Abstract
Condylar hyperplasia of mandible is overdevelopment of condyle, unilaterally or bilaterally, leading to facial asymmetry, mandibular deviation, malocclusion and articular dysfunction. This is a series of five such patients managed at our centre.
Keywords: Facial asymmetry, Condylar hyperplasia
Introduction
Condylar hyperplasia of mandible is overdevelopment of condyle, unilaterally or bilaterally, leading to facial asymmetry, mandibular deviation, malocclusion and articular dysfunction. It normally occurs in mid teens with increasing deformity until cessation of growth [1]. Prominent features include an enlarged mandibular condyle, elongated condylar neck, outward bowing and downward growth of body and ramus of mandible on affected side, causing fullness of face on that side and flattening of face on the contralateral side [1]. If deformity occurs before growth is complete, the occlusal plane usually becomes slanted for dental compensation, whereas posterior open bite is usually apparent if deformity occurs after completion of growth.
Unilateral condylar hyperplasia must be differentiated from other states of overdevelopment like hemifacial hypertrophy (unilateral enlargement of all hard and soft tissues of face), unilateral macrognathia (unilateral mandibular hypertrophy, which is a three dimensional enlargement of mandible, including both condyles, ramus and ends at midline of symphysis) and laterognathia (asymmetrical prognathism where both condyles are equal in size). Chondroma and osteochondroma may produce similar symptoms and signs, but they grow more rapidly and may cause even greater asymmetric condylar enlargement.
Materials and Methods
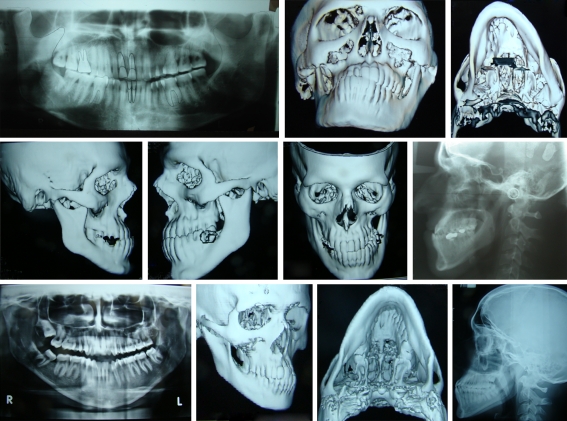
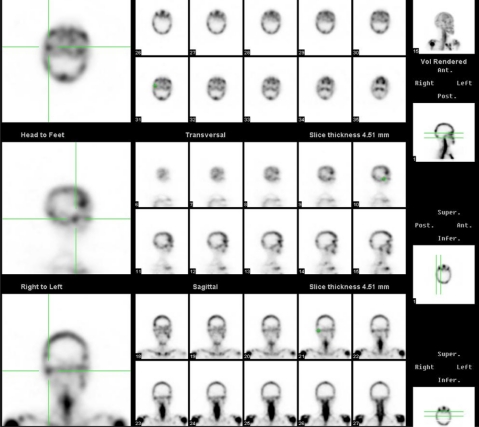
A total of five patients with the primary complaint of facial asymmetry due to condylar hyperplasia who visited the outpatient department of Oral and Maxillofacial Surgery, CSMMU (formerly King George’s Medical University), Lucknow between 2005 and 2006 and were randomly selected. Informed consent was taken from all the patient’s or the parents in case of minor patient prior to their inclusion in the study. Age, sex and a detailed history of the mode of onset and duration were recorded. Any obvious facial asymmetry, scar mark or deviation of chin were examined. The oral cavity was examined to see the deviation of midline, occlusion, crossbite (Fig. 1), any evidence of protrusive, retrusive and lateral movements, gingival condition, caries and any impacted or abnormally placed teeth. Dental models were fabricated to analyze the occlusal discrepancies. Radiological assessment (Fig. 2) of both the joints was carried out with orthopantomograms and CT scan (both axial and coronal view). Scintigaphy (Fig. 3) using 99mTc-MDP was advocated as a method of diagnosis and presurgical assessment of patients with condylar hyperplasia to distinguish the growing condyle from non growing one and to assess whether there was still phase of growth. Routine haematological examination were carried out in all the patients preoperatively. All the patients were operated under general anaesthesia with nasoendotracheal intubation. The joint was exposed through Al-Kayat Bramley incision and a high condylar shave or condylectomy as planned, was carried out with the help of surgical bone cutting device (Stryker). Specimen was sent for histopathological examination. Saggital split osteotomy was planned and performed bilaterally, when gross asymmetry existed along with protrusion, and unilaterally, in cases of minor discrepancies. All the patients were evaluated postoperatively for their improvement in facial esthetics, occlusion and any obvious complication.
Fig. 1.
Preoperative occlusion of patients
Fig. 2.
Radiographs of cases
Fig. 3.
Scintigraphy showing hot spots
Results
The present study was conducted on five patients with facial asymmetry due to condylar hyperplasia (three males, two females). Most of the cases were in their teens (three patients) or young adult (one patient). The mean age of study population was 22.8 years. Trauma was the most common etiology seen in four patients (80%).
Facial asymmetry (Fig. 4) was the most common clinical finding, followed by midline shift, protruded chin, contralateral crossbite and maxillary cant. Radiographic examination revealed change in shape of condylar head (one patient), elongated condylar neck (three patients), bowing of inferior border (two patients) and hemimandibular enlargement (two patients). Two patients were planned for condylectomy as their first procedure, but facial symmetry and a normal occlusion was achieved by that single procedure. So, they did not undergo any further surgeries. A patient with good intercuspal dental relationship was treated only with high condylar shave. Patient with gross facial asymmetry and prognathic mandible required bilateral sagittal split osteotomy to gain a good functional occlusion while another patient gained a good occlusion just with unilateral sagittal split osteotomy.
Fig. 4.
Preoperative and postoperative pictures of cases 1, 2, 4, 5
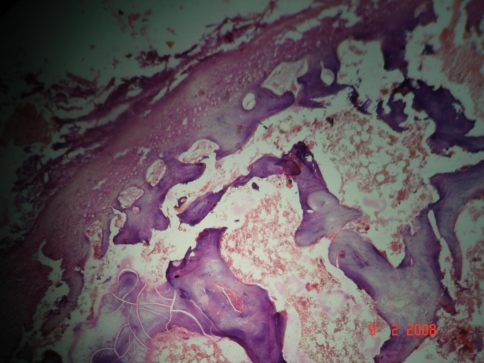
Histopathological examination revealed thickened irregular bony trabeculae, uninterrupted layer of undifferentiated mesenchymal cells, hypertrophic cartilage, islands of chondrocytes in subchondral trabecular bone and increased thickness of cartilaginous layer (Fig. 5).
Fig. 5.
Histopathological picture showing thickened, irregular bony trabeculae, with increased thickness of cartilaginous layer (condylar hyperplasia)
The patients were followed up regularly in their postoperative phase for a period of 2 years (Table 1).
Table 1.
Demographic data, clinical features and treatment done
| S no. | Age | Sex | Side | History | Asymmetry | Enlarged condyle | Elongated condylar neck | Inferior border bowing | Hemimandibular enlargement | Maxillary cant | Occlusion | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 42 | M | Rt | Trauma | √ | √ | X | x | X | X | Crossbite | Condylectomy |
| 2 | 16 | F | Lt | Trauma | √ | √ | √ | X | Crossbite | Condylectomy | ||
| 3 | 17 | F | Lt | Trauma | √ | X | X | √ | x | High condylar shave | ||
| 4 | 18 | M | Rt | Trauma | √ | √ | √ | x | X | Crossbite | Condylectomy + bilateral sagittal split osteotomy | |
| 5 | 21 | M | Rt | x | √ | x | x | √ | x | Crossbite | Unilateral sagital split osteotomy |
Review of Literature
Asymmetric conditions attributed to condylar hyperplasia of the mandible were first reported by Adams in 1836. Gottlieb [2] described condylar hyperplasia as an osteoma causing unilateral deformity and prognathic deviation subsequent to a bilateral disproportion in the size of the condyles. Rowe [3] characterized unilateral condylar hyperplasia as being associated with elongation of the condylar neck, bowing of the inferior body of the mandible, lateral crossbite, and contralateral concavity of the lateral aspect of the ramus.
Slowly progressive unilateral enlargement of the head and neck of the condyle causes crossbite malocclusion, facial asymmetry, and shifting of the midpoint of the chin to the unaffected side [4]. The patient may appear prognathic. Often, the lower border of the mandible may be convex on the affected side.
Two types of deformity are usually observed: increased anteroposterior mandibular length with associated buccal crossbite or increased vertical ramus height with tilted occlusal plane and lateral open bite resulting in facial asymmetry and reduced opening on affected side. Asymmetry improves as mouth is opened due to translation of condyle on the normal side.
However, additional factors like hormonal influences [5], hypervascularity, heredity [6], infection or trauma [7, 8] may stimulate this excess growth of condyle. It is invariably unilateral, if bilateral is asymmetric.
Sequential study models, radiological and scintigraphic methods are commonly used for diagnosis and monitoring of its macroscopic aspects. Lateral and posteroanterior cephalograms [9], transcranial and panoramic radiographs are evaluated for possible differences in size, shape, and length of the condyle, condylar neck, mandibular body or rami on the right/left side. The radiographs are also used for purposes of tracing and determining bilateral discrepancies contributing to the skeletal asymmetry as well as assessing the amount of deviation of dental and skeletal midlines from mid saggital plane, elongation of the involved mandibular condyle/condylar neck, and downward bowing of the mandibular ramus or body. Condylar elongation is calculated through transcranial view of skull by measuring the distance from top of the condyle to a line drawn through the base of sigmoid notch and compared to contralateral side. Computerized Tomography (CT)[10] is performed to assess if the bone growth is generalized, which confirms the diagnosis, or localized to a part of the condylar head. If growth is localized, a biopsy may be necessary to distinguish between tumor and hyperplasia. The 3D tomography is useful to evaluate precisely the morphological and structural alterations of the craniofacial bones on a three dimensional base.
Not only the macromorphology but also the micromorphology of the diseased condyle differs from that on the unaffected side [11]. Gray et al. [12] reported that bony trabeculae were often thickened and irregular resulting in consistently large volume of trabecular bone and higher than normal percentage of surfaces covered in osteoids. Histologically [13], the presence of an uninterrupted layer of undifferentiated germinating mesenchymal cells, hypertrophic cartilage, and islands of chondrocytes in the subchondral trabecular bone, were also said to be typical. When normal and hypertrophic mandibular condyles are compared, the thickness of cartilaginous layer seems to be considerably increased in condylar hyperplasia [14].
Isotope bone scans have been used for a number of years to assess growth activity in the mandibular condyle in patients who present with facial asymmetry to distinguish normal bone growth within the condyle from increased activity that may be the cause of the asymmetry. Previous studies have, however, relied only on planar images [15, 16]. SPECT (Single Photon Emission Computed Tomography) [17, 18] has been used with quantitative assessments of one mandibular condyle to clivus or lumbar spine, but when one condyle is compared with the other, it is more sensitive and accurate in detecting abnormal activity. A relative percentage uptake of 55% or more in the affected mandibular condyle is considered to be abnormal, and this has been validated by comparison with an age-matched control group. SPECT has been used as an aid to diagnosis and treatment in 18 patients with asymmetrical growth and have constructed a therapeutic algorithm to aid the treatment of these patients [19]. Various diagnostic methods in cases of hyperplasia of the mandibular condyle in a growing subject have been studied [20] like bone scintigraphy [21, 22], 3D tomography and electrognathographic analysis, associated with standard radiography and cephalometry, which are important methods of diagnosis in order to make an early diagnosis of hyperplasia of the mandibular condyle and differentiate it with other pathologies. Bone scintigraphy is a useful screening procedure to detect if the pathology is in an active phase or not. Finally, the electrognathographic test records the mandibular activity both in physiological and pathological conditions. PET Scan has been successfully used in the assessment and management of condylar hyperplasia [23]. All these instrumental techniques allow to make a diagnosis and lead to a possible therapeutical approach.
Treatment usually includes condylectomy during the period of active growth. If growth has stopped, orthodontics and surgical mandibular repositioning are indicated. If the height of the mandibular body is greatly increased, facial symmetry can be further improved by reducing the inferior border [24].
Discussion
Treatment depends on age, degree of deformity and hypofunction [25]. The basic considerations in the management of facial asymmetry secondary to condylar hyperplasia must include control of the growth process to allow more balanced facial development. This can be done by high condylectomy or condylar shave in actively growing cases [26] and in cases in which a definite tissue diagnosis is mandated. If noticed in puberty while still growing, condylectomy alone may suffice [27]. If seen later, when compensatory growth has occurred, would need condylectomy and osteotomies often of mandible and maxilla to restore facial symmetry and normal occlusion [28, 29]. Treatment usually includes condylectomy during the period of active growth. The decision of whether condylectomy is required involves consideration of evidence of active change in the hyperplastic condyle or radiographic or clinical suggestions of pathologic conditions such as chondroma, osteoma, or other neoplasm that may warrant tissue diagnosis. Osteochondroma or osteoma mimics condylar hyperplasia, however, these pathologies show an asymmetric condylar growth on radiograph also they occur later in life than condylar hyperplasia. Condylectomy [30] not only restores symmetry in such cases, but also allows histological examination of the tumor mass. When neoplasia is not suspected, performing unilateral ramus surgery will shorten the affected ramus just as condylectomy does and will also restore symmetry. If a condyle is mature and stable, with normal function and cessation of growth an osteotomy to shorten the ramus is indicated. Thus, a slightly enlarged condyle that functions normally is left intact, and it may later remodel. It has been concluded by Lippold et al. [11] that condylectomy can correct hemimandibular hyperplasia, even in patients with active condylar growth, by removing the underlying disease.
If growth has stopped, orthodontics and surgical mandibular repositioning are indicated. If the height of the mandibular body is greatly increased, facial symmetry can be further improved by reducing the inferior border.
Traditionally, bilateral mandibular ramus osteotomy have been performed for treatment of the facial deformity in cases without abnormally high growth activity. In the simpler types, an osteotomy on one side of the mandibular ramus alone suffices to restore occlusion and symmetry whereas in the fully developed condition with dentally compensated unilateral condylar hyperplasia and maxillary cant, spatial correction is required with a Lefort Osteotomy.
Zhonghua [30] investigated the temporomandibular joint (TMJ) function of the condylar hyperplasia patients after condylectomy on twelve patients and examined the Fricton’s Craniomandibular Index (CMI) to assess the functional disorder of TMJ. A dramatic improvement in facial asymmetry was noted after condylectomy. New cortex formed on the surface of the operated condyle, the TMJ function was improved. Hence Condylectomy was considered as an effective method to remedy facial asymmetry and, at the same time, improve the TMJ function of the condylar hyperplasia patients.
An intraoral technique vertico-sagittal ramus osteotomy has been discussed by Choung [31] to reduce high condylar process fractures and to recontour hyperplastic condyles while simultaneously correcting the malocclusion. This method is considered useful particularly to treat vertical discrepancies associated with the hyperplastic or hypoplastic condyle. Condylar reconstruction by oblique sliding vertical-ramus osteotomy in cases of condylar hyperplasia after condylectomy has been described [32]. Wolford [26, 27] studied and showed that patients with active condylar hyperplasia, treated with high condylectomy, articular disc repositioning, and orthognathic surgery of single or both jaws have stable, predictable outcomes compared with those treated with orthognathic surgery alone. However, some authors have advocated orthognathic surgery alone as a treatment modality for hemi-mandibular hyperplasia so as not to disturb the TMJ anatomy.
It is a significant finding that in most patients with this anomaly, the mandibular arch form remains approximately symmetric with the maxillary arch, and there is no major compensatory alveolar modifications, and that except for the condylar enlargement and increased length of the condylar neck causing deviation of the mandible and chin to the opposite side and cross-bite, the general contour of the displaced mandible is symmetric. Pre-surgical orthodontic treatment [25] is some time needed is used to worsen the dental midline shift to allow greater osseous movements. Post-surgical orthodontics is offered to the patients if an ideal occlusion is desired, and when skeletal and dental studies do not mandate orthodontic treatment pre-surgically.
Footnotes
This paper discusses the various modalities of treatment for condylar hyperplasia.
References
- 1.Motamedi MH. Treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg. 1996;54(10):1161–1169. doi: 10.1016/S0278-2391(96)90341-9. [DOI] [PubMed] [Google Scholar]
- 2.Gottleib O. Hyperplasia of the mandibular condyle. J Oral Surg. 1951;9(2):118–135. [PubMed] [Google Scholar]
- 3.Rowe NL. Aetiology, clinical features and treatment of mandibular deformity. Br Dent J. 1960;108:41–64. [Google Scholar]
- 4.Nitzan DW, Katsnelson A, Bermanis I, Brin I, Casap N. The clinical characteristics of condylar hyperplasia: experience with 61 patients. J Oral Maxillofac Surg. 2008;66(2):312–318. doi: 10.1016/j.joms.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 5.Götz W, Lehmann TS, Appel TR, Rath-Deschner B, Dettmeyer R, Luder HU, Reich RH, Jäger A. Distribution of insulin-like growth factors in condylar hyperplasia. Ann Anat. 2007;189(4):347–349. doi: 10.1016/j.aanat.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Yang J, Lignelli JL, Ruprecht A. Mirror image condylar hyperplasia in two siblings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):281–285. doi: 10.1016/j.tripleo.2003.08.027. [DOI] [PubMed] [Google Scholar]
- 7.Lineaweaver W, Vargervik K, Tomer BS, Ousterhout DK. Posttraumatic condylar hyperplasia. Ann Plast Surg. 1989;22(2):163–172. doi: 10.1097/00000637-198902000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Eales E, Jones ML, Sugar AW. Condylar hyperplasia causing progressive facial asymmetry during orthodontic treatment: a case report. Int J Pediatr Dent. 1993;3(3):145–150. doi: 10.1111/j.1365-263X.1993.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 9.Lannetti G, Cascone P, Belli E, Cordaro L. Condylar hyperplasia: cephalometric study, treatment planning, and surgical correction our experience. Oral Surg Oral Med Oral Pathol. 1989;68(6):673–681. doi: 10.1016/0030-4220(89)90154-0. [DOI] [PubMed] [Google Scholar]
- 10.Mutoh Y, Ohashi Y, Uchiyama N, Teradak K, Hanada K, Sasaki F. Three dimensional analysis of condylar hyperplasia with computed tomography. J Craniomaxillofac Surg. 1991;19:49. doi: 10.1016/s1010-5182(05)80606-7. [DOI] [PubMed] [Google Scholar]
- 11.Lippold C, Kruse-Losler B, Danesh G, Joos U, Meyer U. Treatment of hemimandibular hyperplasia: the biological basis of condylectomy. Br J Oral Maxillofac Surg. 2007;43(5):351–360. doi: 10.1016/j.bjoms.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Gray RJ, Sloan P, Quayle AA, Carter DH. Histopathological and scinitigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg. 1990;19(2):65–71. doi: 10.1016/S0901-5027(05)80196-1. [DOI] [PubMed] [Google Scholar]
- 13.Slootweg PJ, Muller H. Condylar hyperplasia. A clinico-pathological analysis of 22 cases. J Maxillofac Surg. 1986;14(4):209–214. doi: 10.1016/S0301-0503(86)80291-0. [DOI] [PubMed] [Google Scholar]
- 14.Eslami B, Behnia H, Javadi H, Khiabani KS, Saffar AS. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(6):711–717. doi: 10.1016/S1079-2104(03)00379-2. [DOI] [PubMed] [Google Scholar]
- 15.Chan WL, Carolan MG, Fernandes VB, Abbati DP. Planar versus SPECT imaging in the assessment of condylar growth. Nucl Med Commun. 2000;21(3):285–290. doi: 10.1097/00006231-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Saridin CP, Raijmakers P, Becking AG. Quantitative analysis of planar bone scintigraphy in patients with unilateral condylar hyperplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(2):259–263. doi: 10.1016/j.tripleo.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Dimonte M, Inchingolo F, Minonne A, Arditi G, Di Palma G. Bone SPECT in management of mandibular condyle hyperplasia. Report of a case and review of literature. Minerva Stomatol. 2004;53(5):281–285. [PubMed] [Google Scholar]
- 18.Pripatnanont P, Vittayakittipong P, Markmanee U, Thongmak S, Yipintsoi T. The use of SPECT to evaluate growth cessation of the mandible in unilateral condylar hyperplasia. Int J Oral Maxillofac Surg. 2005;34(4):364–368. doi: 10.1016/j.ijom.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Hodder SC, Rees JI, Oliver TB, Facey PE, Sugar AW. SPECT bone scintigraphy in the diagnosis and management of mandibular condylar hyperplasia. Br J Oral Maxillofac Surg. 2000;38(2):87–93. doi: 10.1054/bjom.1999.0209. [DOI] [PubMed] [Google Scholar]
- 20.Silvestri A, Incisivo V, Mariani G. Treatment of mandibular condylar hyperplasia in developmental age. Clinical case. Minerva Stomatol. 2000;49(10):501–510. [PubMed] [Google Scholar]
- 21.Robinson PD, Harris K, Coghlan KC, Altman K. Bone scans and the timing for treatment of condylar hyperplasia. Int J Oral Maxillofac Surg. 1990;19(4):243–246. doi: 10.1016/S0901-5027(05)80402-3. [DOI] [PubMed] [Google Scholar]
- 22.Pogrel MA. Quantitative assessment of isotope activity in the temporomandibular joint regions as a means of assessing unilateral condylar hypertrophy. Oral Surg Oral Med Oral Pathol. 1985;60(1):15–17. doi: 10.1016/0030-4220(85)90206-3. [DOI] [PubMed] [Google Scholar]
- 23.Colin Liew, Hosseini H, Hussein Z, Goddard R, Wong WL, Bounds G. PET scan in the assessment and management of condylar hyperplasia. Br J Oral Maxillofac Surg. 2007;45(7):e60. doi: 10.1016/j.bjoms.2007.07.092. [DOI] [Google Scholar]
- 24.Hampf G, Tasanen A, Nordling S. Surgery in mandibular condylar hyperplasia. J Maxillofac Surg. 1985;13(2):74–78. doi: 10.1016/S0301-0503(85)80020-5. [DOI] [PubMed] [Google Scholar]
- 25.Stephan Crank, Gray S, Sidebottom AJ. Condylar hyperplasia—review of treatment outcomes and suggested pathway for management. Br J Oral Maxillofac Surg. 2007;45(7):e60–e61. doi: 10.1016/j.bjoms.2007.07.094. [DOI] [Google Scholar]
- 26.Feldmann G, Linder AS, Rindler A, Soderstrom U. Orthodontic and surgical treatment of unilateral condylar hyperplasia during growth—a case report. Eur J Orthod. 1991;13(2):143–148. doi: 10.1093/ejo/13.2.143. [DOI] [PubMed] [Google Scholar]
- 27.Wolford LM, Mehra P, Reiche-Fischel O, Morales-Ryan CA, García-Morales P. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop. 2002;121(2):136–150. doi: 10.1067/mod.2002.118403. [DOI] [PubMed] [Google Scholar]
- 28.Wolford LM. Concomitant temporomandibular joint and orthognathic surgery. J Oral Maxillofac Surg. 2003;61(10):1198–1204. doi: 10.1016/S0278-2391(03)00682-7. [DOI] [PubMed] [Google Scholar]
- 29.Jagielak M, Tomasik D, Piekarczyk B, Piekarczyk J. Orthognatic surgery of condylar hyperplasia and other deformities disturbing facial symmetry. Int J Oral Maxillofac Surg. 2005;34(4):364–368. doi: 10.1016/j.ijom.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Long X, Yang XW, Li XD, Deng MH. Evaluation of temporomandibular joint function after condylectomy for condylar hyperplasia. Zhonghua Zheng Xing Wai Ke Za Zhi. 2006;22(3):175–179. [PubMed] [Google Scholar]
- 31.Choung PH, Nam IW. An intraoral approach to treatment of condylar hyperplasia or high condylar process fractures using the intraoral vertico-sagittal ramus osteotomy. J Oral Maxillofac Surg. 1998;56(5):563–570. doi: 10.1016/S0278-2391(98)90452-9. [DOI] [PubMed] [Google Scholar]
- 32.Martinez-Lage JL, Gonzalez J, Pineda A, Alvarez I. Condylar reconstruction by oblique sliding vertical-ramus osteotomy. J Craniomaxillofac Surg. 2004;32(3):155–160. doi: 10.1016/j.jcms.2003.12.006. [DOI] [PubMed] [Google Scholar]