Abstract
Giant cell rich osteosarcomas, histological variant of conventional osteosarcomas account for 3% of all cases of osteosarcomas and most of them are arise from the appendicular skeleton. Giant cell rich osteosarcomas have been rarely reported in the head and neck region. This is the first case report of giant cell rich variant of osteosarcoma in the maxilla. It is important to recognize this variant, as its prognosis is worse as compared to conventional osteosarcomas of the head and neck region. We here present a case of giant cell rich variant of osteosarcoma of the maxilla and along with its characteristic radiological and histopathological picture.
Keywords: Giant cell variant of osteosarcoma, Maxilla, Worse prognosis
Introduction
Osteogenic sarcoma is a rare malignancy of bone that occurs primarily in the appendicular skeleton [1]. Osteosarcoma of head and neck region accounts for 6 to 13% of all cases of osteosarcomas [2]. Giant cell rich osteosarcoma is the rare morphologic variant, constituting about 3% of all osteosarcomas. On review of world literature, most of cases giant cell rich osteosarcoma has been reported in the extremities. To the best our knowledge giant cell rich osteosarcoma of the maxilla has never been reported in the world literature. Giant cell rich osteosarcoma is often confused histopathologically with giant cell rich variety of malignant fibrous histiocytoma, giant cell tumor and chondrosarcoma. Owing to the different prognosis and treatment strategies of these tumors, it is important that right diagnosis is made. This article reports a case of giant cell rich osteosarcoma of the maxilla long with its characteristic radiological and histopathological features.
Case Report
A 56 year old woman presented with history of left cheek swelling for last 5 years. Initially the swelling was apparent on left upper alveolus but gradually it involved the left half of palate and left cheek. She complained of sudden increase in size of swelling for last 1 year. She complained of left sided nasal obstruction and nasal discharge which was occasionally blood stained for last 2 years. She had difficulty in chewing and swallowing for 6 months. There was neither history of difficulty in opening the mouth nor had any visual complaints.
On external examination there was 10 × 10 cm swelling, on left cheek extending superiorly from inferior orbital rim to angle of mandible. Medially it was extending from medial canthus to zygoma laterally with broadening of nasal dorsum and obliteration of left naso-facial groove (Fig. 1). The swelling was firm to hard in consistency. On oral cavity examination a 5 × 5 cm bulge was seen involving left side hard palate starting from central incisor to the third molar tooth. Anterior rhinoscopic examination revealed reddish mass occupying whole of the left nasal cavity with deviation of nasal septum to the right. Vision was normal in both eyes with preserved extraocular movements. Sensation over the cheek was decreased on the left side. Skin over the swelling was not pinchable over the zygoma.
Fig. 1.
Clinical photograph showing preoperative tumor extension
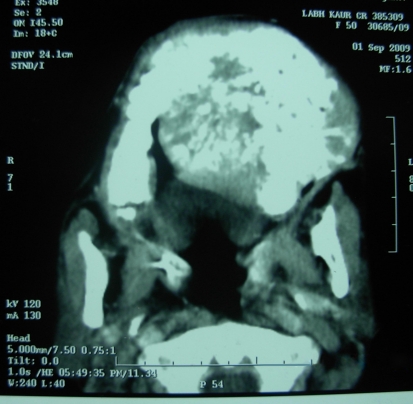
Contrast enhanced CT scan showed an expansile, hyperdense soft tissue mass occupying the whole of maxilla. There was destruction of nasal septum, anterior wall of maxilla with tumor extending till the subcutaneous plane of the skin. Tumor was extending into the orbit with destruction of the floor of the orbit. The upper alveolus and the hard palate were destroyed with tumor extending into palate. Areas of calcification were seen within the substance of tumor with sclerosis of adjacent bone (Figs. 2, 3). Fine needle aspiration cytology from the mass showed features suggestive of malignant fibrous histiocytoma.
Fig. 2.
CT scan (Coronal) showing expansile and destructive lesion involving left maxilla
Fig. 3.
CT scan (axial cuts) showing expansile and destructive lesion involving left maxilla
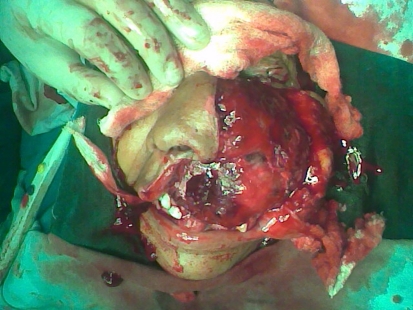
The case was discussed in tumor board and decision for total maxillectomy with postoperative radiotherapy was made. Using the standard Weber-Ferguson, total maxillectomy was done under general anesthesia. 10 × 10 cm tumor was involving the maxilla, the orbital muscle was free, and the tumor was removed in toto (Fig. 4). The tumor was of variable consistency with soft cystic areas and solid areas. Postoperative period was uneventful. Histopathology of the excised specimen showed a pleomorphic tumor arranged in fascicular pattern as well as in sheets. The tumor cells were highly pleomorphic with some of them ovoid to round and some spindle shaped with numerous giant cells. Areas of lace like osteoid formation by the tumor cells were also seen. The tumor cells had vesicular nuclei and high mitosis. Based on the histopathological features, a definite diagnosis of giant cell rich osteosarcoma was made. The patient referred to radiotherapy department for chemoradiation. She received 60 Gy of radiotherapy with 5 cycles of chemotherapy. She is now under regular follow up. Her last follow up visit was 1 month back and has no recurrence till date.
Fig. 4.
Intra operative picture showing extensive tumor being excised
Discussion
Giant cell rich osteosarcomas, first described by Bathurst and Sanekin, are rare variants of osteosarcoma that account for 3% of all cases of primary osteosarcomas [2]. Typically occurring in the extremities, giant cell rich osteosarcoma in the head and neck region is extremely rare in the literature. On searching the world literature, we could not find single case report of giant cell rich osteosarcoma of the maxilla.
Osteosarcomas are highly malignant bone tumor and it is relatively a rare disease in the head and neck region. They accounted for 0.5% of all head and neck tumors. Most of osteosarcomas in the head and neck arise from the mandible and maxilla. Gnathic osteosarcomas exhibit some behavioral features that separate them from the lesions of the rest of the skeleton. Jaw lesions tend to occur at an older mean age [3]. Some series in literature also suggests the female predominance [4]. Present case is also a female from older age group. They usually exhibit lower aggressive potential than their long bone counterparts and have excellent prognosis if completely resected [5]. However giant cell rich osteosarcomas of the jaws are very rare in literature. They are usually undifferentiated forms of sarcomas and thus prognosis is much poorer in these cases.
The radiological features of giant cell rich osteosarcoma are different from the conventional osteosarcomas. They mimic non mineralized benign or malignant bone tumors. In the long bones they present as osteolytic lesion with cortical thinning and ballooning without obvious cortical destruction [6]. While in our case contrast enhanced CT scan showed expansile heterogeneous mass filling the maxilla with extensive destruction of the all the walls of the maxilla, areas of speckled calcification within the tumor and adjacent sclerosis. The tumor was destroying the palate and extending into oral cavity. Radiologically, the differential diagnosis includes aneurysmal bone cyst, chondrosarcoma, Chondromyxoid fibroma. Our initial radiological diagnosis was of chondrosarcoma and malignant fibrous histiocytoma.
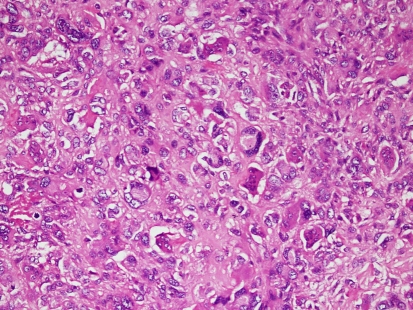
Histologically, giant cell rich osteosarcoma is an undifferentiated sarcoma with scanty osteoid formation.The microscopic appearance of giant cell rich osteosarcoma is characterised by numerous osteoclast-like giant cells dominating the picture, however the presence of osteoid formation by the tumor cells gives a clue regarding the diagnosis [6]. This osteoid or new bone is recognised by eosinophilic staining quality glassy appearance irregular contours and it is surrounded by rim of osteoblasts. These giant cells appeared as nodular clusters admixed with fibroblasts or histiocyte-like cells, or alternated with bundles of collagen-rich fibroblastic tissue (Fig. 5).
Fig. 5.
Photomicrograph showing numerous osteoclast-like giant cells, admixed with undifferentiated stromal tumor cells with nuclear atypia (haematoxylin and eosin, ×200)
In the present case, the histology showed tumor cells arranged in fascicular pattern as well as in sheets. The tumor cells were highly pleomorphic with some of them ovoid to round and some spindle shaped, with numerous osteoclast-like giant cells. Areas of lace like osteoid formation by the tumor cells were also seen. Based on the histopathological features, a definite diagnosis of giant cell rich osteosarcoma was made. Histologically, differential diagnosis includes giant cell tumor of bone and giant cell rich malignant fibrous histiocytoma [7]. In the former, similarity of the nuclei of osteoclastic giant cell and the tumor cells gives the clue while in later, storiform pattern and obvious pleomorphism is quite characteristic [8]. Likewise in the presented case the preoperative cytology of the tumor was in close resemblance with malignant fibrous histiocytoma and postoperative histopatholgic appearance of the tumor was in favour of giant cell rich osteosarcoma (Fig. 6).
Fig. 6.
Postoperative photograph after completion of chemoradiation therapy
Conclusion
Apart from the common variants, giant cell rich osteosarcoma is a rarer variant which has very close resemblance with malignant fibrous histiocytoma. Giant cell rich osteosarcomas are undifferentiated sarcoma and have poorer prognosis. So a careful histopathologic examination is required to diagnose them and differentiate from the other types of osteosarcoma. Clinicians and pathologists should be aware of its radiological and histological characteristics and main differential diagnosis to avoid late recognition and better management.
Acknowledgments
Conflict of interest There is no conflict of interest or financial disclosure to be made.
References
- 1.Caron AS, Hajdu SI, Strong EW. Osteogenic sarcoma of the facial and cranial bones: a review of forty-three cases. Am J Surg. 1971;122:719–725. doi: 10.1016/0002-9610(71)90434-X. [DOI] [PubMed] [Google Scholar]
- 2.Bathurst N, Sanerkin N, Watt L. Osteoclast rich osteosarcoma. Br J Radiol. 1986;59:667–673. doi: 10.1259/0007-1285-59-703-667. [DOI] [PubMed] [Google Scholar]
- 3.Clark JL, Unni KK, Dahlin DC, Devine KD. Osteosarcoma of the jaw. Cancer. 1983;51:2311–2323. doi: 10.1002/1097-0142(19830615)51:12<2311::AID-CNCR2820511224>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 4.Regezi JA, Zarbo RJ, McClatchey KD, Courtney RM, Crissman JD. Osteosarcomas and chondrosarcoma of the jaws: immunohistochemical correlations. Oral Surg Oral Med Oral Pathol. 1987;64:302–307. doi: 10.1016/0030-4220(87)90009-0. [DOI] [PubMed] [Google Scholar]
- 5.Zarbo RJ. Malignant non-odontogenic neoplasms of the jaws. In: Regezi JA, Schuibba J, editors. Oral pathology clinical pathologic correlations. Philadelphia: W.B. Saunders Company; 1993. pp. 436–457. [Google Scholar]
- 6.Sato K, Yamamura S, Iwata H, Sugigura H, Nakashima N, Nagasaka T. Giant cell rich osteosarcoma: a case report. Nagoya J Med Sci. 1996;59:151–157. [PubMed] [Google Scholar]
- 7.Bennett JH, Thomas G, Evans AW, Speight PM. Osteosarcoma of the jaws: a 30-year retrospective review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:323–333. doi: 10.1067/moe.2000.108274. [DOI] [PubMed] [Google Scholar]
- 8.Sciot R, Samson I, Dalcin P, et al. Giant cell rich parosteal osteosarcoma. Histopathology. 1995;27:51–55. doi: 10.1111/j.1365-2559.1995.tb00290.x. [DOI] [PubMed] [Google Scholar]