Abstract
Hemimasticatory spasm is a rare neuromuscular disorder where the patient experiences involuntary, painful spasm of muscles of mastication. Only 15 cases have been reported in literature. We present a case which was treated unconventionally with satisfactory outcome.
Keywords: Hemimassetric spasm, Masseter, Botulinum, Masseter stripping
Introduction
Hemimasticatory spasm is a rare neurologic disorder of muscles of mastication affecting on one side of the face [1]. It was first described by Gowers [2], who named it as ‘masticatory spasm of Romberg’. In the scientific literature only 15 cases have been reported. Almost all of these cases have been treated using botulinum toxin with favourable outcome. We present a case of hemimasticatory spasm which was managed surgically.
Case Report
A 38-year-old laborer reported to our OPD with a complaint of severe pain and spasm on the right side of his face associated with inability to open mouth since 6 months. History revealed that he was apparently asymptomatic 6 months back when he developed mild, painful involuntary twitching on right side of the face lasting a few seconds. Initially occurring three to four times a day the duration and frequency increased over time. The intensity also increased with time and was soon associated with severe pain on the affected side. At the time of reporting he gave a history of spasms occurring almost throughout the day, each episode lasting 5–15 seconds but at times lasting up to 30 seconds. During the spasm the patient was not able to open his mouth, speak or his routine activities. The spasm was characteristically absent during sleep. He gave no history of any previous ailment or injury for which he had to seek medical attention. He was a chronic smoker and tobacco chewer for the past 20 years.
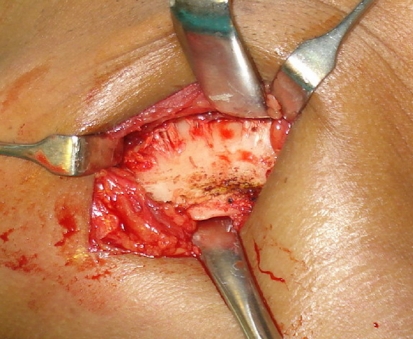
On examination the patient had an asymmetric face with hypertrophy of the masseter on right side (Figs. 1, 2). The spasm began spontaneously over the region of right masseter and temporalis muscles as brief twitches and gradually increased in intensity and would stop abruptly (Fig. 3). The patient winced with pain during the episode and would press his palm against his face to get relief. After a brief duration the spasm would recur. At times light tapping of the skin over the region also evoked these spasms. During these spasm the muscles of facial expression were not involved and blink reflex was normal. There was no regularity in both the intensity and duration. Neurosensory and motor examination of the face revealed no abnormalities in the cranial nerves. Mouth opening was 45 mm and mandible showed normal movements. Based on the clinical findings the patient was diagnosed as hemimasticatory spasm [HMS]. However because of unavailability of EMG we could not ratify our diagnosis. Injection Botulinum toxin can be given for a duration of 6 months. Since the patient could not afford the treatment. Debulking and stripping of the muscle fibers surgically. Patient was explained the procedure and consent was obtained. Under GA Risdon’s incision was placed and masseter muscle was exposed. Debulking of the muscle was carried out by stripping middle and deep fibers and muscle was left to reattach itself (Fig. 4). Postoperatively the patient recovered uneventfully and showed no signs of spasm. Patient was followed up for 1 year. There was no signs of recurrences. There was no difficulty in mastication or speech.
Fig. 1.
Right side massetric hypertrophy
Fig. 2.
Profile view of patient
Fig. 3.
Profile view during spasm
Fig. 4.
Masseter muscle stripping at its insertion on lower border of mandible
Discussion
HMS is believed to be a rare neurological disorder due to demyelination of the third branch of trigeminal nerve. Review of literature reveals only 15 cases have been reported making it an extremely rare phenomenon. In these cases a predominance of female to male by 2:1 was seen. Certain triggers such as chewing, touching the face, electrical and mechanical stimulation of mentalis and clenching have been reported. Interestingly almost 73% had associated hemifacial atrophy of the ipsilateral side and 40% had localized scleroderma along with hypertrophy of the involved muscles. There is varying reports on the severity of the lesion, at times patient have bitten their lips and tongue during these spasm [3], and dislocation of the temporomandibular joint on the affected side [4]. The EMG usually shows rapid burst of motor unit potentials with discharge up to 200 Hz. The most diagnostic of HMS is the loss of silent periods during the spasm. The silent period has been defined as a reflexive pause in muscle activity following functional tooth contact (as in chewing or swallowing), or following an experimentally produced tap on the chin of a subject whose teeth are clenched together (jaw-jerk reflex) [5].
The etiology of HMS is still unclear, however various authors have noted its similarity to hemifacial spasm [HFS]. Thompson and Carrol suggested a peripheral motor nerve deafferentation with generation of ectopic impulses. They also do not rule out inflammatory lesion and vascular compression of the motor root by superior cerebellar artery as seen in HFS [6]. Ho Jin et al. [1] suggested demyelination of peripheral branches of the mandibular division of trigeminal nerve secondary to compression and stretching due to deep tissue changes caused by facial hemiatrophy.
Some authors have attempted treating the disorder with carbamazepine and phenytoin with some success [7], majority believe local injection of botulinum is the treatment of choice. In our case we have achieved remission of the lesion by stripping the muscle and allowing it to reattach. We are unsure of mechanism of action of this technique, possibly destruction of the ectopic foci may be a possible explanation suggesting a peripheral motor branch involvement.
Conclusion
HMS is an interesting but rare lesion which has no mention in the routine textbooks read by maxillofacial surgery trainees. The aim of this article is to appraise the maxillofacial community of this peculiar lesion and need to include it in differential diagnosis of the neuropathies of the maxillofacial region. Botulinum injection is the choice of treatment for this lesion, however we have achieved remission by stripping of masseter. Further investigations are required to justify this mode of management.
References
- 1.Ho Jin K, Beom SJ, Kwang-Woo L. Hemimasticatory spasm associated with localized scleroderma and facial hemiatrophy. Arch Neurol. 2000;57(4):576–580. doi: 10.1001/archneur.57.4.576. [DOI] [PubMed] [Google Scholar]
- 2.Gowers WR. A manual of diseases of the central nervous system. 2. Philadelphia: Blakiston; 1897. pp. 221–224. [Google Scholar]
- 3.Thompson PD, Obeso JA, Delgado G, Gallego J, Marsden CD. Focal dystonia of the jaw and the differential diagnosis of unilateral jaw and masticatory spasm. J Neurol Neurosurg Psychiatry. 1986;49(6):651–656. doi: 10.1136/jnnp.49.6.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaufman MD. Masticatory spasm in facial hemiatrophy. Ann Neurol. 1980;7(6):585–587. doi: 10.1002/ana.410070614. [DOI] [PubMed] [Google Scholar]
- 5.Skiba TJ, Laskin DM. Masticatory muscle silent periods in patients with MPD syndrome before and after treatment. J Dent Res. 1981;60(3):699–706. doi: 10.1177/00220345810600030501. [DOI] [PubMed] [Google Scholar]
- 6.Thompson PD, Carroll WM. Hemimasticatory spasm—a peripheral paroxysmal cranial neuropathy? J Neurol Neurosurg Psychiatry. 1983;46(3):274–276. doi: 10.1136/jnnp.46.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Auger RG, Litchy WJ, Cascino TL, Ahlskog JE. Hemimasticatory spasm: clinical and electrophysiologic observations. Neurology. 1992;42(12):2263–2266. doi: 10.1212/wnl.42.12.2263. [DOI] [PubMed] [Google Scholar]