Abstract
Aim
The aim of this study was to clinically evaluate the outcomes of pterygoid disjunction (PD) carried out as the primary treatment modality for reducing disc displacement type of internal derangement (ID) of temporomandibular joint (TMJ) refractory to conservative management and arthrocentesis.
Patients and Method
59 PD were carried out in 33 patients. In 26 cases procedure was done bilaterally and in 7 cases unilaterally as per the presentation from 2008 to 2010. Three patients were lost to follow up. Using the Helkimo Anamnestic and Clinical Dysfunction Indices cases were evaluated pre and postoperatively after 1 year.
Results
All 30 cases showed improvement. After 1 year follow up 6 cases were in Dio and 22 cases were in DiI and 2 cases were in DiII of clinical dysfunction index. From which we can co-relate that post surgically all the patients were benefited by this procedure.
Conclusion
PD as a primary surgical option significantly reduces pain and improves function in the refractory cases of reducing disc displacement type of ID of TMJ.
Keywords: Pterygoid disjunction, Reducing disc displacement, Internal derangement, Temporomandibular joint, Helkimo anamnestic index
Introduction
Treatment of patients with internal derangement (ID) of the temporomandibular joint (TMJ) typically begins with nonsurgical treatment modalities. Bite appliance therapy, diet modifications, non-steroidal anti-inflammatory medications, muscle relaxants, moist heat or ice, and physical therapy have been found to be efficacious. Surgical intervention in the cases of ID of TMJ is a controversial issue. It is generally contemplated in refractory cases not responding to conservative management [1, 2]. There are several surgical options, which include open operation (arthrotomy) or closed operation (arthroscopy or arthrocentesis). Though there are many clinical studies on the results of arthroscopy and arthrocentesis, which show their benefits and limitations, but arthroscopic instruments are not available in most of the institutes. Several open surgical techniques like discopexy or discectomy have been described, but there have been few studies of long-term results. In our case series PD was carried out in refractory cases of reducing disc displacement type of ID to return the patient to a regular diet, with some limitations, and to establish an adequate functional range of motion of mouth opening. The procedure is minimally invasive and preserves the articular tissue, it permits normalization and regeneration of synovium, and a restoration of the articular relations to permit the joint structures to adapt and function through an adequate range of motion [3].
Patients and Methods
All patients of MRI diagnosed reducing disc displacement type of ID refractory to conservative management such as bite appliance therapy, diet modifications, nonsteroidal anti-inflammatory medications, muscle relaxants, moist heat or ice, physical therapy and arthrocentesis prescribed at various service hospitals were included in the study. Patients on whom any type of open surgical procedure was performed were excluded from the study. All patients were evaluated before surgery and found to be in AiII index according to Helkimo anamnestic index (Table 1) [4]. All PD were performed by the same surgeon. 59 PD were carried out under general anaesthesia in 33 radiologically (Magnetic resonance imaging) and clinically diagnosed refractory cases of reducing disc displacement type of ID patients not responding to the conservative management (Figs. 1, 2, 3 and 4). In 26 cases procedure was done bilaterally and in 7 cases unilaterally as per the presentation from 2008 to 2010. 17 patients out of 33 were females and 16 were males. During the postoperative period limited mouth opening and soft diet was advised for 2 weeks. Thereafter active mouth opening exercises were carried out to achieve normal range of mouth opening. In active mouth opening patients were instructed to open until they perceive pain and then advised to hold for several seconds and repeat this exercise several times a day. An active lateral stretch permitting the contra lateral LPM to be stretched may be accomplished by visualizing themselves in a mirror. In the active protrusion, also performed in front of the mirror, the mandible is protruded forward stretching the LP bilaterally. All active excursions are maintained for several seconds and slowly released. All the cases were evaluated at 1, 3, 6, 12 months. Cases were analyzed using clinical dysfunction index (Tables 2, 3) postoperatively after 1 year. The position of the disc was assessed using MRI. The criteria for success are to return the patient to a regular diet, with some limitations, and to establish an adequate functional range of motion. The goal for surgical procedure included preservation of articular tissue to permit normalization and regeneration of synovium, and a restoration of the articular relations to permit the joint structures to adapt and function through an adequate range of motion.
Table 1.
Helkimo anamnestic index
| Index | Criteria |
|---|---|
| Ai0 | No symptoms from the masticatory index |
| AiI | TMJ sounds/tiredness in jaws/stiffness in the morning/stiffness on mandibular movements |
| AiII | Trismus/Locking/jaw “out of joint”/pain in TMJ region and masticatory musculature/pain on mandibular movement |
Fig. 1.
Reducing anteriorly displaced disc of left side on closed mouth position
Fig. 2.
Anteriorly displaced disc of left side in open mouth position
Fig. 3.
Reducing anteriorly displaced disc of right side on closed mouth position
Fig. 4.
Anteriorly displaced disc of right side in open mouth position
Table 2.
Helkimo clinical dysfunction index scoring criteria
| Score | Criteria |
|---|---|
| Mandibular mobility (opening, laterotrusive, protrusive) | |
| 0 | Normal range of movement (maximum opening >40 mm, maximum lateral excursion excursion/protrusion >7 mm) |
| 1 | Slightly impaired mobility (maximum opening 30–39 mm, maximum lateral excursion/protrusion 4–6 mm) |
| 5 | Severely impaired mobility (maximum opening <29 mm, maximum lateral excursion/protrusion <3 mm) |
| Symptom: impaired TMJ function | |
| 0 | Smooth movement without TMJ sounds and deviation on opening or closing movement <2 mm |
| 1 | Sounds in 1 or both joints and/or deviation >2 mm on opening or closing movements |
| 5 | Locking/and/or luxation of the TMJ |
| Symptom: muscle pain | |
| 0 | No tenderness to palpation in masticatory muscles |
| 1 | Tenderness to palpation in 1–3 palpation sites |
| 5 | Tenderness to palpation in ≥ 4 palpation sites |
| Symptom: TMJ pain | |
| 0 | No tenderness to palpation |
| 1 | Tenderness to palpation laterally |
| 5 | Tenderness to palpation posteriorly |
| Symptom: pain on movement of the mandible | |
| 0 | Pain on movement |
| 1 | Pain on 1 movement |
| 5 | Pain on ≥ 2 movements |
| Clinical dysfunction code: sum of A + B + C + D + E (0–25) | |
Table 3.
Helkimo clinical dysfunction index
| Code | Clinical dysfunction | Definition |
|---|---|---|
| 0 | Di0 | Clinically asymptomatic |
| 1–4 | DiI | Small dysfunction |
| 5–9 | DiII | Middle dysfunction |
| 10–25 | DiIII | Strong dysfunction |
Surgical Procedure
All procedures were performed under general anesthesia, by nasal endotracheal intubation. All patients received perioperative Ampicillin 500 mg and Hydrocortisone 100 mg intravenously. Intraoral zygomatic buttress was exposed using upper vestibular incision after infiltrating 4 ml of Lignocaine with adrenaline (1:80,000). PD was done using a pterygoid chisel (Fig. 5). Hemostasis was achieved before closure. Postoperatively patient received Inj. Diclofenac sodium 75 mg intramuscularly and Inj. Dexamethasone 4 mg intravenously for 5 days.
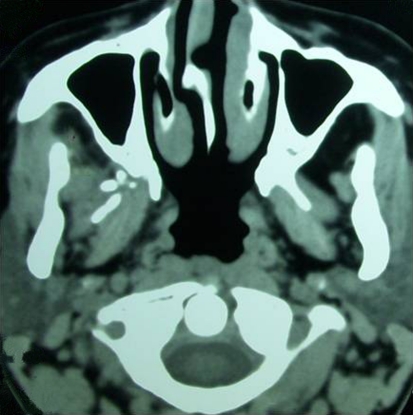
Fig. 5.
Pterygoid disjunction on axial section
Results
All 33 patients were in Anamnestic index AII (Trismus/Locking/jaw “out of joint”/pain in TMJ region and masticatory musculature/pain on mandibular movement) before surgery. 3 cases were lost to follow up. Rest of the cases were evaluated at 1, 3, 6, 12 months. Position of the disc was evaluated after 1 year. Normal range of mandibular movement was found in 07 cases. In 13 cases smooth movement without TMJ sounds was achieved. Muscle pain was completely relieved in 6 cases. In 9 cases tenderness was there in TMJ on palpation laterally. Pain on movement was still there in 7 cases. Reducing disc displacement was still present in 2 cases. Stable disc reduction was found in 28 cases (Figs. 6, 7, 8 and 9). Each patient indicated that they experienced subjective improvement in their preoperative pain and dysfunction. Overall 06 cases were in Dio and 22 cases were in DiI and 2 cases were in DiII of clinical dysfunction index (Table 4).
Fig. 6.
Stable disc reduction on left side on closed mouth
Fig. 7.
Stable disc reduction on left side on open mouth
Fig. 8.
Stable disc reduction on right side on closed mouth
Fig. 9.
Stable disc reduction on right side on open mouth
Table 4.
Data of patients
| No. | Age/Sex | Side | AI | Follow up (years) | Mandibular mobility | TMJ function | Muscle pain | TMJ pain | Pain with movement | Clinical dysfunction score | Clinical dysfunction index | Stable disc reduction (1 year) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | M/48 | R & L | AiII | 2 | 0 | 0 | 1 | 0 | 0 | 1 | DiI | Yes |
| 2. | M/54 | R | AiII | 2 | 1 | 0 | 1 | 0 | 0 | 2 | DiI | Yes |
| 3. | F/36 | R | AiII | 2 | 1 | 0 | 1 | 0 | 0 | 2 | DiI | Yes |
| 4. | F/34 | R & L | AiII | 2 | 1 | 0 | 1 | 0 | 0 | 2 | DiI | Yes |
| 5. | F/37 | R | AiII | 2 | 1 | 0 | 1 | 0 | 0 | 2 | DiI | Yes |
| 6. | M/29 | R & L | AiII | 2 | 1 | 0 | 2 | 0 | 0 | 3 | DiI | Yes |
| 7. | M/27 | L | AiII | 2 | 1 | 0 | 1 | 0 | 0 | 2 | DiI | Yes |
| 8. | M/34 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 0 | 3 | DiI | Yes |
| 9. | M/36 | R & L | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 10. | M/47 | L | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 11. | M/53 | R | AiII | – | – | – | – | – | – | – | – | – |
| 12. | F/54 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 1 | 4 | DiI | Yes |
| 13. | F/56 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 1 | 4 | DiI | Yes |
| 14. | F/29 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 1 | 4 | DiI | Yes |
| 15. | M/47 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 1 | 4 | DiI | Yes |
| 16. | F/42 | R & L | AiII | – | – | – | – | – | – | – | – | – |
| 17. | F/43 | L | AiII | 2 | 1 | 1 | 1 | 0 | 0 | 3 | DiI | Yes |
| 18. | M/48 | L | AiII | 2 | 1 | 1 | 1 | 0 | 0 | 3 | DiI | Yes |
| 19. | F/26 | R & L | AiII | – | – | – | – | – | – | – | – | – |
| 20. | F/23 | R | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 21. | F/41 | R & L | AiII | 2 | 1 | 1 | 1 | 0 | 1 | 4 | DiI | Yes |
| 22. | M/29 | R | AiII | 2 | 5 | 1 | 1 | 1 | 1 | 9 | DiII | No |
| 23. | M/34 | L | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 24. | F/32 | R & L | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 25. | M/26 | R & L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 26. | F/28 | R & L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 27. | F/29 | R & L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 28. | M/24 | R & L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 29. | M/35 | L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 30. | F/34 | L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 31. | F/37 | L | AiII | 2 | 1 | 1 | 1 | 1 | 0 | 4 | DiI | Yes |
| 32. | F/32 | R | AiII | 2 | 0 | 0 | 0 | 0 | 0 | 0 | DiO | Yes |
| 33. | M/56 | R | AiII | 2 | 5 | 1 | 1 | 1 | 1 | 9 | DiII | No |
Discussion
The management of ID of TMJ starts with conservative modalities, failing which surgical procedures may be resorted to. In opting for surgical management, each patient needs to be reviewed on a case-to-case basis and objectives planned individually. The success of the procedure is not related to achieving a finite mouth opening in each case, and the aim of management is to enable a patient to return to a regular diet, with some limitations, and to establish an adequate functional range of motion. The indices of surgical outcomes should rather be based on patient’s response to therapy according to whether the patient feels there has been a total eradication, significant reduction, or minimal reduction of his or her complaints, or no change or worsening of the condition. For most patients, the primary concern is the facial pain and they are satisfied with limited mouth opening if adequate relief of pain is achieved. Additional magnetic resonance and arthroscopic information about the structure and function of the joint in health and disease is needed to establish reliable indicators and predictors of surgical outcome [5].
Any surgical intervention should aim at preservation of articular tissue to permit normalization and regeneration of synovium, and a restoration of the articular relations to permit the joint structures to adapt and function through an adequate range of motion. The joint function may be asymptomatic and satisfactory in the presence of various types of ID. Repositioning the disk is recommended in the patient with minimal changes in the joint structures, in which symptoms have persisted despite nonsurgical and arthroscopic intervention [6]. This may not be the appropriate modality in all cases especially when the disk is so severely damaged as to be incapable of healing; which is a rare occurrence. In such instances, removing the disk would be preferred [7].
Several surgical procedures have been reported with good results in the management of ID of TMJ. The basic difference has been degree of invasiveness of the procedure. The therapeutic principle of arthrocentesis and arthroscopic intervention appears to be similar [5]. Open surgical approaches to TMJ internal derangements are now resorted to following nonsurgical therapy and arthrocentesis/arthroscopy for most conditions and in treatment of certain mechanical conditions directly attributed to a disk obstruction. The age-old arthrocentesis with and without steroid injection, a procedure commonly performed by many surgeons in yester years, has become a mainstay for treatment but most of the institutes lack the facility of arthroscopic instruments. We concluded from our results that PD is the least invasive procedure for reducing disc displacement type of ID of TMJ refractory to conservative management and arthrocentesis.
Conflict of interest
None declared.
References
- 1.Alpaslan C, Kahraman S, Güner B, Cula S. Does the use of soft or hard splints affect the short-term outcome of temporomandibular joint arthrocentesis? Int J Oral Maxillofal Surg. 2008;37(5):424–427. doi: 10.1016/j.ijom.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 2.Mercuri LG. Internal derangement outcomes reporting. J Oral Maxillofac Surg. 2010;68(6):1455. doi: 10.1016/j.joms.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 3.Varghese M, George A, Keshava PY, Puthanveedu RK. Pterygoid plate disjunction: minimally invasive treatment for internal derangement of the temporomandibular joint. Asian J Oral Maxillofac Surg. 2005;17:247–255. [Google Scholar]
- 4.Helkimo M. Studies on function and dysfunction of the masticatory system. Sven Tandlak Tidskr. 1974;67:165. [PubMed] [Google Scholar]
- 5.Naveen C, Chhabra S, Kumar YR. Use of a calibrated beaker in TMJ arthrocentesis. B J Oral Maxillofac Surg. 2009;47(4):329–330. doi: 10.1016/j.bjoms.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Abramowitz Shelly M, Dolwick F. 20-Year follow-up study of disc repositioning surgery for temporomandibular joint internal derangement. J Oral Maxillofac Surg. 2010;68(2):239–242. doi: 10.1016/j.joms.2009.09.051. [DOI] [PubMed] [Google Scholar]
- 7.Miloro M, Henriksen B. Discectomy as the primary surgical option for internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 2010;68(4):782–789. doi: 10.1016/j.joms.2009.09.091. [DOI] [PubMed] [Google Scholar]