Abstract
Background
The variety of health problems (patient mix) that medical trainees encounter is presumed to be sufficient to masterthe required competencies.
Aim
To describe the patient mix of GP trainees, to study differences in patient mix between first-year and third-year GP trainees, and to investigate differences in exposure to sex-specific diseases between male and female trainees.
Design and setting
Prospective cohort study in Dutch primary care.
Method
During a 6-month period, aggregated data about International Classification of Primary Care diagnosis codes, and data on the sex and age of all contacts were collected from the electronic patient record (EPR) system.
Results
Seventy-three trainees participated in this study. The mean coding percentage was 86% and the mean number of face-to-face consultations per trimester was 450.0 in the first year and 485.4 in the third year, indicating greater variance in the number of patient contacts among third-year trainees. Diseases seen most frequently were: musculoskeletal (mean per trimester = 89.2 in the first year/91.0 in the third year), respiratory (98.2/92.7) and skin diseases (89.5/96.0). Least often seen were diseases of the blood and blood-forming organs (5.3/7.2), male genital disorders (6.1/7.1), and social problems (4.3/4.2). The mean number of chronic diseases seen per trimester was 48.0 for first-year trainees and 62.4 for third-year trainees. Female trainees saw an average of 39.8 female conditions per trimester — twice as many as male trainees (mean = 21.3).
Conclusion
Considerable variation exists trainees in the number of patient contacts. Differences in patient mix between first- and third-year trainees seem at least partly related to year-specific learning objectives. The use of an EPR-derived educational instrument provides insight into the trainees' patient mix at both the group and the individual level. This offers opportunities for GP trainers, trainees, and curriculum designers to optimise learning when exposure may be low.
Keywords: clinical competence, medical education, primary health care, problem based learning
INTRODUCTION
In most contemporary medical-speciality curricula, trainees acquire the demanded competencies through work-based learning,1 which allows competency development through clinical exposure to real patients (patient mix). Earlier research suggested that the patient mix of GP trainees differs from that of their trainers; trainees were exposed to more minor ailments and fewer chronic diseases and severe conditions.2–7 These studies were, however, small scale, covered a small period, or were relatively old.2,7–12
An explanation for disparities between the patient mix of trainers and trainees, suggested by Stubbings and Gowers, may be that the trainer is the senior, more experienced partner, thereby attracting older and more complex patients.7 The assigning behaviour of medical receptionists was not found to explain such disparities.13
Low exposure in some fields of patient mix was also found in undergraduate medical curricula, clerkships, and other specialist training programmes. 5,14–22 Ericsson's ‘Deliberate practice’ theory argues that low exposure has a negative impact on competency development. It assumes that becoming an expert requires sufficient practical experience and appropriate reflection, which can be stimulated by feedback from coaches or trainers.23 Within this framework, patient mix is an important training condition. Empirical evidence supports the importance of adequate patient mix to the effectiveness of rotations24 and the instructional quality of GP settings.25 The importance of an appropriate patient mix was also acknowledged by the World Federation For Medical Education (WFME), a strategic partner of the World Health Organization (WHO). In the WFME global standards for quality improvement in postgraduate education, it is stated: ‘The training must expose the trainee to a broad range of experience in the chosen field of medicine’.26
Electronic data extracted from electronic patient record (EPR) systems have proven valid for providing insight into the patient mix confronting GP trainees.9,27–29 In the Netherlands, most GPs keep detailed EPRs, including a standardised system of diagnosis codes: the International Classification of Primary Care (ICPC).30 Stimulated by the Dutch GP Association, all EPR systems now include the ICPC-1 codes. This allows uniformity in descriptions of the patient mix of GP trainees. The WHO has accepted ICPC as a reason for encounter classification, and users may use it as a classification for primary care or general practice wherever applicable.
Detailed descriptions of patient mix can be used to determine whether, and in which areas, low exposure actually exists. Teaching and rotation programmes may be adapted accordingly. For instance, trainees confronted with many older patients during their first-year practice period could benefit from subsequent assignment to a practice with many young families, or a rotation in a child health centre.
How this fits in
Earlier studies have shown disparities between the health problems GP trainees and trainers encounter, suggesting low exposure for trainees in several areas. In the present study electronic patient record extractions were used for getting a clear picture of the patient mix the trainees are exposed to. Variation between trainees in the number of patient contacts increased during their training. Areas of potential low exposure were identified. These areas need attention.
For GP trainers, detailed knowledge about the actual patient mix of their trainees is necessary to optimise this mix for specific learning objectives. The first-year curriculum focuses on minor ailments and daily care, while chronic-disease management is a formal learning objective in the third year GP trainers can tailor their trainees' patient mixes to these objectives.
Several authors have mentioned differences between male and female physicians regarding the number of contacts with patients with female conditions.7,31–33 Female trainees saw more female conditions than male trainees did, leaving the latter with relatively low exposure. The opposite could apply to male conditions, causing relatively low exposure for female trainees.
Definition of patient mix
For this study, patient mix was defined as the quantity and variety of diseases and the age and sex distribution of patients. This broad definition was used, as patient demographic characteristics can be relevant for learning objectives.4,5,24,25
Research questions
The research questions were as follows:
what patient mix do GP trainees encounter?
how does patient mix differ between first-year and third-year trainees regarding number of patient contacts, mean patient age, and number of diagnosis codes within the different organ systems?
how do male and female trainees differ in their exposure to sex-specific diseases?
how many patients with chronic diseases do trainees encounter?
METHOD
Participants
Participants were 49 first-year and 24 third-year GP trainees at the Institute of GP Specialty Training of the Academic Medical Center University Amsterdam.
Setting
This study was conducted in 2008–2009 in GP practices affiliated with the Institute of GP Specialty Training, which facilitates a 3-year training programme in which first- and third-year trainees are stationed in GP training practices. In their second year, trainees do clinical rotations. A full-time working week was 36 hours, including 6.5 hours of modular education at the institute and 29.5 hours in the practices.
Design and procedures
This was a prospective cohort study. Between March and December 2008, GP trainers with trainees in their practices starting a training period of 9–12 months were approached for inclusion. For each trainee, data were extracted for 6 months. Data-extraction software was developed for four different types of EPR, covering approximately 80% of the EPRs used by the affiliated training practices.
First, the trainers were asked to participate. The trainees of those who agreed were invited for the study. All GP trainers and trainees were asked for informed consent and provided with reference cards detailing the basic ICPC coding rules and some standard coding problems and solutions. All trainees attended a session that introduced the study and explained the content of the reference card. The regular training programme also addresses ICPC coding, and ICPC-coding assistance was available by email or telephone throughout the study.
Data extraction and instrument
Data were extracted directly from the EPR every 3 months by either the GPs or the researchers. The raw extraction data were processed by multiple software routines using MS Visual Basic routines in MS Access. Decision rules were programmed to ensure logic and consistency in counting the codes (Box 1). The resulting aggregate data were emailed to the researchers. No information about individual patients could be recovered. The data contained information about ICPC diagnosis codes (I) and patient contacts (II). The latter were aggregated according to sex, age, and consultation type (telephone, face-to-face or home visit).
Box 1. Decision rules
ICPC diagnosis codes (I)
Each newly entered ‘distinct’ diagnosis code was counted. In case of multiple diagnosis codes, all were counted, even if they took place in the same consultation.
Codes for specific patients on specific days that were entered twice or more were counted only once.
All codes were counted for patients who were seen on separate days for similar problems, leading to the same ICPC codes. (Note that this approach is different from calculating morbidity rates).35
For diagnosis codes linked to episodes of care, the episode code was counted only if no other new diagnosis code was entered during that contact; the episode code was ignored if a distinct diagnosis code was entered and linked to the episode code (for example, if pneumonia was linked to a chronic obstructive pulmonary disease (COPD) episode, only the pneumonia code was counted, whereas COPD would have been counted in the absence of the pneumonia code during that specific consultation orvisit).
If no diagnosis code (distinct or episode) was present, the consult was counted as non-coded.
Diagnosis codes linked to administrative tasks or repeat prescriptions were ignored.
Contact-type codes (II)
Contact codes were categorised as face-to-face, telephone, or home visit.
ICPC diagnosis codes
Developed by the ICPC Working Party and published in 1987 by the World Organization of National Colleges, Academies (WONCA), the ICPC consists of 17 chapters covering the organ systems, a general chapter, and a social chapter WHO includes the ICPC (Version 2) within its FIC (Family of International Classifications). The differences between ICPC-1 and ICPC-2 regarding diagnosis codes are minor.30 The ICPC coding system allows the coding of both symptom diagnoses (for example, headache, ankle complaints) and ‘definite’ diagnoses (for example, pneumonia, appendicitis, hypothyroidism).
Chronic diseases
The list of chronic diseases published by Knottnerus and colleagues was used to count the number of chronic diseases the trainees encountered.34
Data analysis
Descriptive analyses were used to report the mean number of contacts per trimester, encounters per ICPC chapter, and coding percentage. Differences between male and female trainees and between first- and third-year trainees were tested using analysis of variance and t-tests; 95% significance level.
The coding percentage was calculated by dividing the total number of ICPC diagnosis codes in a trimester by that same number plus the number of non-coded contacts. Because there can be multiple diagnosis codes per contact, this formula could overestimate the coding percentage. The coding percentages were therefore corrected by multiplying the non-coded contacts in each case by the individual mean number of ICPC diagnosis codes per contact.
Data from part-time trainees were adjusted to give values as if they worked full-time, by multiplying the absolute numbers of diagnoses and contact codes by 1/(part-time percentage/100).
RESULTS
Participants
During the inclusion period, trainees were starting training periods in 109 practices affiliated with the researchers' institute. The 98 practices that had suitable EPR systems were contacted. The sample included 73 GP training practices, 49 first-year trainees, and 24 third-year trainees. Reasons for non-inclusion (n = 25) are displayed in Figure 1. Eleven (15%) practices were single-handed, 17 (23%) were dual-handed, and 45 (62%) were group practices.
Figure 1.
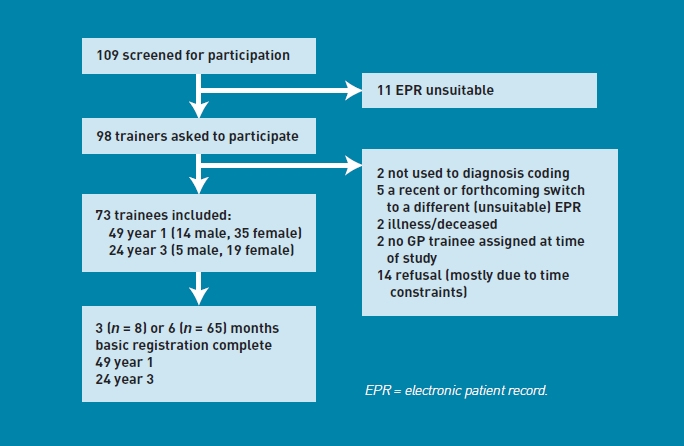
Flow chart.
The mean age of trainees was 31.2 years (standard deviation [SD] = 3.2 years) years: 30.2 years (SD = 2.5) for first-year trainees and 33.2 years (SD = 3.7 years) for third-year trainees. Six first-year trainees (12%) and eight third-year trainees (33%) worked part-time, with a mean part-time percentage of 86% corresponding to 31 hours per week.
Coding percentage
The mean (corrected) coding percentage of 86% (SD = 13.2) was similar in both training years (86% versus 87%). Data regarding the ICPC codes for one trainee with a very low coding percentage (27%) were disregarded.
Consultations and home visits
The mean number of contacts per trimester was 583.8. Table 1 presents the mean number of contacts in the first and third training years, averaged over two trimesters. There were no significant differences between the first and third years, although the SD for face-to-face consultations in year 3 was twice as high as for year 1, indicating greater variance in the number of patient contacts among third-year trainees.
Table 1.
Mean contact frequencies, number of ICPC diagnosis codes, and number of non-coded contacts for first- and third-year trainees, averaged over two trimesters
| First-year trainees, n = 49 | Third-year trainees, n = 24 | |||
|---|---|---|---|---|
| Mean per trimester (SD) | Minimum/maximum | Mean per trimester (SD) | Minimum/maximum | |
| Face-to-face | 450.0 (86,6) | 251 / 641 | 485.4(159.1) | 252 / 797 |
| Telephone | 64.0 (35,9) | 5 / 139 | 75.4(56.6) | 11 / 224 |
| Home visit | 35.6 (30,2) | 0 / 147 | 35.5 (26.7) | 6 / 120 |
| Total contact codes | 549.6 (111.3) | 302 / 782 | 596.3 (181.1) | 301 / 939 |
| ICPC diagnosis codesa | 537.6(153.1) | 337 / 884 | 578.4(201.7) | 261 / 955 |
| Non-coded contactsb | 75.9 (71.8) | 0 / 392 | 76.8(86.8) | 4 / 372 |
Number of ICPC codes, averaged over two trimesters, corrected for part-time work.
Mean number of noncoded contacts, averaged over two trimesters, corrected for part-time work. ICPC = International Classification of Primary Care. SD = standard deviation
The mean number of ICPC diagnosis codes per trimester, and the mean number of non-coded contacts are also presented in Table 1. The mean number of ICPC codes per contact was 1.13 in the first year and 1.11 in the third year. The total number of problems encountered can thus be estimated at 621.0 in the first year and 661.9 in the third year.
Age and sex distribution of patients
Figure 2 presents the age distribution of the patients. Third-year trainees saw significantly more patients aged between 45 and 64 years than did first-year trainees (t (71) = −2.58, P = 0.012). No significant differences between first-year and third-year trainees were found for the other age groups.
Figure 2.
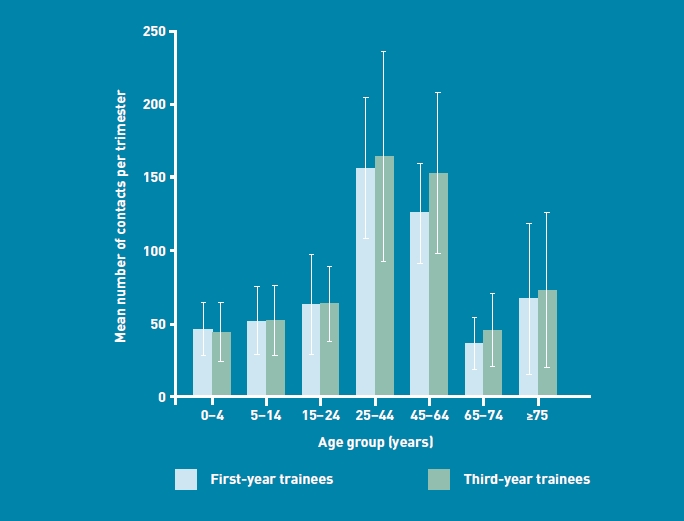
Means and standard deviation for number of contacts per age group for first- and third-year trainees, averaged over two trimesters.
Female patients were seen significantly more (mean = 344.6, SD = 92.3) than male patients (mean = 220.3, SD = 59.3) (t (144) = −9.68, P = 0.00). No differences were found between male and female trainees regarding the sex distribution of patients (t (71) = 0.503, P = 0.61).
Organ systems
Figure 3 presents the patient mix by organ system and the mean numbers of diagnosis codes per trimester Musculoskeletal (year 1 mean per trimester [SD]/year 3 mean [SD] = 89.2 [28.6]/91.0 [39.2]), respirator (98.2 [30.8]/92.7 [34.7]), and skin diseases (89.5 [26.3]/96.0 [32.8]) were seen most often. Diseases of the blood and blood-forming organs (5.3 [3.3]/7.2 [4.8]), male genital disorders (6.1 [3.4]/7.1 [6.6]), and social problems (4.3 [3.2]/4.2 [3.1]) were seen the least.
Figure 3.
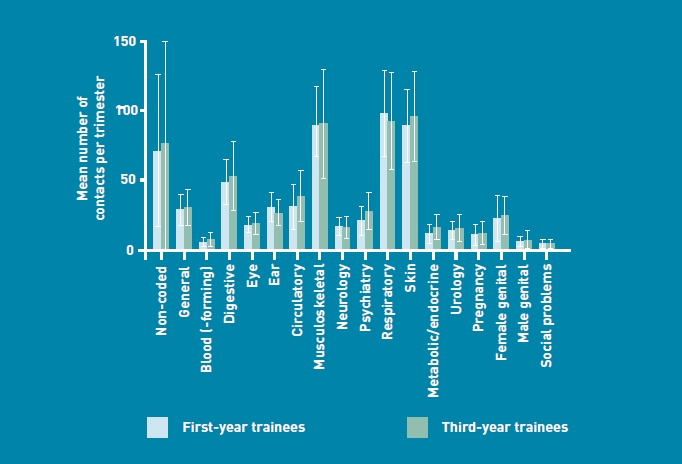
Means and standard deviations of ICPC codes for first- and third-year trainees, averaged over two trimesters.
Significant differences were found between years 1 and 3 for blood and blood-forming diseases, (t (70) = -2.02, P = 0.047) psychiatric diseases (t (70)= -2.56, P = 0.013), and metabolic diseases (t (70)= -2.53, P = 0.014).
Conditions seen most frequently
Table 2 presents the 20 conditions most often seen in either training year Differences between first- and third-year trainees were minor: otitis media was in the top 20 of first-year trainees (third-year rank 23, mean = 4.9 contacts per trimester), whereas diabetes mellitus was in the top 20 of the third-year trainees (first-year rank 26, mean = 4.5 contacts per trimester).
Table 2.
Mean contacts per trimester for the conditions seen most frequently in years 1 and 3, averaged over two trimesters
| Rank | Year 1 | Mean | Year 3 | Mean |
|---|---|---|---|---|
| 1 | Acute respiratory infection | 28.7 | Acute respiratory infection | 24.0 |
| 2 | Cough | 15.8 | Hypertension | 14.2 |
| 3 | Hypertension | 11.3 | Cough | 12.8 |
| 4 | Dermatomycosis | 9.6 | Dermatomycosis | 10.9 |
| 5 | Otitis media | 8.5 | Low back pain | 8.5 |
| 6 | Low back pain | 7.8 | Cystitis or other urinary infection | 8.3 |
| 7 | Cystitis or other urinary infection | 7.5 | Acute or chronic sinusitis | 7.8 |
| 8 | Acute or chronic sinusitis | 7.5 | Other musculoskeletal disease | 7.4 |
| 9 | Weakness/tiredness | 7.4 | Contact/allergic dermatitis | 7.1 |
| 10 | Acute bronchitis or bronchiolitis | 7.0 | Weakness or tiredness | 7.1 |
| 11 | Knee symptom/complaint | 6.6 | Diabetes mellitus | 6.8 |
| 12 | Dermatitis or atopic eczema | 6.5 | Acute bronchitis or bronchiolitis | 6.6 |
| 13 | Contact or allergic dermatitis | 6.3 | Abdominal pain/cramps (general) | 6.4 |
| 14 | Localised abdominal pain | 6.2 | Musculoskeletal injury | 6.4 |
| 15 | Shoulder symptoms | 6.0 | Asthma | 6.1 |
| 16 | Otitis externa | 5.9 | Knee symptom/complaint | 5.9 |
| 17 | Asthma | 5.9 | Dermatitis/atopic eczema | 5.7 |
| 18 | Gastroenteritis | 5.4 | Constipation | 5.7 |
| 19 | Musculoskeletal injury | 5.4 | Conjunctivitis | 5.3 |
| 20 | Pneumonia | 5.3 | Gastroenteritis | 5.3 |
Chronic diseases
The mean number of chronic diseases seen per trimester was 48.0 (SD = 21.9; 39.5 first trimester, 56.5 second trimester) for first-year trainees, and 62.4 (SD = 32.6; 55.3 first trimester, 78.3 second trimester) for third-year trainees. The seven chronic conditions seen most frequently were the same for both years: diabetes mellitus, asthma, constitutional eczema, emphysema or chronic obstructive pulmonary disease (COPD), depression, heart failure, and leg ulcer
Sex-specific conditions
Female trainees saw almost twice as many (mean per trimester = 39.8, SD = 24.1) female conditions as did male trainees (mean = 21.3, SD = 9.2). This difference was significant (F(1,68) = 7.38, P = 0.008), irrespective of training year For male conditions, no similar pattern was found.
DISCUSSION
Summary
The patient mix of 73 GP trainees was studied by using EPR-derived data extractions, and compared the first and third training years. It was found that the patient mix is generally well spread out over all ages and organ systems, although it is possible to indicate areas of relative low exposure. Some differences were found between the patient mixes of first- and third-year trainees that seemed related to year-specific learning objectives. Third year trainees saw more chronic diseases than first years did. It was also found that female trainees saw more female conditions than their male counterparts.
Contrary to expectations, no higher contact frequencies were observed in the third training year, although frequencies varied more than in the first year. Closer examination showed that this was largely due to a number of trainees who saw exceptionally large numbers of patients. This kind of information about the patient mix of individual trainees was not known before monitoring was started. The results presented here may in general seem satisfactory for the group as a whole, but since the variance in contacts and exposure to the different organ systems was substantial, individual trainees may, perhaps unknowingly, be suffering from low exposure in certain areas. This study's findings show the importance of monitoring the patient mix for each individual GP trainee.
Strengths and limitations
Using EPR data to describe patient mix has been successful before.9,27,35 One strength of the present study was the use of data from EPR systems combined with decision rules to describe patient mix. Many earlier studies used handwritten or digital logbooks intended solely for educational purposes.5,14,36 These type of data are subject to social-desirability bias by the trainee. Extracted from EPR systems, the data of the present study were not biased by any threat of formal assessment. Such systems can be of great educational value.
Diagnosis-coding percentages were satisfying, at about 86%, although it is not possible to be sure whether this patient mix was representative. For example, the data could have been biased if trainees tended not to code complex cases.
Although ICPC coding is useful for describing patient mix, its validity is potentially diminished by its dependence on the diagnostic competence of the trainees and the adequacy of the attribution of the codes (for example, definite instead of symptom diagnosis).37
Although all trainees were affiliated with the same speciality-training institute, the authors do not think that this influenced the results, as other studies in different times, scales, and areas have shown similar results.
Comparison with existing literature
The trainees were exposed to diseases of all organ systems. Most prominent were respiratory, skin, and musculoskeletal diseases, followed by digestive, circulatory and ear diseases. This exposure pattern reflects the general morbidity pattern in the Netherlands (2nd Dutch National Survey of General Practice [DNSGP-2]).37 These findings seem robust, as other studies (for example, the 1991 and 1992 British Morbidity Surveys) have found similar exposure patterns, although these studies were small scale, covered a small period, or were relatively old.2,7–12
Trainees were less likely to encounter diseases of the blood and blood-forming organs, male genital disorders, and social problems. This was also the case in the DNSGP-2 and the British Morbidity Survey (excepting social problems), meaning that licensed GPs are also less likely to encounter these conditions. From an educational perspective, however, potential underexposure in these areas is conceivable.
Several authors have warned about underexposure to chronic conditions.38–41 Earlier studies report that GP trainees saw fewer chronic conditions than did British principals4 or Dutch trainers.6 In 2004, Darer and colleagues found that US physicians considered their training in chronic illness care inadequate.39 In the present study, exposure to chronic diseases increased steadily during training. This should be considered positive, as the third-year curriculum emphasises chronic and complex conditions as learning objectives. The actual number of chronic conditions encountered by trainees is probably higher than the findings of this study, as the software was programmed to count actual health problems and not intercurrent chronic conditions. For example, coughing and dyspnoea in an 82-year-old patient with a history of diabetes, stroke, and Parkinson's disease may be coded simply as a common cold, even if all comorbidity was taken into account.
It was found that female conditions were seen more often by female trainees. This is in line with studies on the clinical skills of medical students and family medicine residents.32,33 Levy and Merchant found that male students received more experience with male-specific examination skills, but the present data do not show that male GP trainees saw more male-specific conditions.31
The low number of codes regarding social conditions might be due to underreporting. Although trainees may be aware of a patient's social problems, they may not be coded unless they were the complaints presented by the patient (for example, in the interest of time, carefulness, or legal considerations).
Although there are no data available about the trainees' competence development in areas of low exposure, these areas may need attention by GP trainers and curriculum designers. They should be aware that adequate supervision is needed in areas of low exposure, in order to maximise the learning experiences. Another option for addressing potential lacunas is to extend the training with clinical rotations in these areas.
Implications for research
The higher variation of contact frequencies in the third year, mainly due to several trainees seeing an exceptional large amount of patients, is interesting from an educational perspective. Trainees who see large numbers of patients might build more experience, learn more, and perform better. It would be interesting to identify whether this is due to individual characteristics of these trainees, their trainers or the patient supply within the training practice.
Another question for further study involves whether steering trainees' patient mix can affect competence development.42 For example, the results of this study suggest that steering patients with female conditions to male trainees may be rational.
If approached with caution, the results may help to identify specific practices with high concentrations of patients with specific characteristics. Future studies could investigate whether the intentional allocation of trainees with specific learning objectives to suitable practices improves the patient mix.
It may be attractive to formulate minimum quotas or estimates of the number of patients needed to develop competence in certain areas.43 Although the present results suggest what is normally encountered, caution is advised, as the relation between patient mix and competence development is complex44 and differs between individuals.
Funding
All authors work in the employ of the General Practice Specialty Training institute of the Academic Medical Center, Amsterdam. This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical approval
This study was approved retrospectively by the Ethical Review Board of the Netherlands Association for Medical Education (NERB-ID 42) in an online procedure. Please note that this review board started on 16 July 2010. Before this date, educational research was not admissible for ethical review boards of academic centres because according to Dutch Law no approval is needed.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have support from the General Practice Specialty Training of the AMC.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Dornan T, Boshuizen H, King N, Scherpbier A. Experience-based learning: a model linking the processes and outcomes of medical students' workplace learning. Med Educ. 2007;41(1):84–91. doi: 10.1111/j.1365-2929.2006.02652.x. [DOI] [PubMed] [Google Scholar]
- 2.Wollstadt LJ. Case mix in a primary care teaching practice for two clerkship schedules. J Fam Pract. 1979;8(1):107–112. [PubMed] [Google Scholar]
- 3.Tan LH. Amsterdam: University of Amsterdam; 1989. Tekorten in de huisartsopleiding, proefschrift UvA. [Deficiencies in the curriculum of the vocational training for general practitioners] [Google Scholar]
- 4.Eccles M, Bamford C, Steen N, Russell I. Case mix and content of trainee consultations: findings from the north of England study of standards and performance in general practice. Br J Gen Pract. 1994;44(387):437–440. [PMC free article] [PubMed] [Google Scholar]
- 5.Markham FW, Rattner S, Hojat M, et al. Evaluations of medical students' clinical experiences in a family medicine clerkship: differences in patient encounters by disease severity in different clerkship sites. Fam Med. 2002;34(6):451–454. [PubMed] [Google Scholar]
- 6.Vintges M, Van Weert H, Van der Wiele E, et al. What health problems do trainees in general practice see? Data from electronic patient records compared with the ‘qualification terms' of the Dutch vocational training for general practitioners. Huisarts Wet. 2001;44:485–489. [Google Scholar]
- 7.Stubbings CA, Gowers JI. A comparison of trainee and trainer clinical experience. J R Coll Gen Pract. 1979;29(198):47–52. [PMC free article] [PubMed] [Google Scholar]
- 8.Carney TA. Clinical experience of a trainee in general practice. J R Coll Gen Pract. 1979;29(198):40–44. [PMC free article] [PubMed] [Google Scholar]
- 9.Nkoy FL, Petersen S, Antommaria AH, Maloney CG. Validation of an electronic system for recording medical student patient encounters. AMIA Annu Symp Proc. 2008;6:510–514. [PMC free article] [PubMed] [Google Scholar]
- 10.Parkerson GR, Jr, Griffin EW. Clinical experience during family medicine residency training. South Med J. 1987;80(7):895–900. doi: 10.1097/00007611-198707000-00021. [DOI] [PubMed] [Google Scholar]
- 11.St George I. What do trainee interns see in general practice? N Z Med J. 1982;95(712):506–507. [PubMed] [Google Scholar]
- 12.McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice. Fourth national study 1991-1992. London: HMSO; 1995. http://www.statistics.gov.uk/downloads/theme_health/MB5No3.pdf (accessed 11 Jul 2011) [Google Scholar]
- 13.De Jong J, Visser MRM, Wieringa-de Waard M. Who determines the patient mix of GP trainees? The role of the receptionist. Fam Pract. 2011;28(3):287–293. doi: 10.1093/fampra/cmq102. [DOI] [PubMed] [Google Scholar]
- 14.Raghoebar-Krieger HM, Sleijfer DT, Hofstee WK, et al. The availability of diseases for medical students in a university hospital. Med Teach. 2001;23(3):258–262. doi: 10.1080/01421590120043026. [DOI] [PubMed] [Google Scholar]
- 15.Morris-Stiff G, Ball E, Torkington J, et al. Registrar operating experience over a 15-year period: more, less or more or less the same? Surgeon. 2004;2(3):161–164. doi: 10.1016/s1479-666x(04)80078-7. [DOI] [PubMed] [Google Scholar]
- 16.Feldman M, Nasmyth G. An evaluation of operative training lists for senior house officers in a district general hospital. Ann R Coll Surg Engl. 2005;87(4):277–282. doi: 10.1308/147870805X45957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haney E, Nicolaidis C, Hunter A, et al. Relationship between resident workload and self-perceived learning on inpatient medicine wards: a longitudinal study. BMC Med Educ. 2006;6:35. doi: 10.1186/1472-6920-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ballal RS, Eisenberg MJ, Ellis SG. Training in cardiac catheterization at high-volume and low-volume centers: is there a difference in case mix? Am Heart J. 1996;132(2 Pt 1):460–462. doi: 10.1016/s0002-8703(96)90450-0. [DOI] [PubMed] [Google Scholar]
- 19.Eisenberg MJ, Claire J, Mak KH, Ellis SG. Importance of case mix during training in interventional cardiology. Am J Cardiol. 1996;77(11):1010–1013. doi: 10.1016/s0002-9149(97)89161-8. [DOI] [PubMed] [Google Scholar]
- 20.Hand R, Garg M, Dajani KF. Patient mix in the primary ambulatory care clinics of an academic medical center. Acad Med. 1993;68(10):803–805. doi: 10.1097/00001888-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 21.McLeod PJ, Snell L. Casemix in an internal medicine clerkship: educational value of the clinical problems seen. J Gen Intern Med. 1991;6(5):455–459. doi: 10.1007/BF02598171. [DOI] [PubMed] [Google Scholar]
- 22.Wimmers PF, Schmidt HG, Splinter TA. Influence of clerkship experiences on clinical competence. Med Educ. 2006;40(5):450–458. doi: 10.1111/j.1365-2929.2006.02447.x. [DOI] [PubMed] [Google Scholar]
- 23.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10 Suppl):S70–S81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 24.Dolmans DHJM, Wolfhagen IHAP, Essed GGM, et al. The impacts of supervision, patient mix, and numbers of students on the effectiveness of clinical rotations. Acad Med. 2002;77(4):332–335. doi: 10.1097/00001888-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Van der Zwet J, Hanssen VG, Zwietering PJ, et al. Workplace learning in general practice: supervision, patient mix and independence emerge from the black box once again. Med Teach. 2010;32(7):e294–e299. doi: 10.3109/0142159X.2010.489128. [DOI] [PubMed] [Google Scholar]
- 26.Karle H. Postgraduate medical education: WFME global standards for quality improvement. Copenhagen: World Federation for Medical Education; 2003. http://www3.sund.ku.dk/Activities/WFME%20Standard%20Documents%20and%20translations/WFME%20Postgraduate.pdf (accessed 11 Jul 2011) [Google Scholar]
- 27.Mulloy JV, Leuschen M, Rowe BH. Computer-based patient encounter tracking. Development of a system for family medicine residents. Can Fam Physician. 1995;41:1742–1751. [PMC free article] [PubMed] [Google Scholar]
- 28.Alderson TS, Oswald NT. Clinical experience of medical students in primary care: use of an electronic log in monitoring experience and in guiding education in the Cambridge Community Based Clinical Course. Med Educ. 1999;33(6):429–433. doi: 10.1046/j.1365-2923.1999.00336.x. [DOI] [PubMed] [Google Scholar]
- 29.Nierenberg DW, Eliassen MS, McAllister SB, et al. A web-based system for students to document their experiences within six core competency domains during all clinical clerkships. Acad Med. 2007;82(1):51–73. doi: 10.1097/01.ACM.0000249990.86538.ac. [DOI] [PubMed] [Google Scholar]
- 30.Lamberts H, Woods M. International classification of primary care. Oxford: Oxford University Press; 1987. [Google Scholar]
- 31.Levy BT, Merchant ML. Differences in clinical experiences based on gender of third-year medical students in a required family medicine preceptorship. Acad Med. 2002;77(12 Pt 1):1241–1246. doi: 10.1097/00001888-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Carney PA, Dietrich AJ, Eliassen S, et al. Differences in ambulatory teaching and learning by gender match of preceptors and students. Fam Med. 2000;32(9):618–623. [PubMed] [Google Scholar]
- 33.Sabir S, Godwin M, Birtwhistle R. Men and women residents' experiences with women's health care in a family medicine center. Acad Med. 1997;72(4):293–295. doi: 10.1097/00001888-199704000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Knottnerus JA, Metsemakers J, Hoppener P, Limonaro C. Chronic illness in the community and the concept of social prevalence'. Fam Pract. 1992;9(1):15–21. doi: 10.1093/fampra/9.1.15. [DOI] [PubMed] [Google Scholar]
- 35.Lyman JA, Schorling J, Nadkarni M, et al. Development of a web-based resident profiling tool to support training in practice-based learning and improvement. J Gen Intern Med. 2008;23(4):485–488. doi: 10.1007/s11606-007-0467-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raghoebar-Krieger HM, Sleijfer D, Bender W, et al. The reliability of logbook data of medical students: an estimation of interobserver agreement, sensitivity and specificity. Med Educ. 2001;35(7):624–631. doi: 10.1046/j.1365-2923.2001.00963.x. [DOI] [PubMed] [Google Scholar]
- 37.Van der Linden M, Schellevis F, Westert G. Morbidity in the population and in general practice: 2nd Dutch National Survey of General Practice [DNSGP-2] Utrecht: NIVEL; 2004. [Google Scholar]
- 38.Cohen AJ. Caring for the chronically ill: a vital subject for medical education. Acad Med. 1998;73(12):1261–1266. doi: 10.1097/00001888-199812000-00015. [DOI] [PubMed] [Google Scholar]
- 39.Darer JD, Hwang W, Pham HH, et al. More training needed in chronic care: a survey of US physicians. Acad Med. 2004;79(6):541–548. doi: 10.1097/00001888-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Hasler JC. Do trainees see patients with chronic illness? Br Med J (Clin Res Ed) 1983;287(6406):1679–1682. doi: 10.1136/bmj.287.6406.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pham HH, Simonson L, Elnicki DM, et al. Training U.S. medical students to care for the chronically ill. Acad Med. 2004;79(1):32–40. doi: 10.1097/00001888-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Fouracre R, Savory JN. Steering patients with selected conditions to trainees. J R Coll Gen Pract. 1980;30(221):729–733. [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson N, Hasler J, Toby J, Grant J. Consensus minimum standards for use in a trainer's report for summative assessment in general practice. Br J Gen Pract. 1996;46(404):140–144. [PMC free article] [PubMed] [Google Scholar]
- 44.Jolly BC, Jones A, Dacre JE, et al. Relationships between students' clinical experiences in introductory clinical courses and their performances on an objective structured clinical examination (OSCE) Acad Med. 1996;71(8):909–916. doi: 10.1097/00001888-199608000-00021. [DOI] [PubMed] [Google Scholar]


