Abstract
With the increasingly wide spread application of microvascular free tissue transfer technique for oral cavity reconstruction, the routine need for variety of local and regional flap has decreased. However, a number of such flaps remains quite useful and should be included in modern armamentarium of reconstructive surgeon. Nasolabial flap is versatile, simple, easy to harvest local flap that can cover a variety of defect in face. We present the success and utility of bilateral pedicled flap for reconstruction of mandibular anterior alveolus after the wide excision of squamous cell carcinoma of mandibular anterior alveolus. And the restoration of esthetics and functional dental health with the artificial prosthesis. Patient had been followed for two years and six month with no signs of recurrence as yet.
Keywords: Squamous cell carcinoma, Mandibular anterior alveolus, Bilateral nasolabial pedicled flap
Introduction
The subcutaneous pedicled nasolabial flap appears to have been originally described in works of Susruta in 600 bc [1]. For centuries thereafter it was used primarily in external nasal reconstruction. Thiersch [2] was the first to use transbuccal use of this flap for the closure of an oral cavity defect. Esser [3] reported the use of cutaneous nasolabial flap transferred in two stages to increase its reliability.
With the advent of musculocutaneous flaps and microsurgical transfer, intraoral or nasal reconstruction has entered an area of sophistication where by defects of any size can be repaired, however sometimes these technique are inappropriate because either the defect is too small or the patient’s age and medical status do not permit a lengthy anesthetic and surgical procedure. The nasolabial flap represents the available local tissue that, in right circumstances, often circumvents these problems for repair of small or moderate sized local intra or extra-oral defect [4].
The nasolabial flaps are very useful and versatile local flap with robust vascularity that can be readily elevated without any delay.
We present a case diagnosed with the early invasive squamous cell carcinoma of mandibular anterior alveolus without nodal metastasis. Patient was surgically treated with the wide excision of lesion along with marginal mandibulectomy. The resultant surgical defect closed using the bilateral pedicled nasolabial flap. Rehabilitation of the patient was done with complete dentures. Patient was followed up for a period of 2 years with no signs of recurrence.
Case Report
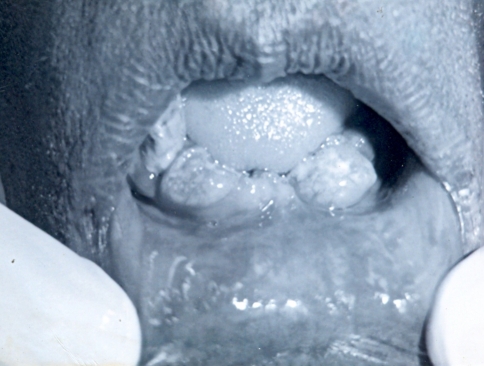
A 75 year old patient reported to the department of Oral and Maxillofacial Surgery, V. S. Dental College and Hospital, Bangalore with a complaint of growth in the anterior region of the lower jaw since 3 months. Examination revealed a solitary, well defined, irregularly shaped growth in the lower anterior alveolus extending from the right canine to left canine region. The surface of the growth was papillary with erythematous changes, borders-well defined and clearly demarcated from the surrounding structures with slightly everted margins (Fig. 1). No lymph nodes were palpable clinically. It was T3NoMo lesion. The incisional biopsy report read the lesion to be a well differentiated squamous cell carcinoma. The treatment plan was divided into three phases,
Fig. 1.
Stage 1: pre-operative lesion
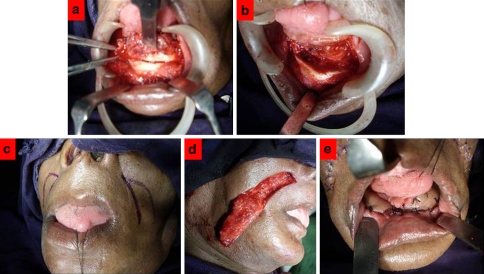
Stage 1: Surgical procedure: Wide excision of lesion with anterior marginal mandibulectomy from lower canine to canine tooth, the defect measured around 4 × 2 cm and reconstruction of defect was done with the bilateral pedicled nasolabial flaps (Fig. 2).
Fig. 2.
Stage 2: surgical technique. a Mandibular anterior osteotomy cuts. b Resultant surgical defect. c Inferiorly based nasolabial flap marked. d Flap elevated from and tunneled through buccal mucosa. e Bilateral pedicled flap sutured to the surgical defect
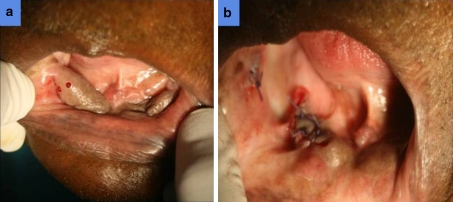
Stage 2: Detachment of flap: Three weeks post-operatively the flaps were detached. And subsequently patient referred for prophylactic radiotherapy (Fig. 3).
Fig. 3.
Stage 3: detachment of bilateral flaps. After three week nasolabial flap in position with bleeding points shows good vascularity
Stage 3: Oral cavity rehabilitation: Six month post-operatively artificial prosthesis was given (Fig. 4).
Fig. 4.
Stage 4: rehabilitation of oral cavity with prosthesis. a Three months post operatively surgical site with the color and texture of flaps is close to normal mucosa. b Artificial prosthesis-complete denture. c Patient profile with the restoration of dental stomatognathic unit for better esthetics
Surgical Technique
After the excision of the lesion and marginal mandibulectomy from canine to canine region, size of the defect was measured and inferiorly based nasolabial flaps were outlined on each cheek and raised with sufficient enough subcutaneous tissue to ensure good blood supply but thin enough not to be too bulky and to remain superficial to the facial muscles. The base of the flap was broad and maintained just above the corner of the mouth. At the level of the lateral commissure of the mouth, a transbuccal tunnel was created.
The buccal mucosa at this point was incised. The width of this entry into the oral cavity was as wide as the flap width to prevent any constriction in the blood supply to the flap. The flap thus tunneled into the oral cavity was used to reconstruct the defect following mandibulectomy. The tip of each flap was sutured edge to edge and the corresponding borders were sutured to the lingual and the labial mucosa using 3-0 Vicryl. The donor site defect was closed primarily, because of the laxity of the skin. The subcutaneous layer was closed using 3-0 vicryl and the skin was closed using 5-0 prolene. Three weeks later the pedicle was dissected and the defect in the buccal mucosa was sutured using 3-0 vicryl.
Patient was referred to radiotherapy after 3 weeks. Six months postoperative follow up showed satisfactory healing. The complete rehabilitation of oral cavity is achieved with complete denture and patient followed for two years with no signs of recurrence as yet.
Discussion
Even relatively small defects of the oral cavity often require reconstruction to avoid anatomical distortion and subsequent limitation of function. The versatility and the usefulness of the nasolabial flaps are well recognized in the reconstruction of the nose.
The nasolabial sulcus is formed by the junction of the upper lip and lower nose with the cheek. It is created by the insertion of the several of the mimetic facial muscle into skin of the lip at this juncture. The force of muscle contraction and gravity with time creates an outpouching or mould of skin lateral to this crease in medial area of cheek, which is called the nasolabial cheek fold.
The vascular anatomy of the nasolabial flaps is based on the angular artery (a branch from the anterior facial artery), the infra-orbital artery, the transverse facial artery and the infra-trochlear artery. Because of the rich vascular supplies and the free anastomosis between the terminal branches of the supplying vessels of the flap; superior, inferior, medial, and lateral flaps can be raised. Due to rich sub dermal plexus the flap can be used either a random flap based or axial pattern flap.
Superiorly based nasolabial flaps can be used for the reconstruction of nasal defects, lower eyelid, and the cheek except for the most cephalad part of nose. If flap is carried too far superiorly, it can result in a medial lower eyelid ectropion when the donor site is closed. The potential disadvantage of the superiorly based nasolabial flap includes the trapdoor or pincushion effect caused by scar contracture, blunting of the nasolabial sulcus, and asymmetry of the nasolabial sulcus.
Inferiorly based flaps are considered useful in reconstruction of the lip, oral commissure and the anterior oral cavity. Bilateral subcutaneous pedicled inferiorly based flaps were raised to reconstruct the surgical defect in our case. The transbuccal tunnel should be made next according to the site of defect in oral cavity. The tunnel should be large enough to easily accommodate 1 or 2 fingers (1.5–2.0 cm). The flap transferred in tension free manner and inset with series of interrupted 3-0 absorbable sutures. The closure of donor defect should be done to evert the skin along the nasofacial portion of the incision to achieve a flat scar once healing is completed. However, along the nasolabial fold, a slightly depressed scar (hence, minimal eversion at time of closure) results in more natural appearance.
In our case we employed the two stage technique for flap transfer, where a second stage was required, the division and onset of flap is performed three weeks after the initial procedure. During flap division, it is important to remove the entire transbuccal component of the flap rather than to simply divide it flushes it with the cheek tissue on the oral cavity side. Failure to do so will invariably result in the presence of the visible long term fullness at the level of the lateral commissure.
The advantages of using the nasolabial flap; in addition to the robust vascularity; includes the simplicity and the time saving that the procedure provides. The proximity of the recipient defect, best colour match and the satisfactory contour created from the relatively hairless areas utilized from the nasolabial fold are the major advantage of the technique. The higher vascularity of the flap and the less donor site morbidity compared with the median forehead flap makes it a superior alternative in facial reconstruction. However, the limitation of the flap use includes; the limited flap size, width and the limited arc of rotation. This makes it only suitable for small or medial sized defect [5].
Frederick [6] successfully showed two-stage reconstruction of the alar lobule with a subunit nasolabial flap can produce near-normal results. Because the entire alar subunit is resurfaced, border scars lay hidden within the joins that outline the unit. The alar skin is of uniform quality and uncrossed by scars.
The nasolabial flap is generally outside of the radiation therapy portals used in combined modality therapy for squamous cell carcinoma. Thus, its vascularity is generally not compromised in this patient population. The administration of planned post operative external beam radiation therapy may, in fact, be beneficial, especially in males, because it limits the subsequent hair growth along the flap and, thus, obviates the need for epilation.
To conclude nasolabial flap is versatile, simple, easy to harvest local flap that can cover a variety of defect in face. The flap also gives better esthetics as resultant scar is hidden in nasolabial flap and obviate the need for second donor site.
References
- 1.Ducic Y, Burye M. Nasolabial flap reconstruction of oral cavity defects: a case report of 18 cases. J Oral Maxillofac Surg. 2000;58:1104–1108. doi: 10.1053/joms.2000.9564. [DOI] [PubMed] [Google Scholar]
- 2.Thiersch C. Verschluss eines loches im harten gaumen durch dic weichtheile der wange. Arch Heilkunde. 1868;9:159. [Google Scholar]
- 3.Esser JSF. Deckung von gaumendefektan mittels gestielter naso labial haultlappen. Deutsch Zeitschrift fur Chirurgie. 1918;147:128. [Google Scholar]
- 4.Lazaridis N, Zouloumts L, Venetis G, Karakasis D. The inferiorly and superiorly based nasolabial flap for the reconstruction of moderate-sized oronasal defects. J Oral Maxillofac Surg. 1998;56:1255–1259. doi: 10.1016/S0278-2391(98)90603-6. [DOI] [PubMed] [Google Scholar]
- 5.El-Marakby HH. The versatile naso-labial flaps in facial reconstruction. J Egypt Nat Cancer Inst. 2005;17(4):245–250. [PubMed] [Google Scholar]
- 6.Menick FJ. The two-stage nasolabial flap for subunit reconstruction of the ala. Oper Tech Plast Reconstr Surg. 1998;5(1):59–64. doi: 10.1016/S1071-0949(98)80031-0. [DOI] [Google Scholar]