Abstract
Interaction between human and animals has increased in recent time regarding the fight for habitats. Animal inflicted injuries are mostly associated with the soft tissue injury and facial fractures. As literature has documented, this type of injuries are most commonly seen in rural communities. This article discusses a report a case of soft tissue injury associated with mandibular fracture undisplaced cervical spine fracture and review cases reported in the literature.
Keywords: Wild boar, Facial injury, Animal attack
Introduction
Man animal conflicts have increased nowadays as a result of fight for food and habitat. Dog bites are the most common animal bite, but, injuries from other animals such as cats, camel, cows, horses, pigs, and donkeys have also been reported [1].
The current report describes a case of wild boar injury. Wild boars are native to the jungles of India, the extension of human habitat into the forests causes ferocious attack. The tusks of the boar usually deep soft tissue injuries as well as fracture of the mandible.
Case Report
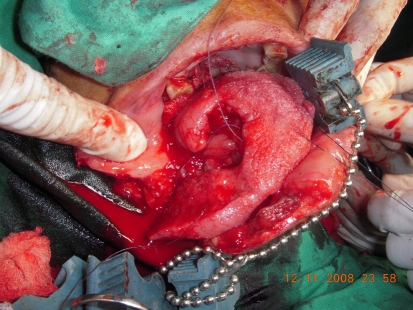
A 65 year old female reported to Oral and Maxillofacial Surgery department of the college with a chief complaint of pain and swelling on right side of face with history of attack by a wild boar two days back while working in the farm. Patient was rendered primary treatment in the primary health care centre in vicinity; the lacerated wound on face and chest were sutured and was referred to our institute for further management. Examination revealed lacerated wound on the right cheek and neck which was sutured primarily (Fig. 1). The lacerated tongue was debrided with the hydrogen peroxide and normal saline. The patient was admitted and started with amoxicillin with clavulanic acid and continued for 5 days. Amoxicillin with clavulanic acid is active against virtually all the bacteria isolated from bite wounds and seems to be the optimal antimicrobial treatment [3].
Fig. 1.
Showing sutured laceration wound primarily
The patient’s occlusion was disturbed and step deformity was palpated on inferior border of mandible on right side.
There was diffuse swelling on right side of face with circumorbital ecchymosis, subconjunctival hemorrhage, lacerated tongue on right side (Fig. 1) and the Coleman’s sign was positive.
Fig. 2.
Tongue lacerations
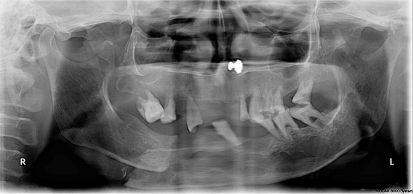
A panoramic radiograph showed the overriding right mandibular body fracture with low level subcondylar fracture extending from coronoid process to posterior border of ramus (Fig. 3). In addition to this CT revealed undisplaced fracture of the sixth cervical vertebra. The patient was decided to be taken up for open reduction of the mandibular fracture under general anesthesia, while taking care of the cervical fracture.
Fig. 3.
OPG (overriding right mandibular body fracture with low level subcondylar fracture)
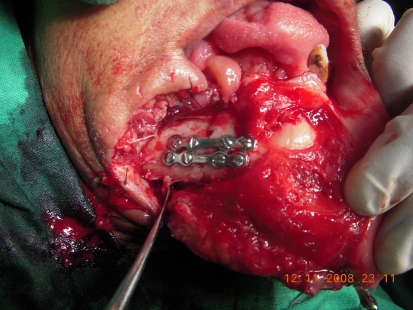
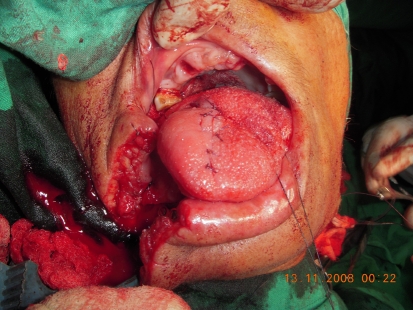
Rigid internal fixation of fracture mandible on right body and left subcondylar region was carried out (Fig. 4). Edges of the laceration on cheek, chest and tongue were debrided, freshened and sutured (Fig. 5). She was advised to wear soft cervical collar for the undisplaced C6 vertebral fracture. Postoperative recovery was uneventful (Fig. 6).
Fig. 4.
Rigid internal fixation
Fig. 5.
Laceration of the tongue freshened and sutured
Fig. 6.

Postoperative photograph
Discussion
In developing country like India many people depend on farming for their daily needs. Patient in the reported case was attacked by the wild boar while working in farm [1–3]. Our patient had lacerated lip tongue and wound on thorax. Injuries caused by animals commonly affect the upper extremities, especially the hands [1, 4]. On the face, the predominant sites are the lips, chin, nose, and auricles [1, 4]. Involvement of the head, face, and neck is seen in 9–33% of cases and majority of victims are children [1, 4]. According to Lackmann’s classification of severity of bite our patient falls under stage IVB as there were extensive injury with muscle involvement and bony involvement [3, 5]. Lackmann’s classification helps to render the treatment according to the severity of the bite (Table 1).
Table 1.
Lackmann’s Classification. Severity of bite wound on the face and head
| Stage | Clinical appearance |
|---|---|
| I | Superficial injury without involvement of muscle |
| II | Deep injury with involvement of muscle |
| III | Deep injury with involvement of muscle and tissue defect |
| IVA | Stage III in combination with vascular nerve injury |
| IVB | Stage III in combination with bony involvement or organ defect. |
Facial fractures are rare in animal-related incidents [1, 6]. In our case, the moderate size of the animal involved and the force of impact, coupled with age of the patient are probably responsible for the bony injuries sustained.
In the treatment of animal bite wounds on the face and head, it is important both to avoid infection and to achieve an aesthetically pleasing result.
While most reports are in agreement on the need for immediate and thorough wound irrigation, there is still no accord on the timing of subsequent treatment with regards to wound debridement, primary, and secondary repair, or the routine use of prophylactic antibiotics. Antibiotic prophylaxis after the bite is obligatory for all wounds of Lackmann class II and more. Antibiotic prophylaxis should be continued for at least 5 days [3].
The most frequently associated aerobic bacteria are alpha and beta hemolytic Streptococci, S. aureus, S. epidermis, E. coli, Pseudomonas and anaerobic bacteria includes Bacteroides, Prevotella, Fusobacterium species [2, 4, 7]. In our case soft tissue wounds and fractures were regarded as contaminated, so patient was given tetanus vaccine and broad-spectrum antibiotic coverage irrespective of the interval between injury and presentation for treatment [1]. Mandibular fracture was treated with open reduction and rigid internal fixation access was gained through the same existing laceration.
Satisfactory results were recorded by debridement, irrigation, primary closure with reduction and stabilization simultaneously with use of cervical collar for c-spine injury.
References
- 1.Ugboko VI, Olasoji HO, et al. Facial injuries caused by animals in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40(5):433–437. [PubMed] [Google Scholar]
- 2.Ogunbedede EO, Arotiba JT. Camel bite injury of the orofacial region: report of a case. J Oral Maxillofac Surg. 1997;55(10):1174–1176. doi: 10.1016/S0278-2391(97)90303-7. [DOI] [PubMed] [Google Scholar]
- 3.Kesting MR, Holzle F, Pox C, Thurmuller P, Wolff KD. Animal bite injuries to head: 132 cases. Br J Oral Maxillofac Surg. 2006;44(3):235–239. doi: 10.1016/j.bjoms.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham L, Fonda JR, Robinson G, Richard H. Management of human and animal bites. In: Fonseca RJ, Walker RV, Betts NJ, editors. Oral and maxillofacial trauma. 3. St. Louis: Saunders; 2005. pp. 843–862. [Google Scholar]
- 5.Wolff KD. Management of animal bite injuries of the face: experience with 94 patients. J Oral Maxillofac Surg. 1998;56(7):838–843. doi: 10.1016/S0278-2391(98)90009-X. [DOI] [PubMed] [Google Scholar]
- 6.Robert G. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31(2):51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 7.Haug RH. The changing microbiology of maxillofacial infections. Oral Maxillofac Surg Clin North Am. 2003;15(1):1–15. doi: 10.1016/S1042-3699(02)00076-6. [DOI] [PubMed] [Google Scholar]