Abstract
The term internal derangement was first adopted to describe any pathologic entity that interfered with the smooth function of the temporomandibular joint (TMJ). The term is currently used exclusively to describe alterations in disc–fossa relations. Internal derangement of the TMJ does not always cause pain, although when the disc becomes displaced, noises and locking can occur and ligamentous, capsular or retrodiscal pain may dominate the clinical picture. Meniscopexy of TMJ was done in ten patients where clinical features suggest true internal derangement of the TMJ refractory to conservative treatment with restricted movement and pain identified as arising primarily from the joint. Magnetic resonance imaging was done to identify the cause of problem.
Keywords: Meniscopexy, Internal derangement, Temporomandibular joint, Magnetic resonance imaging
Introduction
Treatment of patients with internal derangement of the TMJ typically begins with nonsurgical treatment modalities. Bite appliance therapy, diet modifications, nonsteroidal anti-inflammatory medications, muscle relaxants, moist heat or ice, and physical therapy have been found to be efficacious. Surgical intervention in the cases of internal derangement of TMJ is a controversial issue. It is generally contemplated in refractory cases not responding to conservative management. There are several surgical options which include open operation (arthrotomy) or closed operation (arthroscopy or arthrocentesis). Though there are many clinical studies on the results of arthroscopy and arthrocentesis, which show their benefits and limitations [1], but arthroscopic instruments are not available in most of the institutes. Several open surgical techniques have been described [2], but there have been few studies of long term results. Meniscopexy was carried out to return the patient to a regular diet, with some limitations, and to establish an adequate functional range of motion of mouth opening. It also included preservation of articular tissue to permit normalization and regeneration of synovium, and a restoration of the articular relations to permit the joint structures to adapt and function through an adequate range of motion.
Patients and Methods
Twenty meniscopexies were carried out under general anaesthesia in 10 radiologically (magnetic resonance imaging) and clinically diagnosed refractory cases of internal derangement patients not responding to the conservative management. These patients were initially placed on conservative approach for 6 months like bite appliance therapy, diet modifications, nonsteroidal anti-inflammatory medications, muscle relaxants, moist heat or ice, and physical therapy. Seven patients out of 10 were females and 3 were males. Average preoperative mouth opening was 25.9 mm. During the postoperative period limited mouth opening and soft diet was advised for 2 weeks. Thereafter active mouth opening exercises were carried out to achieve normal range of mouth opening. In active mouth opening patients were instructed to open until they perceive pain and then advised to hold for several seconds and repeat this exercise several times a day. An active lateral stretch permitting the contralateral lateral pterygoid to be stretched may be accomplished by visualizing themselves in a mirror. In the active protrusion, also performed in front of the mirror, the mandible is protruded forward stretching the lateral pterygoids bilaterally. All active excursions are maintained for several seconds and slowly released. All the cases were assessed clinically and radiologically on monthly basis for 1 year (Table 1). The criteria for success are to return the patient to a regular diet, with some limitations, and to establish an adequate functional range of motion. The goals for all surgical procedures should include preservation of articular tissue to permit normalization and regeneration of synovium, and a restoration of the articular relations to permit the joint structures to adapt and function through an adequate range of motion.
Table 1.
Results obtained following meniscopexy
| S No. | Age/sex | Side | Type of internal derangement | TMJ pain | TMJ click | Preop mouth opening (mm) | Follow up (years) | Pain relief | Reduction in TMJ noise | Postop mouth opening (mm) | Stable disc reduction at 1 year | Relapse of the disc reduction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | F | R&L | Non reducing disc displacement | Yes | Yes | 24 | 1 | Yes | No | 36 | No | Yes |
| 2 | F | R&L | Reducing disc displacement | Yes | Yes | 28 | 1 | Yes | Yes | 35 | Yes | No |
| 3. | M | R&L | Non reducing disc displacement | Yes | Yes | 24 | 1 | Yes | No | 38 | No | Yes |
| 4. | F | R&L | Reducing disc displacement | Yes | Yes | 32 | 1 | Yes | No | 38 | No | Yes |
| 5. | M | R&L | Reducing disc displacement | Yes | Yes | 34 | 1 | Yes | Yes | 38 | Yes | No |
| 6. | F | R&L | Reducing disc displacement | Yes | Yes | 26 | 1 | Yes | Yes | 38 | Yes | No |
| 7. | F | R&L | Non reducing disc displacement | Yes | Yes | 20 | 1 | Yes | Yes | 32 | Yes | No |
| 8. | M | R&L | Non reducing disc displacement | Yes | Yes | 23 | 1 | Yes | Yes | 35 | Yes | No |
| 9. | F | R&L | Non reducing disc displacement | Yes | Yes | 24 | 1 | Yes | Yes | 34 | Yes | No |
| 10. | F | R&L | Non reducing disc displacement | Yes | Yes | 24 | 1 | Yes | Yes | 38 | Yes | No |
Technique
The TMJ was approached through Popowich & Crane’s modification of Alkayat & Bramley’s preauricular incision to permit anterior mobilization of the tissue and exposure of the capsule of the TMJ (Fig. 1). The access incision is extended inferiorly by 10 mm, to give access to the condylar neck below the capsule. Patients with arthrosis or condylar atrophy will have lost much of the condylar head and care should be taken to remain close to the capsule and periosteum of the condylar neck so as to avoid damage to the superior branches of the facial nerve. Anteriorly the periosteum over the eminence is raised to reach its anterior border, and posteriorly the preauricular “avascular zone” deepened behind the capsule of the joint to more than half its width. To prevent bleeding later as the meniscus is mobilized, 1 ml of 1:200,000 adrenaline is injected into the upper joint space through the capsule. An elliptical incision is made on the capsule and redundant tissue is removed (Fig. 2). The meniscus is mobilised and is sutured from medial to lateral aspect. The meniscus is pulled and held over the lateral pole by interrupted 4-0 proline sutures (Fig. 3). The capsule is closed with interrupted 4-0 proline sutures (Fig. 4). The operated site is closed in layers after placing the drain which was removed after 72 h.
Fig. 1.

Popowich & Crane’s modification of Alkayat & Bramley’s preauricular incision
Fig. 2.
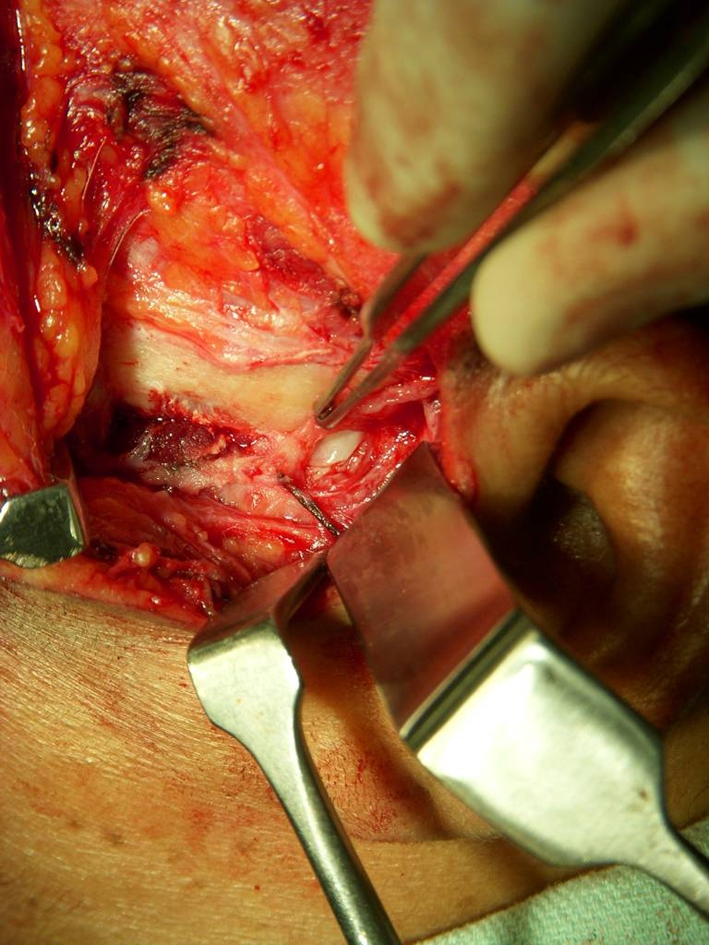
An elliptical incision is made on the capsule and redundant tissue is removed and meniscus is pulled
Fig. 3.
Meniscus is held over the lateral pole by interrupted 4-0 proline sutures
Fig. 4.
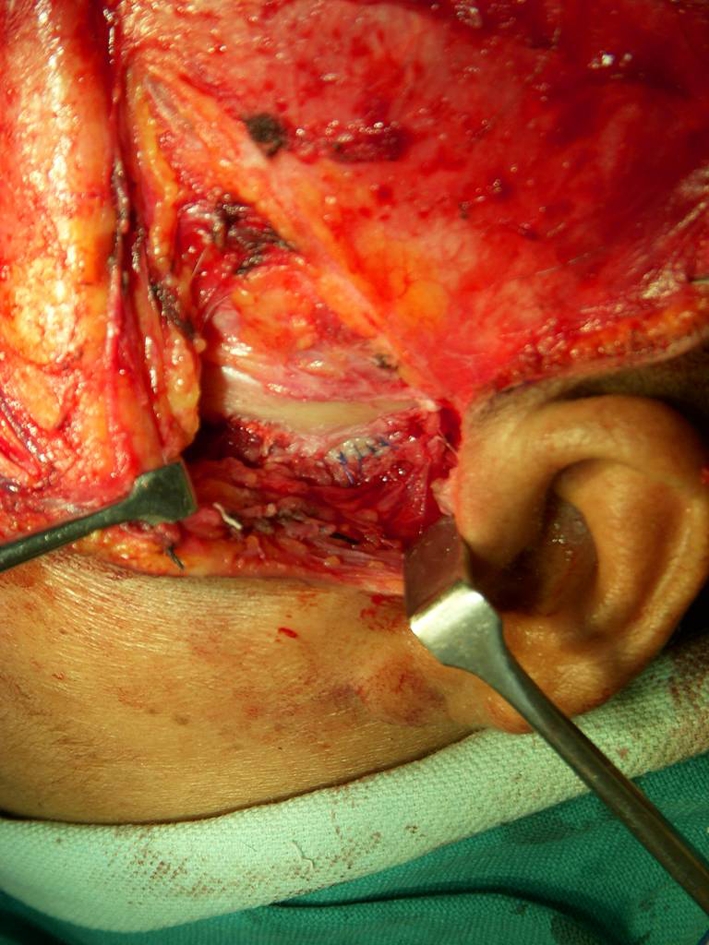
The capsule is closed with interrupted 4-0 sutures
Results
An adequate functional range of motion in opening was achieved in all the cases. In three cases there was deviation of mouth on opening to one side, absence of smooth closure and opening and some restriction in protrusive and laterotrusive movements. Seven cases were having no pain, reduction in joint noises and stable disc reduction out of 10 cases. Average mouth opening achieved was 36.2 mm. Stable disc reduction was achieved in seven cases and relapse of disc reduction was found in 3 out of 10 cases (Figs. 5a, b, 6a, b, 7a, b; Table 1).
Fig. 5.
MRI of a closed mouth non-reducing anteriorly displaced disc and b open mouth anteriorly displaced disc
Fig. 6.
MRI of a closed mouth reducing anteriorly displaced disc and b open mouth anteriorly displaced disc
Fig. 7.
MRI of a open mouth stable disc reduction and b closed mouth stable disc reduction
Discussion
Meniscal plication of the TMJ has a high success rate. Suturing the meniscus to the capsule reduces the risk of disc displacement, although it eliminates the lower joint space. This technique has been reported to have high success rate and to cause improvement in the range of motion post surgically which do not respond to conservative treatment. Absence of pain sounds and more than 35 mm of opening movement was achieved [3]. When the disc is considerably displaced or badly damaged, discectomy seems to give better results than suturing the disc in place [3, 4]. Discectomy without reposition of the disc followed by rehabilitation treatment reduces pain and results in an acceptable range of movement at opening in the long term, although crepitus is common, probably as a result of degeneration of the surfaces of the TMJ [3, 4]. Rehabilitation is an important complement to operation. With comprehensive rehabilitation, mobility of the TMJ, which is considerably impaired by the operation, improves significantly during the 6 months after operation. After operation, the risk of intra-articular bleeding should be balanced against the risk of fibrosis. Strict mandibular immobilisation for a week and elastic blockage of the jaws for 2 weeks has been recommended after meniscopexy, to avoid pain and suture dehiscence. If the disc has been removed, it has been recommended to wait for 2–3 days before starting gentle postoperative exercises [5]. The patients in the present study had limited mouth opening and soft diet was advised for 2 weeks. Thereafter active mouth opening exercises were carried out to achieve normal range of mouth opening. Although all the patients in this study had an internal derangement of the TMJ, the range of movement was considerably variable between patients. This could be a consequence of the variety of presentations in this group: for instance, some patients had a recent closed lock which restricted mouth opening, while others had chronic luxation of the disc, and therefore could open wider as a result of elongation of the ligaments of the TMJ. Open operation and rehabilitation significantly increased the range of movement, but also reduced its variability. Indeed, those patients who could open less than 36 mm before operation gained additional opening ability, while those who could open wider than 36 mm had a reduction. As the operation is intended to create an adhesion between the head of the condyle and the lower side of the disc, the final range of movement that could be obtained by rehabilitation was restricted to a maximum of around 40 mm, as the movement in the lower articular compartment was practically suppressed. This is in contrast with other surgical techniques, such as condylotomy, that do not often cause joint fibrosis, and so the range of jaw movement becomes greater [6]. The reduction in the TMJ noises after operation is explained by the attachment of the meniscus to the redundant capsule, which eliminates the mobility within the lower joint space, and to the reduction of the range of opening movement in patients with hypermobility of the TMJ. This is in contrast to arthrocentesis, which does not modify joint sounds in patients with reducing disc displacement, and increases joint sounds in patients with non-reducing disc displacement, probably because it improves disc mobility [7]. Our data suggest that meniscopexy can successfully treat patients with disc displacement and degenerative joint disease who do not respond to conservative treatment. Although the jaw movements remain somewhat restricted, it is possible to obtain satisfactory function of the TMJ and a significant reduction of pain and joint noises in the long term with a proper rehabilitation program.
Acknowledgments
Conflict of Interest None.
References
- 1.Murakami KI, Tsuboi Y, Bessho K, Yokoe Y, Nishida M, Iizuka T. Outcome of arthroscopic surgery to the temporomandibular joint correlates with stage of internal derangement: five-year follow-up study. Br J Oral Maxillofac Surg. 1998;36:30–34. doi: 10.1016/S0266-4356(98)90744-6. [DOI] [PubMed] [Google Scholar]
- 2.Carvajal WA, Laskin DM. Long-term evaluation of arthrocentesis for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2000;58:852–855. doi: 10.1053/joms.2000.8201. [DOI] [PubMed] [Google Scholar]
- 3.Dolwick MF. Disc preservation surgery for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2001;59:1047–1050. doi: 10.1053/joms.2001.26681. [DOI] [PubMed] [Google Scholar]
- 4.Takaku S, Sano T, Yoshida M. Long-term magnetic resonance imaging after temporomandibular joint discectomy without replacement. J Oral Maxillofac Surg. 2000;58:739–745. doi: 10.1053/joms.2000.7257. [DOI] [PubMed] [Google Scholar]
- 5.Eriksson L, Westesson PL. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up. J Oral Maxillofac Surg. 2001;59:750–758. doi: 10.1053/joms.2001.24288. [DOI] [PubMed] [Google Scholar]
- 6.Werther JR, Hall HD, Gibbs SJ. Disk position before and after modified condylotomy in 80 symptomatic temporomandibular joints. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:668–679. doi: 10.1016/S1079-2104(05)80298-7. [DOI] [PubMed] [Google Scholar]
- 7.Wilkes CH. Internal derangement of the temporomandibular joint pathological variations. Arch Otolaryngol Head Neck Surg. 1989;115:469–477. doi: 10.1001/archotol.1989.01860280067019. [DOI] [PubMed] [Google Scholar]