Abstract
Introduction
Mandibular defects usually involve a combination of osseous and soft tissue deficiency and are among the most challenging problems in maxillofacial surgery, many options are available for mandibular reconstruction. One of the options discussed in literature recently being distraction osteogenesis.
Aim and Objective
The aims and objectives of the study were to evaluate clinically the technique of distraction osteogenesis to reconstruct mandibular defects, using indigenous transport distractors, and to evaluate the efficacy of Indigenous transport distraction osteogenesis device.
Materials and Methods
A prospective, experimental study was designed to examine the use of transport distraction osteogenesis in the treatment of defects of the mandible. Four patients with defects of the mandible were subjected to distraction osteogenesis with indigenously manufactured distraction device. The regenerate was assessed clinically and radiographically.
Results
The results showed that the regenerate was clinically as hard as the adjacent unaffected mandible and radiologic evidence of bone regeneration was observed. The major advantage being regeneration of hard tissue and soft tissue components without the morbidity of donor site, so that functional rehabilitation of the patient is possible.
Conclusion
Thus from our study it is shown that transport distraction osteogenesis using indigenous distractors is a reliable yet affordable option for reconstruction of mandibular defects.
Keywords: Distraction osteogenesis, Mandible, Reconstruction, Transport
Introduction
Mandibular defects can range from isolated segmental defects to large extensive areas of bone involving the entire jaw. These defects are often congenital, as a result of trauma, infection or resection of benign and malignant tumors [1]. The treatment of defects of the mandible has long been a difficult reconstructive challenge to the oral and maxillofacial surgeon. These deformities usually involve a combination of osseous and soft tissue deficiency and are among the most challenging problems in maxillofacial surgery, many options are available for mandibular reconstruction, including reconstruction plates, and particulate bone grafts, block bone grafts, and micro vascular free tissue transfer [1].
Although great studies have been made in this field, no single technique is uniformly superior, as evidenced by a century of effort and by the sheer number of reconstructive options available.
To begin, it is important to appreciate the six primary goals of mandibular reconstruction:
Restoration of osseous continuity,
Restoration of osseous bulk,
Restoration of alveolar height,
Restoration of arch form, width and alignment,
Maintenance of the bone graft/graft durability,
Acceptable facial form and appearance.
Adherence to these principles will yield a patient with a relatively normal functional and cosmetic result [2]. Over the years, numerous advances have been made, towards achieving these goals of reconstruction. Most recently, another treatment option has been described in the literature, “distraction osteogenesis” Although distraction osteogenesis has been widely used in long bones for several decades; it is not until the 1990s that this technique became a common method in mandibular lengthening. By means of this procedure new bone is created after, osteotomy followed by gradual separation of bony fragments [3]. First described by Codivilla in 1905 [4], but was popularized and studied extensively through the work of Professor Gavrill A. Ilizarov, beginning in 1951 [4]. Recently distraction osteogenesis has been shown to be a successful technique not only in the surgical treatment of the congenital and acquired mandibular hypoplasia, but also in the reconstruction of segmental mandibular defects.
Professor Ilizarov described the biological foundation upon which he developed and pioneered the clinical protocols for distraction osteogenesis [5]. Distraction osteogenesis has the unique ability to correct osseous and soft tissue deficiencies simultaneously. Most of these deformities in the mandible involve a combination of osseous and soft tissue deficiencies making satisfactory reconstruction with conventional methods difficult or impossible. This concept of distraction osteogenesis challenged traditional thought in orthopedic surgery by demonstrating that bone growth and healing of defects could be stimulated by the distraction, or pulling apart, of bone segments, and not by compression, as was previously held to be true.
Distraction osteogenesis works by what is described as the “Principle of Tension-stress”, which governs the response of tissues to elongation [4]. He showed that living tissue became metabolically activated in both the biosynthetic and proliferative pathways when subjected to slow, steady traction. Periosteum which is a specialized connective tissue anchored to bone, that is lined by an inner layer called cambial layer which is a reservoir of undifferentiated pluripotent mesenchymal cells which differentiate into chondrogenic and osteoblastic progenitor cells [6]. This phenomenon is independent on vascularity and functional use.
Transport distraction osteogenesis is the process whereby a space or defect in a limb can be filled with bone by creating a ‘transport disc’ on one side of the defect, and advancing this disc gradually across the defect. This disc leaves regenerated bone in its wake under the influence of tensional stress [7]. Transport distraction osteogenesis is divided into three groups based on the number of distraction or compression sites as Monofocal, Bifocal and Trifocal [8].
This technique is a proven option for reconstruction of continuity defects of the long bones [9], the challenge for surgeons operating on the mandible lies in the application of Ilizarov’s principles to the treatment of continuity defects, much as our orthopedic colleagues have done. The purpose of this study was to clinically evaluate the technique of transport distraction osteogenesis to reconstruct defects of the mandible using an indigenously made distraction device. Since Ilizarov used external pin fixator frames for distraction which was a modification of Wagner device [10] a huge multitude of devices are available for distraction.
Materials and Methods
The study was conducted on those patients who require reconstruction of mandibular defects that result following surgery for pathology or trauma, in the department of Oral and Maxillofacial Surgery, V.S. Dental college and Hospital, Bangalore, and those cases who reported to the department with such established defects were also included.
Both male and female patients with mandibular defects secondary to pathology or trauma were included. Patients with systemic diseases where surgery is contraindicated, patients with systemic bone pathology, mentally retarded patients were excluded.
A prospective, experimental study was designed to examine the use of transport distraction osteogenesis using Indigenous device in the treatment of defects of the mandible. Four patients, three males and one female. The patients were of age ranging from 20 to 35 years. Three of them had reported to our department with pathologic lesions and subsequently underwent resection. One patient reported with an established segmental defect of the mandible. The size of the defects ranged from 25 to 60 mm. All surgical procedures were performed by the same surgeon.
Surgical Procedure
All the patients were premedicated with Amoxicillin + Clavulanic acid and Metronidazole. After anesthetizing the patient, either using an extra oral or an intra oral incision, the lateral border of the mandible was exposed with minimal periosteal stripping of the buccal cortex and no periosteal stripping of the lingual cortex. Using a fissure bur corticotomy was created on the lateral and inferior surface of the mandible to outline the transport segment. The transport device was then applied using bicortical pin fixation. To avoid a significant scar, the pins were placed through individual stab incisions with the help of trocar and sleeve. The device was then attached to the pins, verifying the vector and trajectory of the planned transport segment. The device was then attached to fit passively on the fixation pins and the clamps locked in position and the device was removed. The corticotomy was then converted into osteotomy. The distraction device was then reattached and mobility of the transport disk checked. The device was then closed until the bone edges approximated followed by wound closure (Figs. 1, 2, 3, 4, 5, 6).
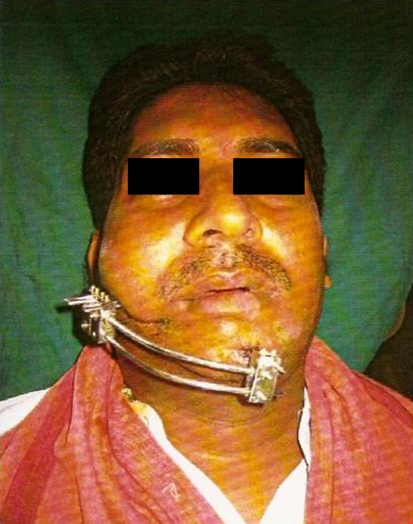
Fig. 1.
Pre-op (extraoral distraction)
Fig. 2.
Distraction device in place
Fig. 3.
Postoperative view (6 months)
Fig. 4.
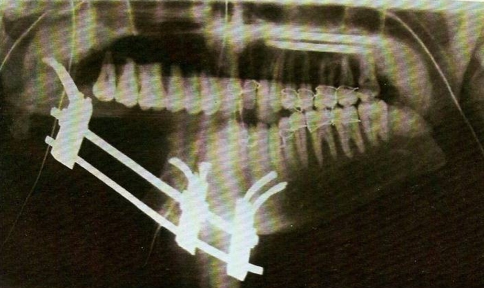
OPG (pre-op)
Fig. 5.
OPG (distraction in progress)
Fig. 6.
OPG (16 weeks post distraction)
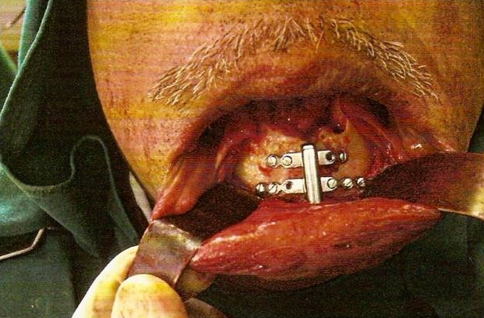
In the case of intra oral vertical alveolar distraction device the device was first fixed onto the buccal cortex of the mandible and then the osteotomy was done. The device was checked for unimpeded movement and the distractor reversed to obtain approximation of the bony edges. Then the wound was closed (Figs. 7, 8).
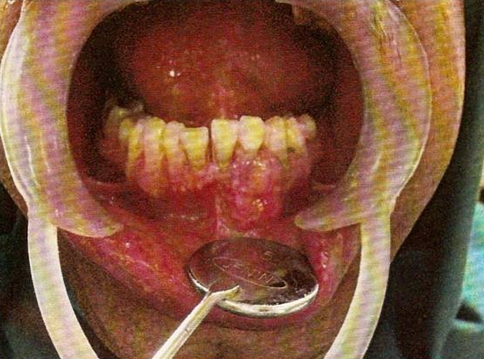
Fig. 7.
Pre-op (intraoral distraction)
Fig. 8.
Distraction device in place after excision of lesion
All the patients continued on antibiotics for 1 week post operatively and regular dressing of the external pin fixation sites was done with betadine (Povidone Iodine 5%) soaked gauze for one patient and Neosporin (Polymixin B sulphate, Neomycin sulphate and Zinc bacitracin) powder was used on the others for the patient with intra oral device betadine (Povidone Iodine 1%) oral rinse was advised.
All patients were subjected to varying periods of latency, rate and rhythm of the distraction varied based on the clinical situation. At the end of distraction the device was left in place for consolidation usually for 2–3 months. Then the distraction device was retrieved under local anesthesia. The regenerate was assessed clinically and radiographically. Orthopantomograms were taken on the 4th, 8th, and 15th weeks post distraction.
Results and Observations (Table 1)
Table 1.
Patient data
| Case I | Case II | Case III | Case IV | |
|---|---|---|---|---|
| Age/gender | 30/Male | 25/Female | 21/Male | 30/Male |
| Diagnosis | Ameloblastoma | Reconstruction plate fracture | Complex odontoma | Follicular ameloblastoma |
| Defect size (mm) | 50 | 60 | 35 | 25 |
| Defect location | Right body of mandible | Right body of mandible | Right angle of mandible | Anterior mandibular alveolus |
| Anesthesia | General anesthesia | General anesthesia | General anesthesia | Local anesthesia |
| Approach | Intraoral | Extraoral | Extraoral | Intraoral |
| Device used | Extraoral | Extraoral | Extraoral | Intraoral |
| Length of transport segment (mm) | 20 | 30 | 20 | 10 |
| Latency period (days) | 7 | 15 | 10 | 10 |
| Rate of distraction (mm/day) | 0.7 | 0.7 | 1.4 | 1 |
| Consolidation (weeks) | 16 | 18 | 15 | 8 |
All the patients irrespective of whether they fixed with extra-oral or intra oral device had no difficulty in the immediate post operative phase. The duration of latency period was uneventful. The patients were advised to be on soft diet. In the early post-operative days three patients with extra-oral device had mild discomfort with posture, as they were not able to sleep on the side the device was placed.
At the beginning of the distraction phase there was no pain or difficulty during the activation. There was no intraoral gaping or exposure of the transport disk during the distraction phase except for one case where there was an exposure of the alveolar crest of healing extraction socket intraorally which was nibbled with a bone ronguer and further distraction was carried out uneventfully. In all the three cases of extra oral distraction, minor dehiscence around the pins of transport block was noted during the distraction phase and consolidation phase. The infections were treated with course of antibiotics (Amoxicillin + Clavulonic acid) and Metronidazole, and also with local application of antiseptic dressing.
The extra oral device in all the three left pin tract scar. The length of the linear scar much smaller than the length through which the transport segment was distracted. The activation port of the intra-oral device left a small extraoral scar at the centre of chin measuring about 8 mm. Later the scar was excised and plastic closure was done. None of the patients developed marked cross bite as a result of application of the distraction force. Though one of the patients who reported with an established continuity defect had a cross bite before the start of distraction which aggravated during the course of the treatment and was managed by providing a guiding plate in the maxillary arch. Interestingly this was the only case in which distraction was carried across the midline. The direction of vector was lost in the case where the segment had to pass through the curve of symphysis.
Radiographic examination during the distraction phase and 3rd–4th weeks post distraction the defect appeared radiographically similar to the surrounding soft tissue, even though on clinical palpation the reconstructed area felt no different from the pre existing mandible. By the 7th or 8th week radio-opaque material tapered from the surfaces of the transport disc and proximal stump. 12th–15th weeks radiograph reveals dense non homogenous bands of calcification seen throughout the regenerate. The leading nut of the transport had to be sacrificed in all the three cases of extraoral distraction as the nut by itself caused a hindrance to the utilization of the distraction space available. The bulky extraoral device caused problem for the patients’ public appearance there by restricting their professional and social activities.
Discussion
Reconstruction of the mandible following ablative surgery or trauma has a number of options; reconstruction of mandibular defects in a way that provides acceptable functional and aesthetic results is difficult. The various methods used include the insertion of bone grafts, allogeneic materials, and vascularized free flaps. None of these is completely satisfactory; the alloplastic materials carry the risk of bacterial infection and perforation of the skin or oral mucosa. Harvesting of bone graft is associated with morbidity and possible functional impairment at the donor site. The attraction of applying the distraction technique for mandibular reconstruction is its lack of donor site morbidity and its ability to increase the overlying soft tissues by inducing histogenesis [11].
Transport distraction osteogenesis offers many advantages over microvascular free tissue transfer. It was found that microvascular free tissue transfer is technically difficult and invasive with significant donor site morbidity. Free flaps often result in inadequate bone for mandibular rehabilitation with osseointegrated dental implants [12]. In transport osteogenesis the callus formed during gradual distraction has all the characteristics of an ideal transplant material that requires no mechanical stimulation. The main stimulator of bone growth was found to be tension on the callus while the proximal surfaces are mobilized [3]. Various types of distraction osteogenesis are classified according to the number of distraction or compression sites as monofocal, bifocal and trifocal. Reconstructing segmental defects require either bifocal or trifocal distraction osteogenesis.
The first application of transport (bifocal) distraction osteogenesis for reconstructing segmental mandibular defects was done by Constantino et al. in 1990. The regenerated bone had a similar diameter to the preexisting mandible, and the inferior alveolar artery and vein were found to recannulate through the regenerated bone [13]. Other animal studies have shown that the diameter of the regenerated bone is comparable to pre existing bone. Gantous et al. [14] demonstrated that distraction osteogenesis was feasible even in previously radiated mandible. Annino et al. successfully applied trifocal distraction to bridge the defect by moving two transport segments towards each other in dogs. This concept of transport distraction in mandible was subsequently applied in clinical mandibulectomy reconstruction as well [15].
The present study is based on the study conducted by Block et al. [7]. Four patients with defects of the mandible were subjected to distraction osteogenesis with indigenously manufactured distraction device. The study was undertaken as an attempt to evaluate the technique of distraction osteogenesis and the efficacy of indigenous distraction device in reconstruction of mandibular defects.
The external and internal device used was bone borne type. The extraoral device (manufactured by Mahesh engineering and company Chennai) was based on the design used by Shvyrkov [9], also by Constantino and Wagner. It consists of double pin fixation clamps on a threaded guiding rod, however to counteract the vertical rotation of the fixation clamps around the rail a stabilization rod was introduced in the lower end of the clamp in our present device. They were fixed to the mandible by 2.5 mm Tzanck pins. The device allowed bidirectional movement of the transport segment. The intraoral device (manufactured by S.K. Surgicals—Pune) was based on the track intra alveolar distractor [16]. It was fixed to distraction segment by monocortical S.S. screws.
The device was fixed either intraorally or extraorally. In extra oral approach the percutaneous pins were placed through a stab incision over skin. The parallelism of the docking surfaces is critical in order to have a complete docking of the transport segment with the docking stump vertical in the vertical plane. This if not maintained will require bone grafting to fill up the wedge shaped defect left as a result of incomplete docking.
The percutaneous pin should be placed in such a way that the distance between the pin entry point and the docking surface of the transport segment should be greater than or equal to the sum of the width of the nut (a) and the distance from the leading edge to the pin entry point on the double pin fixation clamp (b). If this is not followed, the device by itself may prevent docking (Fig. 1). To overcome this the leading nut was sacrificed to gain final compression at the docking site. And also it was found through our study that if the corners of the double pin fixation is clamp are rounded off, the distraction space can still be improved on the guide rod to some extent (Fig. 2).
In all the cases of the present study, teeth in the transport segment were removed so that teeth does not impede the free movement of the transport segment and moreover in large defects teeth come to lie in unnatural position like in the angle of mandible at the end of the distraction process. This is contradictory to studies conducted by Shvyrkov [9] who used the teeth as support for providing a bridge for occlusal rehabilitation. Allan Herford [1], Block et al. [7] in their studies suggested that the teeth in transport segment be extracted about 2 weeks prior to surgery in order to allow the alveolus to heal. However in our study extractions was done on the OT table and follow up extraction sockets on the transport segment healed normally except for one case (case 1) where there was exposure of alveolar crest, which was nibbled with a bone ronguer and the further distraction, carried out uneventfully. The placement of device caused mild discomfort to the patients in terms of posture as the extra oral device was hindering in their regular sleeping posture.
The literature suggests a latency period of 7–10 days for transport distraction. However they suggest a modification of this period depending on the clinical circumstances. In the present study after the osteotomy and fixation of the distraction device the patients were on varying latency period from 7 to 15 days. The latency period was extended depending on the width of osteotomy, the length of the defect, integrity of periosteum and the age of the patient. In none of our cases early consolidation occurred as a result of extended latency period up to 15 days. So It may be suggested that the variation of latency period up to 15 days depending upon the clinical situation poses no risks of early consolidation.
The rate of distraction of 0.7–1.5 mm per day was used on the patients with no difference in the clinical outcome. There was no discomfort experienced during the distraction phase. The rate of 1 mm distraction is considered ideal as the osteon grow at the rate of 1 mm per day during regeneration as reported by Shvyrkov [9] The rhythm of distraction was maintained at one turn per day and it was consistent enough to give promising clinical results, however the literature shows that multiple small distractions over many increments in a day will give ideal results.
The extra oral pins generally lead to mild wound dehiscence and minor infections at their entry sites, which were easily managed and resolved uneventfully. There were no instances of pin bending, pin breakage, loss of pins or loss of device as proposed by Suhr [17] who calculated a 33.1% of complication were due to mechanical problems. The extra oral device left a pin tract scar over the face but the length of the scar was much smaller to the length of the bone regenerate. This can be attributed to the stretching of skin as the pins passed through them. The activation port of intraoral device left a small scar which was excised and plastic closure done at the time of retrieval of the device.
The process of distraction left no permanent loss of sensation in any case. Though the patients complained of paresthesia after the device was fixed, the condition resolved by itself during the course of the treatment. There was transient buccal nerve paresthesia in the patients with extraoral device when the pins passed through their course but all recovered at the end of consolidation. The patients with segmental resection recovered sensation at the end of consolidation phase; this can be attributed to the histogenesis of the nerve simultaneously during the course of distraction. This phenomenon of regeneration of nerve tissue leading to regaining of sensation in cases of segmental resection was observed in the present study (Fig. 3).
The removal of extra oral device was simple, just pin removal done under LA and the pin was entry site were left to heal secondarily. The intra oral device however required raising a mucoperiosteal flap under L.A.
The regenerate was found to be clinically as hard as the adjacent unaffected mandible on palpation at the end of consolidation phase. The thickness and height was similar to the dimensions of the transport segment on clinical palpation. On intraoral examination the residual alveolar ridge was constructed with the attached gingiva and the regenerate was found to have sufficient lingual and buccal sulcus to receive either dental implants or dentures.
On radiographic examination, during the distraction phase and also up to 3–4 weeks in consolidation period the defect appeared radiographically similar to surrounding soft tissue. By 7th–8th week radiopaque material tapered from the surface of the transport disc and proximal stump to the centre of the regenerate this was found to be of parallel strands of “paint brush” type. The 12th–15th weeks radiograph revealed dense non homogenous bands of calcification throughout the regenerate. These results were consistent with those noted by James Aronson [10]. He further found out that radiolucent spaces interspersed between osteogenic columns which represented the large vascular channels extending from the fibrous interzone proximally and distally towards each osteotomy surface. During routine new bone formation, the ossification makes a transition from the fibrous to cambium layer of periosteum perpendicular to the fibers, where as in distraction osteogenesis, ossification was distinctly parallel to the fibers.
The present study shows that the main disadvantage of technique are
The long duration of treatment
The prolonged use of external or internal fixators
Inconvenience to the patients in social and professional aspects.
The major advantage being regeneration of hard as well as soft tissue without morbidity to donor site, so that functional rehabilitation of the patient is possible.
Thus from the present study it is shown that transport distraction osteogenesis using indigenous distractors is a reliable yet affordable option for reconstruction of mandibular defects.
Summary and Conclusion
Functional and esthetic reconstruction of the mandible after bone loss continues to be a formidable problem in head and neck surgery. Grafts, flaps, and synthetic materials have been used to reconstruct the mandible. Unfortunately, grafts and flaps result in added morbidity, and may be of limited availability. Synthetic materials generally retain the characteristics of a foreign body and fail to fully replace living tissues in appearance or function. Distraction osteogenesis has been proposed as an alternate method of reconstruction, through which mandibular defects could be replaced by new bone grown from the remaining mandible [14].
From the present study it can be concluded that, indigenous distraction device can be used successfully in the mandibular reconstruction. That by understanding the biological consequences of the principles of tension-stress, one can treat a large variety of mandibular defects. Distraction osteogenesis is a promising treatment for reconstructing the defect of the mandible. It shares all the advantages of autogenous bone graft with minimal donor site morbidity, and by the use of indigenous distractors this technique of reconstruction of the mandible is reliable yet affordable [3, 7, 18, 19].
Our study had certain limitations like the small sample size, all the patient’s had benign lesions. Further studies are required to help in adapting this technique using indigenous distraction device to reconstruct defects involving the symphysis region of the mandible. In future distraction osteogenesis will be carried out with sophisticated devices which allow three dimensional manipulations of the callus. Distraction osteogenesis may also be used in combination with growth factors to make reconstruction faster and more efficient.
References
- 1.Herford AS. Use of plate guided distraction device for transport distraction osteogenesis of the mandible. J Oral Maxillofac Surg. 2004;62:412–420. doi: 10.1016/j.joms.2003.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Gervais NL (1996) The use of bifocal distraction osteogenesis for the treatment of continuity defects in the rabbit mandible. Dissertation, McGill University, Montreal
- 3.Rubio-Bueno P, et al. Internal distraction osteogenesis with a unidirectional device for reconstruction of mandibular segmental defects. J Oral Maxillofac Surg. 2005;63:598–608. doi: 10.1016/j.joms.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy JG, et al. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992;89:1–10. doi: 10.1097/00006534-199289010-00001. [DOI] [PubMed] [Google Scholar]
- 5.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 6.Kanno T, et al. Tensile mechanical strain up regulates Runx2 and osteogenic factor expression in human periosteal cells: implications for distraction osteogenesis. J Oralmaxillofac Surg. 2005;63:499–504. doi: 10.1016/j.joms.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Block MS, et al. Bifocal distraction osteogenesis for mandibular defect healing: case reports. J Oralmaxillofac Surg. 1996;54:1365–1370. doi: 10.1016/S0278-2391(96)90499-1. [DOI] [PubMed] [Google Scholar]
- 8.Costantino PD, et al. Experimental mandibular regrowth by distraction osteogenesis. Arch Otolaryngol Head Neck Surg. 1993;119:511–516. doi: 10.1001/archotol.1993.01880170035007. [DOI] [PubMed] [Google Scholar]
- 9.Shvyrkov MB. Non-free osteoplasty of the mandible in maxillofacial gun shot wounds: mandibular reconstruction by compression osteodistraction. Br J Oral Maxillofac Surg. 1999;37:261–267. doi: 10.1054/bjom.1999.0120. [DOI] [PubMed] [Google Scholar]
- 10.Aronson J, et al. The histology of distraction osteogenesis using different external fixators. Clin Orthop Relat Res. 1989;241:106–116. [PubMed] [Google Scholar]
- 11.Raghoebar Gerry M, et al. Distraction osteogenesis in the irradiated mandible. A case report. J Craniomaxillofac Surg. 2005;33:246–250. doi: 10.1016/j.jcms.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Whitesides LM et al (2005) Mandible reconstruction using a two phase transport disc distraction osteogenesis. A case report. J Oral Maxillofac Surg 261–266 [DOI] [PubMed]
- 13.Cosantino PD, et al. Segmental mandibular regeneration by distraction osteogenesis: an experimental study. Arch Otolaryngol Head Neck Surg. 1990;116:535–545. doi: 10.1001/archotol.1990.01870050035003. [DOI] [PubMed] [Google Scholar]
- 14.Gantous A, et al. Distraction osteogenesis in the irradiated canine mandible. Plast Reconstr Surg. 1994;93(1):164–168. doi: 10.1097/00006534-199401000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Chung LK, et al. Reconstruction of maxillary defect by transport distraction osteogenesis. Int J Oral Maxillofac Surg. 2003;32:515–522. [PubMed] [Google Scholar]
- 16.Samchukov ML, Cope JB, Cherashin AM, editors. Craniofacial distraction osteogenesis. St. Louis: Mosby; 2001. [Google Scholar]
- 17.Suhr MAA, Kreusch T. Technical consideration in distraction osteogenesis. Int J Oral Maxillofac Surg. 2004;33:89–94. doi: 10.1054/ijom.2003.0462. [DOI] [PubMed] [Google Scholar]
- 18.Oda T, et al. Segmental mandibular reconstruction by distraction osteogenesis under skin flaps. Int J Oral Maxillofac Surg. 1998;27:9–13. doi: 10.1016/S0901-5027(98)80087-8. [DOI] [PubMed] [Google Scholar]
- 19.Fukuda M, et al. Two stage distraction osteogenesis for mandibular segmental defect. J Oral Maxillofac Surg. 2004;62:1164–1168. doi: 10.1016/j.joms.2003.11.017. [DOI] [PubMed] [Google Scholar]