Abstract
Objective
The study aims to evaluate the efficacy of arthrocentesis in the treatment of internal derangement of the temporomandibular joint (TMJ).
Study Design
Thirty patients with TMJ internal derangement underwent arthrocentesis using saline. Pain using visual analog scale, maximum mouth opening, joint noises and mandible deviation were documented pre-operatively and post-operatively. Patients were followed for 1 year. Statistical analysis of pain was done by Wilcoxon signed Rank’s test and dysfunction by students paired t test.
Results
The mean pre-operative pain was 4.8 ± 2.65 and post-operatively at 1 year was 0.27 ± 0.45 with an average decrease of 4.72 (P = 0.000). The mean maximal mouth opening pre-operatively was 29.8 ± 2.35 mm and post-operatively 41.9 ± 2.48 mm at 1 year. The mean increase in the mouth opening was 12.1 ± 3.0 mm (P = 0.000).
Conclusion
Arthrocentesis is simple, minimally invasive procedure with less risk of complications and significant benefits in patients with TMJ internal derangement.
Keywords: Temporomandibular joint, Internal derangement, Arthrocentesis
Internal derangement of the temporomandibular joint (TMJ) is characterized by displacement of the intra-articular disc, resulting in clicking and popping sounds. However, the displacement of the articular disc does not always cause a mechanical obstruction. These conditions may be painless or they may be associated with pain, especially during function. The most common causes are trauma, which results in an immediate displacement of the disc, or chronic parafunction, which results in degenerative changes in the articular surfaces, increased friction, and gradual disc displacement.
TMJ internal derangement has always presented as therapeutic challenge to the maxillofacial surgeons. Up to 25% of the entire population has internal derangement of TMJ and usually they are treated with nonsurgical methods such as medications, physiotherapy and occlusal splints in the initial period [1]. When these methods are unsuccessful, they are often managed by surgical methods. The mainstay of surgical treatment is based on changing the morphology or position of the disc, or removal of the disc with or without replacement. There are variable reports of success with the open surgical methodologies and are associated with surgical risks and potential long term sequelae [2].
New insights into the joint pathology of internal derangement were provided by the observations made during TMJ arthroscopic lysis and lavage and outcomes after such treatment. The physical action of lysis and lavage in the superior joint space, rather than disc repositioning, is believed to be responsible for the success of arthroscopic surgery [3, 4]. This has led to the use of TMJ arthrocentesis as a relatively less invasive alternative to reduce the inflammation in the superior joint space and restore normal range of motion [3]. The study aims to discuss the role of arthrocentesis in the treatment of internal derangement of the TMJ and present clinical data relating to the efficacy of arthrocentesis.
Materials and Methods
This prospective clinical study was approved by the institutional review board and ethical commission written informed consent was obtained. Criteria for selection of the patients was based on history and clinical findings characteristic of internal derangement. All these patients were initially treated with NSAIDS for 1 week and occlusal splints for 1 month had failed to respond to these conservative treatments. A transpharyngeal TMJ view radiograph was taken in all of them to rule out degenerative joint diseases. The patients with degenerative joint diseases such as osteoarthritis, rheumatoid arthritis, gout etc. causing temporomandibular joint dysfunction were excluded from the study. A total of 30 patients with TMJ internal derangement with failed conservative management, of whom 24 had nonreducing disc displacement and 6 had closed lock which were subjected to TMJ arthrocentesis.
Under aseptic precautions, arthrocentesis was performed in the superior joint space. With patient seated at 45° angle, the points of needle insertion were marked on the skin according to the method suggested by Mc. Cain. A line was drawn from the middle of the tragus to the outer canthus. Entry points were marked along this canthotragal line. The first point corresponding to glenoid fossa was marked 10 mm from the midtragus and 2 mm below the line and second point corresponding to articular eminence was marked 10 mm from the first point and 10 mm below the line. 2 ml of 2% Lignocaine was injected to anesthetise the articular branch of auriculotemporal nerve. Patients were asked to open the mouth wide and mandible was held in the protruded position. A 19 gauge needle was then introduced at the first point and 2 ml of saline was injected through this needle to distend the joint space. Another 19 gauge needle was then inserted at the second point to establish a free flow of the solution through the joint space. A syringe filled with saline was injected under pressure into the superior joint space through the first needle and second needle provided the outflow for the saline. A total of 50–100 ml solution was used to lavage the superior joint space and the needles were removed. Patient’s lower jaw was gently manipulated in the vertical, protrusive and lateral excursions to free up the disc. Post-operatively antibiotics, NSAIDS and muscle relaxants were advised for 1 week. (Fig. 1)
Fig. 1.
Lavage of the joint
The pre-operative and post-operative clinical assessment was done by a single clinician for signs and symptoms of TMJ disorders which included pain, mouth opening, joint noises and jaw deviation. Pain was assessed using a visual analog scale (0–10). Mouth opening was measured as the maximum interincisal distance in millimeters using a scale. The patients were assessed for all the parameters pre-operatively, and post-operatively on day 1, 1 week, 2 weeks and then monthly till 6 months and later once in 2 months till 1 year. All results were calculated using the mean value and standard deviation for each of the parameters considered and checked for statistical significance using Wilcoxon signed ranks test for pain and students paired t test for mouth opening.
Results
Pain was studied in 30 patients with internal derangement, pre-operatively 27 patients complained of pain and 3 of them with closed lock did not have pain. With arthrocentesis 26 (96%) patients showed significant decrease in the level of pain in the followup period.
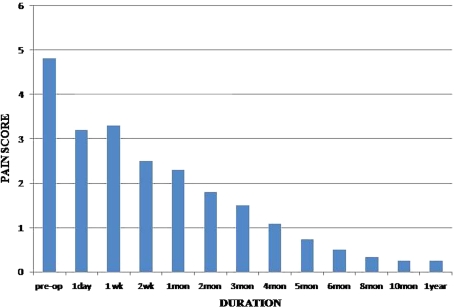
The mean of pain score was pre-operatively five. In the post-operative period pain score reduced to 3.3 at 1 week (P = 0.000), 2.25 at 1 month (P = 0.000) and 1.7 at 2 months (P = 0.000). The presence of pain at 1–2 months can be attributed to post-operative pain of different quality. There was gradual reduction in the mean pain score from pre-operatively 5–0.5 till 6 months and thereafter patients did not complain of any pain excepting in those where pre-operative pain score was more than seven, complained of mild pain (pain score-1) which further reduced to 0.27 by 1 year. The mean reduction of pain noted after 1 year was 4.72, which is statistically significant (P = 0.000) (Table 1, Fig. 2).
Table 1.
The comparison of pre-treatment and post-treatment degree of pain
| Period | Mean | Z value | Z value | Mean | P value | P value |
|---|---|---|---|---|---|---|
| 1 day post-operative | 1 year | Diff. | 1 day post-operative | 1 year | ||
| Pre-operative | 4.8 ± 2.65 | 4.617 | 4.553 | 4.72 | 0.000 | 0.000 |
| After 1 year | 0.27 ± 0.45 |
Fig. 2.
Graph showing pain evaluation
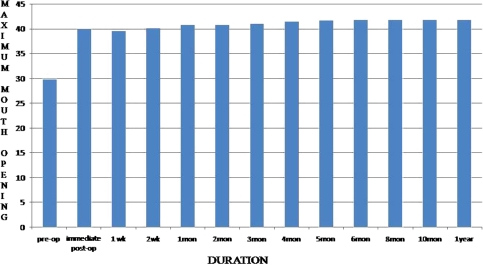
The mean maximum mouth opening(MMO) pre-operatively was 29 mm and increased to 40 mm immediately following arthrocentesis which increased by 0.5–1 mm at every month followup with mean MMO of 42 mm at 6 months. Thereafter it remained consistent till 1 year. The mean increase in the mouth opening at 1 year was 12 mm and is statistically significant (P = 0.000) (Table 2, Fig. 3.
Table 2.
Comparison of pre-treatment and post-treatment mouth opening
| Period | Mean | t value | t value | Mean | P value | P value |
|---|---|---|---|---|---|---|
| Immediate post-operative | 1 year | Diff. | Immediate post-operative | 1 year | ||
| Pre-operative | 29.8 ± 2.35 | 17.727 | 22.164 | 12.1 ± 3.0 | 0.000 | 0.000 |
| After 1 year | 41.9 ± 2.48 |
Fig. 3.
Graph showing mouth opening evaluation
The effect of the treatment for clicking and deviation was made on the basis of the proportion of improvement at the end of treatment by noting their presence or absence.
Of the 30 patients, 24 initially complained of clicking. At the end of 1 year, 15 (62%) patients stated no evidence of clicking. All the study group had deviation and improvement was seen in 21 (70%) patients.
Discussion
There is clinical evidence supporting the existence of disc displacement in TMJ internal derangement. However, current concept suggests that a change in the position of the disc is not a primary factor in TMJ pain and dysfunction but alterations in joint pressure (negative intra-articular pressure), a variety of biochemical substances, constituents of the synovial fluid (and thereby failure of lubrication) may lead to clicking and derangement of the TMJ [3, 5, 6]. The presence of inflammatory cells and inflammatory mediators, including arachidonic acid metabolites and cytokines were demonstrated in symptomatic TMJs [5, 6]. Lavage of the upper joint space reduces pain by removing inflammatory mediators from the joint, increasing mandibular mobility by removing intra-articular adhesions, eliminating the negative pressure within the joint, recovering disc and fossa space and improving disc mobility, which reduces the mechanical obstruction caused by the anterior position of disc. [7–10].
Arthrocentesis has developed as a natural consequence of the success of arthroscopic lavage and lysis for the treatment of internal derangements [4]. Nitzan et al. first described arthrocentesis as the simplest form of surgery in the TMJ, aiming to release the articular disc and to remove adhesions between the disc surface and the mandibular fossa by means of hydraulic pressure from irrigation of the upper chamber of the TMJ [7, 9, 11].
Studies done to know whether the effect of arthrocentesis on internal derangements are merely palliative or it provides long term relief of the associated symptoms have shown that arthrocentesis can produce long term relief of pain and dysfunction in patients with internal derangements of the TMJ [2, 12]. Arthrocentesis is 91% effective in treating patients with anterior disc displacement without reduction [8, 13, 14].
In this study 96% showed significant reduction in pain with arthrocentesis. The pain reduction is attributed to the high pressure irrigation which washes away inflammatory mediators and providing pain relief. Failure in pain relief in one case may be due to pain originating from causes other than internal derangement.
Arthrocentesis under sufficient pressure can also remove adhesions, widen the joint spaces and improve mouth opening [3, 15, 16]. In patients who presented with limited mouth opening, significant improvement was seen in the immediate post-operative period and with reduction in pain, mouth opening further increased from third to sixth months. The mean increase in the mouth opening was 12.15 mm. Marginal improvement was observed with jaw deviation and clicking. Assessment of these parameters will require a larger sample and longer followup.
In cases where TMJ arthrocentesis fails to achieve the desired outcome, a number of factors should be considered. Appropriate case selection is important, as this technique is not effective in certain conditions such as with bony changes, fibroankylosis and perforation of the disc [11, 15]. Even when the indications are apparent other associated factors such as muscle spasm must be brought under control prior to arthrocentesis. Cases were arthroscopy or open joint surgery is indicated but the clinician is uncertain of the diagnosis, arthrocentesis may be used as a simple interim measure that can confirm the need for more invasive procedure [9, 17].
A major disadvantage of arthrocentesis is the failure to directly observe intra-articular pathology, the ability to biopsy pathological tissue and difficulty in treating more mature adhesions [18]. Sweeping and other non-operative arthroscopic maneouvres which can be performed with arthroscopic lysis and lavage are not possible with arthrocentesis. Transient facial paresis due to the local anaesthetic or swelling of the neighboring tissues caused by perfusion of solution may occur during arthrocentesis [19]. Two patients in this study complained of transient altered motor function on the side of arthrocentesis.
Conclusion
Arthrocentesis is a simple and minimally invasive procedure. Lavage of superior joint space with saline exerts its effects through its ability to eliminate joint effusion thus reducing the symptoms. These observations make arthrocentesis proposed line of treatment option for patients with TMJ internal derangements.
References
- 1.Barkin S, Weinberg S. Internal derangements of the TMJ: the role of arthroscopic surgery and arthrocentesis. J Can Dent Assoc. 2000;69:199–203. [PubMed] [Google Scholar]
- 2.William A, Carvagal Daniel M, Laskin Long term evaluation of arthrocentesis for the treatment of internal derangements of the temporomandibular joint. J Oral Maxillofac Surg. 2000;58:852–855. doi: 10.1053/joms.2000.8201. [DOI] [PubMed] [Google Scholar]
- 3.Franklin Dolwick M. Intra articular disc displacement part I: its questionable role in temporomandibular joint pathology. J Oral Maxillofac Surg. 1995;53:1069–1072. doi: 10.1016/0278-2391(95)90126-4. [DOI] [PubMed] [Google Scholar]
- 4.David Frost E, Barry Kendell D. “The use of arthrocentesis for treatment of temporomandibular joint disorders”. J Oral Maxillofac Surg. 1999;57:583–587. doi: 10.1016/S0278-2391(99)90080-0. [DOI] [PubMed] [Google Scholar]
- 5.Alpaslan C, et al. Effect of arthrocentesis and sodium hyaluronate injection on nitrite, nitrate, and thiobarbiturate acid- reactive substance levels in the synovial fluid. Oral Surg Oral Med Oral Pathol. 2000;89:686–690. doi: 10.1067/moe.2000.105518. [DOI] [PubMed] [Google Scholar]
- 6.Nishimura M, Segami N, Kaneyama K, Sato J, Fujimura K. Comparison of cytokinin level in synovial fluid between successful and unsuccessful cases in arthrocentesis of temporomandibular joint. J Oral Maxillofac Surg. 2004;62(3):284–287. doi: 10.1016/j.joms.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Dorrit W, Nitzan, et al. Temporomandibular joint arthrocentesis simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163–1167. doi: 10.1016/0278-2391(91)90409-F. [DOI] [PubMed] [Google Scholar]
- 8.Kaneyama K, Segami N, Nishimura M, Sato J, Fujimura K, Yoshimura H. The ideal volume for removing bradykinin, interleukin-6 and protein from the temporomandibular joint by Arthrocentesis. J Oral Maxillofac Surg. 2004;62(6):657–661. doi: 10.1016/j.joms.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 9.Moses J, et al. The effect of arthroscopic surgical lysis and lavage of the superior joint space on temporomandibular joint disc position and mobility. J Maxillofac Surg. 1989;47:674–678. doi: 10.1016/S0278-2391(89)80004-7. [DOI] [PubMed] [Google Scholar]
- 10.Dimitroulis G, Dolwick MF, Martinez A. TMJ arthrocentesis and lavage for the treatment of closed lock. Br J Oral Maxillofac Surg. 1995;33:23–27. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 11.Kirk L, Fridrich, et al. Prospective comparison of arthroscopy and arthrocentesis for temporomandibular joint disorders. J Oral Maxillofac Surg. 1996;54:816–820. doi: 10.1016/S0278-2391(96)90526-1. [DOI] [PubMed] [Google Scholar]
- 12.Alpaslan C, Dolowick MF, Heft MW. ”Five year study of retrospective evaluation of temporomandibular joint arthrocentesis”. Int J Oral Maxillofac Surg. 2003;32:263–267. doi: 10.1054/ijom.2003.0371. [DOI] [PubMed] [Google Scholar]
- 13.Dorrit W, Nitzan The use of arthrocentesis for the treatment of osteoarthritic temporomandibular joint. J.Oral Maxillo Surg. 2001;59:1154–1159. doi: 10.1053/joms.2001.26716. [DOI] [PubMed] [Google Scholar]
- 14.Emshoff R. “Clinical factors affecting the outcome of arthrocentesis and hydraulic distention of temporomandibular joint” oral surgery, oral medicine, oral pathology, oral radiology. Endodontics. 2005;100(4):409–414. doi: 10.1016/j.tripleo.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 15.Yura S, et al. Can arthrocentesis release intracapsular adhesions? Arthroscopic findings before and after irrigation under sufficient hydraulic pressure. J Oral Maxillofac Surg. 2003;61:1253–1256. doi: 10.1016/S0278-2391(03)00724-9. [DOI] [PubMed] [Google Scholar]
- 16.Yura S, Totsuka Y. Relationship between effectiveness of arthrocentesis under sufficient pressure and condition of temporomandibular joint. J Oral Maxillofac Surg. 2005;63(2):225–228. doi: 10.1016/j.joms.2004.06.053. [DOI] [PubMed] [Google Scholar]
- 17.Howard Israel A, et al. The relationship between temporomandibular joint synovitis and adhesions: pathologic mechanisms and clinical implications for surgical management. J Oral Maxillofac Surg. 2006;64:1064–1074. doi: 10.1016/j.joms.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 18.Dorrit W, Nitzan “Arthrocentesis–incentives journal for using this minimally invasive approach for temporomandibular disorders”. Oral Maxillofac Surg Clin North Am. 2006;18:311–328. doi: 10.1016/j.coms.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Gokhan H, Alpaslan C, Alpaslan Efficacy of temporomandibular joint arthrocentesis with and without injection of sodium hyaluronate in treatment of internal derangements. J Maxillofac Oral Surg. 2001;59:613–618. doi: 10.1053/joms.2001.23368. [DOI] [PubMed] [Google Scholar]