Abstract
Background:
Given the fact that bruxism is a prevalent oral habit among children and a potential destructor of oral tissues, the present study aimed to investigate the relationship between intestinal parasitic infections and bruxism among kindergarten children.
Methods:
Questionnaires were administered among parents of kindergarten children in Isfahan to select 50 children identified by their parents to have the habit of bruxism and 50 without the habit as control group. Informed consent was obtained prior to the investigation. Parents were delivered sampling instruments with proper instructions to collect stool samples from both groups for parasitological tests. The diagnostic parasitological tests involved the direct stool smear, formol-ether concentration, and Scotch tape tests. Comparison for the frequency distribution of intestinal parasitic infections between the two groups was performed using the chi-square test (α = 0.05).
Results:
Parasitic infections were observed in 19 (11/50 cases and 8/50 controls) children. A statistically significant relationship was observed between infection with pathogenic parasites and bruxism (P < 0.05).
Conclusion:
Our findings suggest that pathogenic parasites may serve as the cause of initiation of bruxism habits among children.
Keywords: Bruxism, Child, Parasites, Parasitic diseases, Pathogenicity
Introduction
Prevention is generally known to be an effective measure in reducing dental defects due to negligence of dental care during childhood. Moreover, while the selection of a proper preventive measure for any disease drastically draws upon its etiological factors, oral habits are considered as one of the environmental etiological factors causing orthodontic problems. Based on these considerations, population-based surveys are strongly required to collect statistical and epidemiological information to be used as foundations for detecting the present and future health care requirements of the population under study. The information will further serve as a basis for monitoring levels of oral symptoms and the associated problems due to oral habits.1
Bruxism is a predominant oral habit which is potentially destructive to oral tissues. Bruxism is defined as the nonfunctional, mostly nocturnal, grinding or clenching of teeth during sleep.2 Most children, however, tend to exhibit the habit diurnally as well.3 If continued over long periods of time, the habit leads to wear and erosion of both primary and permanent teeth.2 Attanasio4 and Cash5 declared that bruxism is a periodic trait of all children. Most children are found to have the habit, which in most cases, causes a moderate wear of their primary canines and molars. In extremely few cases (except for mental retarded children) the wear is severe enough to cause secondary dentin formation, thus endangering dental pulp. Masticatory muscle and temporo-mandibular joint pains have also been attributed to bruxism. While no definitive factor for initiation of bruxism has yet been identified, attention has been mostly concentrated on likely local, general, and psychological factors.6
The systemic factors of bruxism include intestinal parasites, subclinical nutritional deficiencies such as calcium and magnesium deficiencies, allergies, and endocrine disturbances.3 Bruxism due to intestinal parasites can be attributed to metabolites known as non-specific proteins which often have toxic effects and are secreted from the parasite during its various stages of life.7 Such symptoms as nervousness, insomnia, and teeth grinding are typically ascribed to Enterobius vermicularis, Ascaris lumbricoides8 and other parasites.9–13 The intestinal parasites are generally classified as helminthes, protozoa, and arthropods, helminthes being of utmost importance on a world scale due to their prevalence and severity of their verminous intoxification.7 The most common pathogenic intestinal parasites in children are Enterobius vermicularis and Giardia lamblia while the most common nonpathogenic ones are Entamoeba coli and Endolimax nana.14–18 The objective of the present study was to investigate the relationship between parasitic infections and bruxism in children.
Materials and Methods
This analytic, short-term study investigated a population of 100 children of 3 to 6-year-old in kindergartens in the city of Isfahan, Iran. Permit was initially obtained from the relevant authorities to visit a number of kindergartens, in which 50 children with bruxism and 50 without the habit were selected. Parents of both groups of children were then called to a one-day workshop to receive training and instructions on sample collection using three-a-day Scotch tapes. Sample containers with an instruction manual were given to each parent. Three fecal samples were collected one every other day along with Scotch tapes, which were all delivered to the kindergarten at specified dates. The samples were then transferred to the parasitological lab at the School of Medicine for direct stool smear and formol-ether concentration tests. The direct stool smear is the easiest and simplest parasitological test requiring a minimum of stool and equipment. According to this method, physiological serum and lugol's solution is used to make a smear of the stool for examination under the microscope. Parasitic ova and larvae, trophozoites, and protozoan cysts can be easily detected in the stool smear.19 In the formalin-ether concentration method, about 1 to 2 grams of the stool was emulsified in 8 ml of formalin, then was strained through two layers of wet gauze directly into a 15 ml conical centrifuge tube. Then, it was sieved through strainers, to which 3 ml of ether was added, and finally centrifuged at 1000 rpm for 5 minutes. An advantage of the technique is the high probability of detecting infections as a greater quantity of the faeces is tested. The Scotch tape method is used for detecting Enterobius vermicularis because this parasite lays its eggs outside the intestine on the peri-anal area which is also the reason for the severe epidermal pruritus around the anus. The sample was taken from peri-anal skin in the morning before washing peri-anal area. This is because this parasite lays its eggs outside the intestine on the peri-anal area, which is also the reason for the severe epidermal pruritus around the anus. The tape was manually adhered to the anus to ensure full contact with the wrinkles of the area. The tape was then removed and stuck on the microscope slide for lab tests. Ova and larvae of the parasites were detected under the microscope.7–9,19
Comparison of the frequency distribution of intestinal parasitic infections between the two groups was performed. The relationship between family histories of bruxism and child habit of bruxism and also the relationship between systemic factors and initiation of bruxism were evaluated. Chi-square test was used to compare the data. P value less than 0.05 was considered significant.
Results
Out of 100 subjects examined, 19 children were found to be infected with parasites. The most common pathogenic parasite species found in this study, in order of the highest to the lowest frequency, were Enterobius vermicularis, Giardia lamblia and Hymenolepis nana, while the most common nonpathogenic ones included Entamoeba coli and Endolimax nana. Among the children with bruxism (the case group), 11/50 children and among the control group, 8 children (8/50) were found to be infected with intestinal parasites.
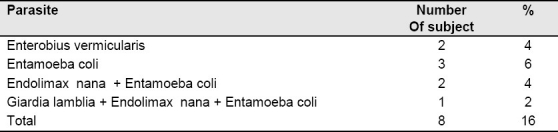
The frequency of pathogenic parasites in the case group showed a significant difference from that in the control group (P < 0.05). The details of the parasitological investigations in each of the two groups are summarized in Tables 1 and 2. Also, the prevalence of Enterobius vermicularis (8/50 in the case group and 2/50 in the control group) indicated a significant relationship between infection with this parasite and the development of bruxism habits (P < 0.05).
Table 1.
Prevalence of parasitic infections in the case group
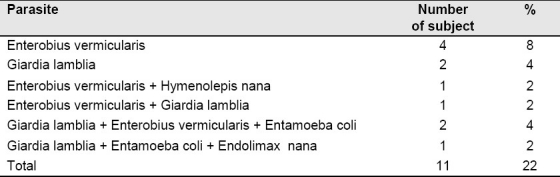
Table 2.
Prevalence of parasitic infections in the control group
Family bruxism histories were reported in 24% of the case group and in 2% of the control one, which also indicates a significant difference (P < 0.05). The relationships between systemic factors and initiation of bruxism were not statistically significant.
Discussion
Most people, including adults and children, get into degrees of nocturnal bruxism habit in one stage of their lives. The chewing muscles normally adapt themselves to this behavior but in some people, the accumulation of muscular energy build-up goes beyond the person's capacity leading to a number of malfunctions in the patient. A number of studies have suggested psychological stresses to be the most stable and persistent factors of bruxism.3–5 However, bruxism may also be caused by such systemic factors as parasitic infections.3,12 Along with these lines, the present study was carried out to investigate the relationship and the correlation between parasitic infections and bruxism in 3 to 6-year-old children. For the purpose of this study, the case and the control groups were compared for the frequency of parasitic infections. A general parasitic infection frequency of 19/100 was obtained in the population of 100 children studied, which was relatively lower than the findings reported by previous studies in Iran and other countries.14–18 A few points can be mentioned to clarify this difference: Higher hygiene standards achieved by the society compared to the past; the samples used in this study were collected from children who were educated in kindergartens, which indicates a higher socio-economic status of their families and, hence, the lower parasitic infections observed; and during the period when this study was being carried out, the drinking water supplies in Isfahan were contaminated with oil leaks so that most families lived on water bottles. This naturally had almost completely eliminated a major source of infections.
The frequency of parasitic infections does not indicate any significantly greater frequency rate in the case group. However, since all the 11/50 of the detected infections in the case group included pathogenic parasites while from the 8/50 parasitic infections found in the controls, only 3/50 involved pathogenic infections, a statistically significant relationship can be established between parasitic infection and bruxism. Furthermore, infection with Enterobius vermicularis showed a statistically significant difference between the two groups. In a similar study in Brazil, Diaz-Serrano found higher parasitic infection prevalence in the control than in the case group, which indicated no relationship between bruxism and parasitic infections. It needs to be mentioned, however, that Diaz-Serrano only used the conventional precipitation technique in his study, which is not a reliable technique, and that he used far less subjects.20 The diagnostic parasitological tests in this study involved the direct stool smear, formol-ether concentration, and Scotch tape tests. In a different study, such habits as bruxism and anal pruritus were compared between two groups with parasitic infections and without such infections and found considerable and interesting results in the group with parasitic infections.21
The present study revealed a statistically significant relationship between family histories of bruxism and child habit of bruxism. Although our findings indicated no statistically significant relationships between systemic factors and initiation of bruxism, the considerable enhancement of the symptoms (i.e., anal pruritus, gum or nasal bleeding, nocturnal enuresis, etc.) in the case group compared to the control warrants more extensive research into this relationship.
Conclusion
Our findings suggest that pathogenic parasites may serve as the cause of initiation of bruxism habits among children.
Acknowledgments
This article was prepared based on a doctoral thesis approved by the Medical Ethics and Research Office at the Isfahan University of Medical Sciences. The authors would like to extend their most sincere thanks to Torabinejd Dental Research Center and Dr. Soleimani. The staff members of the Deputy for Research of the School of Dentistry as well as the Dean and the staff members of the Department of Mycology and Parasitology of the School of Medicine; they deserve special thanks for their support and cooperation during the execution of this research project.
Footnotes
This paper derived from a doctoral thesis in Isfahan University of Medical Sciences.
References
- 1.Winocur E, Littner D, Adams I, Gavish A. Oral habits and their association with signs and symptoms of temporomandibular disorders in adolescents: a gender comparison. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(4):482–7. doi: 10.1016/j.tripleo.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Graber TM, Vanarsdall RL. Orthodontics: Current Principles and Techniques. 3rd ed. Philadelphia: C.V. Mosby; 2000. pp. 326–8. [Google Scholar]
- 3.Christensen JR, Fields HW, Adair SM. Oral habits. In: Pinkham JR, editor. Pediatric dentistry: infancy through adolescence. Philadelphia: Elsevier Saunders; 2005. pp. 437–8. [Google Scholar]
- 4.Attanasio R. Nocturnal bruxism and its clinical management. Dent Clin North Am. 1991;35(1):245–52. [PubMed] [Google Scholar]
- 5.Cash RC. Bruxism in children: review of the literature. J Pedod. 1988;12(2):107–27. [PubMed] [Google Scholar]
- 6.Kuch EV, Till MJ, Messer LB. Bruxing and non-bruxing children: a comparison of their personality traits. Pediatr Dent. 1979;1(3):182–7. [PubMed] [Google Scholar]
- 7.Craig CF, Faust EC. Clinical Parasitology. 8th ed. Philadelphia: Lea and Febiger; 1970. p. 67. [Google Scholar]
- 8.Ormazdi H. Tehran University of Medical Sciences and Health Services. 1st ed. 2007. Medical Parasitology: Entomology; pp. 191–208. [Google Scholar]
- 9.Brown HW, Neva FA. Basic Clinical Parasitology. 5th ed. New York: Appleton-Century-Crofts; 1993. p. 130. [Google Scholar]
- 10.Arfaa F. Medical helminthology. Tehran: Dibaj Press; 2010. p. 185. [Google Scholar]
- 11.Bogitsh BJ, Cheng TC. Human Parasitology. 1st ed. London: Academic Press; 1990. pp. 215–30. [Google Scholar]
- 12.Athari A. Essential of Helminthology. 1st ed. Tehran: Noor va Danesh; 2002. pp. 37–47. [Google Scholar]
- 13.Cook GC, Zumla AI. Manson's Tropical Diseases. 21st ed. Philadelphia: Saunders Ltd; 2002. pp. 215–40. [Google Scholar]
- 14.Baghai M, Pestehchian N, Alavi Naeini Z. Infection with intestinal parasites in students of exceptional and ordinary city: 1375-1376 academic year. Journal of Isfahan University of Medical Sciences. 1999;4(2-3):62–5. [Google Scholar]
- 15.Menezes AL, Lima VM, Freitas MT, Rocha MO, Silva EF, Dolabella SS. Prevalence of intestinal parasites in children from public daycare centers in the city of Belo Horizonte, Minas Gerais, Brazil. Rev Inst Med Trop Sao Paulo. 2008;50(1):57–9. doi: 10.1590/s0036-46652008000100013. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen KH, Ribeiro PS, Quist BK, Rydbeck BV. Prevalence of intestinal parasites in young Quichua children in the highlands of rural Ecuador. J Health Popul Nutr. 2007;25(4):399–405. [PMC free article] [PubMed] [Google Scholar]
- 17.Astal Z. Epidemiological survey of the prevalence of parasites among children in Khan Younis governorate, Palestine. Parasitol Res. 2004;94(6):449–51. doi: 10.1007/s00436-004-1234-1. [DOI] [PubMed] [Google Scholar]
- 18.Waikagul J, Krudsood S, Radomyos P, Radomyos B, Chalemrut K, Jonsuksuntigul P, et al. A cross-sectional study of intestinal parasitic infections among schoolchildren in Nan Province, Northern Thailand. Southeast Asian J Trop Med Public Health. 2002;33(2):218–23. [PubMed] [Google Scholar]
- 19.Garsia LS. Diagnostic Medical Parasitology. 4th ed. Washington: American Society for Microbiology; 2001. pp. 14–8. [Google Scholar]
- 20.Diaz-Serrano KV, da Silva CB, de Albuquerque S, Pereira Saraiva MC, Nelson-Filho P. Is there an association between bruxism and intestinal parasitic infestation in children? J Dent Child (Chic) 2008;75(3):274–9. [PubMed] [Google Scholar]
- 21.Cazorla D, Acosta M, Garci’a E, Garvett M, Ruiz A. Enterobius vermicularis infection in preschool and schoolchildren of six rural communities from a semiarid region of Venezuela: A clinical and epidemiological study. Helminthologia. 2006;43(2):81–5. [Google Scholar]


