Abstract
Background and Objectives
Intubating a patient with temporomandibular joint ankylosis is always a challenge particularly when fibreoptic laryngoscope is not available. Awake blind nasotracheal intubation requires sufficient patient co operation and comfort. Presently available short-acting analgesics and amnesics are excellent choices for this exercise.
Study Design
This prospective randomized double blind study was designed to determine an appropriate dosage of fentanyl for awake blind nasotracheal intubation. We compared two different dosage of fentanyl. Eighty patients were randomly assigned to receive midazolam 0.05 mg/kg and fentanyl 2μg/kg in bolus (group I), or midazolam 0.05 mg/kg, fentanyl 3μg/kg in bolus (group II).
Results
Both dosage regimen ensured patient comfort and sedation. Patients in group II were more calm and sedated as compared to group I. Hemodynamics was also more stable in group II.
Conclusion
For awake blind nasotracheal intubation, we therefore recommend midazolam 0.05mg/kg plus fentanyl 3μg/kg in bolus.
Keywords: Awake intubation, Temporomandibular joint ankylosis, Conscious sedation
Introduction
Temporomandibular joint interpositional gap arthroplasty is done under general anaesthesia with nasotracheal intubation. General anaesthesia and nasotracheal intubation are the main problems of surgery in temporomandibular joint ankylosis because it is difficult to intubate the patient of temporomandibular joint ankylosis as the laryngeal inlet is not visible [1, 2]. Intubating a patient with temporomandibular joint (TMJ) ankylosis has always been a challenge to the anaesthesiologist. A number of techniques are available which include blind nasal intubation, retrograde intubation using a guide wire, intubating with the help of a fibreoptic laryngoscope and tracheostomy [3]. If services of flexible fiber optic bronchoscope are not available, blind nasotracheal intubation is performed. Awake blind nasotracheal intubation has been widely described in the literature [4]. Apart from temporomandibular joint ankylosis awake blind nasotracheal intubation is indicated in all those situations where it is difficult to perform laryngoscopy. Instrumentation of the airway is uncomfortable and distressing to an awake patient [5]. An informed and reassured patient adds to the success of awake intubation. Modern short-acting analgesics and amnesics are excellent for this purpose and have improved the use of this technique by providing conscious sedation and maintaining spontaneous ventilation [5, 6].
Fentanyl is a short acting opioid, undergoes hepatic metabolism and provides immediate analgesia for 30–60 min after a single intravenous dose [7, 8].
Midazolam is an ultra short-acting benzodiazepine derivative. It has potent anxiolytic, amnesic [9], hypnotic, anticonvulsant, skeletal muscle relaxant, and sedative properties [10]. Midazolam is unique amongst benzodiazepines in that it is water soluble rather than fat soluble like most other benzodiazepines. It is considered an ultra short-acting benzodiazepine, with an elimination half-life of about 2 h. It is used in some countries for the short term treatment of insomnia and in many countries as a premedication before anaesthesia [11, 12].
This study was designed to determine a proper fentanyl dosage required for awake blind nasotracheal intubation providing adequate analgesia and maintaining spontaneous respiration in patients undergoing temporomandibular joint interpositional gap arthroplasty. The effects of two different dosage of fentanyl on patient sedation and hemodynamic stability were compared.
Method
After getting a written informed consent from all subjects 80 cases (Table 1) of ASA physical status grade I or II, admitted for temporomandibular joint ankylosis surgery, were enrolled in the study, between January 2006 and April 2010. Obstinate patients, patients with any cardiac and/or respiratory disease, reactive airway disease, hepatic or renal disorders, a history of drug abuse and patients allergic to local anaesthetic agents were excluded from the study. Patients were also excluded if they had associated micrognathism or hypognathism.
Table 1.
Patients characteristics
| Group I (n = 40) | Group II (n = 40) | ‘t’ value | ‘P’ value | |
|---|---|---|---|---|
| Mean age ± SD (Years) | 25.975 ± 6.023 | 26.700 ± 4.304 | 0.619 | 0.537 |
| Mean weight ± SD (Years) | 54 ± 6.9 | 55 ± 8.0 | 0.737 | 0.463 |
| Height (cm) | 153 ± 4.1 | 154 ± 4.3 | 1.190 | 0.2369 |
The study design was double blind, and prospective and randomized. Subjects were informed about the procedure. Subjects were selected using simple randomized sampling and allocated to either of the two groups using sealed opaque envelopes, by the numbers randomly generated by computer table. An independent anesthesiologist who did not participate in the study or data collection made the group assignments.
All subjects were fasted for 10 h and no sedative premedication was given. Preparations were made for emergency access to the airway. Intravenous line established and lactated ringer infusion started. Standard monitoring with non-invasive blood pressure (NIBP), electrocardiography and pulse oximetry was done. All subjects received injection glycopyrrolate 0.004 mg/kg body wt and injection ondansetron 0.08 mg/kg body wt intravenously before starting the study. Nasal mucosa of both nostrils of all patients was prepared with a vasoconstrictor (xylometazoline) and 4% topical lignocaine. Topical anaesthesia of pharyngeal structures was achieved with 10% lignocaine spray.
Patients were randomly allocated to one of the two groups using a computer generated table of random numbers. Group I patients received injection midazolam 0.05 mg/kg and injection fentanyl 2 μg/kg intravenously in slow bolus. Group II patient received injection midazolam 0.05 mg/kg and injection fentanyl 3 μg/kg intravenously in slow bolus. Airway manipulation was started 3 min after the injection, by that time all patients were calm, tranquilized and able to respond to simple commands such as “open eyes”.
A well lubricated (with lignocaine jelly 2%) nasopharyngeal airway was then gently introduced to test the patency of the nasal passage and provide additional topical anesthesia to the hypopharynx, epiglottis and larynx.
Nasopharyngeal airway was then replaced by the nasotracheal tube. The neck was extended and the position of the tube assessed in relation to the trachea by looking for a visible bulge in anterior neck or by listening the breath sounds. The nasotracheal tube was rotated accordingly to the right or left in order to obtain a more favorable alignment between the trachea and the tube. To improve the anterior-posterior relationship of the tube to the trachea the head was flexed. Patient was then asked to take rapid deep breath so that intubation is accomplished during inhalation or exhalation. During the entire period of the tube manipulation, breath sounds are observed and when the highest intensity of breath sounds is heard, the nasotracheal tube is advanced rapidly until it reaches the trachea. Successful intubation is frequently followed by coughing, but the only reliable indication is the visual observation of gas exchange through the reservoir bag and verification of pulmonary breath sounds with a stethoscope.
The position of the tube was confirmed with mainstream capnography and the cuff inflated. Propofol 2 mg/kg and rocuronium 0.9 mg/kg intravenously were administered to induce general anesthesia and establish mechanical ventilation.
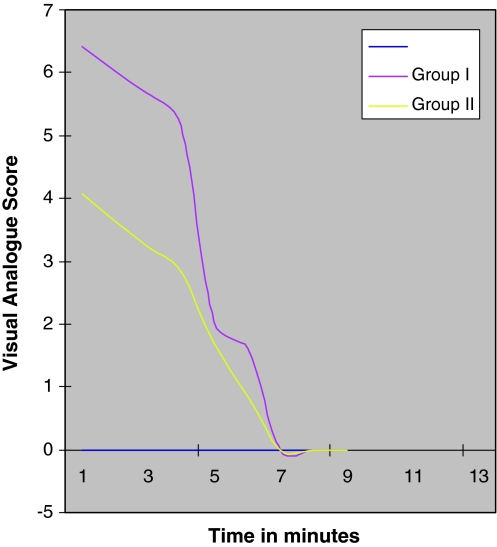
Modified Ramsay scale [13] was used for rating sedation by measuring six component categories, and the total score was assigned (Table 2). Modified Ramsay scale was determined before injecting the study medication and every 2 min during airway manipulation. On the next postoperative day a blinded anaesthesiologist evaluated the patients about the level of discomfort during intubation. The visual analog scale (VAS) score from 0 to 10 described “insignificant discomfort” to “severe discomfort” (Fig. 1). With 80% power (20% beta error) and 95% confidence level (5% alpha error), the sample size calculated was 33, in each group. For the purpose of our study, we have taken 40 subjects in each group. Sample size was calculated using power and sample size calculator by department of Biostatics, Vanderbilt University, USA. Statistical calculations were made by analysis of variance (ANOVA) with Bonferroni correction and Fischer’s exact test. The SPSS 11 software was used for statistical analysis.
Table 2.
Modified Ramsay scale for rating sedation
| Indication | Score |
|---|---|
| Anxious, agitated, restless | 1 |
| Awake, cooperative, oriented, tranquil | 2 |
| Semiasleep but responds to commands | 3 |
| Asleep but responds briskly to glabellar tap or loud auditory stimulus | 4 |
| Asleep with sluggish or decreased response to glabellar tap or loud auditory stimulus | 5 |
| No response can be elicited | 6 |
Fig. 1.
Visual analogue score
Results
Awake blind nasotracheal intubation could be achieved in 72 of 80 patients. Severely deviated nasal septum did not permit transnasal passage of the tube in four patients. In two patients we had to abandon the process because of epistaxis. Two patients were intubated using flexible fiber optic bronchoscope.
Both study groups were similar with respect to demographic characteristics (Table 1). Sedation was adequate in all patients, however patients in group II were more calm and sedated with a mean Ramsay score of 1.2250 ± 0.439 in contrast to the patients in group I with a mean Ramsay score of 1.050 ± 0.221 (Table 3). Different doses of fentanyl were responsible for differences in mean Ramsay scores between the two groups. No patient complained pain in either group. Sixteen patients (40%) in group I had no recall (VAS 0) 24 h after intubation; trivial memories (VAS 2) were expressed by fourteen patients (35%). Clear but not horrible memories (VAS 3–5) were expressed by the remaining four patients (10%). Six patients could not be intubated with this technique in group I. Flexible fiber optic bronchoscope too failed to intubate these patients and tracheostomy had to be performed to administer anaesthesia. Twenty patients (50%) in group II had no recall (VAS 0) and eighteen (45%) patients described only slight memories (VAS 1–2). Two patients in group II were intubated with flexible fiber optic bronchoscope.
Table 3.
Mean modified Ramsay score
| Group I | Group II | ‘t’ value | ‘P’ value | |
|---|---|---|---|---|
| Ramsay score (Mean ± SD) | 1.050 ± 0.221 | 1.2250 ± 0.439 | 2.576 | 0.012 |
Heart rate and mean arterial pressure were better maintained in group II after 2, 5 and 10 min of starting the procedure and this was statistically significant (Tables 4, 5).
Table 4.
Hemodynamics
| Heart rate per min. | Before starting the procedure | 5 min after starting the procedure | 10 min after starting the procedure | 15 min after starting the procedure | ||||
|---|---|---|---|---|---|---|---|---|
| Group I | Group II | Group I | Group II | Group I | Group II | Group I | Group II | |
| Mean ± SD | 98.050 ± 6.862 | 99.875 ± 7.097 | 111.000 ± 0.7673 | 102.975 ± 7.843 | 109.250 ± 8.186 | 99.950 ± 6.891 | 103.200 ± 7.881 | 99.950 ± 6.891 |
| Change in Mean ± SD | – | – | 12.95 ± 4.57 | 3.10 ± 1.92 | 11.20 ± 5.67 | 0.08 ± 1.47 | 5.15 ± 4.37 | 0.04 ± 0.74 |
| ‘t’ value | – | – | 17.907 | 10.28 | 12.490 | 0.322 | 7.462 | 0.322 |
| ‘P’ value | – | – | 0.001 | 0.01 | 0.001 | 0.749 | 0.001 | 0.749 |
Table 5.
Hemodynamics
| Mean arterial pressure | Before starting the procedure | 5 min after starting the procedure | 10 min after starting the procedure | 15 min after starting the procedure | ||||
|---|---|---|---|---|---|---|---|---|
| Group I | Group II | Group I | Group II | Group I | Group II | Group I | Group II | |
| Mean ± SD | 84.800 ± 4.020 | 84.350 ± 2.896 | 89.550 ± 3.637 | 84.625 ± 2.733 | 87.700 ± 3.695 | 84.850 ± 2.931 | 89.550 ± 3.637 | 84.625 ± 2.733 |
| Change in Mean ± SD | – | – | 4.75 ± 2.99 | 0.28 ± 1.11 | 2.90 ± 2.31 | 0.50 ± 1.62 | 4.75 ± 2.99 | 0.28 ± 1.11 |
| ‘t’ value | – | – | 10.035 | 1.568 | 7.950 | 1.955 | 10.035 | 1.568 |
| ‘P’ value | – | – | 0.001 | 0.125 | 0.001 | 0.058 | 0.001 | 0.125 |
Oxygenation was quite sufficient in all patients throughout the study (SpO2 > 90%).
Discussion
Numerous combinations of analgesics and amnesics have been used for awake blind nasotracheal intubation [14]. Fentanyl and alfentanil with diazepam, as well as fentanyl with propofol [15–17] have been studied for the purpose. Fentanyl a short acting opioid analgesic is an admirable option for the brief hurting airway stimulus during blind awake nasotracheal intubation [18, 19].
Fentanyl was recently compared with remifentanil supplemented with midazolam for awake fiberoptic intubation and remifentanyl was found to improve intubating conditions and quality of fiberoptic intubation [20]. Respiratory impairment did not result and sufficient spontaneous ventilation was maintained in patients of both study groups. The use of fentanyl alone fails to provide sufficient sedation [21] that is why midazolam was added in our study to improve the quality of sedation in patients. Fentanyl, a short acting opioid provides instant analgesia devoid of any significant side effect. Midazolam provides good anxiolysis, amnesia, hypnosis and sedation without any cardiorespiratory depression [7–10].
The same dose of midazolam was used in both study groups. Injection glycopyrrolate 0.2 mg μl and injection ondansetron 0.08 mg/kg body wt IV was administered to our patients to reduce secretions and to avoid fentanyl induced nausea, vomiting, bradycardia and hypotension during awake blind nasotracheal intubation [22–24].
The aim of our study was to determine an appropriate fentanyl dose required for awake blind nasotracheal intubation. The adequate dose should provide patient comfort and sedation. Furthermore, it should make sure of, adequate suppression of airway reflex, preserving sufficient spontaneous ventilation and hemodynamic stability. Our data suggest that patients receiving large dose fentanyl were sedated more profoundly and than patients receiving small dose fentanyl. Hemodynamics during airway instrumentation was more stable in patients receiving large dose fentanyl.
Conclusion
We found that the fentanyl 3 μg/kg supplemented with midazolam 0.05 mg/kg provides better patient comfort and sedation in conjunction with adequate suppression of airway reflex, preserving sufficient spontaneous ventilation and retaining hemodynamic stability during awake blind nasotracheal intubation.
References
- 1.Colmenero C, Esteban R, Albarino AR, Colmenero B. Sleep apnoea syndrome associated with maxillofacialabnormalities. J Laryngol Otol. 1991;105(2):94–100. doi: 10.1017/S002221510011504X. [DOI] [PubMed] [Google Scholar]
- 2.Dhasmana S, Singh V, Pal US, Mohammad S. Temporomandibular joint interpositional gap arthroplasty under intravenous (I.V) conscious sedation. J Maxillofac Oral Surg. 2009;8(4):372–374. doi: 10.1007/s12663-009-0089-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vithal K. Dhulkhed retrograde intubation in temporomandibular joint ankylosis—a double guide wire technique. Indian J Anaesth. 2008;52(1):90–92. [Google Scholar]
- 4.Francis A, Neidorf C. Blind awake nasal intubation. Anaesth Prog. 1977;24:15–17. [PMC free article] [PubMed] [Google Scholar]
- 5.Batra YK, Mathew PJ. Airway management with endotracheal intubation including awake intubation and blind intubation. Indian J Anaesth. 2005;49(4):263–268. [Google Scholar]
- 6.Anette-Marie M, Christopher G, Andrea H, Dorothea A, Christian K, Zimpfer M, Udo M. Illievich awake nasotracheal fiberoptic intubation: patient comfort, intubating conditions, and hemodynamic stability during conscious sedation with remifentanil. Anesth Analg. 2003;97:904–908. doi: 10.1213/01.ANE.0000074089.39416.F1. [DOI] [PubMed] [Google Scholar]
- 7.Chaturvedi S, Chaturvedi A. Postoperative pain and its management. Ind J Crit Care Med. 2007;11(4):204–211. doi: 10.4103/0972-5229.37716. [DOI] [Google Scholar]
- 8.Stoelting RK, Hillier SC (eds) (2006) Opioid agonists and antagonists. In: Pharmacology and physiology in anesthetic practice, 4 th edn. Lippincott Williams and Wilkins, Philadelphia
- 9.“Benzodiazepine Names”. non-benzodiazepines.org.uk. http://www.non-benzodiazepines.org.uk/benzodiazepine-names.html. Accessed 29 Dec 2008
- 10.Mandrioli R, Mercolini L, Raggi MA (2008). Benzodiazepine metabolism: an analytical perspective. Curr Drug Metab 9(8):827–844. doi:10.2174/138920008786049258. PMID 18855614. http://www.benthamdirect.org/pages/content.php?CDM/2008/00000009/00000008/0009F.SGM [DOI] [PubMed]
- 11.Kanto JH (1985) Midazolam: the first water-soluble benzodiazepine. Pharmacology, pharmacokinetics and efficacy in insomnia and anesthesia. Pharmacotherapy (3):138–55. PMID 3161005 [DOI] [PubMed]
- 12.Kumar P. Sedation and pain relief. Indian J Anaesth. 2003;47(5):396–401. [Google Scholar]
- 13.Ramsay MA, Savege TM, Simpson BR, et al. Controlled sedation ith alphaxalone-alphadolone. Br Med J. 1974;920:656–659. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duncan HP, Zurich NJ, et al. Should we reconsider awake neonatal intubation? A review of the evidence and treatment strategies. Paediatr Anesth. 2001;11(2):135–145. doi: 10.1046/j.1460-9592.2001.00535.x. [DOI] [PubMed] [Google Scholar]
- 15.Sutherland AD, Williams RT. Cardiovascular responses and lidocaine absorption in fiberoptic-assisted awake intubation. Anesth Analg. 1986;65:389–391. doi: 10.1213/00000539-198604000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Randell T, Valli H, Lindgren L. Effects of alfentanil on the responses to awake fiberoptic nasotracheal intubation. Acta Anaesthesiol Scand. 1990;34:59–62. doi: 10.1111/j.1399-6576.1990.tb03042.x. [DOI] [PubMed] [Google Scholar]
- 17.Andel H, Klune G, Andel D, et al. Propofol without muscle relaxants for conventional or fiberoptic nasotracheal intubation: a dose-finding study. Anesth Analg. 2000;91:458–461. doi: 10.1097/00000539-200008000-00043. [DOI] [PubMed] [Google Scholar]
- 18.Simpson RK, Jr, Edmonson EA, Constant CF, Collier C. Transdermal fentanyl as treatment for chronic low back pain. J Pain Symptom Manag. 1997;14:218–224. doi: 10.1016/S0885-3924(97)00183-8. [DOI] [PubMed] [Google Scholar]
- 19.Carli D, Correa NS, Silva TC, Maradei EM. Blind nasotracheal intubation in awaken patient scheduled for hemimandibulectomy. Rev Bras Anestesiol. 2008;58(1):55–62. doi: 10.1590/S0034-70942008000100008. [DOI] [PubMed] [Google Scholar]
- 20.Puchner W, Egger P, Puhringer F, et al. Evaluation of remifentanil as single drug for awake fiberoptic intubation. Acta Anaesthesiol Scand. 2002;46:350–354. doi: 10.1034/j.1399-6576.2002.460403.x. [DOI] [PubMed] [Google Scholar]
- 21.Tosun Z, Esmaoglu A, Coruh A. Propofol–ketamine vs propofol–fentanyl combinations for deep sedation and analgesia in pediatric patients undergoing burn dressing. Paediatr Anesth. 2008;18:43–47. doi: 10.1111/j.1460-9592.2007.02380.x. [DOI] [PubMed] [Google Scholar]
- 22.Smith I, Walley G, Bridgman S. Omitting fentanyl reduces nausea and vomiting, without increasing pain, after sevoflurane for day surgery. Eur J Anaesthesiol. 2008;25(10):790–799. doi: 10.1017/S026502150800464X. [DOI] [PubMed] [Google Scholar]
- 23.Bowdle TA. Adverse effects of opioid agonists and agonist-antagonists in anaesthesia. Drug Saf. 1998;19(3):173–189. doi: 10.2165/00002018-199819030-00002. [DOI] [PubMed] [Google Scholar]
- 24.Boynes SG, Moore PA, Lewis CL, Zovko J, Close JM. Complications associated with anesthesia administration for dental treatment in a special needs clinic. Spec Care Dentist. 2010;30(1):3–7. doi: 10.1111/j.1754-4505.2009.00114.x. [DOI] [PubMed] [Google Scholar]