Abstract
We measured changes in physical activity in 2 obese preschool children when a package intervention was evaluated in a reversal design. Physical activity was measured via direct observation and pedometers. Although the intervention produced only modest increases in activity, the results provide preliminary concurrent validation for the dependent measures used, in that the two measures covaried and a similar degree of change was observed with each across baseline and intervention phases.
Keywords: goal setting, obesity, percentile schedules, physical activity, shaping
The prevalence of overweight and obese boys and girls between 2 and 5 years of age is estimated to be around 8.5%, with less conservative estimates placing the prevalence rate at 24% (Ogden, Carroll, & Flegal, 2008). Overweight and obesity contribute to a variety of serious health problems (e.g., heart disease, Type 2 diabetes), especially in adulthood. There also are significant financial consequences; annual childhood obesity-related hospital costs were estimated at $127 million during 1997, 1998, and 1999 (U.S. Centers for Disease Control and Prevention, n.d.).
In general, behavioral interventions for overweight and obesity produce outcomes superior to other approaches (Jelalian & Saelens, 1999) and typically involve package interventions that target eating and physical activity (Epstein, Myers, Raynor, & Saelens, 1998). However, much of the published research relies on weight loss and self-reports of eating and activity as the primary dependent measures; thus, the accuracy of the data is questionable, and little is revealed about the relative influence of eating and activity on weight loss.
Because the validity and reliability of self-report measures are suspect (especially with children) and because physical activity is an important health-related behavior, researchers have developed a number of measures to assess physical activity. These include direct observation systems such as the Behaviors of Eating and Activity for Children's Health Evaluation System (BEACHES; McKenzie et al., 1991) and, more recently, the Observation System for Recording Activity in Children (OSRAC; e.g., McIver, Brown, Pfeiffer, Dowda, & Pate, 2009). The five activity levels (ranging from sedentary to vigorous physical activity) proposed by the BEACHES have been validated via concurrent heart-rate monitoring, but no studies have validated the OSRAC.
Pedometers are mechanical devices worn at the hip that can be used to assess physical activity (i.e., the number of steps taken by the wearer). Several studies have demonstrated the utility of pedometers as dependent measures and as tools for self-monitoring in behavioral interventions (Normand, 2008; VanWormer, 2004). However, the participants in these studies were adults, and the utility of pedometer measures with young children has yet to be determined. The purpose of the current study was to compare activity data from the OSRAC Preschool Version with those produced by a pedometer. This was done in the context of a package intervention intended to increase physical activity in obese children to assess the utility and validity of the observation system.
METHOD
Participants and Setting
Two typically developing 4-year-old children, Meg (female) and Chris (male), participated. Their body mass index (BMI) placed them in the 95th percentile of the U.S. Centers for Disease Control and Prevention BMI-for-age growth charts. All sessions took place during a 20-min outdoor recess period on a school playground. Various activities were available, including bicycles, sandbox, fixed equipment, and water tables. No structured activities were arranged, and participants were not prompted to engage in any specific activity.
Response Measurement and Reliability
Participants wore a New Lifestyles NL-2000 pedometer, calibrated for height, weight, and age, throughout each session. At the end of each session, an observer recorded the number of steps taken by each participant, with a step defined as any activity that resulted in a count being recorded on the pedometer. Using the OSRAC, observers also recorded activity using a momentary time-sampling system with 5 s to observe and 25 s to record per interval. Five activity codes indicated the level of physical activity (see Table 1), and the highest level of physical activity observed during an interval was recorded. All other categories (i.e., activity type, initiator, group composition, prompts, engagement, and context) also were coded with reference to the activity level code; however, only the activity-level data are reported.
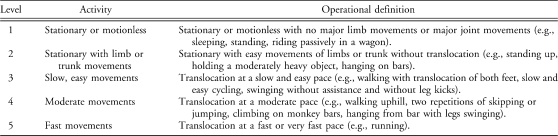
Table 1.
Activity Level Codes Specified by McIver et al. (2009)
For the purposes of analysis, the OSRAC activity codes were collapsed into three categories: sedentary (i.e., stationary), light (i.e., stationary with limb movements and slow movements), and moderate-to-vigorous physical activity (MVPA). The activity codes were collapsed because it was hypothesized that relative metabolic and physiological measures did not significantly differ for some codes. Activity Codes 2 (stationary with limb movements) and 3 (slow movements) were combined, as were Activity Codes 4 (moderate movements) and 5 (fast movements). The latter combination was indicative of MVPA, and the former combination was indicative of light-intensity activity. McIver et al. (2009) combined categories in a similar way. Moreover, combining the activity codes in this way improved interobserver agreement scores.
For 31% of all sessions, two observers independently recorded both activity levels using the OSRAC and the step totals displayed on the pedometers for each participant. An agreement was scored if both observers recorded the same activity code for a given interval or the same step total was recorded at the end of the session. To calculate interobserver agreement, we divided number of agreements by the total number of agreements plus disagreements and multiplied by 100%. Mean agreement scores across three coding categories (sedentary, light, and MVPA) were 82% for Chris (range, 74% to 90%) and 80% for Meg (range, 58% to 95%). Agreement was 100% for step totals.
Procedure
An intervention package comprised of goal setting, performance feedback, and reinforcement was evaluated using a reversal design. Throughout the study, goals were set related to step totals. The degree of covariation between the pedometer step totals and OSRAC activity codes was assessed within and across conditions.
Baseline
Each participant wore a pedometer but did not have any performance goals and did not receive programmed consequences for activity. The pedometer screens were covered, and observers ensured that participants did not uncover the screens or tamper with the pedometers during sessions. At the end of the session, observers collected the pedometers and recorded the total steps displayed for each participant.
Goal setting and feedback
Rather than arbitrarily setting goals (e.g., at 10% above the baseline average; Donaldson & Normand, 2009), we used the percentile schedule of reinforcement equation, k = (m + 1)(1 − w), to determine step-total goals for each participant (Galbicka, 1994). In the equation, w (the density of reinforcement) was set to 0.5 and the m value (number of responses included in the calculation) was set at 5 to match the number of sessions during baseline. During the intervention phase, the five most recent step totals were arranged in ascending order. The k value (the third value in the order) was used as the goal for the next session.
Before each session, the primary observer explained to the participants that the pedometer would measure each step they took. The observer then stated the performance goal, wrote it on a sticker, and placed it on the pedometer. When 10 min had elapsed from the start of the session, the observer provided feedback by opening the pedometer, reading the step total, and describing how close the participant was to meeting the goal. At the end of the 20-min session, the experimenter presented the participants who met or exceeded their goal with a prize box and allowed them to choose one item identified by the teacher as highly preferred (e.g., stickers, stamps, pencils, pens, buttons, etc.). Participants who did not meet the goal received no prize and were encouraged to reach their goal during the subsequent session.
RESULTS AND DISCUSSION
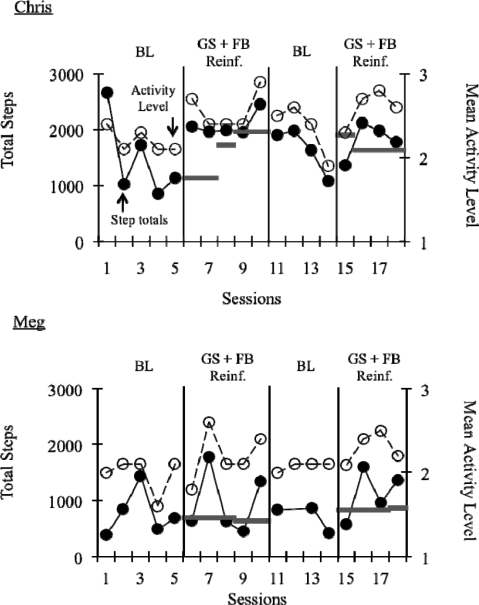
Figure 1 depicts step totals and mean activity level per session for each participant, with the horizontal bars representing the step-total goals. The number of steps taken per session covaried with the mean OSRAC activity level scored per session; both measures indicated a similar degree of change across baseline and intervention phases. For Chris, mean step totals during baseline, intervention, return to baseline, and the final intervention phase were 1,478, 2,082, 1,649, and 1,809, respectively, and he met his goal for 78% of sessions. Mean percentages of intervals engaged in MVPA per phase were 19%, 61%, 48%, and 55%. For Meg, mean step totals during each phase were 769, 965, 706, and 1,125, and she met her goal for 67% of sessions. Mean percentage of intervals engaged in MVPA per phase was 13%, 28%, 12%, and 31%. This correspondence suggests that either method of assessment can be used to evaluate interventions designed to increase physical activity in children.
Figure 1.
Total steps and mean activity level per session for Chris and Meg. Horizontal lines indicate step-total goals.
However, more research is necessary to determine the conditions under which step totals and observed activity levels would differ enough to warrant the use of one measure over another. For example, because of differences in stride length, running a given distance can result in fewer steps being taken than when walking the same distance. Direct observation would then indicate a higher level of activity than would a pedometer. Further, pedometers cannot measure activities that do not involve hip displacement and do not distinguish among activities that require more or less physical exertion. Because pedometers are likely to underestimate activity, they might be preferable to direct observation in some circumstances because they produce more conservative estimates of behavior and behavior change.
The package intervention produced modest increases in activity for Chris when compared to baseline activity levels. However, there was substantial overlap in activity levels across baseline and intervention phases for Meg; thus, the degree to which activity levels changed is questionable for this participant. The intervention might have failed to produce substantial increases in activity because the items available in the prize box were not reinforcers. No formal preference assessment was conducted; instead, all of the teacher-nominated stimuli were included in the prize box. Future research should employ systematic preference assessments, conducted frequently throughout the intervention, to increase the likelihood that effective reinforcers are provided. Also, time constraints precluded extended phases; lengthier intervention phases might produce more robust changes in physical activity.
The specific components of the goal-setting procedures also deserve further evaluation. Step totals did not closely track step-total goals, and participants rarely requested additional feedback during a session or attempted to view the pedometers. These results suggest that general prompts that do not require calculation might be as effective as specific (percentile) goals with preschoolers and that performance feedback might be unnecessary or ineffective. The results also suggest that interventions that teach children to self-monitor using a pedometer might be worthy of consideration. Finally, a number of mechanical devices are available to measure physical activity or indicators thereof, such as accelerometers and heart-rate monitors. The utility of such devices, which are typically more costly than pedometers but produce more detailed information about the intensity of physical activity, warrant consideration with preschoolers.
Acknowledgments
We thank Scott Greenberg, Ella Sargent, and the other members of the behavior analysis research group at the University of the Pacific for their assistance throughout the conduct of this study.
REFERENCES
- Donaldson J.M, Normand M.P. Using goal setting, self-monitoring, and feedback to increase calorie expenditure in obese adults. Behavioral Interventions. 2009;24:73–83. [Google Scholar]
- Epstein L.H, Myers M.D, Raynor H.A, Saelens B.E. Treatment of pediatric obesity. Pediatrics. 1998;101:554–570. [PubMed] [Google Scholar]
- Galbicka G. Shaping in the 21st century: Moving percentile schedules into applied settings. Journal of Applied Behavior Analysis. 1994;27:739–760. doi: 10.1901/jaba.1994.27-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelalian E, Saelens B.E. Empirically supported treatments in pediatric psychology: Pediatric obesity. Journal of Pediatric Psychology. 1999;24:223–248. doi: 10.1093/jpepsy/24.3.223. [DOI] [PubMed] [Google Scholar]
- McIver K, Brown W.H, Pfeiffer K.A, Dowda M, Pate R.R. Assessing children's physical activity in their homes: The observational system for recording physical activity in children—home. Journal of Applied Behavior Analysis. 2009;42:1–16. doi: 10.1901/jaba.2009.42-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie T.L, Sallis J.F, Nader P.R, Patterson T.L. BEACHES: An observational system for assessing children's eating and physical activity behaviors and associated events. Journal of Applied Behavior Analysis. 1991;24:141–151. doi: 10.1901/jaba.1991.24-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Normand M.P. Increasing physical activity through self-monitoring, goal setting, and feedback. Behavioral Interventions. 2008;23:227–236. [Google Scholar]
- Ogden C.L, Carroll M.D, Flegal K.M. High body mass index for age among US children and adolescents, 2003–2006. Journal of the American Medical Association. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C.E, McClain J.J, Hart T.L, Sisson S.B, Washington T.L. Expected values for pedometer-determined physical activity in youth. Research Quarterly for Exercise and Sport. 2009;80:164–174. doi: 10.1080/02701367.2009.10599550. [DOI] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention. Preventing obesity and chronic diseases through good nutrition and physical activity. n.d. Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/fact_sheets/obesity.htm. [Google Scholar]
- VanWormer J.J. Pedometers and brief e-counseling: Increasing physical activity for overweight adults. Journal of Applied Behavior Analysis. 2004;37:421–425. doi: 10.1901/jaba.2004.37-421. [DOI] [PMC free article] [PubMed] [Google Scholar]