Abstract
Objective:
The aim is to show ultrasound (US) findings of additional malignant lesions of breast carcinoma visualized on targeted second-look US that were not identified by mammography or US prior to the time of diagnosis.
Materials and Methods:
A double-blind retrospective review of the US results from January 2008 through August 2010 of 228 patients with known breast cancer was conducted by two expert radiologists. The focus of the review was on the second-look US characteristics (following BI-RADS criteria) of 26 documented additional malignant lesions of the 76 with successful sonographic correlation from the 123 lesions detected by magnetic resonance imaging (MRI). All of them, before the MRI, had an initial mammography and a US with a histopathological biopsy of the primary lesion.
Results:
Approximately 60 to 70% of the findings were classified as BI-RADS 2 and BI-RADS 3, while assessing the final US category. The review of the second-look US showed the size of the second malignant additional lesion ranged from 3 to 22 mm, of which 90% were smaller than 10 mm and 66% were smaller than 7 mm.
Conclusions:
Most additional malignant lesions, nonpalpable carcinomas, which were previously not detected by mammography and US at first-look diagnosis, were detected by a targeted second-look US examination. These lesions were of category BI-RADS 2 and BI-RADS 3 and smaller than 7 mm.
Keywords: Breast cancer, breast magnetic resonance imaging, second-look ultrasound, staging breast cancer, targeted ultrasound
INTRODUCTION

Breast magnetic resonance imaging (MRI) offers the highest sensitivity of all breast modalities.[1–3] When MRI identifies lesions not previously detected on conventional imaging, additional investigations may be required to rule out malignancy.[4] Second-look ultrasound (US) is a technique that can be used to perform a re-evaluation of the breast after review of the MRI findings.
Few published articles, among the most recently reviewed literature, include findings from targeted US of malignant lesions. In the present study, the sonography correlation was found to be 62% (76 of 123), of which 66% (50 of 76) were found to be benign lesions and 34% (26 of 76) were found to be malignant. Of the malignant lesions, 70% were correlated sonographically. The conclusion based on these results is that most additional malignant lesions found during targeted US are small in size and nonspecific.
The purpose of this study was to analyze second-look US features of malignant lesions that were not previously detected based on the results of mammography or US conducted prior to the time of diagnosis.
MATERIALS AND METHODS
A retrospective study was conducted from January 2008 through August 2010. The MRI reports of 228 patients with known breast tumors were selected and reviewed. Included in the review were lesions that were visible by MRI, nonpalpable, and occult during mammography and first-look US. The correlation with second-look US was studied. Pathological reports were reviewed to select malignant lesions and retrospectively examined for US second-look features [Figure 1].
Figure 1.
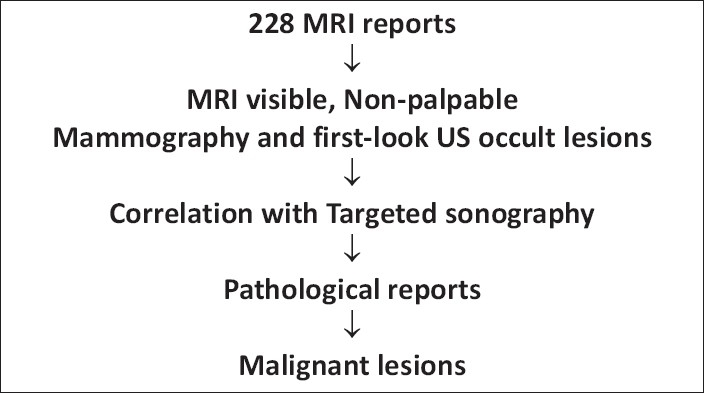
Flow chart of the study.
Additionally, benign lesions (all smaller than 5 mm) were confirmed using US-guided biopsy or upon review of pathological reports after surgery (of lesions located close to the principal cancer) and by follow-up MRI conducted after six months and most after one year. No evidence of malignancy was found during these follow-up studies.
MRI examinations were performed using a 1.5 T GE Signa Excite with an 8-channel breast coil with the following specifications:
T1-weighted (TR/TE 400/10ms) Fast Spin Echo (FSE) axial images
T2-weighted FSE axial images with fat suppression(TR/TE 4400/85ms), with a slice thickness of 4 mm (spacing 1 mm)
Acquisition time was 5 minutes for each sequence
For a contrast-enhanced dynamic series, a three-dimensional gradient echo-pulse (3D GRE) sequence (sagittal VIBRANT multiphase, flip angle = 10°), with a slice thickness of 2.5 mm was used; one precontrast and five postcontrast acquisitions were obtained sequentially, 1.20 minutes each, with a total acquisition time of 7.20 minutes.
Included was a postcontrast axial 3D GRE sequence, with a slice thickness of 2 mm. The total acquisition time was 4.5 minutes for this final sequence.
US examinations were performed using a 7 to 12-MHz linear-array transducer on a HD11 XE (Philips Healthcare) scanner.
A total of 123 new MRI lesions not previously detected were observed.
Included was a focus or foci near the index lesion or in a different quadrant with suspicious kinetics, such as a rapid uptake or washout and mass-like and non-mass-like enhancement with any type of kinetics. Multiple bilateral foci were excluded.
One investigator selected representative sonographic images for each pathologically proven malignant lesion. Subsequently, two radiologist, experts in breast imaging (experience ranging from 3-12 years, 7.5 years on average), conducted a double-blind retrospective analysis to describe the US features: Shape (round or oval, irregular), orientation (parallel, non-parallel), margin (circumscribed, noncircumscribed, angular, microlobulated, spiculated), echo pattern (hypoechoic, isoechoic), lesion boundary (abrupt interface, echogenic halo), and posterior acoustic features (no posterior acoustic shadowing, posterior acoustic shadowing).[5]
Each investigator was then asked to give a BI-RADS-ACR final assessment score for each lesion.[6] BI-RADS category 0, 1, and 6 were excluded, and Kappa statistics were calculated to assess the interobserver agreement proportion using the Epidat System 3.1, where a value of k = 1 indicates perfect agreement.[7,8]
RESULTS
A total of 123 new MRI lesions not previously detected 50 were observed. US correlation was established in 62% (76 of 123) of the lesions, with 66% of these (50 of 76) being benign and 34% (26 of 76) malignant [Figure 2]. A relatively high degree of interobserver agreement was obtained for BI-RADS lexicon, even for those lesions that tended to be nonspecific [Table 1].
Figure 2.
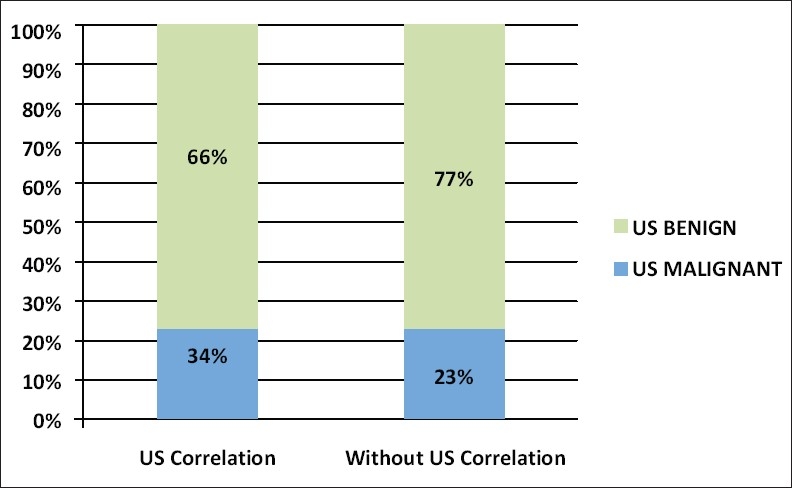
US correlation of 123 new MRI lesions not previously suspected.
Table 1.
Comparison of US features noted by two observers
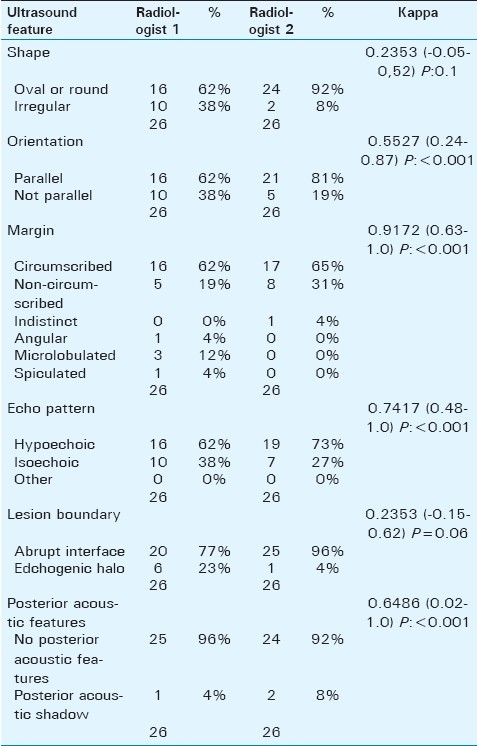
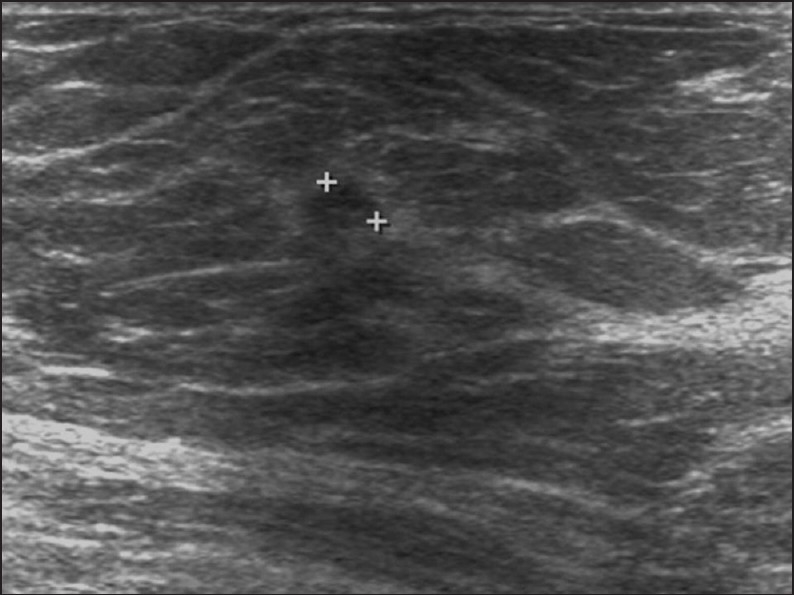
The descriptions of shape and lesion boundary were the most discordant between observers. During the retrospective analysis, 62% and 92% of the lesions were described as oval or round [Figure 3], and 77% and 96% of the lesions were described as abrupt interface [Figure 4]. Moderate agreement in describing orientation was obtained, with 62% and 85% of the lesions described as parallel [Figure 5]. High agreement was obtained in describing echogenicity with 62% and 73% of the lesions described as hypoechoic [Figure 6]. Near-perfect agreement was obtained in describing margin with 62% and 65% of the lesions described as well-circumscribed [Figure 7].
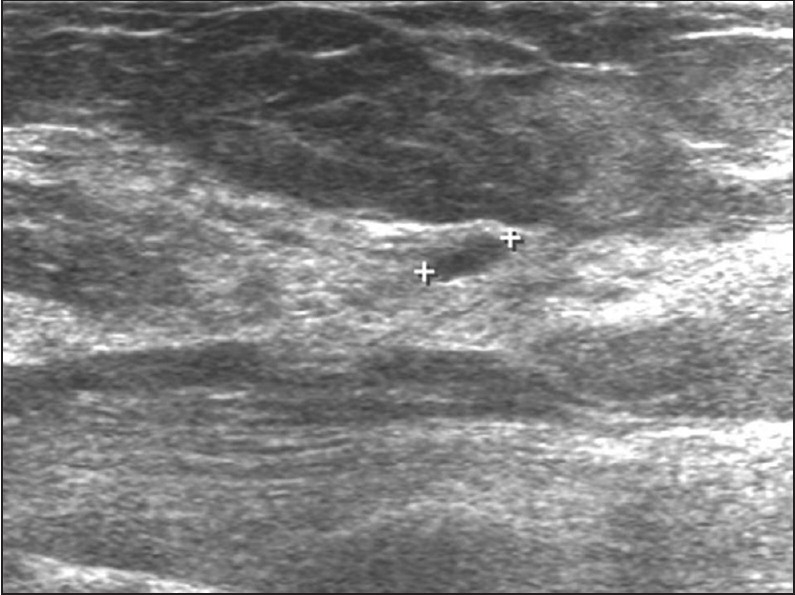
Figure 3.
Shape: Oval sonographic appearance of infiltrating ductal carcinoma.
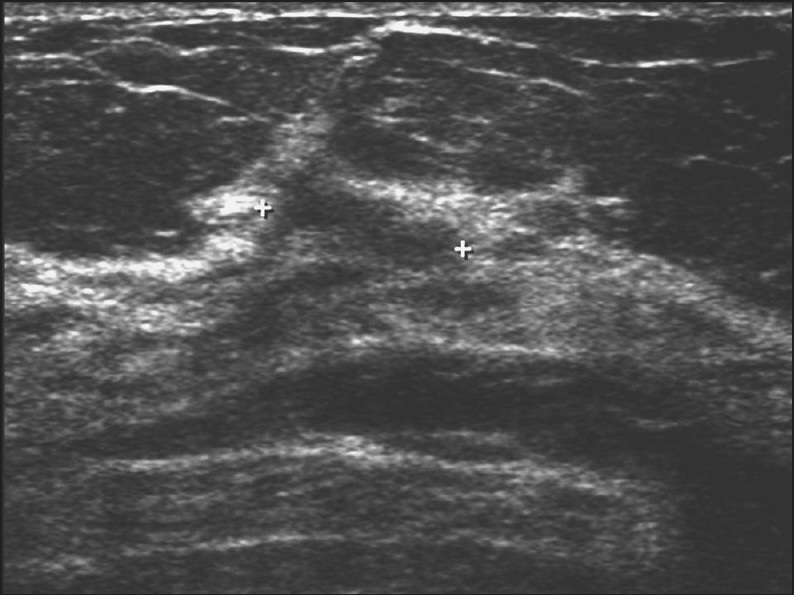
Figure 4.
Lesion boundary: This malignant lesion shows an abrupt interface.
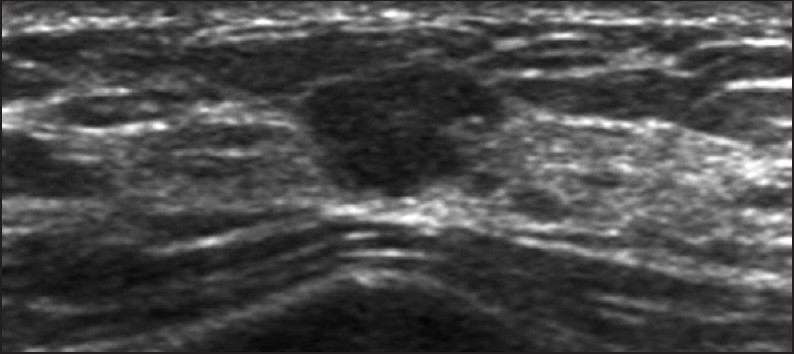
Figure 5.
Orientation: Lesion parallel to skin that mimics a fat lobule. Ductal carcinoma in situ and infiltrating ductal carcinoma were confirmed by core biopsy.
Figure 6.
Echogenicity: Hypoechoic lesion, infiltrating ductal carcinoma was obtained at histology.
Figure 7.
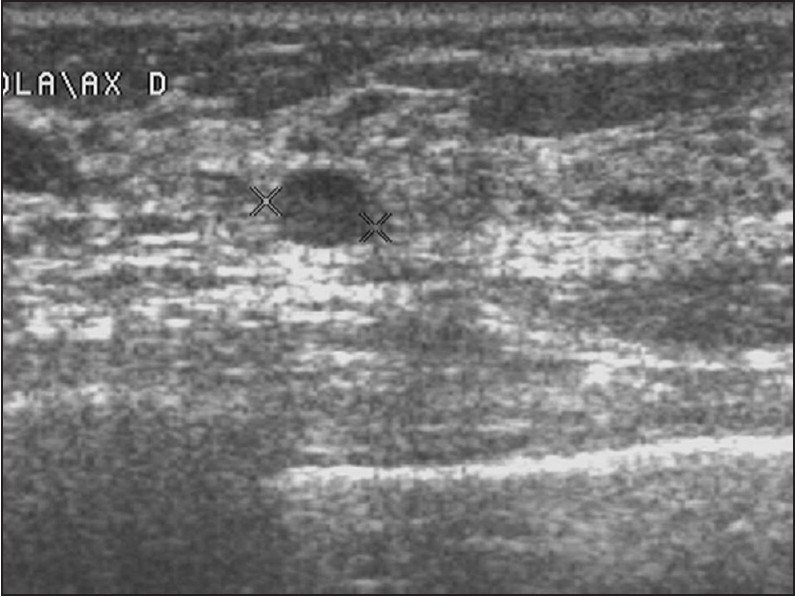
Margin: A round lesion with well-defined margin not suspected of malignancy. Core biopsy showed malignant histology.
Classic malignant finding were often not present, with only 4 to 8% showing posterior acoustic shadowing, 19 to 30% presenting an uncircumscribed margin, and 4 to 23% presenting an echogenic halo. Therefore, a considerable number of malignant lesions detected by MR-directed US examination were nonspecific and without malignant features.
In assessing the final category, including subclassification of category 4 into 4a, 4b, and 4c, the overall agreement was very high. Kappa statistics were calculated with a resulting value of k = 0.81 (IC95% = 0.615-0.999), where k = 1 corresponds to complete agreement. Among the 26 lesions that were subsequently found to be malignant, 61 to 69% had a benign (BI-RADS US 2) or probably benign (BI-RADS US 3) sonographic appearance and 31 to 38.4% were described as BI-RADS US 4a. In one case per observer, a lesion was categorized as BI-RADS 4c [Figure 8].
Figure 8.
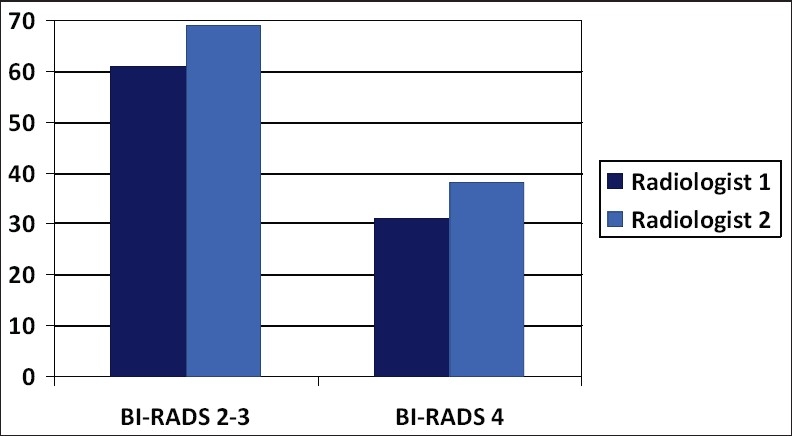
Distribution of final BI-RADS categories of the 26 lesions with US malignant characteristics described by Radiologist 1 and Radiologist 2
The sizes of the lesions were analyzed using US. The results showed a mean value of 6.78 mm (range, 3-22 mm). 90% of the lesions were smaller than 10 mm, and two-thirds of the lesions were smaller than 7 mm [Figure 9].
Figure 9.
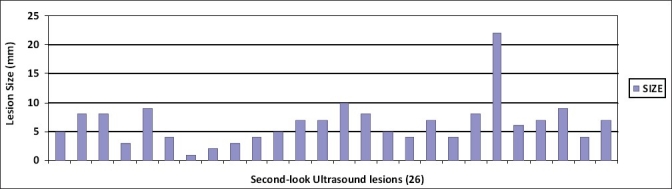
Distribution of second-look ultrasound lesion sizes in millimeters. 90% of lesions were smaller than 10 mm, and 66% of lesions were smaller than 7 mm.
Concerning MRI findings, sonographic correlation was established in 57.69% of the mass lesions, 26.92% of the foci, and 15.38% of the non-mass lesions. The MRI appearance of the lesions was mostly mass-like enhancement, and the dimensions were smaller than 10 mm [Figure 10].
Figure 10.
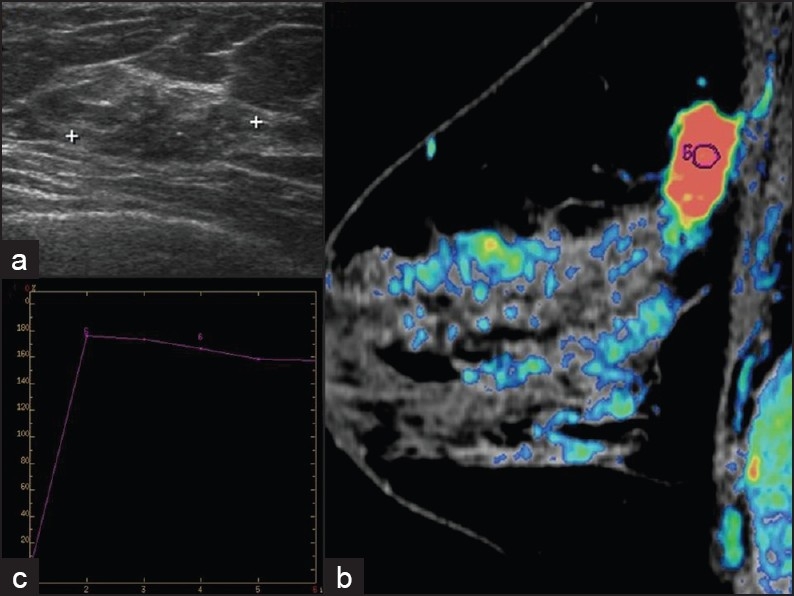
Sonographic-MRI correlation: (a) Oval, parallel to skin lesion at ultrasonographic examination. (b and c) MRI study shows a mass-like enhancement with suspicious type 3 curve.
Regarding histopathology findings, 44.4% (12 of 26) of the malignant lesions observed through second-look US were infiltrating ductal carcinoma, 29.6% (8 of 26) of the lesions were found to be carcinoma ductal in situ, and 11.11% (3 of 26) were found to be infiltrating carcinoma and carcinoma in situ.
DISCUSSION
Targeted US studies are an essential complement to breast MRI to investigate indeterminate and suspicious findings.[9–11] In the present study, sonographic correlation was established in more than 62% (76 of 123). The results are in agreement with other studies in which the rate of incidental MRI findings detected by second-look US was reported to vary between 23 and 89% according to patient selection.[10–16] It should be noted that physicians in the present study perform whole-breast US before MRI, which might have affected the results.
For malignant lesions, 70% were sonographically correlated, which coincides with the results of a recent study performed by Hiroyuki Abe et al[11] Of the lesions that were visible on second-look sonography, 34% (26 of 76) were histologically proven carcinomas, which was a higher percentage than malignant lesions without sonographic correlation, 23% (11 of 47). These results are in agreement with observations made by others where percentages varied between 9 and 27%. The present study comprised patients with previously identified breast cancer and did not include results from high-risk screening MRI examinations or results for patients with other than extent of disease. In addition, any enhancement other than the main tumor (including satellite lesions next to the cancer) was included, potentially inflating the number of new cancers observable sonographically and with occult US.
Only a limited number of published articles among the recently reviewed literature included a check for findings of targeted US of malignant lesions. The results of the present study are comparable with those of the recent study conducted by Hiroyuki Abe et al, in which lesions appeared nonspecific and subtle and, in most cases, without malignant features.[11]
In the present study, a large number of malignant lesions detected during MRI-directed US examination, between 60 and 70%, were initially classified as benign (BI-RADS 2) or probably benign (BI-RADS 3), and only a few presented some malignant characteristics. The most discordant classifications were made for shape description and lesion boundary, most probably due to the small lesion size. The median size of second-look US malignant lesions was 6.78 mm. Comparatively, this mean varied between 8 and 13 mm in other studies.[10,11] The detection rate using second-look US was higher for mass-like MRI lesions (57.69%), although this area deserves additional studies. The present study only included the review of MRI reports.
The main limitation of the present study was that MRI-Guided biopsy was not practised. In the absence of US correlation, the presence of a tumor cannot be ruled out. Various techniques are used where there is a high level of suspicion.[12] Of the 11 lesions that were found to be malignant and that were not detected using US (seven multifocal lesions and four multicentric lesions), wide lumpectomy was recommended in four cases. Wide lumpectomy and quadrantectomy were recommended in one case. Mastectomies were recommended in the remaining six cases, where the principal cancer was sufficiently massive to justify this approach or where multicentric cancer was previously demonstrated and mastectomy had been justified.
Other limitations in the present study include the following: US is an operator-dependent technique, and transverse and longitudinal US images were not available in all cases. Color flow features were not used, as this was a retrospective study and color flow imaging was available in only a few cases. The correlation between the MRI and US results were not exact in all cases, despite setting the following strict criteria: “After a correlate has been found and percutaneous biopsy performed, we recommend obtaining a T1-weighted noncontrast MRI sequence to verify metallic marker placement at the site of biopsy. This step ensures correct correlation between imaging modalities, provides immediate feedback for the radiologist, and, in case of error, allows the patient to be immediately redirected to repeat biopsy“ (Trop et al[4]) or radio-guided surgery, if considered necessary.
Clinical relevance/Application
Targeted US can be a reliable method for correlating MRI abnormalities in breast cancer patients and has been used to demonstrate that most additional malignant lesions are small and of category BI-RADS 2 and 3.
SUMMARY
In summary, most additional malignant lesions of multifocal, multicentric, and bilateral nonpalpable carcinomas that are detected using second-look US are nonspecific, present benign features in most cases, are small in size (under 7 mm in diameter), and go unnoticed during mammography and first-look US.
ACKNOWLEDGMENTS
Elisa Chilet Rosell, Research Assistant, Group of Public Health Research of the University of Alicante (Spain).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/34/82338
Presented as a scientific presentation at Spanish Society of Breast Imaging, 2009. None declared.
Presented as an oral scientific presentation at Radiological Society of North America, 2010.
REFERENCES
- 1.Orel SG, Schnall MD, Powell CM, Hochman MG, Solin LJ, Fowble BL, et al. Staging for suspected breast cancer: Effect of MR Imaging and MR-guided Biopsy. Radiology. 1995;196:115–22. doi: 10.1148/radiology.196.1.7784554. [DOI] [PubMed] [Google Scholar]
- 2.Malur S, Wurdinger S, Moritz A, Michels W, Shneider A. Comparision of written reports of mammography, sonography and magnetic resonance mammography preoperative evaluation of breast lesions, with special emphasis on magnetic resonance mammography. Breast Cancer Res. 2001;3:55–60. doi: 10.1186/bcr271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR Imaging in preoperative assessment of breast cancer. Radiology. 2004;233:830–49. doi: 10.1148/radiol.2333031484. [DOI] [PubMed] [Google Scholar]
- 4.Trop I, Labelle M, David J, Mayrand MH, Lalonde L. Second-look targeted studies after breast magnetic resonance imaging: Practical tips to improve lesion. Curr Probl Diagn Radiol. 2010;39:200–11. doi: 10.1067/j.cpradiol.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Mendelson EB, Baum JK, Berg WA, Merrit CR, Rubin E. Reston, VA: American College of Radiology; 2003. Breast Imaging Reporting and Data System BI. RADS: Ultrasound. [Google Scholar]
- 6.3rd ed. Reston, VA: American College of Radiology; 1998. American College of Radiology. Breast imaging reporting and data system (BI-RADS) [Google Scholar]
- 7.Fleis JL. 2nd ed. New York: John Wiley and Sons Inc; 1981. Statistical methods for rates and proportions. [Google Scholar]
- 8.Landis JR, Jock GG. The measurement of Observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 9.Demartini WB, Eby PR, Peacock S, Lehman CD. Utility of Targeted Sonography for Breast Lesions That Were Suspicious on MRI. AJR Am J Roentgenol. 2009;192:1128–34. doi: 10.2214/AJR.07.3987. [DOI] [PubMed] [Google Scholar]
- 10.Destounis S, Ariento A, Somerville PA, Seifert PJ, Murphy P, Morgan R, et al. Community-based practice experience of unsuspected breast magnetic resonance imaging abnormalities evaluated with second-look sonography. J Ultrasound Med. 2009;28:1337–46. doi: 10.7863/jum.2009.28.10.1337. [DOI] [PubMed] [Google Scholar]
- 11.Abe H, Schmidt RA, Shah RN, Shimauchi A, Kulkarni K, Sennett CA, et al. MR-Directed (“Second-Look”) Ultrasound Examination for Breast Lesions Detected Initially on MRI: MR and Sonographic Findings. AJR Am J Roentgenol. 2010;194:370–7. doi: 10.2214/AJR.09.2707. [DOI] [PubMed] [Google Scholar]
- 12.Carbognin G, Girardi V, Calciolari C, Brandalise A, Bonetti F, Russo A, et al. Utility of second-look ultrasound in the management of incidental enhancing lesions detected by breast MR imaging. Radiol Med. 2010;115:1234–45. doi: 10.1007/s11547-010-0561-9. [DOI] [PubMed] [Google Scholar]
- 13.DeMartini WB, Eby PR, Peacock S, Lehman CD. Utility of targeted sonography for breast lesions that were suspicious on MRI. AJR Am J Roentgenol. 2009;192:1128–34. doi: 10.2214/AJR.07.3987. [DOI] [PubMed] [Google Scholar]
- 14.LaTrenta LR, Menell JH, Morris EA, Abramson AF, Dershaw DD, Liberman L. Breast lesions detected with MR Imaging: Utility and hispopathologic importance of identification with US. Radiology. 2003;227:856–61. doi: 10.1148/radiol.2273012210. [DOI] [PubMed] [Google Scholar]
- 15.Beran L, Liang W, Nims T, Paquelet J, Sickle-Santanello B. Correlation of targeted Ultrasound with magnetic resonance Imaging abnormalities of the breast. Am J Surg. 2005;190:592–4. doi: 10.1016/j.amjsurg.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 16.Wiratkapun C, Duke D, Nordmann AS, Lertsithichai P, Narra V, Barton PT, et al. Indeterminate or suspicious breast lesions detected initially with MR Imaging: Value of MRI-directed breast Ultrasound. Acad Radiol. 2008;15:618–25. doi: 10.1016/j.acra.2007.10.016. [DOI] [PubMed] [Google Scholar]


