Abstract
Background:
Considering the role of T cells in the pathogenesis of periodontitis, the purpose of this study was to compare the amount of IFNγ, IL4 and IL17 in advanced periodontal lesions with healthy gum areas to determine each TH1, TH2 and TH17 cells activity in comparison with each other and finally, to compare the value and the role of humoral, cell mediate and autoimmune responses.
Methods
In this descriptive analytical study, those with moderate to advanced periodontitis, having pocket with 4 to 7 mm in depth, were randomly selected. After preparing the healthy and affected sample tissues, the amount of the specific antibody in I IFNγ, IL4 and IL17 cytokines were measured using ELISA method and were compared between the two groups. The findings were analyzed using the software and descriptive statistical methods and Pearson correlation statistical analysis (α = 0.05).
Results:
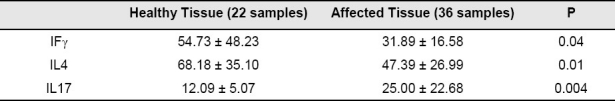
This study was performed on 37 patients with moderate to severe periodontitis and 22 healthy individuals without any periodontal disease. IL4 and IFNγ levels in the patients with chronic periodontitis compared to those of healthy gingival samples showed a significant reduction (P > 0.05) whereas the amount of IL17 in tissue samples of chronic periodontitis compared to healthy gums had a significant increase (P < 0.05).
Conclusion:
It appears that in the periodontitis pathogenesis, as well as TH1 and TH2 responses, IL17 causes the host immunological response to the periodontal pathogenesis.
Keywords: Periodontitis, T Cell, IL17, IL4, IFNγ
Introduction
Chronic periodontitis is an infectious disease that develops to the loss of slowly or moderate.1 The main starter cause of chronic periodontitis is dental plaque accumulation on tooth surface and gingiva in the confluence of teeth and gums (dento gingival junction). Losing attachments and the bone loss is associated with increasing the ratio of gram-negative organisms in the plaque under the gums and increasing organisms that are specifically known as peridonto pathogens. Porphyromonas gingivalis, Tannerella forsythia and Treponema denticola, also known as red complex, are often associated with losing attachments and the bone corrosion in chronic periodontitis. The contrast of pathogenic bacterial and host bacteria is effective in the disease progression.2,3
Microbiological and immunological factors are included in the factors causing the disease. Although periodontal pathogenic bacteria are the factors causing periodontitis, the key to the disease progression and its severity is by the immune responses to infection.4
There are various evidences that show the main destruction factor in the periodontal lesions are caused by the presence of immune cells including monocytes, macrophages and lymphocytes. Specific performance and the response of T cells to the periodontal pathogenic bacteria and the subsequent lack of balance in the T cells configuration mechanism may be involved in the pathogenesis of periodontitis.5 Following bacterial invasion to the periodontal tissue, CD+4 cells enter the lesions and connective tissue and cause the T cells stimulation.6 TH1 is a subgroup cell that produces IL2, IFNγ and TNFα which are called the pre-inflammatory cytokines.7,8 Another cell subgroup is TH2 that produces IL4, IL5, IL6, IL9 and IL13 which are called anti-inflammatory cytokines.9 TH1 and TH2 cells, are responsible for cell-dependent and humoral immune responses, respectively, and each of these two groups in some cases can have inhibitory effect on the other.10
Recently, another type of host response is specified to pathogenic bacteria that is the IL17/IL23 path, and this response occurs when IL23 replaces IL129 and this group plays an important role in configuring autoimmune and inflammatory diseases. IL23 and IL12 have opposite functions; IL12 prevents synthesis of IL17 whereas IL23 causes synthesis evolution.5
IL17 is a cytokine which has a central role in the initiation and persistence of the immune response and this is produced by neutrophils and active CD +4. IL17's main function is to strengthen the immune response by stimulating and secretion of chemokine, cytokine and the cell surface markers.11 IL17 has a great impact on the etiology of inflammatory bone diseases including periodontitis9 and also, it is involved in the progression of infection in chronic periodontitis, chronic obstructive pulmonary disease, diabetes, cardiovascular disease, and rheumatoid arthritis.12
Therefore, the researchers were concentrated on another group of T cells which would produce IL17.9 IL17 cells have effects on osteoclasts maturity as a stimulating factor; therefore, it can have a significant role in bone degradation.13 So, compared to the healthy areas, in advanced lesions, the amount of IL17 which characterizes the IL17 cell activity should be detected in higher levels.14
This study attempted to compare the amount of IL4, IL17, and IFNγ in advanced periodontal lesions with healthy gum areas to determine each TH1, TH2, and TH17 cells activity in comparison with each other and finally, to compare the value and the role of humoral, cell mediate and autoimmune responses.
Materials and Methods
In this descriptive analytical study, those with mod-erate to advanced periodontitis, having pocket with 4 to 7 mm in depth were randomly selected. At the beginning, the patients’ general health and medical history was examined, not having any systemic disease and non-smoking were also other conditions to be reviewed and then, individuals with history of systemic diseases such as diabetes or use of any specific medication in the past six months were excluded.
Gingival tissues of patients who were candidate for 4 to 7 mm packet operation were studied as the test group and the healthy tissue of the teeth areas of pulling teeth candidate were studied as the control group because of orthodontic treatment.
Tissue samples were taken from the moderate to severe periodontitis patients’ 4 to 7 mm packet areas that were flap operation candidates and referred to specialist periodontology department of Isfahan University of Medical Sciences. The samples were taken out of interdental area by scalpel, so that the tissue is contained all the gingival sulcus, junctional epithelium and adjacent connective tissue.
Then, immediately the tissues with the patients’ details on them were placed in microtubes and kept inside the freezer at -70°C degree until the testing time.
To perform ELISA test, the tissues were prepared during the following steps: samples incubation, homogenizing the tissues using Crush method, centrifuging the tubes containing crushed tissue and collecting the superficial fluid solution (supernatant) and finally, aliquot the surface liquid into three equal groups to assess IL4, IL17 and IFNγ cytokines.
To measure the specific antibody for the desired antigen, ELISA method (sandwich) was used. The steps to ELISA method after preparing the samples were as follows: coating the specific antibodies specific for the desired antigens within the microval, adding sample liquid tissue and the standard liquid to attach the antigen to the coated antibodies, adding biotin conjugate, washing out the extra protein and not bonded with the antigens by wash buffer, adding conjugated and labeled with the HRT enzyme specific antibody to microval and adding substrate solution and colored material. After this stage as for the presence of the enzyme (HRT), substrate was converted to product; the amount and intensity of the color in this conversion was proportional to the amount of antibody in the standard tissue and the samples. Then, the reaction was ended by stop solution which was an acid and the amount of its light absorption was 450 nm and then, standard dilution rate and sample concentration were determined using the prepared standard curve for IL4, IL17, and IFNγ cytokines. The amount of IL4, IL17, and IFNγ then was measured in picograms (pg) and the result was determined by standard curve.15
The findings were analyzed using Pearson correlation statistical analysis.
Results
This study was performed on 37 patients with moderate to severe periodontitis and 22 healthy individuals without any periodontal disease. There were 27 males and 10 females with an average range of 42.51 years old in the periodontitis patients and there were 14 males and 8 females with an average range of 42.28 years old in the healthy individuals group.
Mean ± SD of concentration of IFγ, IL4, and IL17 are presented in separated patient tissue group and normal tissue group in Table 1.
Table 1.
Mean ± SD of concentration of IFγ, IL17 and IL4 in normal and patient groups
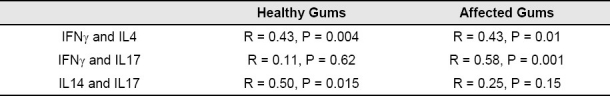
The results from Pearson correlation analysis to investigate the relationship between cytokine in healthy and affected gums are presented in Table 2.
Table 2.
Pearson correlation between the cytokines studied in affected and healthy gums
Discussion
Periodontitis is a disease which causes inflammation and subsequently, tissue destruction by the mediators of the host immune cell; numerous studies have attempted to relate these clinical symptoms to a specific immune system.16 Recently, cytokine studies have become one of the most important aspects of clinical research and it is expected by measuring the cytokine production in clinical performances, they can be used as new markers for diagnosis or treatment. But, as for the number of cytokines involved in the process of immune response and control response is very different, finding several cytokine indices is very essential. Although their clinical application is still not cost-effective, there are many researches done on them.
Our findings indicated that in addition to TH1 and TH2 responses in the periodontitis pathogenesis, IL17 immune track also causes the host immunological response to the periodontal pathogens.
In this study, there was a significant reduction of IFN in the patients with chronic periodontitis compared to the healthy gingival samples. Various studies have been performed in this field and different results have been achieved. According to some studies, IFNγ has a protective role in periodontitis disease so that there is a negative correlation between IFNγ and periodontitis and generally the amount of IFNγ in initial periodontitis lesion is higher than that in the advanced lesions.17
While some studies have reported the cytokine increase in periodontal lesions,18,19 in Gaffen and Hajishengallis17 study which was done on inflammatory cytokine in 2009, IFNγ increase along with IL17 was known as an effective factor in the destructive periodontal lesions and reducing it through anti-cytokine and biological medications. Also, inhibiting the destructive activity was presented as an effective step in treating the destructive periodontal lesions caused by immune system responses.
In a study in Iran, there was not any accompanying and increased IFNγ observed in patients prone to chronic periodontitis and the reason was expressed as not accompanying IFNγ polymorphism genes in these patients.20
In this study, IL4 had a significant reduction in patients with chronic periodontitis compared to healthy gingival samples. Findings of previous studies in this area are contradictory. Some, like our study reported reduction of IL4 in periodontal lesions. Dutzan et al.19 reported a reduction in IL4 in the active area of periodontal lesions compared to the healthy area, while based on Lapin and colleagues’ findings, the TH2 cytokines such as IL4, IL6, IL10 and IL13 are dominant anti-inflammatory in periodontitis lesions.21 In Gaffen and colleagues17 study also no relationship was observed between shortages of IL4 and IL10 cytokines and outbreak of tissue destruction.
In Hooshmand et al.20 study in Iran also no increase in the amount of IL4 was observed in patients with chronic periodontitis and those prone to destructive periodontal lesions.
In our research, there was almost a 100% increase of IL17 in sample tissues with chronic periodontitis comparing to healthy gums. Small number of researches has been done in this field. In 2009, Cardoso conducted some studies about the presence of TH17 in chronic periodontal lesions and concluded that TH17 is present in gum disease and bone corrosions caused by periodontitis; and the evolution and progression of periodontal disease is not because of TH1/TH2 contrast but the existence of these various cytokine profiles under the effect of other factors such as pre-inflammatory function of IL17 which increases more in inflamed tissues and compared to other inflammatory cells in terms of value is not dramatically higher. However, TH17 plays a key role in regulating immune cell population and it is likely that this little but effective production causes damages in homeostasis tissue, a high rate of corrosion lesions and loss of tooth. The presence of IL17 in periodontal lesions is led to production of matrix metalloproteinases (MMP) and also the inflammatory mediators are produced by the gum fibroblasts activation which is a positive loop to boost the inflammatory responses. In rheumatoid arthritis, the T cells use the IL17's ability in producing RANKL to corrupt the bone. IL17 is a major stimulating factor for osteoclast differentiation and activity. Other cytokines such as IFNγ and IL-1β also make RANKL but of course between all, IL17 has a higher rate in making RNAKL; IL17 function can also have a synergy role and as it is considered as a destructive element in rheumatoid arthritis, it can be concluded that they have similar roles in chronic periodontitis and it was observed that they are presented in the host area to deal with gram-negative bacteria.22 Lester said that in addition to TH1 and TH2 responses, this route was another response to periodontal pathogens, but of course he reminded in his research that although these cytokines were either actively damaged or in recovery mode, however, increasing IL17's density together with intensity of adhesion analysis (CAL) suggested this cytokine as a factor in the etiology of inflammation. However, other studies accompanying IL6, IL-1β and IL17 in the patient's sample tissues strengthened the presence of IL17 in the inflamed tissue and this inflammatory response also was emerged even in the presence of TH1 and IL12 and IFNγ cytokines and their lack of robust response to periodontal pathogenic bacteria10 ; and Cardoso mentioned among these the TGFB dual role is noticeable because in one hand it is considered as an anti-inflammatory cytokine and causes FOX +3 reg T cell's evolution22 and also, TH17's evolution on the other hand.11 In Vernal et al.23 study, the high level of IL17 was observed in GCF liquid and supernatant in the periodontitis patients’ cell cultivation. Thus, it seems discovering these cytokines and recognizing the physiological density from the gum tissue's pathologic density will be followed by the possibility of increased credibility and strength performance and it should be noted in treatment that by controlling the immune system and stopping its performance, although the autoimmune destruction is prevented, it causes increased performance of the destructive gram-negative bacteria.
In this study, the amount of IL17, IFNγ and IL4 in chronic periodontitis was examined. In Slots’ study, only the amount of IL17 and its increase in the affected and healthy tissues were assessed.24 In Gaffen et al.17 study about two IL4 and IFNγ cytokines, plenty of discrepancy was observed and it was reminded that this discrepancy can be explained by TH17. As it was expressed in the current study, a significant reduction of IL4 and IFNγ and a significant increase of IL17 were witnessed in the chronic periodontitis. Although the gingival tissue might be healthy in clinical terms, under examination by brush microscopic will be consistently accompanied by inflammation.25 The percentages of lymphocytes in this tissue are alerted and also produce protective sytokines26 because in an injury, the homeostasis system attempts to repair the inflammation or prevent its progression. Therefore, with the presence of booster inflammatory factors, in contrast, the mechanism of anti-inflammatory cytokine production and repair will prevent the lesions development including the TGFB and IL10 which are strongly anti-inflammatory and protective. So it appears that the reduction of two types of cytokines created in early stages of TH1 and TH2 immune response (damage creation process) is controlled by the repair cytokines and as all the cytokines in the process are not measured, there is a gap that the relative reduction of two index cytokines (IL4 and IFNγ) in the affected tissue has a reducing process comparing to healthy tissue and on the other hand, increasing the TGFB cytokine is itself a factor to stimulate and produce IL17.26
Conclusion
According to our study and the correlation coefficient between IFN and IL17, and reduced IFN and increased IL17 in the affected areas, it seems a reason to confirm this theory that increased activity of IL17 causes the suppression of IFN which of course requires wider researches.
The study limitations were as follows: limited available tissue in some cases, on time delivery of prepared tissues to the test environment to prevent the lease of tissues, kits protection, high cost of cytokines diagnostic tests and long time scales to access the kits.
However, it seems that to make practical use of the findings of this study, interaction and collaboration of periodontics and immunologist professionals is essential to do more research, especially in the role of IL17 in the pathophysiology of periodontitis.
Acknowledgments
This article was prepared based on a thesis and a research project (# 387284) approved by the Medical Ethics and Research Office at the Isfahan University of Medical Sciences.
Footnotes
This paper derived from a thesis and a research project No. 387284 in Isfahan University of Medical Sciences.
References
- 1.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Haffajee AD, Socransky SS, Ebersole JL. Survival analysis of periodontal sites before and after periodontal therapy. J Clin Periodontol. 1985;12(7):553–67. doi: 10.1111/j.1600-051x.1985.tb01389.x. [DOI] [PubMed] [Google Scholar]
- 3.Slots J. Subgingival microflora and periodontal disease. J Clin Periodontol. 1979;6(5):351–82. doi: 10.1111/j.1600-051x.1979.tb01935.x. [DOI] [PubMed] [Google Scholar]
- 4.Seymour GJ, Gemmell E, Reinhardt RA, Eastcott J, Taubman MA. Immunopathogenesis of chronic inflammatory periodontal disease: cellular and molecular mechanisms. J Periodontal Res. 1993;28(6 Pt 2):478–86. doi: 10.1111/j.1600-0765.1993.tb02108.x. [DOI] [PubMed] [Google Scholar]
- 5.Romagnani S. Human Th17 cells. Arthritis Res Ther. 2008;10:206. doi: 10.1186/ar2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aarvak T, Chabaud M, Miossec P, Natvig JB. IL-17 Is Produced by Some Proinflammatory Th1/Th0 Cells But Not by Th2 Cells. The Journal of Immunology. 1999;162:1246–51. [PubMed] [Google Scholar]
- 7.Spellberg B, Edwards JE., Jr Type 1/Type 2 immunity in infectious diseases. Clin Infect Dis. 2001;32(1):76–102. doi: 10.1086/317537. [DOI] [PubMed] [Google Scholar]
- 8.Mosmann TR, Sad S. The expanding universe of T-cell subsets: Th1, Th2 and more. Immunol Today. 1996;17(3):138–46. doi: 10.1016/0167-5699(96)80606-2. [DOI] [PubMed] [Google Scholar]
- 9.Yamazaki K, Nakajima T. Antigen specificity and T-cell clonality in periodontal disease. Periodontol 2000. 2004;35:75–100. doi: 10.1111/j.0906-6713.2004.003558.x. [DOI] [PubMed] [Google Scholar]
- 10.Lester SR, Bain JL, Johnson RB, Serio FG. Gingival Concentrations of Interleukin-23 and -17 at Healthy Sites and at Sites of Clinical Attachment Loss. Journal of PeriodontologyAugust. 2007;78(8):1545–50. doi: 10.1902/jop.2007.060458. [DOI] [PubMed] [Google Scholar]
- 11.Fossiez F, Djossou O, Chomarat P, Flores-Romo L, Ait-Yahia S, Maat C, et al. T cell interleukin-17 induces stromal cells to produce proinflammatory and hematopoietic cytokines. J Exp Med. 1996;183(6):2593–603. doi: 10.1084/jem.183.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kramer JM, Gaffen SL. Interleukin-17: a new paradigm in inflammation, autoimmunity, and therapy. J Periodontol. 2007;78(6):1083–93. doi: 10.1902/jop.2007.060392. [DOI] [PubMed] [Google Scholar]
- 13.Sato K, Suematsu A, Okamoto K, Yamaguchi A, Morishita Y, Kadono Y, et al. Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J Exp Med. 2006;203(12):2673–82. doi: 10.1084/jem.20061775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbas AK, Murphy KM, Sher A. Functional diversity of helper T lymphocytes. Nature. 1996;383(6603):787–93. doi: 10.1038/383787a0. [DOI] [PubMed] [Google Scholar]
- 15.Bi Y, Liu G, Yang R. Th17 cell induction and immune regulatory effects. J Cell Physiol. 2007;211(2):273–8. doi: 10.1002/jcp.20973. [DOI] [PubMed] [Google Scholar]
- 16.Honda T, Aoki Y, Takahashi N, Maekawa T, Nakajima T, Ito H, et al. Elevated expression of IL-17 and IL-12 genes in chronic inflammatory periodontal disease. Clin Chim Acta. 2008;395(1-2):137–41. doi: 10.1016/j.cca.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Gaffen SL, Hajishengallis G. A new inflammatory cytokine on the block: re-thinking periodontal disease and the Th1/Th2 paradigm in the context of Th17 cells and IL-17. J Dent Res. 2008;87(9):817–28. doi: 10.1177/154405910808700908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seymour GJ, Gemmell E. Cytokines in periodontal disease: where to from here? Acta Odontol Scand. 2001;59(3):167–73. doi: 10.1080/000163501750266765. [DOI] [PubMed] [Google Scholar]
- 19.Dutzan N, Vernal R, Franco ME, Cisterna C, Dezerega A, Gamonal J. Th1, Th2 and Th17 Cytokines in Progressive Periodontal Lesions. Journal Dent Res. 2008;87:817–28. [Google Scholar]
- 20.Hooshmand B, Hajilooi M, Rafiei A, Mani-Kashani KH, Ghasemi R. Interleukin-4 (C-590T) and interferon-gamma (G5644A) gene polymorphisms in patients with periodontitis. J Periodontal Res. 2008;43(1):111–5. doi: 10.1111/j.1600-0765.2007.01006.x. [DOI] [PubMed] [Google Scholar]
- 21.Lappin DF, Rastan T, Kinane DF. A comparison of costimulatory molecules, and Th1 and Th2 cytokine expression in periodontal disease. J periodontal. 2002;9:10–15. [Google Scholar]
- 22.Cardoso CR, Garlet GP, Crippa GE, Rosa AL, Junior WM, Rossi MA, et al. Evidence of the presence of T helper type 17 cells in chronic lesions of human periodontal disease. Oral Microbiol Immunol. 2009;24(1):1–6. doi: 10.1111/j.1399-302X.2008.00463.x. [DOI] [PubMed] [Google Scholar]
- 23.Vernal R, Dutzan A, Chaparo A. level of inter leukin-17 in gingival tissue from patient with chronic peri-odontitis. J clin periodontal. 2005:383–9. doi: 10.1111/j.1600-051X.2005.00684.x. [DOI] [PubMed] [Google Scholar]
- 24.Slots J. Subgingival microflora and periodontal disease. J Clin Periodontol. 1979;6(5):351–82. doi: 10.1111/j.1600-051x.1979.tb01935.x. [DOI] [PubMed] [Google Scholar]
- 25.Loe H, Holm-Pedersen P. Absence and presence of fluid from normal and inflamed gingivae. Periodontics. 1965;3:171–7. [PubMed] [Google Scholar]
- 26.Oswaldo IP, Gazzinelli RT, Sher A, James SL. IL-10 synergises with IL-4 and transforming growth factor-beta to inhibit macrophage cytotoxic activity. J Immunol. 1992;148:3578–82. [PubMed] [Google Scholar]


