Abstract
Objective
Purpose of this study to introduce a new minimal access technique for management of anterior mandible fracture with several advantages over conventional methods.
Method
Four cases of undisplaced anterior mandibular fracture were selected. Tension band was achieved either by arch bar fixation to mandible or placement of interdental wire followed by intermaxillary fixation. With a 1 cm vertical incision was placed adjacent to fractured line. Fractured segment was immobilized with lag screw with minimal stripping. All patients were followed for 6 months.
Results
All four cases shown good stable segment after 6 months of post operative follow up. OPG revealed well placed lag screw and there were no surgical complications, for example parasthesia, scarring and odema.
Conclusion
Fixation of anterior mandible fracture using this technique can achieve good stability and appropriate compression. The technique is simple and easily performed, reducing the surgical time, reduce the chances of infection due to less exposure and promote the healing process by producing stress in the fracture lines.
Keywords: Anterior mandible fracture, Lag screw, Minimal access technique
Introduction
Fracture of anterior mandible fracture may be treated by various techniques that follow the standard principles of open reduction and internal fixation with either plates and screws or lag screws. Lag screw osteosynthesis of anterior mandibular fractures is a sensitive, facile, predictable, and relatively inexpensive method for internal fixation of indicated fractures [1]. A modification of traditional method of lag screw fixation is proposed following the principle of minimal access surgery with potential advantages, which include shorter time, more economical, decreased morbidity, and early improvement in functional rehabilitation due to the less traumatic procedure.
Indications, Contraindications and Preoperative Assessment
This technique is indicated for any favorable linear fracture in the anterior mandible. These include sagittal fractures with split buccal and lingual cortical plates of the mandible, vertically oriented fractures, and short oblique fractures with sufficient access along the curve of the anterior mandible for screw placement. Contraindications include unfavourable fracture patterns (long oblique comminuted, flat mandibular plane), poor dental support for the tension band, inability to determine the fracture pattern preoperatively and operator inexperience.
Clinical experience has demonstrated that the fracture site becomes filled with blood clot and soft tissue within 24 h after the injury. This interfragmentary debris interrupts the anatomical reduction of fractured bony segments. Wide exposure of the fracture site allows the surgeon to facilitate the anatomic reduction by distracting the fractured segments and debriding the fracture site. This is impossible with the technique described above and, therefore, an advantage in achieving a satisfactory reduction is provided by early (<48 h) surgical intervention wherever possible. Important parameters include fracture location, degree of comminution, a condition of occluding dentition, and timing of repair. Accurate radiographic interpretation of fracture pattern is very important and may be obtained with an orthopantomograph or occlusal mandibular view. Location of mental foramen and space availability between apices of the teeth and lower border of the mandible should be assessed.
Technique
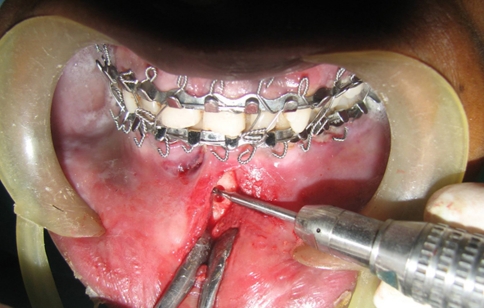
Application of this technique relies on a tension band principle. Tension band can be achieved either by arch bar fixation to mandible or placement of interdental wire and resistance of intercusp relationship of teeth after intermaxillary fixation. A minimally displaced mandibular symphysis fracture case was selected (Fig. 1) and premorbid occlusion was restored with intermaxillary fixation. A 1 cm long incision was made at the previously anticipated location (Fig. 2). A minimum amount of periosteal stripping was performed to drill the cortex.
Fig. 1.
Minimally displaced mandibular symphysis fracture
Fig. 2.
Arch bar placed as tension band and intermaxillary fixation achieved. One centimeter vertical incision placed adjacent to fracture line
Drilling the cortex is the most important step in this technique. Two factors should be taken into consideration, the point and angulation of drill. Point of drill should be equidistant from fracture line so that the threaded part of the screw engages the other fragment and produces static interfragmentary compression and satisfactory fixation of the fracture. Angulation and depth must be in such ways that drill should not breach the lingual cortex beyond its limit.
A gliding hole was created and drill was performed just 2 mm below the apices of anterior teeth (Fig. 3), a 20 mm lag screw was placed (Fig. 4), while placing the lag screw digital pressure was applied for counter force. Second drill was made above the lower border of the mandible and same length lag screw was placed. A single screw is sufficient for fixation, although the second screw can also be placed with slight extension of incision in selected cases.
Fig. 3.
Gliding hole is created and drilling is in progress
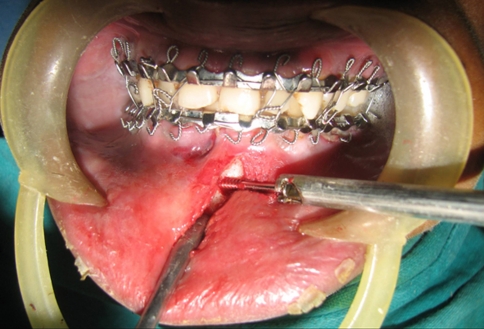
Fig. 4.
Lag screw insertion
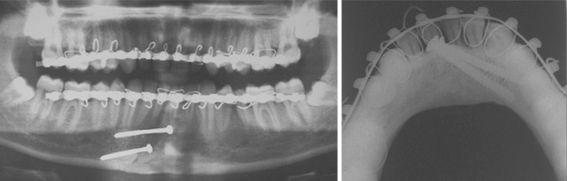
The mandible was released from intermaxillary fixation, and occlusion was checked. The incision was closed with absorbable sutures. Post operative orthopantomograph and mandible occlusal radiograph was taken to confirm the position of lag screws (Fig. 5). This technique was performed in three more cases (Figs. 6, 7, 8). On post operative follow up, no patient complained of malocclusion and sensory disturbance and intraoral scarring was minimal.
Fig. 5.
Postoperative OPG (left) and occlusal view (right) confirms the position of lag screws
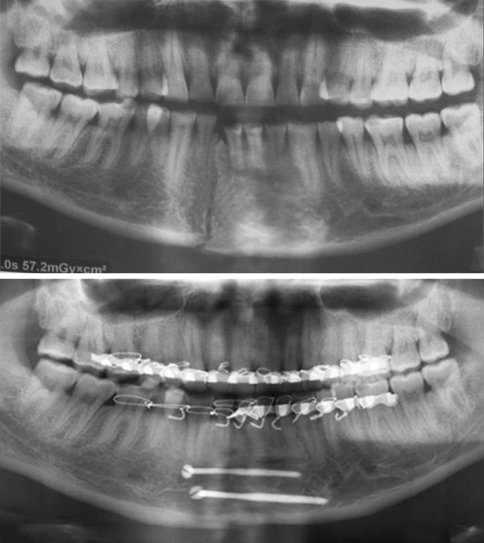
Fig. 6.
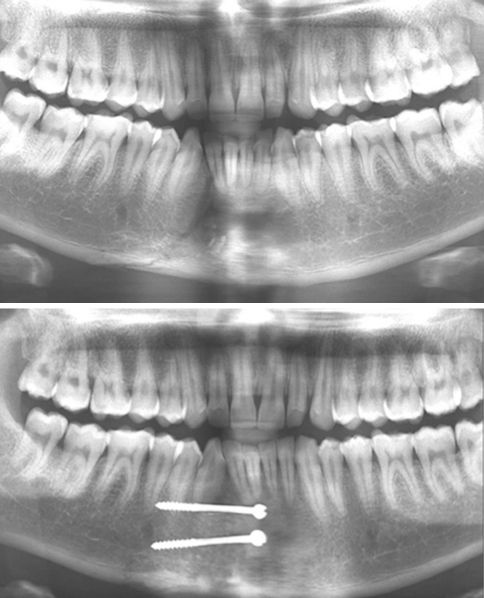
Case 2: OPG reveals right parasymphysis fracture of mandible (above) and 1 month postoperative OPG (below)
Fig. 7.
Case 3: OPG reveals right parasymphysis fracture of mandible (above) and 6 months postoperative OPG (below)
Fig. 8.
Case 4: OPG reveals right parasymphysis fracture of mandible (above) and 6 months postoperative OPG (below)
The complications of this technique include breakage of the drill, malocclusion, and lingual cortex breach. Only one complication was encountered in second case where two lag screws were used for fixation. The lower lag screw breached the lingual cortex due to wrong angulation during drilling (Fig. 9). Lag screw was removed and redirected with proper angulation and again placed into the newly drilled area. Position of the screw confirmed with mandible occlusal radiograph.
Fig. 9.
Occlusal radiographs shows lingual cortex breach (left) and lag screw was removed and redirected to correct position (right)
Discussion
The development of the different systems for internal fixation of facial trauma and their application in the treatment of mandibular fractures has meant a change in the criteria for postsurgical immobilization. It has also made possible a more rapid return of function, resulting in the patient being able to resume his or her normal life earlier.
There are different systems of internal mandibular fixation, each of which is based on specific principles that reflect one philosophy of treatment. The 2 mm miniplate system originated from the work of Champy et al [2]. The A0 (Arbeitsgemeinschaft fur Osteosynthesefragen) is based on a diametrically opposite approach to treatment. An alternative to the plate and screw system is osteosynthesis using only lag screws. It has been shown that mandibular fractures in both the anterior and angle regions can be successfully treated using metal screws [3]. Ellis and Ghali [4] found lag screw fixation of anterior mandibular fractures to be an extremely simple and successful means of rigidly securing bone segments. With lag screw osteosynthesis the screw glides freely through the cortex of the near fragment and engages the cortex of the far fragment with its threads. When tightened, it draws the fragments together and compresses their surfaces. Compression is facilitated by countersinking the external cortex of the head of the screw [4]. Each of these procedures has its defenders and detractors, and there are those who advocate for the almost unlimited potential for each of them, but with contradictory results.
However, these techniques require large degloving incision at the anterior mandible and subperiosteal stripping of tissue to facilitate implant placement that may lead to various postoperative sequelae e.g. increase risk of blood loss due to wide incision, lower lip muscle dysfunction, difficulty with oral hygiene and nutrition, devascularization of bone segments, injury to mental nerve and postoperative swelling.
Development of minimal access and endoscopic repair of facial fractures is new and evolving technique that offers the potential for reduced patient morbidity and operating time, as well as quicker patient recovery. Current applications include the management of orbital blow-out, frontal sinus, zygomatic arch, and subcondylar fractures. It should be emphasized that endoscopy augments, rather than replaces, the ‘time tested’ principles of adequate skeletal exposure, accurate fracture reduction, and appropriate internal fixation [6]. Very few large studies of endoscopic fracture repair exist. The current literature, however, suggests that, when compared with an open approach, smaller endoscopic incisions result in reduced patient morbidity with similar outcomes [5]. This article describes a technique that combines minimal access surgery with the benefits of open reduction and internal fixation to anterior mandible fracture.
Similar minimal access technique has been described in literature by Forrest and Christopher [5] in 1999. In their technique, they used two incisions equidistant from fracture line in the anterior mandible to facilitate the compression of bony fragments using towel clip while in lag screw placement, we used a single incision in our technique, keeping two points—(a) This technique is indicated in undisplaced linear fracture where there are fewer chances of flaring of segments. (b) Proper application of arch bar or interdental wiring as a tension band and resistance of inter cusp relationship of teeth after intermaxillary fixation obviates the application of compression of bony segments. If required we may apply digital pressure during screw placement. In the real sense, our technique is the modification of Forrest’s technique with the single incision to get more advantages.
A small single incision in our technique has potential advantages over the traditional methods that include less postoperative scarring and swelling, improved dental hygiene, faster recovery, decrease chances of injury to mental nerve, maintenance of vascular supply of bone fragments, fewer amounts of implant material, and a decrease operative time.
Technical complications with this technique are breakage of the drill bit and lingual cortex breach. Drill bit breakage usually occurs due to forceful drilling and change in angulation ones it is in the cortex. Lingual cortex breach occurs because of over drilling the cortices and wrong direction. We experienced breach of lingual cortex in our second presented case. This was confirmed by an occlusal radiograph, which is very useful in our technique. A postoperative occlusal view shows accurate positioning of lag screws. The lag screw was removed, and drilling was repeated with calculated depth and proper orientation and replacement of the lag screw. The technique described herein relies on precise diagnosis and assessment of the fracture pattern to arrive at the choice of fixation technique. Inadequate radiologic visualization and inaccurate assessment of the nature of the fracture may result in sub optimal fixation, displacement, and postoperative malocclusion.
Conclusion
Fixation of anterior mandible fracture using this technique can achieve good stability and appropriate compression. The technique is simple and easily performed, reducing the surgical time, reduce the chances of infection due to less exposure and promote the healing process by producing stress in the fracture lines. The case selection and careful instrumentation are major factors for consideration. It is hoped that this technique will decrease the morbidity associated with traditional methods but at the same time maintained the standard of care associated with internal fixation techniques.
References
- 1.Tiwana PS, Kushner GM, Alpert B. Lag screw fixation of anterior mandibular fractures: a retrospective analysis of intraoperative and postoperative complications. J Oral Maxillofac Surg. 2007;65:1180–1185. doi: 10.1016/j.joms.2006.11.046. [DOI] [PubMed] [Google Scholar]
- 2.Champy M, Lodde JP, Schmit R. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978;6:14. doi: 10.1016/S0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 3.Niederdellmann H, Shetty V. Solitary lag screw osteosynthesis in the treatment of fractures of the angle of mandible: a retrospective study. Plast Reconstr Surg. 1987;80:688. doi: 10.1097/00006534-198707000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Ellis E, Ghali GE. Lag screw fixation of anterior mandibular fractures. J Oral Maxillofac Surg. 1991;49:13–21. doi: 10.1016/0278-2391(91)90259-O. [DOI] [PubMed] [Google Scholar]
- 5.Forrest CR. Application of minimal-access techniques in lag screw fixation of fractures of the anterior mandible. Plast Reconstr Surg. 1999;104:2127–2134. doi: 10.1097/00006534-199912000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Pham AM, Strong EB. Endoscopic management of facial fractures. Curr Opin Otolaryngol Head Neck Surg. 2006;14:234–241. doi: 10.1097/01.moo.0000233593.84175.6e. [DOI] [PubMed] [Google Scholar]