.27) |
| Area deprivationc | ||||
| Least | 219 | 25 (11) | 1.00 | 1.00 |
| Mid | 468 | 48 (10) | 0.89 (0.53, 1.48) | 0.96 (0.54, 1.71) |
| Most | 68 | 3 (4) | 0.36 (0.10, 1.23) | 0.36 (0.09, 1.38) |
| BMId | ||||
| Normal/underweight | 161 | 9 (6) | 1.00 | 1.00 |
| Overweight | 345 | 40 (12) | 2.21 (1.05, 4.68) | 2.15 (0.98, 4.69) |
| Obese | 244 | 27 (11) | 2.10 (0.96, 4.59) | 1.82 (0.79, 4.15) |
| Anxious or depressede | ||||
| No | 338 | 31 (9) | 1.00 | – |
| Yes | 416 | 45 (11) | 1.20 (0.74, 1.95) | |
| Pain elsewheref,g | ||||
| No | 114 | 13 (11) | 1.00 | 1.00 |
| Baseline or follow-up | 219 | 27 (12) | 1.09 (0.54, 2.21) | 0.83 (0.39, 1.75) |
| Both baseline and follow-up | 422 | 36 (9) | 0.72 (0.37, 1.42) | 0.49 (0.24, 1.01) |
| Unilateral knee paine,g | 271 | 21 (8) | 1.00 | – |
| Bilateral knee pain | 474 | 52 (11) | 1.47 (0.86, 2.49) | |
| Non-severe knee pain | 281 | 9 (3) | 1.00 | 1.00 |
| Severe baseline or follow-up | 206 | 23 (11) | 3.80 (1.72. 8.40) | 3.99 (1.76, 9.04) |
| Severe baseline and follow-up | 268 | 44 (16) | 5.94 (2.84, 12.42) | 7.08 (3.22, 15.58) |
Numbers may not add to 755 due to missing data. aAdjusted for other presented variables; bat follow-up survey; cbased on SOA, divided into 20% of SOAs least deprived and 20% of SOAs most deprived; dbased on largest BMI recorded at baseline and follow-up survey; eat baseline or follow-up survey; fhip, low back, foot/ankle, hand, neck; gself-report.
Discussion
Summary of main findings
Overall, we found that NICE Step 3 management of knee pain or disability is mainly related to clinical need and influences other than socio-economic factors seem to drive referral and management for people who consult primary care. A substantial group of patients with persistent and severe knee pain or disability appear to be managed within primary care and do not get referred on. This finding may be due to reluctance to refer by the GP, or to be referred by the patient. As conservative treatments aim to manage (not cure) pain, it may be expected that people continue to report persistent and severe pain.
Our study showed that most of the older adults who consult primary care with knee pain receive a Step 3 intervention. Guidelines suggest these should only be considered when further treatment is needed. This group may have needed further treatment, although we do not have reliable data on their use of Step 1 or 2 treatment as these are not routinely coded in GP records. It is previously recognized that clinical practice for OA does not reflect guideline recommendations [22, 37].
Older people were less likely to be referred to secondary care, and a possible reason may be comorbidity. However, 44% of those aged ≥75 years who had been referred had a record of TKR compared with 21% of those aged <75 years, which suggests that once referred, those of older age are more readily accepted for TKR.
Comparison with other studies
Reporting severe knee pain or disability in both surveys had the strongest relationship with NICE Step 3 interventions including referral and surgery. Prescription of NSAIDs was not seemingly related to severity of pain or disability. Blamey et al. [38] highlighted irregular use of analgesics among hospital attenders, including some reporting severe pain. McHugh et al. [20] also observed little change in medication use despite increased pain levels in adults with end-stage lower limb OA. Other studies highlight complex decision making for medications use and our findings may be a reflection of this (e.g. perceptions of risk of adverse events, presence of other illness, reluctance) [39–41]. Rates of injection and X-ray in our study, and rates of NSAID use, were similar to previous studies [21, 23, 25]. However, rates of referral to physiotherapy or other specialists were lower in these self-report studies. Previous estimates of health care for knee pain may, therefore, be underestimated.
We found no relationship between referral and either individual socio-economic status or local area deprivation. These findings are in agreement with Thorstensson et al. [9] who found deprivation was not associated with help seeking behaviour although urban living was. Mitchell et al. [23] found that those referred on by the GP did not have more self-reported severity and there were differences in patients’ beliefs about their illness, income and economic circumstances. That survey had a 34% response rate so the results may be affected by selection bias. Jordan et al. [21] found no difference in the use of paracetamol or NSAIDs according to socio-economic groups, although those in higher social class groups had a higher use of physiotherapy services. In Solomon’s study of 160 people with knee or shoulder problems, education levels or medical insurance type were not related to referral to a rheumatologist or orthopaedic surgeon [24].
Strengths and limitations
We have undertaken an extensive manual search of general practice records including free text that GPs can enter. We also used multiple data sources and searched over a 10-year period. This time frame enabled a comprehensive and long-term assessment of management in primary care. We have not, however, been able to study patient factors such as illness perceptions, and these alongside beliefs about effectiveness of treatment have influenced uptake of care in previous studies [23, 42].
Our analyses only covered Step 3 (outer circle) of the NICE guidelines as data on Steps 1 and 2 are variable within medical records. Broadbent et al. [43] highlight this problem. They used nine quality indicators to measure the quality of recorded primary care treatment. There was variation from 17 to 30% in recording related to provision of information for OA and ‘considerable scope for improvement in the recording of high-quality care’ (p. 839).
There was some evidence of social inequity in receiving a TKR with those of higher social class or living in areas of lower deprivation more likely to receive a TKR. The number of TKRs, however, were small, hence the results were not statistically significant and so caution is needed. Also some people may have had a TKR before the start of the study. The majority of people, however, receiving a TKR in our study received it after the follow-up survey.
Another potential limitation of our study is the study setting, which was three general practices in North Staffordshire. While the general practices cover a range of socio-economic areas (a rural affluent town, a semi-rural mixed deprived area, a urban deprived area), the scope for assessing area deprivation differences may be limited. There was some survey non-response at 3 years. However, the data in Fig. 2 are standardized to the England and Wales population and the non-response is unlikely to affect the associations reported here.
Implications for research and clinical practice
Overall, we found that the inequalities that exist for joint replacement surgery do not seem to exist in earlier management of this condition. Our findings are both encouraging and worrying. On the one hand, people seem to be getting primary care treatment according to clinical need. On the other hand, non-significant differences exist at the later stages of treatment, for those arguably in most need. This disparity has also been shown elsewhere [14, 44]. The development of local appropriateness criteria for patients thought to be in need of joint replacement (that is owned by both GPs and surgeons), has been suggested as one potential way to reduce these inequalities, together with a focus on capacity to benefit [17]. The reasons for continuing disparities in the provision of TKRs require further research.
Many patients with severe knee pain or disability do not get referred on. One study highlighted referral status had no association with improvement of pain and function at 12 months [24]. Whether or not there are unmet needs for care in the group who remain managed in primary care requires further study.
Further research is also needed into the provision of management options covered in Steps 1 and 2 of the NICE guidelines, but this relies on more detailed recording of care in primary care settings. Quality indicators may help with this, but as Hunter et al. [37] note those developed hitherto have not been widely adopted. We agree with the suggestion that system-level initiatives may be needed to improve recording and care for OA in primary care [43].
Conclusion
In conclusion, social inequalities in the management and referral of knee problems in primary care were generally not observed, although there were some trends towards differences in likelihood of TKR. Most of the older adults who consult primary care with knee pain receive at least one Step 3 intervention from the NICE OA guidelines. A large group of people with continuing severe problems are managed solely in primary care. Inequalities in care for knee pain in older adults seem to be related to the provision of surgery only, at the point of uptake, and not within preceding management and referral in primary care.
Acknowledgements
Funding: This work was funded by the North Staffordshire Primary Care Research and Development Consortium and National Co-ordinating Centre for Research Capacity Development (NCC RCD) (now part of National Institute for Health Research) (PH1/03/C1/025).
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Busija L, Hollingsworth B, Buchbinder R, Osborne RH. Role of age, sex, and obesity in the higher prevalence of arthritis among lower socioeconomic groups: a population-based survey. Arthritis Rheum. 2007;57:553–61. doi: 10.1002/art.22686. [DOI] [PubMed] [Google Scholar]
- 2.Morris S, Sutton M, Gravelle H. Inequity and inequality in the use of health care in England: an empirical investigation. Soc Sci Med. 2005;60:1251–66. doi: 10.1016/j.socscimed.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Lubar D, White PH, Callahan LF, et al. A National public health agenda for osteoarthritis. Semin Arthritis Rheum. 2010;39:323–6. doi: 10.1016/j.semarthrit.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Lidgren L, Smolen J, Bentley G, et al. European action towards better musculoskeletal health. A public health strategy to reduce the burden of musculoskeletal conditions. Lund: University Hospital Lund; 2004. [Google Scholar]
- 5.Department of Health. The Musculoskeletal Services Framework. A joint responsibility: doing it differently. London: Department of Health; 2006. [Google Scholar]
- 6.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 7.Woolf AD. Healthcare services for those with musculoskeletal conditions: a rheumatology service. Recommendations of the European Union of Medical Specialists Section of Rheumatology/European Board of Rheumatology. Ann Rheum Dis. 2006;66:293–301. doi: 10.1136/ard.2006.061176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institute for Health and Clinical Excellence. Osteoarthritis. The care and management of adults with osteoarthritis. London: NICE; 2008. [Google Scholar]
- 9.Thorstensson CA, Gooberman-Hill R, Adamson J, Williams S, Dieppe P. Help-seeking behaviour among people living with chronic hip or knee pain in the community. BMC Musculoskelet Disord. 2009;10:153. doi: 10.1186/1471-2474-10-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hopman-Rock M, de Bock GH, Bijlsma JW, Springer MP, Hofman A, Kraaimaat FW. The pattern of health care utilization of elderly people with arthritic pain in the hip or knee. Int J Qual Health Care. 1997;9:129–37. doi: 10.1093/intqhc/9.2.129. [DOI] [PubMed] [Google Scholar]
- 11.Jordan K, Jinks C, Croft P. A prospective study of the consulting behaviour of older people with knee pain. Br J Gen Pract. 2006;56:269–76. [PMC free article] [PubMed] [Google Scholar]
- 12.Jinks C. Screening for knee pain and disability in the community. PhD Thesis, Keele University, Keele, UK, 2003. [Google Scholar]
- 13.Bedson J, Mottram S, Thomas E, Peat G. Knee pain and osteoarthritis in the general population: what influences patients to consult? Fam Pract. 2007;24:443–53. doi: 10.1093/fampra/cmm036. [DOI] [PubMed] [Google Scholar]
- 14.Yong PF, Milner PC, Payne JN, Lewis PA, Jennison C. Inequalities in access to knee joint replacements for people in need. Ann Rheum Dis. 2004;63:1483–9. doi: 10.1136/ard.2003.013938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juni P, Dieppe P, Donovan J, et al. Population requirement for primary knee replacement surgery: a cross-sectional study. Rheumatology. 2003;42:516–21. doi: 10.1093/rheumatology/keg196. [DOI] [PubMed] [Google Scholar]
- 16.Juni P, Low N, Reichenbach S, Villiger PM, Williams S, Dieppe PA. Gender inequity in the provision of care for hip disease: population-based cross-sectional study. Osteoarthritis Cartilage. 2010;18:640–5. doi: 10.1016/j.joca.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Dieppe P, Dixon D, Horwood J, Pollard B, Johnston M. MOBILE and the provision of total joint replacement. J Health Serv Res Policy. 2008;13:47–56. doi: 10.1258/jhsrp.2008.008018. [DOI] [PubMed] [Google Scholar]
- 18.Kane RL, Wilt T, Suarez-Almazor ME, Fu SS. Disparities in total knee replacements: a review. Arthritis Rheum. 2007;57:562–7. doi: 10.1002/art.22675. [DOI] [PubMed] [Google Scholar]
- 19.Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Ethnicity, socio-economic position and gender-do they affect reported health-care seeking behaviour? Soc Sci Med. 2003;57:895–904. doi: 10.1016/s0277-9536(02)00458-6. [DOI] [PubMed] [Google Scholar]
- 20.McHugh GA, Luker KA, Campbell M, Kay PR, Silman AJ. A longitudinal study exploring pain control, treatment and service provision for individuals with end-stage lower limb osteoarthritis. Rheumatology. 2007;46:631–7. doi: 10.1093/rheumatology/kel355. [DOI] [PubMed] [Google Scholar]
- 21.Jordan KM, Sawyer S, Coakley P, Smith HE, Cooper C, Arden NK. The use of conventional and complementary treatments for knee osteoarthritis in the community. Rheumatology. 2004;43:381–4. doi: 10.1093/rheumatology/keh045. [DOI] [PubMed] [Google Scholar]
- 22.Porcheret M, Jordan K, Jinks C, Croft P. Primary care treatment of knee pain-a survey in older adults. Rheumatology. 2007;46:1694–700. doi: 10.1093/rheumatology/kem232. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell HL, Carr AJ, Scott DL. The management of knee pain in primary care: factors associated with consulting the GP and referrals to secondary care. Rheumatology. 2006;45:771–6. doi: 10.1093/rheumatology/kei214. [DOI] [PubMed] [Google Scholar]
- 24.Solomon DH, Bates DW, Schaffer JL, Horsky J, Burdick E, Katz JN. Referrals for musculoskeletal disorders: patterns, predictors, and outcomes. J Rheumatol. 2001;28:2090–5. [PubMed] [Google Scholar]
- 25.Linsell L, Dawson J, Zondervan K, et al. Prospective study of elderly people comparing treatments following first primary care consultation for a symptomatic hip or knee. Fam Pract. 2005;22:118–25. doi: 10.1093/fampra/cmh609. [DOI] [PubMed] [Google Scholar]
- 26.Jinks C, Jordan K, Ong BN, Croft P. A brief screening tool for knee pain in primary care (KNEST) 2. Results from a survey in the general population aged 50 and over. Rheumatology. 2004;43:55–61. doi: 10.1093/rheumatology/keg438. [DOI] [PubMed] [Google Scholar]
- 27.Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community: (KNEST 3) Rheumatology. 2007;46:877–81. doi: 10.1093/rheumatology/kem013. [DOI] [PubMed] [Google Scholar]
- 28.Jinks C, Lewis M, Ong BN, Croft P. A brief screening tool for knee pain in primary care. 1. Validity and reliability. Rheumatology. 2001;40:528–36. doi: 10.1093/rheumatology/40.5.528. [DOI] [PubMed] [Google Scholar]
- 29.Porcheret M, Hughes R, Evans D, et al. Data quality of general practice electronic health records: the impact of a program of assessments, feedback, and training. J Am Med Inform Assoc. 2004;11:78–86. doi: 10.1197/jamia.M1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.NHS Information Authority. The Clinical Terms Version 3 (The Read Codes) Birmingham: NHS Information Authority; 2000. [Google Scholar]
- 31.Bellamy N. WOMAC Osteoarthritis Index. A Users Guide. London, Ontario: London Health Services Centre, McMaster University; 1996. [Google Scholar]
- 32.Zigmond A S, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 33.Office for National Statistics. National Statistics Socio-economic Classification (NS-SEC 2002) London: Stationery Office; 2002. [Google Scholar]
- 34.Office of the Deputy Prime Minister. The English Indices of Deprivation 2004: Summary. 2004, available from www.communities.gov.uk. [Google Scholar]
- 35.Ashworth M, Seed P, Armstrong D, Durbaba S, Jones R. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract. 2007;57:441–8. [PMC free article] [PubMed] [Google Scholar]
- 36.Jinks C, Jordan KP, Blagojevic M, Croft P. Predictors of onset and progression of knee pain in adults living in the community. A prospective study. Rheumatology. 2008;47:368–74. doi: 10.1093/rheumatology/kem374. [DOI] [PubMed] [Google Scholar]
- 37.Hunter DJ, Neogi T, Hochberg MC Quality of osteoarthritis management and the need for reform in the US. Arthritis Care Res. 2011;63:31–8. doi: 10.1002/acr.20278. [DOI] [PubMed] [Google Scholar]
- 38.Blamey R, Jolly K, Greenfield S, Jobanputra P. Patterns of analgesic use, pain and self-efficacy: a cross-sectional study of patients attending a hospital rheumatology clinic. BMC Musculoskelet Disord. 2009;10:137. doi: 10.1186/1471-2474-10-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carnes D, Anwer Y, Underwood M, Harding G, Parsons S. Influences on older people's decision making regarding choice of topical or oral NSAIDs for knee pain: qualitative study. Br Med J. 2008;336:142–5. doi: 10.1136/bmj.39401.699063.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sale JE, Gignac M, Hawker G. How “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum. 2006;55:272–8. doi: 10.1002/art.21853. [DOI] [PubMed] [Google Scholar]
- 41.Turner AP, Barlow JH, Buszewicz M, Atkinson A, Rait G. Beliefs about the causes of osteoarthritis among primary care patients. Arthritis Rheum. 2007;57:267–71. doi: 10.1002/art.22537. [DOI] [PubMed] [Google Scholar]
- 42.McHugh GA, Luker KA. Influences on individuals with osteoarthritis in deciding to undergo a hip or knee joint replacement: a qualitative study. Disabil Rehabil. 2009;31:1257–66. doi: 10.1080/09638280802535129. [DOI] [PubMed] [Google Scholar]
- 43.Broadbent J, Maisey S, Holland R, Steel N. Recorded quality of primary care for osteoarthritis: an observational study. Br J Gen Pract. 2008;58:839–43. doi: 10.3399/bjgp08X376177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Steel N, Melzer D, Gardener E, McWilliams B. Need for and receipt of hip and knee replacement–-a national population survey. Rheumatology. 2006;45:1437–41. doi: 10.1093/rheumatology/kel131. [DOI] [PubMed] [Google Scholar]