Abstract
Excessive alveolar bone resorption is commonly found when teeth are extracted. This is a problem in anterior part of mouth because it will result in an unaesthetic pontic on a narrow hollowed out alveolar ridge. Yet, another problem is gingival recession and root exposure in adjacent teeth which represent a therapeutic problem to the clinician.
Use of acellular dermal matrix graft is an appropriate solution to obtain root coverage in areas with localized or generalized soft tissue recessions, particularly if the recessions create aesthetic concern or root sensitivity or shallow root caries lesions. This case report describes a surgical technique using acellular dermal matrix graft on a class III ridge defect and Millers grade II gingival recessions.
There was a gain in both bucco-lingual and apico-coronal dimensions of the ridge, in both height and width directions, when compared to baseline and after 3 months. Recession was also covered compared to the baseline condition.
Keywords: Acellular dermal matrix, Alveolar ridge augmentation, Gingival recession, Root coverage
Introduction
Ridge augmentation using soft tissue solely to correct the esthetic problem of an anterior vertical ridge defect was reported by Meltzer 1979.1 Later in 1980 and 1982, Langer and Calagna2 demonstrated ridge augmentation using connective tissue. Gingival recession and root exposure along with soft tissue defect in adjacent edentulous space often pose a therapeutic problem to the clinician.
To obtain root coverage in areas with localized or generalized soft tissue recessions, Miller's class I and II, particularly if the recessions create aesthetic or root sensitivity problems or shallow root caries lesions, and to augment alveolar ridge, soft tissue allografts such as alloderm can be successfully used. This material can also be used in Miller's class I and II gingival recessions.
Acellular dermal matrix graft (ADM) was used in this case report for ridge augmentation and for root coverage.
Alloderm is a donated human soft tissue that is processed to remove its dermal cells, leaving a regenerative collagen matrix behind. It provides components needed to allow the body to restore the missing tissue, with fast healing and excellent cosmetic results. Alloderm is ideal for the patients either lack adequate harvestable tissue or are not willing to undergo a palatal surgery.
ADM is widely used in ridge augmentation and is also used as a substitute for free gingival graft, root coverage and cell occlusive barrier for bone grafting around dental implants, septal perforation repair, and guided tissue regeneration (GTR) matrix.
This allograft is a freeze dried cell free dermal matrix comprised of structurally integrated basement membrane complex and extra cellular matrix, in which collagen bundles and elastic fibers are main components. It is available in two different ranges of thicknesses 0.9-1.6 mm (alloderm), and 0.5-0.9 mm (alloderm GBR).
It has two distinct surfaces; the basement membrane surface (BM) is smooth and does not absorb blood, whereas the connective tissue side (CT) is rough and absorbs blood.
Case Report
A healthy 30 year old male reported to the Department of Periodontics, Rajah Muthiah Dental College and Hospital, Tamilnadu, India with a chief complaint of missing teeth along with unpleasant look in relation to lower anteriors.
Dental history revealed that he had extracted his teeth due to trauma before 10 years of age. Presurgical examination showed a class III ridge defect, 3 mm in height (SEIBERT 1983)1 with a ridge thickness of 3 mm (Figure 1A).
Figure 1.

(A) Preoperative view of defect. (B) Mechanical debridement was done.
Grade II gingival recession had the following characteristics: recession width of 3 mm in lower left lateral incisors, recession depth of 5 mm in lower left lateral incisor and 3 mm width and depth in right lower lateral incisor. Phase I therapy was performed of complete scaling and root planning (Figure 1B).
The case was taken up for ridge augmentation and root coverage using ADM graft (Alloderm- Regenerative Tissue Matrix, BioHorizon, Lifecell). The patient was explained about the procedure and a return consent obtained.
Surgical Procedure
sutured to lingual gingival tissue with resorbable suture. Labially, flap was positioned coronally and sutured to completely cover the allograft. The acellular dermal matrix graft was placed against the root surfaces with its connective tissue side facing the overlying gingival flap. It was sutured using a sling suture technique with a synthetic 5-0 bioabsorbable suture. After placement of the acellular dermal matrix graft, the flap was coronally positioned and sutured using a sling suture technique. The releasing incisions were closed with interrupted sutures and periodontal dressing was given using coe pak (Figures 2G and 2H).
Figure 2.
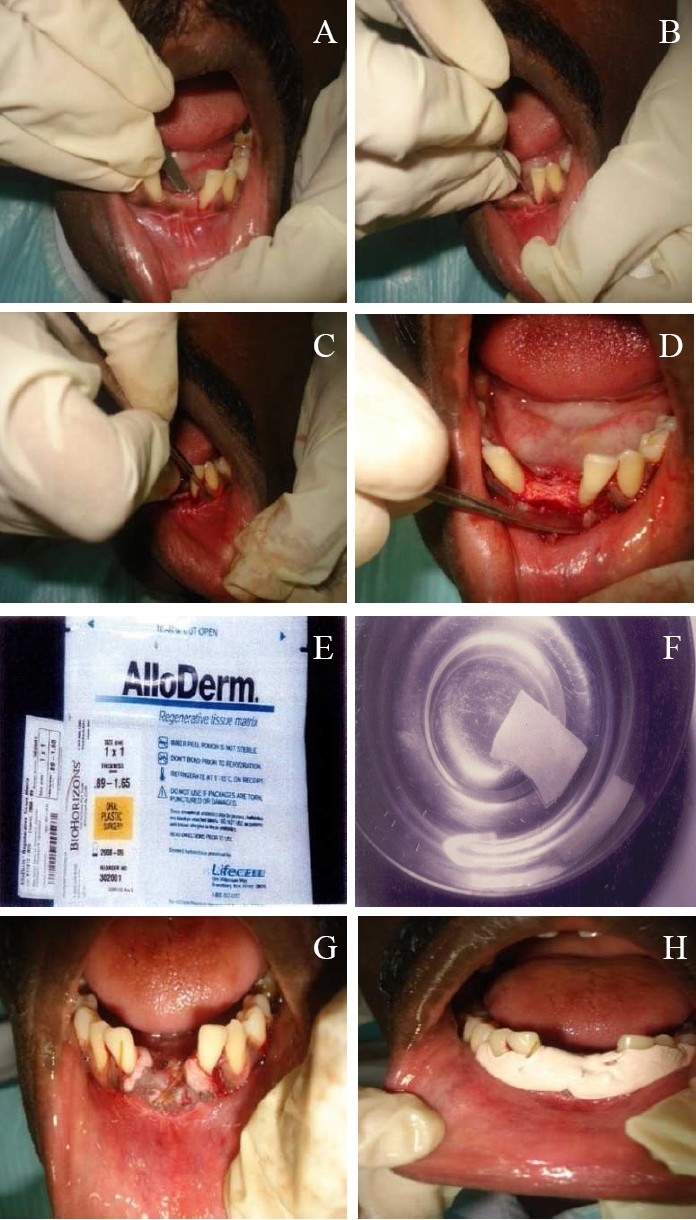
(A) Horizontal incision was given. (B) Crevicular incision was given. (C) Vertical releasing incision. (D) Flap elevated. (E) Alloderm (ADM). (F) ADM graft in saline (G) ADM graft sutured. (H) Coe pack was given.
Post Surgical Care
Patient was instructed to discontinue tooth brushing for 30 days around surgical site, but rinse with 0.12% chlorhexidine solution twice a day. Systemic antibiotics were prescribed along with analgesics for 5 days postsurgically (amoxicillin 500 mg, plus aceclofenac and paracetamol combination).
Patient was recalled after one week and checked for healing. The surgical site was repacked (Figure 3A). Again he was recalled after 2 weeks (Figure 3B), 3 weeks, 1st month (Figure 3C) and 3rd month (Figure 3D). After 3 months, the patient was referred to Department of Prosthodontics for fixed prosthesis.
Figure 3.
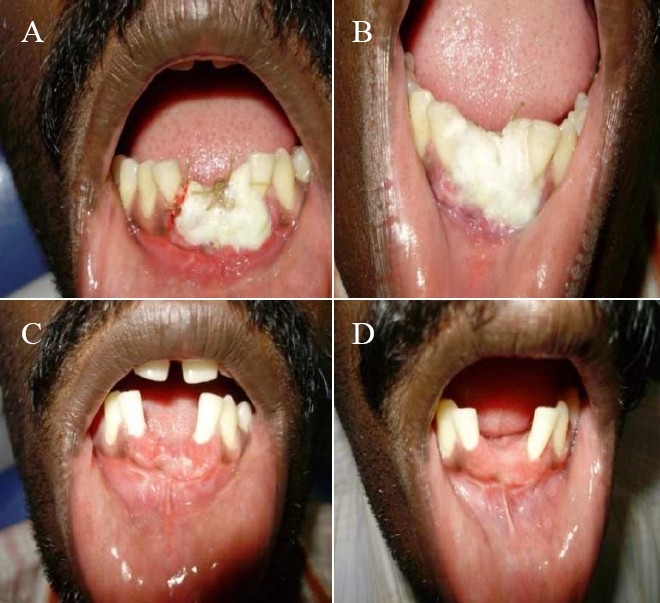
(A) 1st week postoperative condition. (B) 2nd week postoperative condition. (C) 1st month postoperative condition. (D) 3nd month postoperative condition.
Results
A gain in thickness of ridge for 6 mm (3 mm gain compared to the baseline), and a gain in height for 5 mm (2 mm gain compared to the baseline) were obtained using acellular dermal matrix graft. There were gains in both buccolingual and apicocoronal directions of the ridge (gain in both height and width).
Recession depth was reduced to 3 mm in left lower lateral incisor and 2 mm in right lower lateral incisor when compared to baseline using acellular dermal matrix graft.
Discussion
Ridge augmentation using soft tissue solely to correct the esthetic problem of an anterior vertical ridge defect was published by Meltzer in1979.1
Later, many clinicians contributed further by modifying the procedures. Ridge augmentation using connective tissue was described by Langer and Calagna in 1980 and 19821. Garberg and Rosenburg in 19811 introduced pouch technique.
Griffin et al.3, studied the use of acellular dermal matrix to correct soft and hard tissue defects in implants. Correction of ridge deformity caused by a root fracture, submerging of an existing implant, correction of recession defects around adjacent teeth, and ridge preservation for implant placement were presented.
Improving the quality of patient care is vital. Over the years, various studies have been done to obtain predictable root coverage in patients with gingival recession defects, subpedicle acellular dermal matrix graft and autogenous connective tissue graft in the treatment of gingival recession. Luczyszyn et al.4 used acellular dermal matrix and hydroxyapatite in prevention of ridge deformities after tooth extraction.
Mehlbauer and Greenwell5 studied the complete root coverage at multiple sites using an acellular dermal matrix allograft. Griffin et al.3 reconstructed amalgam tattoo surgically, using acellular dermal matrix graft. ADM was used as an alternative source to donor tissue site in this type of surgery.
Shin et al.6 carried out “a comparative study of root coverage using acellular dermal matrix with and without enamel matrix derivative” and concluded that the use of EMD in conjunction with ADM results in a statistically significant effect on keratinized tissue increase, but had no significant effects on probing attachment level or percentage of root surface coverage.
Recently, ADM was used as a substitute for free gingival graft to increase the width of keratinized tissue around the teeth for treatment of alveolar ridge defects, and for root coverage to overcome the need of second surgical site to harvest graft.7
Woodyard et al.8 studied the effects of the use of ADM on gingival thickness and root coverage amount compared to coronally positioned flap (CPF) alone and concluded that CPF plus ADM allograft significantly increased the gingival thickness when compared with CPF alone. The coverage of gingival recession was significantly improved with the use of ADM.
Cortes et al.9 studied the use of coronally positioned flap with or without acellular dermal matrix graft in the treatment of class I gingival recessions in a randomized controlled clinical study. They aimed to clinically evaluate the outcome of the treatment of class I gingival recession by coronally positioned flap procedure with or without ADM and concluded that both techniques can provide significant root coverage in class I gingival recessions; however, a greater keratinized tissue thickness might be expected with ADM.
Conclusion
There was a gain in ridge in both buccolingual and apicocoronal directions, both in height and width. The use of acellular dermal matrix prevents the need of a second surgical site for donor material. It also enhances patient's comfort and satisfaction with the procedure. However, further studies involving more defects and longer follow up periods are required to ascertain the efficacy of acellular dermal matrix in the management of ridge augmentation and root coverage.
References
- 1.Henzi D, Davis E, Jasinevicius R, Hendricson W, Cohen ES. Atlas of cosmetic and reconstructive periodontal surgery. 3rd ed. Canada: B.C. Decker; 2007. pp. 325–9. [Google Scholar]
- 2.Griffin TJ, Cheung WS, Hirayama H. Hard and soft tissue augmentation in implant therapy using acellular dermal matrix. Int J Periodontics Restorative Dent. 2004;24(4):352–61. [PubMed] [Google Scholar]
- 3.Griffin TJ, Banjar SA, Cheung WS. Reconstructive surgical management of an amalgam tattoo using an acellular dermal matrix graft: case reports. Compend Contin Educ Dent. 2005;26(12):853–9. [PubMed] [Google Scholar]
- 4.Luczyszyn SM, Papalexiou V, Novaes AB, Jr, Grisi MF, Souza SL, Taba M., Jr Acellular dermal matrix and hydroxyapatite in prevention of ridge deformities after tooth extraction. Implant Dent. 2005;14(2):176–84. doi: 10.1097/01.id.0000165082.77499.41. [DOI] [PubMed] [Google Scholar]
- 5.Mehlbauer MJ, Greenwell H. Complete root coverage at multiple sites using an acellular dermal matrix allograft. (730-3).Compend Contin Educ Dent. 2005;26(10):727–8. [PubMed] [Google Scholar]
- 6.Shin SH, Cueva MA, Kerns DG, Hallmon WW, Rivera-Hidalgo F, Nunn ME. A comparative study of root coverage using acellular dermal matrix with and without enamel matrix derivative. J Periodontol. 2007;78(3):411–21. doi: 10.1902/jop.2007.060170. [DOI] [PubMed] [Google Scholar]
- 7.Yan JJ, Tsai AY, Wong MY, Hou LT. Comparison of acellular dermal graft and palatal autograft in the reconstruction of keratinized gingiva around dental implants: a case report. Int J Periodontics Restorative Dent. 2006;26(3):287–92. [PubMed] [Google Scholar]
- 8.Woodyard JG, Greenwell H, Hill M, Drisko C, Iasella JM, Scheetz J. The clinical effect of acellular dermal matrix on gingival thickness and root coverage compared to coronally positioned flap alone. J Periodontol. 2004;75(1):44–56. doi: 10.1902/jop.2004.75.1.44. [DOI] [PubMed] [Google Scholar]
- 9.Cortes AQ, Martins AG, Nociti FH, Jr, Sallum AW, Casati MZ, Sallum EA. Coronally positioned flap with or without acellular dermal matrix graft in the treatment of Class I gingival recessions: a randomized controlled clinical study. J Periodontol. 2004;75(8):1137–44. doi: 10.1902/jop.2004.75.8.1137. [DOI] [PubMed] [Google Scholar]


