Abstract
Trichilemmoma is a hamartomatous proliferation arising from cells of hair follicle. Its desmoplastic variant simulates an invasive carcinoma. In this tumor, the cell of origin seems to be located in the superficial level of the hair follicle just below the basement membrane at the sebaceous gland level. We present a similar case which presented with an asymptomatic nodular lesion in the region above the upper lip on left side. Fine needle aspiration cytology raised the cytological possibility of a malignancy for which the lesion was excised. On histopathology the lesion was diagnosed as desmoplastic trichilemmoma. The case highlights the difficulty encountered in differentiating a benign adnexal tumor from malignant lesion based on cytology alone. Moreover, the extensive desmoplasia on histopathology raises the suspicion of invasive malignancy which requires to be carefully excluded. The superficial features of trichilemmoma and lack of cellular atypia is a useful diagnostic clue in such a situation. Positivity of CD34 can also be used to differentiate from basal cell carcinomas. The case reported here had a solitary lesion, but follow up is required for development of more lesions or multiple hamartomas in other organs as a part of Cowden’s disease.
Keywords: Trichilemmoma, Desmoplastic, Hamartoma
Introduction
Trichilemmoma is a benign solid tumor that presents frequently as a lobular formation or plate like growth of glycogen rich clear cells with palisading, sometimes exhibiting central keratinization. Multiple trichilemmomas are associated with acral keratoses, sclerotic fibromas of skin, papillomas of the oral mucosa, and occasionally, tumors of the breast, thyroid, and gastrointestinal tract—a condition known as Cowden’s disease or multiple hamartoma syndrome. A desmoplastic variety of trichilemmoma that simulates an invasive carcinoma has been described [1–3]. Trichilemmal carcinoma is a tumor that combines features of trichilemmal type keratinization with atypical features such as brisk mitotic activity, invasion of reticular dermis, and ulceration [4–8]. Extensive desmoplasia on histopathology of trichilemmoma raises the suspicion of invasive malignancy which requires to be carefully excluded.
Case Report
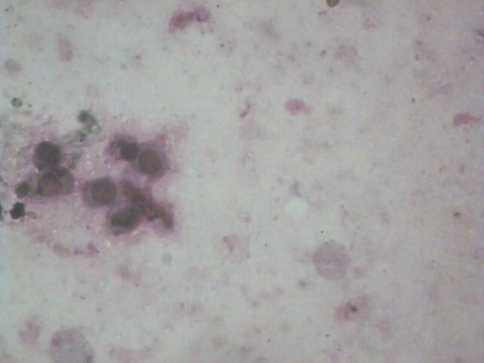
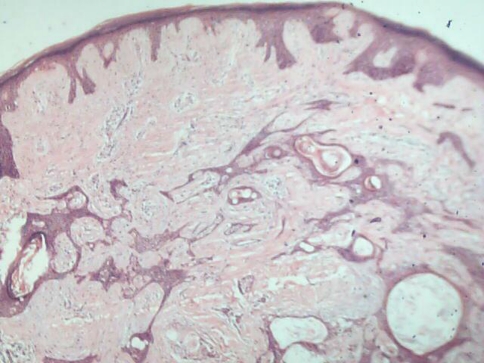
A 37 year old male presented with an asymptomatic nodular lesion in the region above upper lip on the left side since 1 year. Mode of onset was insidious. The lesion progressed to its present size over a period of time. There were no secondary changes and it was not associated with any other sign or symptom. Medical, dental and family history was non contributory. The individual was non smoker, used to consume alcohol occasionally and had no deleterious oral habit. No abnormality was detected on general physical examination. There were no other sign or symptom suggestive of any systemic illness. On examination a single small oval nodule was found in the nasolabial region on the left side (Fig. 1). Cervicofacial group of lymph nodes were not palpable. An FNAC was performed. It revealed paucicellular aspirates with small basaloid cells in clusters and occasional ductal pattern with small round to oval nuclei. The features suggested a differential of basal cell carcinoma and adnexal tumor (Fig. 2). Wide local excision was carried out under general anesthesia taking the lesion as invasive carcinoma. The histopathologic examination led to the diagnosis of desmoplastic trichilemmoma. The initial healing was satisfactory. Six months later the patient is free from recurrence.
Fig. 1.
Nodular lesion in the nasolabial region
Fig. 2.
FNAC photomicrograph of cell (40×) H and E stain
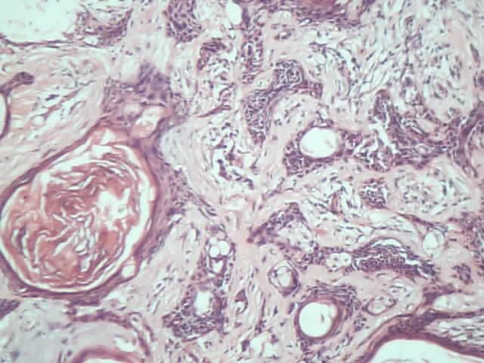
Histopathology (Figs. 3, 4)
Fig. 3.
Low power (H&E stain; 40×) photomicrograph of the lesion on histopathology
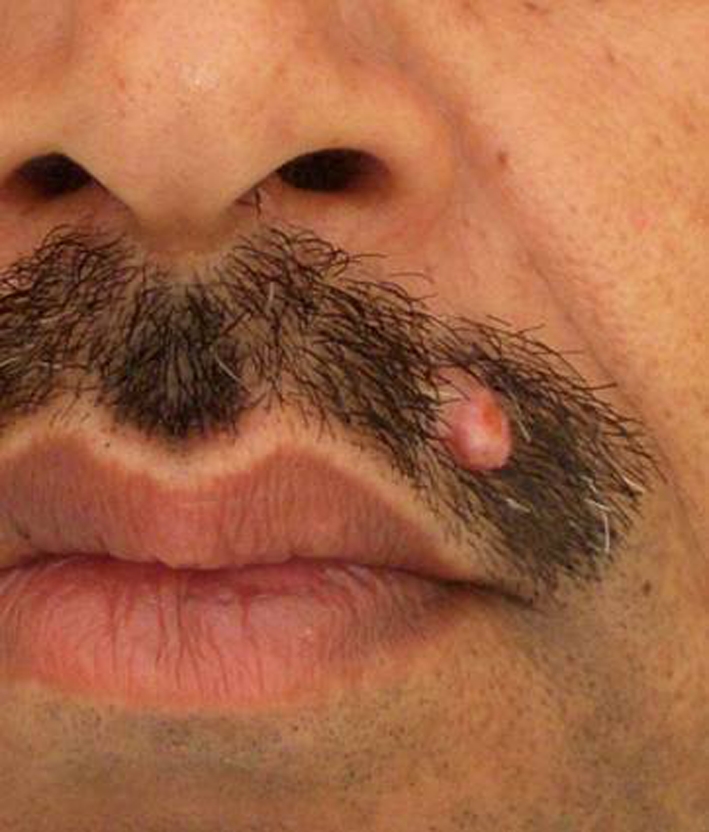
Fig. 4.
High power (H&E stain; 100×) photomicrograph of the lesion on histopathology
On histopathology, a diagnosis of desmoplastic trichilemmoma was made with the warty growth covered by mature keratinizing stratified squamous epithelium. The underlying dermis shows irregular extensions of cords of squamous cells from hair roots in a desmoplastic stroma. These extensions mimic invasion, but lack cytological atypia. The surrounding stroma is composed of fibrocollagenous tissue which in foci shows myxoid changes. The remainder of the tissue shows unremarkable native elements.
Discussion
The trichilemmoma is a hamartomatous proliferation arising from cells of the hair follicle [9]. In this tumor, the cell of origin seems to be located in the superficial level of the hair follicle just below the basement membrane at the sebaceous gland level. Trichilemmomas may occur as solitary, independent tumors, but multiple lesions occur as the dominant feature of Cowden syndrome. In fact, multiple trichilemmomas are the most concise marker for the diagnosis of Cowden syndrome, which is an autosomal dominant trait for multiple hamartomas (99%) as compared to breast tumors (75%), thyroid tumors (88%), and gastrointestinal tumors (70%). Pertinent to the oral and maxillofacial specialist, papillary lesions of the lips, gingival, alveolar ridge, and tongue are seen in almost all patients with Cowden syndrome. These lesions produce a cobblestone appearance to the affected mucosa, which, when biopsied, will show multiple fibromas with the development of internal malignancies. The eruption of multiple skin lesions in a teenager or young adult may raise suspicions for basal cell nevus syndrome as well as Cowden syndrome. As isolated lesions they will also resemble small basal cell carcinomas, skin squamous cell carcinomas, and keratocanthomas [10–13]. They may also resemble the early stages of an outbreak of molluscum contagiosum and, if only one or a few lesions are present the common wart verruca vulgaris. There is a lobular proliferation of uniform small cells into the dermis from epidermis. Glycogen containing clear cells may be conspicuous. The peripheral cells are columnar and palisading. Keratinization occurs on the surface of the epidermis and may be sufficient to form a cutaneous horn. Solitary trichilemmomas may be excised for cure using 2-mm peripheral margins and excision deep to the deepest extent of the tumor [14, 15].
References
- 1.Boscaino A. Tricholemmal carcinoma. A study of seven cases. J Cutan Pathol. 1992;19(2):94–99. doi: 10.1111/j.1600-0560.1992.tb01349.x. [DOI] [PubMed] [Google Scholar]
- 2.Brownstein MH, Wolf M, Bikowski JB. Cowden’s disease. A cutaneous marker of breast cancer. Cancer. 1978;41(6):2393–2398. doi: 10.1002/1097-0142(197806)41:6<2393::AID-CNCR2820410644>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 3.Carlson JG, Nivatvongs S, Snover DC. Colorectal polyps in Cowden’s disease. Am J Surg Pathol. 1984;8(10):763–770. doi: 10.1097/00000478-198410000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Hunt SJ, Kilzer B, Santa Cruz DJ. Desmoplastic trichilemmoma. Histological variant resembling invasive carcinoma. J Cutan Pathol. 1990;17(1):45–52. doi: 10.1111/j.1600-0560.1990.tb01677.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee JY, Tang CK, Leung YS. Clear cell carcinoma of the skin. A tricholemmal carcinoma? J Cutan Pathol. 1989;20(1):31–39. doi: 10.1111/j.1600-0560.1989.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 6.Reis JP, Tellechea O, Cunha MF, Baptista AP. Trichilemmal carcinoma. Review of 8 cases. J Cutan Pathol. 1993;20:44–49. doi: 10.1111/j.1600-0560.1993.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 7.Swanson PE, Marrogi AJ, Williams DJ, Cherwitz DL, Wick MR. Tricholemmal carcinoma. Clinicopathologic study of 10 cases. J Cutan Pathol. 1992;19(2):100–109. doi: 10.1111/j.1600-0560.1992.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 8.Wong TY, Suster S. Tricholemmal carcinoma. A clinicopathologic study of 13 cases. Am J Dermatopathol. 1994;16(5):463–473. doi: 10.1097/00000372-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Woo VL, Abdelsayed R. Oral manifestations of internal malignancy and paraneoplastic syndromes. Dent Clin North Am. 2008;52:203–230. doi: 10.1016/j.cden.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Sanders DSA, Carr RA. The use of immunohistochemistry in the differential diagnosis of common epithelial tumours of the skin. Curr Diagn Pathol. 2007;13(4):237–251. doi: 10.1016/j.cdip.2007.05.012. [DOI] [Google Scholar]
- 11.Carr RA, Taibjee SM, Sanders DSA. Basaloid skin tumours: basal cell carcinoma. Curr Diagn Pathol. 2007;13(4):252–272. doi: 10.1016/j.cdip.2007.05.005. [DOI] [Google Scholar]
- 12.Carr RA, Sanders DSA. Basaloid skin tumours: mimics of basal cell carcinoma. Curr Diagn Pathol. 2007;13:273–300. doi: 10.1016/j.cdip.2007.05.003. [DOI] [Google Scholar]
- 13.Jubb KVF, Kennedy PC, Palmer N. Neoplastic and reactive diseases of the skin and mammary glands. In: Maxie MG, editor. Pathology of domestic animals, 5th edn. New York: Academic Press; 2007. pp. 746–781. [Google Scholar]
- 14.Ruhoy SM, Thomas D, Nuovo GJ. Multiple inverted follicular keratoses as a presenting sign of Cowden’s syndrome: case report with human papillomavirus studies. J Am Acad Dermatol. 2004;51(3):411–415. doi: 10.1016/j.jaad.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 15.Krishnakumar S, RavindraMohan E, Kalpana B, Das D, Biswas J. Eccrine duct carcinoma of the eyelid mimicking meibomian carcinoma: clinicopathological study of a case. Surv Ophthalmol. 2003;48(4):439–446. doi: 10.1016/S0039-6257(03)00050-X. [DOI] [PubMed] [Google Scholar]