Abstract
We systematically mistreat psychological phenomena, both logically and clinically. This article explores three contentions: that the dominant discourse in modern cognitive, affective, and clinical neuroscience assumes that we know how psychology/biology causation works when we do not; that there are serious intellectual, clinical, and policy costs to pretending we do know; and that crucial scientific and clinical progress will be stymied as long as we frame psychology, biology, and their relationship in currently dominant ways. The arguments are developed with emphasis on misguided attempts to localize psychological function via neuroimaging, misunderstandings about the role of genetics in psychopathology, and unfortunate constraints on health-care policy and clinical service delivery. A particular challenge, articulated but not resolved in this article, is determining what constitutes adequate explanation in the relationship between psychology and biology.
Keywords: Causation, dualism, psychopathology, psychophysiology, mental health policy
The headlong rush in recent decades to construe a host of psychological events as being biological events or being reducible to them is, at best, premature. This construal is rampant in scholarly and public spheres, it is indefensible based on available theory and data, and it is at least very suspect on logical grounds. That is, the scientific basis for it is far from adequate, and it can be argued that it could never be adequate. The problem extends well beyond psychopathology, although that is a domain with particularly high stakes, because the misconstrual is doing severe damage to clinical science, clinical practice, and public policy, including federal research-funding and health-care-policy priorities in the biobehavioral sciences, with consequences for fostering mental health and preventing and treating mental illness.
To date, no fully developed demonstration of a mechanism by which psychology or biology affects the other has been offered. In fact, we know little about how (e.g., Rose, 2009) or whether (e.g., Miller, 1996) neural events drive psychological events, or the converse. We tend to believe that we have strong presumptive evidence that such causal relationships exist. There are a host of demonstrations of experimental and natural manipulations that we think of as psychological apparently altering dependent measures that we think of as biological and a host of demonstrations of manipulations that we think of as biological apparently altering dependent measures that we think of as psychological. But the evidence for these being causal relationships is only circumstantial. Perhaps we should not be so certain about the fact or direction of causation without the mechanisms having been fully identified. Intellectual modesty is in order.
This issue of psychology–biology relationships arises quite generally but is particularly important in psychopathology. Doing and supervising perhaps 2,000 assessments of acute psychiatric inpatients persuades me that delusions and hallucinations sometimes occur in the context of mental illness. This belief is based not simply on patients’ statements and other overt behavior but on my interpretation of those data. In part, I try to understand the mechanisms by which that observable behavior is produced. By “mechanisms,” I mean, most immediately, relevant psychological events. The concept of mechanisms is itself controversial, but relevant here is that there is no need to confine the scope of mechanisms of mental illness to biological mechanisms (C. Wright & Bechtel, in press). As will be developed below, psychological mechanisms are logically more proximal, in general, to psychopathology and warrant at least as much attention.
I believe that cognitive dysfunction and emotional dysregulation contribute to and result from delusions, hallucinations, and a wide variety of other symptoms of mental illness. My belief that psychological symptoms occur is not based in the least on psychophysiological methods such as functional magnetic resonance (fMRI), magnetoencephalography (MEG), or electroencephalography (EEG) or on endocrine, genetic, immunological, or autonomic measures. My construal of a cluster of observed symptoms as evidence of psychosis does not arise from or depend on any assumptions about biological events. I nevertheless believe that biological events occur and that understanding them will prove essential in understanding, ameliorating, and preventing mental illness. I have no doubt that biological events unfold along with the psychological events, but the cognitive dysfunction, emotional dysregulation, and other symptoms are psychological.1
I can decide that a person I talk with has a delusional conviction. I do not need to observe the conviction (I do not even need the conviction to be the sort of thing I could observe). As a clinician using scientific methods in my service delivery, I do need to observe (public) evidence of a delusional conviction. Such evidence would typically be statements the person makes, actions taken, associated biological events, and contextual information I have about the reality basis of (as one patient told me) the Vaseline coating he applied to his radiator to block the efforts of the Soviets to spy on him.
The present discussion considers recent trends in what is commonly viewed as adequate explanation of relationships between psychological and biological phenomena and discusses how satisfactory they are likely to prove. In diagnostic interviews and some types of psychotherapy, we often ask the patient for an account of their behavior or of their fate. Even in cooperative, nonpsychotic patients the typical response falls short as a thorough account. Acute inpatients will often provide accounts of how they came to be hospitalized that are strikingly inadequate: “I needed help with ideas” or “The police didn’t know what else to do with me.”
Science should do better, but recent cognitive/affective/clinical neuroscience literature routinely offers interpretations of data with respect to psychological–biological relationships that are not remotely adequate accounts. In many cases, the shortcomings are so severe that what is offered is no sort of account at all, on logical grounds. In daily conversation we are normally forgiven for poor insight about our behavior. As Nisbett and Wilson (1977) famously suggested, many such reports appear to be deductions from one’s theory of oneself rather than valid, disinterested observations. In the same vein, Dennett (1982) characterized individuals as “effortlessly inventing intentional interpretations of our own actions in an inseparable mix of confabulation, retrospective self-justification and (on occasion, no doubt) good theorizing” (p. 70, emphasis in original). Perhaps we would want to hold scientists to a higher standard in their accounts of the phenomena they study, but it is evident from our literature that we do not.
Amundson (2006) cited reliance on “a concept of causation that skips over the unobserved insides of a complex hidden process” (p. 11). Pearl (2009,) noted “the unfriendly semi-formal way in which causal analysis has been presented to the research community…” (p. 102). Is our present lack of an in-depth examination of causal mechanisms merely a function of practical limitations that, in time, will surely be surpassed? Or is it a logical problem, and no amount of experimentation or engineering will provide sufficient evidence? Either way, are we okay ignoring it while we get on with scientific and clinical efforts? Three contentions are examined in this article: that the dominant discourse in modern cognitive, affective, and clinical neuroscience assumes that we know how psychology-biology causation works when we do not; that there are serious intellectual, clinical, and policy costs to pretending that we do know; and that crucial scientific and clinical progress will be stymied as long as we frame psychology, biology, and their relationship in currently dominant ways.
The Dominant Discourse: How Psychology–Biology Causation Works
Can We Simply Equate the Concepts?
We know that, given a gas in a fixed, closed space, heat will increase the pressure. That observation can be seen as providing circumstantial evidence of heat playing a causal role in pressure, but it does not provide a mechanistic account of how it does so. Based on additional work, we can spell out the relevant mechanism at various degrees of granularity, and as a result we are quite satisfied that there is a causal relationship between heat and pressure. Such a thoroughly worked out story of the causal mechanisms is lacking for phenomena we view as involving both psychological and biological phenomena.
Relevant science abounds with demonstrations that we take to imply causal relationships between psychology and biology. The “how” of those causal relationships—the mechanisms—remain a mystery, yet we often write as if we know the mechanisms in scholarly literature and in popular media. Pronouncements such as “depression is a chemical imbalance” or “schizophrenia is a brain disease” became mainstream during the Decade of the Brain and are now widely accepted (France, Lysaker, & Robinson, 2007). According to the then Director of the U.S. National Institute of Mental Health (NIMH; Hyman, 1998, p. 38): “Mental illnesses are real, diagnosable, treatable brain disorders.”
These types of statements confuse whether there is some brain dysfunction (which is clearly so for at least some mental illnesses) with whether the clinical phenomena are adequately accounted for solely in terms of brain dysfunction. This is not possible, given that we conceptualize the clinical phenomena in terms of psychological constructs (Kosslyn & Koenig, 1992; Miller, 1996; see also how the DSM-IV and DSM-V define mental illness). It could be the case that we conceptualize schizophrenia as a brain disorder even though we rely primarily or exclusively on overt behavior and inferred psychological events to diagnose it. But that is not the case for schizophrenia. We conceive and define it as a psychological disorder involving delusions, hallucinations, disorganized speech or behavior, anhedonia, avolition, etc. (American Psychiatric Association, 2000, p. 312). These features are all psychological constructs—not merely symptoms/indicators of schizophrenia but central to the concept (Berenbaum, 1995; Heinrichs, 2005).
One might propose that there is a one-to-one relationship between the psychological phenomenon known as schizophrenia and a particular biological phenomenon. The evidence suggests that such a strong relationship is unlikely, but even such a tight correspondence would not suffice to permit an equation of the psychological and biological, as will be developed below. In the computer world, there is a tight relationship between a series of states of a specific CPU and the algorithm it is pursuing, but neither is reducible to the other. A parallel could be drawn regarding social networking carried out via a network of computers. One’s (social) network is not one’s computer nor its connections to other computers. “A map is not the territory it represents…” (Korzybski, 1958, p. 58, emphasis in original).
One might instead propose to bypass that problem by redeploying the term schizophrenia to refer to the biological phenomenon rather than to the psychological phenomenon to which it conventionally refers. There is nothing wrong with the evolution of terms and their definitions. But it should not happen by fiat, as NIMH and other entities have been trying to accomplish, and in any case it does not alter the phenomenon previously referred to by the term. For example, the phenomenon that a particular usage of the term depression refers to does not change if we redeploy the term to refer to something else, such as the biochemistry associated with depression. If by consensus the term depression refers today to sadness as a psychological state and in 10 years to a brain chemistry state, we have not altered the phenomenon of sadness, nor have we explained it in terms of brain chemistry. Whatever schizophrenia refers to 100 years from now (one certainly hopes it will evolve to mean something much more precise), the (psychological) phenomena it has long referred to will not have changed, will still exist, and will still have the potential to disrupt millions of lives. We do not explain phenomena by changing what the labels we apply mean or by directing our attention to other phenomena.
Lamenting sloppy use of language in the naive biological reductionism of equating biology and psychiatry, Bennett and Hacker (2003) asserted: “The vast majority of neuroscientists already speak and write this way, and none of them offer[s] any explanations of what they mean by ascribing psychological attributes to the brain. Conceptual confusions are built into the received forms of cognitive neuroscientific modes of description” (p. 386, emphasis in original).
This problem in the scientific literature is widely replicated in the popular literature. From a New York Times Op-Ed piece about President Lincoln’s relationship with wife Mary Todd Lincoln: “Lincoln suffered from recurring episodes of what would now be called depression from early childhood onward. In light of what we know today, an effort to link them to emotional disappointments rather than to a chemical imbalance seems quaint rather than scientific” (Schreiner, 2006, p. A19). Life stressors do not contribute to depression? In the research literature, there is no doubt about an association between “emotional disappointments” and depression (Kendler, 2005a; Monroe & Reid, 2009). The problem in the quoted article is not the suggestion that chemistry is relevant but that it is sufficient as a conceptualization of depression and that we can dismiss psychological factors as “quaint rather than scientific.”
We mean so much more than biochemistry when we consider psychological phenomena; sometimes we do not mean anything biological at all. The phenomena that “fear” typically refers to include a functional state, a cognitive processing bias, and a variety of judgments and associations that are conceived psychologically. Fear as a state or a disposition is not something we can observe directly. Per the widely accepted three-systems model of Lang (1968), we may infer fear from language expression, overt behavior, and diverse central and peripheral biological phenomena (see also Cone, 1979; Hempel, 1966; Kagan, 2007; Kozak & Miller, 1982; Lang, 1964, 1978; Miller & Keller, 2000; Miller & Kozak, 1993). Whatever we learn about biological phenomena in fear, surely we will still want to communicate about psychological aspects of it. We should not confuse psychological and biological events. “The aim is not to replace a description of mental events by a description of brain activity. That would be like replacing a description of architecture with a description of building materials. Although the nature of the materials restricts the kinds of buildings that can be built, it does not characterize their function or design” (Kosslyn & Koenig, 1992, p. 4). Mental events are “not the same thing as neural activity; phenomenological experience cannot be described in terms of ion flows, synaptic connections, and so forth” (Kosslyn & Koenig, 1992, p. 432). “It is a basic, if usually unspoken, tenet of modern behavioral science that physiological and psychological processes are not alternative explanations of behavior but parallel explanations” (R. Wright, 1987, p. 15). “[Mental events] and brain events are members of different [logical] categories, and one cannot be replaced by the other…. Any theory of consciousness must describe a phenomenon that cannot be replaced by a description of brain events.” (Kosslyn & Koenig, 1992, p. 432; see also Kagan, 2007; Kozak & Miller, 1982; Miller & Kozak, 1993; Luchins, 2004; Marr, 1982; Miller & Ebert, 1988; Miller & Keller, 2000).
Yet in line with Director Hyman’s (1998, p. 38) declaration that “Mental illnesses are…brain disorders,” in the Decade of the Brain, NIMH revamped its construal of mental illness as if it were biological illness. One might wonder whether the National Institute of Mental Health is now misnamed. For example, in 2003, NIMH’s Clinical Neuroscience Research Branch consisted of three research areas: the Molecular and Cellular Basis of Schizophrenia, Mood, and other Brain Disorders Program; the Integrative Neuroscience of Schizophrenia, Mood and other Brain Disorders Program; and the Developmental Neuroscience of Schizophrenia, Mood and other Brain Disorders Program (www.nimh.nih.gov/diva/index.htm#cnrb, accessed 4/26/03). These program titles clearly construe schizophrenia and mood disorders as brain disorders. They do not convey merely that there is brain dysfunction in schizophrenia and mood disorders, possibly of paramount importance in understanding, preventing, or treating these (psychological) disorders. They equate them. As has been argued by numerous philosophers and scientists and summarized in this article, this is nonsensical.
When Kety, Rosenthal, Wender, and Schulsinger (1968) provided the decisive data for a genetic story in schizophrenia, the phenomenon for which they made their case was a psychological disorder, not a brain disorder. They claimed to examine “the prevalence and nature of mental illness” (p. 346). Deciding that there is a crucial genetic or brain story to be told about schizophrenia—which could be essential to understanding, preventing, or treating it—does not mean that the biological story accounts for, replaces, or simply is the psychological story (Miller, Elbert, Sutton, & Heller, 2007a). Conversely, considerable research indicates that variations in one’s social network affect one’s physical health, but we have no idea what the causal mechanisms are (Cohen & Janicki-Deverts, 2009). We do not handle this challenge by declaring that physical health actually is a person’s social network. Recent compelling evidence suggests Gene × Environment effects and gene–environment correlations (genetically influenced differences in environmental exposure) at work in the development of conduct disorder and related problems (Dodge, 2009; Moffitt, Caspi, & Rutter, 2006). Yet it would be incoherent to suggest that the environment is really the individual’s genome or vice versa.
This now-pervasive error of attempting to declare that the psychological is the biological that emerged from the first Decade of the Brain was not confined to one renegade NIMH Director. Writing in Science, the then Director of the National Institute of Drug Abuse (NIDA) stated that “addiction … is fundamentally, a brain disease.” (Leshner, 1997, p. 46). But, in fact, addiction is fundamentally a psychological phenomenon, “a disease of learning and memory” (Hyman, 2005, p. 1414), “a common and costly … behavioral disorder” (McGue, 1999, p. 109), and an inclination to behave in a particular way—a behavioral disposition, which is a property of behavior, not of brain.
The complete sentence from Leshner (1997) is “That addiction is tied to changes in brain structure and function is what makes it, fundamentally, a brain disease” (p. 46). Leaving aside the vagueness of the meaning of “tied to” (what is not tied to what, in nature?), it is not apparent that mere correlation between psychological events and biological events makes the psychological events biological events. Notably, NIDA’s more recent intentions seem to have broadened from a focus on narrowly drawn animal models emphasizing biological mechanisms to include indisputably psychological phenomena in the domains of cognition and emotion, with a growing emphasis on human cognitive and affective neuroscience in its research portfolio. Just as Hyman (2005), running Harvard University as Provost post-NIMH, backed away from his 1998 biological reductionism, Leshner (2007), running the American Association for the Advancement of Science post-NIDA, noted that “there is no evidence that we will be able to understand all aspects of the mind simply in molecular neurobiological terms” (p. 953). However, the present NIDA Director has nevertheless described drug addiction as “a disease of the brain” on the grounds that scientists have found “long-lasting changes in the brain of individuals addicted to drugs” (Volkow, 2005, p. 1401) —mere correlation. By that reasoning, research documenting structural and functional brain changes after aerobic exercise (e.g., Kramer & Erickson, 2009) would lead to the characterization of exercise as a brain phenomenon. And the present NIMH Director is on board: “Mental disorders are brain disorders” (Thomas Insel, speaking at the April, 18, 2008, NIMH Professional Coalition for Research Progress meeting, Washington, DC, quoted by Bruce, 2009, p. 41) and “…depression is fundamentally a brain disorder” (Insel, 2010, p. 46).
Such extreme biological reductionism produces confusion that is rampant not only in high-profile policy outlets connected with the National Institutes of Health (NIH) but in conventional scholarly presentations, even by some of the most prominent psychopathology scientists. “The word mind refers to those functions of the body that reside in the brain” (Andreasen, 1984, p. 219, emphasis in original). But, as argued below, the mind is not the sort of entity that resides anywhere in space. In a single article, Harrison and Weinberger (2005) stated that “schizophrenia is beyond doubt a brain disease” (p. 41), stated that “schizophrenia is predominantly a genetic disorder” (p. 43), referred favorably to “the view of schizophrenia as a disorder of synaptic signalling” (p. 56), and concluded that “The evidence … is consistent with the view that the disorder is fundamentally one of abnormal information processing at the highest level…” (p. 57). How does one square the claim that psychopathology is about “information processing at the highest level” —obviously a psychological phenomenon—with the claim that “schizophrenia is beyond doubt a brain disease”? In fact, each of Harrison and Weinberger’s characterizations could be sound, and generative, if not treated as mutually exclusive. A common problem is that one or another is offered, in isolation, as the definitive characterization rather than a promising characterization of part of the overall story—perhaps different stages or threads in a single causal chain, if there IS a single causal chain. (Do we need there to be just one?) Suffice to say that the field has not sorted this out.
This chaos2 now permeates presentations aimed at the public. A popular personal investments columnist referred to “…the hippocampus, a part of the brain where long-term memory lives” (Zweig, 2007). But as discussed below, memory does not “live” anywhere—it has no specific physical location. A public-aimed Web site for a university clinic applies “leading-edge research to the clinical treatment of children who suffer from biological brain diseases such as bipolar disorder, depression, autism, and schizophrenia” (www.psych.uic.edu/clinical/child.htm, accessed 10/29/07). Numerous similar examples are readily available. Again, such statements that psychological events are nothing more than brain events, for all their recent popularity, are logical errors.
Psychological pathology is not neural pathology. Redefining terms to avoid fundamental conceptual problems does not advance science.
Does One Phenomenon Underlie the Other?
One step away from treating psychological and biological terms as identities is to cast biology or psychology as something that “underlies” the other; as the “foundation,” “substrate,” or “neural basis”; or as “underpinning” the other: “the brain is the seat of our drives, temperaments and patterns of thought” (Pinker, 2009). Such terms could be arrayed along ordinal scales of imageability and vagueness. (“Seat” would fall well along both dimensions.) To borrow a judgment from C. Wright and Bechtel (in press) about terms such as “demonstrate,” “reveal,” and “indicate”: construals such as “underlie,” “biological basis,” and “neural substrate” seem “particularly counterproductive; for they are typically left as semantic or conceptual primitives, and are not clarified, characterized, or given meaning over and above [their presumed] intuitive” appeal, begging the question of the relationship between psychological and biological phenomena. These and similar construals, now commonplace, typically convey that biological phenomena are somehow more fundamental than psychological phenomena, a view criticized long ago by Jessor (1958, p. 170) commenting on a then “recent upsurge of interest in physiological determinants and physical models of behavior….” Miller (1996) and Lilienfeld (2007) emphasized the growth of this view in parallel with (and surely in part due to) the growth of neuroimaging research.
What can now be called the Decades of the Brain (Miller, 2009) have thus brought us another such surge. From the NIMH Web site in 2009: “The Clinical Neuroscience Research Branch supports programs of research, research training, and resource development aimed at understanding the neural basis of mental disorders.” (www.nimh.nih.gov/datr/a3-ns.cfm, accessed 1/18/09). This might be seen as progress from the 2003 Web page for the NIMH Clinical Neuroscience Research Branch, quoted above, which equated psychological and biological disorders. In 2009, they are at least treated as distinct entities. But this notion of neural basis, implying reduction of psychological events to biological events, is not viable either.
According to current NIMH Director Insel (2010): “…the latest research shows that the malfunction of entire [brain] circuits may underlie many mental disorders” (p. 44). Other examples abound: “Conclusive evidence that stress indeed may cause depression requires demonstration that this condition can derail cerebral circuits supposedly underlying depression or certain depressive features” (van Praag, 2004, p. 892). This bold claim says that no amount of correlation suffices to establish causation, which is fair enough. But it goes further and says that we have to identify the neural mechanism by which stress causes depression to be sure that stress causes depression. That precludes any possibility of a purely psychological account of stress fostering (psychologically or biologically conceived) depression. Yet this stance also assumes that there could be psychological stressors that affect biology, without explaining how. At some early point in the causal chain, events apparently would be thought of as psychological, and at some later point they would be thought of as biological. Where is the transition, and how does it work?
“Although political views have been thought to arise largely from individuals’ experiences, recent research suggests that they may have a biological basis.” (Oxley et al., 2008, p. 1667). These opening words in a Science article imply that we must choose between psychological and biological accounts, that biological stories can be adequate accounts of psychological phenomena (political views), and that cognitive neuroscience data (here, electrodermal response and blink amplitude) can establish such an account. The second sentence of that article (“We present evidence that variations in political attitudes correlate with physiological traits”) invites no quarrel—it simply summarizes the data. But the narrative jumps from that correlation to causation—to “a biological basis.” No argument is provided against the possibility that instead the “individuals’ experiences” alluded to drove the physiology, which presumably would be interpreted as showing that political views (and neural events) have a psychological basis. Late in the article, it is noted that the results “do not permit firm conclusions concerning the specific causal processes at work” (p. 1669). In fact, they provide no information at all about the nature of such processes. The mechanism by which biological factors would drive the attitudes is not addressed. (See Aue, Lavelle, & Cacioppo, 2009, for a critique of other issues that arise in neuroimaging studies of political attitudes.)
It has long been clear that both pharmacological and psychological treatments can lead to changes in brain activity and, in some cases, the same changes in brain activity. For example, Baxter et al. (1992) reported similar changes in caudate nucleus activity assessed by positron emission tomography (PET) following drug versus behavior therapy for obsessive-compulsive disorder. Borkovec, Ray, and Stober (1998) found that psychotherapy normalized excessive EEG beta-band activity recorded over the left frontal cortex. Cognitive behavior therapy normalized hypoactive anterior cingulate cortex (Goldapple et al., 2004). Using MEG to study the functional anatomy of sensorimotor cortex in musicians undergoing treatment for focal hand dystonia, Candia, Wienbruch, Elbert, Rockstroh, and Ray (2003) reported that the representational cortex can be modified by successful behavior therapy. Schauer, Elbert, Gotthardt, Rockstroh, Odenwald, and Neuner (2006) altered brain activity with narrative exposure treatment of PTSD. Kolassa and Elbert (2007) provided a review of studies of PTSD-related trauma as an apparent driver of neural plasticity. Schienle, Schaefer, Stark, and Vaitl (2009) demonstrated fMRI-recorded brain changes as a function of cognitive behavior therapy for phobia, and Felmingham et al. (2007) did the same for PTSD. McNab et al. (2009) reported changes in cortical dopamine receptor density as a function of working-memory training. Popov, Jordanov, Rockstroh, Elbert, Merzenich, and Miller (2011) showed MEG-recorded brain changes as a function of auditory discrimination training in schizophrenia. These are a few of the many examples of psychological events apparently driving biological phenomena.
Thousands of studies show psychophysiological relationships (psychological independent variables, physiological dependent variables). To interpret these results generally as meaning that the biological “underlies” the psychological is at best premature and is often an example of what Poldrack (2006) criticized as reverse inference (i.e., affirming the consequent). As a premise for cognitive, affective, and clinical neuroscience, it is not self-evident that biological data underlie psychological data, or that mental disorders have a neural basis. A given theory may explicitly propose such a relationship, but it must be treated as a proposal, not as a fact inherent in or entailed by data (Miller & Ebert, 1988). Biological data provide valuable information about psychological phenomena that may not be obtainable with self-report or overt behavioral measures (Lang, 1968), but public biological data are not inherently more fundamental, more accurate, more representative, or even more objective than public psychological data.
The reductionism implicit in common uses of underlying warrants some explication. A concept defined in one domain is characterized as being reduced to concepts in another domain (called the reduction science) when all meaning in the former is captured in the latter (Churchland, 1986; Hempel, 1966; Jessor, 1958; Teitelbaum & Pellis, 1992). The reduced concept thus becomes unnecessary. (This is sometimes more specifically called eliminative reductionism, distinct from less thoroughgoing types; see France et al., 2007, and Lilienfeld, 2007, for discussions in the context of cognitive neuroscience and psychopathology.) “A reductionist view concerning psychology holds, roughly speaking, that all psychological phenomena are basically biological or physico-chemical in character or, more precisely, that the specific terms and laws of psychology can be reduced to those of biology, chemistry, and physics.” (Hempel, 1966, p. 106). Hempel’s analysis (1966) concluded that “a full reduction [of psychology to biology] is not remotely in sight” (p. 110). D. Ross and Spurrett (2004b) concurred: a “return to reductionism would be disastrous for the cognitive and behavioral sciences, requiring the dismantling of most existing achievements and placing intolerable restrictions on further work” (p. 603). For example, “reduction [of cell biology] to molecular biology seems impossible because key biological phenomena such as ‘signal sequences’ are multiply realized and context dependent, and because functional roles specified in biological terms are indispensable” (p. 614). D. Ross and Spurrett (2007) went on to argue specifically against the assumption that other sciences can be reduced to physics:
… such reductive physicalism is not at all well supported by contemporary science. Most types of entities and relations that feature in interesting scientific generalizations in [other] sciences do not decompose into types and relations featuring in generalizations of fundamental physics. All that the state of current science justifies in this philosophical neighbourhood is the weaker principle that physics provides constraints on other sciences (p. 65).
It is important to note in this analysis of the notion of mechanism in psychopathology that identification of explanatory mechanisms is not reductionistic (C. Wright & Bechtel, in press):
…a mechanistic explanation is non-reductionistic: explanations at a lower level do not replace, sequester, or exclusively preside over the refinement of higher-level explanations, because mechanisms … involve real and different functions being performed by the whole composite system and by its component parts. Rather than serving to reduce one level to another, mechanisms bridge levels. [Reductionistic] and mechanistic approaches [to explanation] … diverge in important respects…. Mechanistic explanations relate levels, but the relation proposed contrasts sharply with philosophical accounts of intertheoretic reduction that relate levels in terms of the reduction of pairwise theories.
Two general distinctions are helpful here. First, Fodor (1968) distinguished between contingent and necessary identity in the relationship between psychological and biological phenomena. A person in any given psychological state is momentarily in some biological state as well. Fodor characterized this as a contingent identity between the psychological and the biological. In such a relationship, the psychological phenomenon implemented in a given neural structure or circuit is not the same as, is not accounted for by, and is not reducible to that circuit (Fodor, 1968; Jessor, 1958).
There is likely an indefinite set of potential neural implementations of a given psychological phenomenon. Conversely, a given neural circuit may implement different psychological functions at different times or in different individuals. Thus, in Fodor’s terminology, there is no necessary identity between psychological states and brain states. It appears that distinct psychological and biological theories are needed to explain phenomena in each of these domains, and additional theoretical work is needed to relate them.
The second general distinction is between intervening variables and hypothetical constructs (MacCorquodale & Meehl, 1948). If, for example, the meaning of the (traditionally psychological) term fear is entirely representable in language about autonomic physiology, we do not need the (psychological) term fear. We might retain such a psychological term as a convenience, but logically it is unnecessary. If a term has no content or meaning beyond other terms in combination with the operations on those terms by which the term is defined, it is said to be an intervening variable (Hempel, 1966). For example, the statistical standard deviation of a sample contains no information not in the sample from which it is computed. In contrast, some terms have meaning that cannot be fully reduced to other terms and are said to be hypothetical constructs (for discussion of this distinction in psychopathology and neuroscience, see Kozak & Miller, 1982; Miller, 1996; Miller & Kozak, 1993; for a critique of intervening variables as sufficient in scientific theory, see Hempel, 1966, Section 7.5). This distinction is very similar to that between latent and manifest variables (Ruscio & Ruscio, 2004). Critically, hypothetical constructs about which one makes inferences based on public data are not, in general, reducible to intervening variables. “Reichenbach showed that statements concerning inferred entities…are not deducible from the class of observational statements…. This distinction [between latent and manifest variables] is not a matter of taste nor of one’s philosophy of science but, as Reichenbach showed, it is a logical and semantic difference” (Meehl, 2004, p. 40).
If fear is just an intervening variable, a mere summary of other things with no meaning beyond those other things, then it is plausible to delete it from our vocabulary. The present contention is that claims that fear or psychosis or depression are just chemical imbalances or are genetic are untenable. We use terms such as fear (or psychosis, depression, aspiration, shy, aggressive, attachment, etc.) to refer to such a diverse and indefinite set of phenomena that there is no possible enumeration of its constituents or indicators that sufficiently represents its meaning. Prior to the era of infatuations with neuroimaging and the human genome, this was widely understood, as articulated in the widely cited paper on fear by Lang (1968). Fear is a hypothetical construct, irreducible to biological (or other psychological) terms (Kozak & Miller, 1982; Miller & Kozak, 1993). By analogy, the concept of a mousetrap is such that building a better one necessarily involves reaching beyond the traps already invented. The fact that we can build a better one means that the concept of a mousetrap cannot be adequately represented by a mere enumeration of all known mousetraps already invented (Fodor, 1968; Kozak & Miller, 1982). What the concept refers to is larger than any such tally. It is a hypothetical construct, not an intervening variable.
The amygdala appears to be crucially involved in fear (M. Davis, 1989; LeDoux, 1995), and the hippocampus appears to be crucially involved in relational memory (Cohen & Eichenbaum, 1993; Hanlon et al., 2005). But the amygdala is not the neural basis of fear, and its neighbor the hippocampus does not underlie memory. In a given case—perhaps even in all imaginable cases of conventional humans—there may be a contingent identity between memory encoding and hippocampal activity. That does not mean that we can reduce memory encoding to hippocampal activity. The latter is simply not what we mean by the former.
The argument here is not that it is merely inconvenient to enumerate all possible instances of memory encoding, so that we keep the concept around merely as a convenience. The argument is that no amount of enumeration of brain states or brain processes can fully capture what we mean by memory encoding (see also Aron et al., 2007, Fodor, 1968, and Teitelbaum & Pellis, 1992). Furthermore, the present argument is not that we do not yet know how to do the enumeration or how to represent (every instance of) memory encoding in terms of hippocampal (or other brain) events. The argument is that memory encoding refers to nothing about brains at all, though what it refers to is routinely implemented in brains. In fact, at some future time we may have the brain story so well worked out that we focus our efforts on controlling allergens, gene expression, or physical deprivation as a way to manipulate hippocampal function. We may no longer have much use for a (psychological) theory of hippocampal function. But a theory about gene expression or hippocampal function cannot be a (complete) theory of memory encoding, because memory encoding is a psychological phenomenon.
In psychopathology a classic example was the misnamed “dopamine theory of schizophrenia.” (For a recent iteration, see Howes & Kapur, 2009.) It never was and never could be a theory of (the whole of) schizophrenia. It was a theory of how biochemistry goes awry in schizophrenia. It did not provide a mechanism for how biochemistry could account for the (fundamentally psychological) features of schizophrenia. It could not, because we have not identified a causal bridge between biochemistry and psychological phenomena such as delusions, and there may not be a causal bridge to find.
Dolan (2002, p. 1191) suggested that “a neurobiological account of fear, anger, or disgust is an increasingly urgent need.” The present contention is that there can be no comprehensive neurobiological account of emotion, because emotion refers to something psychological. What we can aim for is a neurobiological account of what the brain and the periphery are doing in emotion. Surely that goal is intriguing and valuable, but it could not be a full account of emotion, which is a psychological construct.
In stating that a Turing machine stores information, we have accepted that the implementation of such a machine is at most tangentially relevant and not defining, because the definition of a Turing machine depends not in the least on any physical implementation. In fact, we could conceive of a Turing machine even if we could not conceive of building one. We conceive of unicorns, though we believe that there are no unicorns. Not only do we not need to have an actual implementation of a hypothetical construct to conceive it, we do not even have to be able to implement it in principle. Thus, working out an instance of the implementation of, say, memory encoding in the brain does not reduce memory encoding to brain events. We have identified a contingent identity, not a necessary identity.
Though far less common at present, the converse of the naive biological reductionism that has become widespread in the Decades of the Brain also occurs (Taitano & Miller, 1998): the assumption that psychology underlies or is more fundamental than biology. Zuckerman (1999) noted a long tradition of ignoring biological phenomena in clinical psychology: “One thing that both behavioral and post-Freudian psychoanalytic theories had in common was the conviction that learning and life experiences alone could account for all disorders….” (p. 413) This view implies that psychology underlies biology. One does not have depression because one has a chemical balance, one has a chemical imbalance because one is depressed, just as one gasps at the view because it is beautiful (ne does not find the view beautiful because one gasps). Psychology is thus where one should work in order to explain psychopathology, with biological measures of interest merely to the extent that they inform the psychological theorizing. A consequence is that cognitive theory can evolve without the constraints of biological plausibility. As suggested (not seriously!) at the midpoint of the Decade of the Brain, such a view would justify a Decade of Cognition (Miller, 1996). The American Psychological Association (1998) attempted to declare 2001–2010 the Decade of Behavior (without much impact). Emphasizing brain over behavior remains far more captivating of the public imagination. It is not that psychology is a softer science. In fact it is harder (Meehl, 1978; Miller, 2004), and apparently it is too hard to embrace consistently and coherently.
With the growing impact of psychophysiological measures such as fMRI, PET, EEG, MEG, and optical neuroimaging, it has become commonplace to say that biological events underlie (are more fundamental than) psychological events (e.g., “the brain mechanisms underlying bipolar illness,” Satel, 2007, p. A23; “which brain systems underlie emotions?” Dalgleish, 2004, p. 582). This is a pervasive but unsatisfactory way to characterize the relationship between biological and psychological concepts or events. It is not as obviously indefensible logically as is saying depression is a chemical imbalance, but it still takes too much as given. In virtually every instance, one could delete “underlying” or change it to something less committal such as “involved in” or “associated with” without hobbling a paper.
Are There Different Levels of Analysis?
Framing biology and psychology (and other sciences) as addressing different “levels of analysis” is another problematic commonplace but one that is much more tractable than the approaches critiqued above: “…different levels of analysis afford different types of explanations. Some levels of analysis are more informative for certain purposes than others” (Lilienfeld, 2007, p. 265). Just how does the popular “levels of analysis” notion (e.g., Kendler, 2005a, 2005b; Kopnisky, Cowan, & Hyman, 2002; Kosslyn et al., 2002; Marr, 1982) fare as a sufficient means of characterizing the relationship between biology and psychology?
The levels of analysis notion has some problems. What exactly is a “level”? There is no consensus on this (see C. Wright & Bechtel, in press, for an extended discussion). What are they levels of? (“Levels of analysis” implies something else being analyzed. What is the thing being analyzed, and what levels does it have?) Then, what is the relationship between levels? Of particular interest here, what are the causal mechanisms between levels, if any? Without explicating those points, the levels of analysis notion is a nice metaphor in place of a substantive position. It is valuable in preventing us from collapsing together domains that are logically distinct, but it does not tell us how to connect them, how (or whether) to make inferences across them.
Exemplifying a related stance, Heinrichs (2005) defined schizophrenia as “a complex biobehavioral disorder that manifests itself primarily in cognition” (p. 229). Terms like biobehavioral and biopsychosocial at least acknowledge the broad span of relevant phenomena with diverse, noncollapsible facets, but they do not take any stand on the relationships among those phenomena. The levels metaphor is gently appealing, seeming to allow all subfields some space at the trough. But it is not by itself satisfactory (Jessor, 1958; Marshall, 2009; Rose, 2009, p. 785, criticized the term “biopsychosocial” as “essentially brainless”). It does not convey what constitutes a level and says nothing about the nature of the relationships across levels. Such relationships need to be articulated, else invocation of the levels metaphor accomplishes nothing beyond establishing placeholders that may not hold. Furthermore, the levels metaphor is particularly problematic as a way to structure an account of behavior: “…human behavioral phenotypes are, if anything, several orders of magnitude more complex than heart disease…” (Turkheimer, Gottesman, & Goldsmith, 1995, p. 149). Thus, simply enumerating levels, without articulating the mechanistic relations among them, is not offering much.
The term underlying can be understood in terms of the levels metaphor: each level underlies the one above. But again simply asserting that there are levels says little. The recent psychophysiological literature provides many other examples in which notions such as underlying and levels beg crucial questions. As noted above, rather than attributing mood changes to activity in specific brain regions, why not attribute changes in brain activity to changes in mood? Given EEG (Deldin, Keller, Gergen, & Miller, 2000) or neuropsychological performance (Keller et al., 2000) findings suggesting reduced right-posterior brain activity in depression, are people depressed because of low right-posterior activity, or do they have low right-posterior activity because they are depressed? Given longstanding EEG (Davidson, 1984) and recent fMRI (Engels et al., 2007, 2010; Herrington et al., 2005, 2010) evidence of frontal-cortex functional lateralization associated with emotional valence and depression, does happiness cause lateralized brain differences, or do lateralized brain differences cause happiness? Pronouncements that there are levels or assertions about what underlies what do not help with these questions. In fact, it is not clear that causation is a fruitful characterization of these psychological–biological relationships (D. Ross & Spurrett, 2004b).
Yet another common approach is to say that psychological and biological phenomena interact. Such a claim begs the question of how they interact and even what it means to interact. The concept of the experience of “red” does not interact with the concept of photon-driven chemical changes in the retina and their neural sequelae, nor with electromagnetic wavelengths. We may propose that those neural sequelae implement or support the perceptual experience of “red,” but by “red” we do not mean the neural sequelae, we mean something psychological: a perception. Every time a person has a perceptual experience of “red”, there is some neural activity. Across all such instances, there may be some consistency in the neural activity. But that would establish only a set of contingent identities, not a single, necessary identity between the perceptual experience of “red” and a particular biology. The psychological–biological interaction view is essentially a variant of the levels metaphor and is no more of a solution.
A variety of other characterizations of the biology–psychology relationship appear in scholarly and popular literature, implying a link without providing an explicit mechanism (or even a hint that there might be a mechanism that would define and establish the link), such as biological events mediating psychological events (e.g., Kagan, 2007). Marshall (2009) provided a very scholarly treatment of these issues and discussed a concept of embodiment as a way to relate psychological and biological phenomena. Kendler (2005b), Lilienfeld (2007), Turkheimer et al. (1995), and others have advocated an explicitly insufficient but generative strategy: a limited, “piecemeal connections” (D. Ross & Spurrett, 2004b, p. 624) agenda in service of “integrative explanatory pluralism,” in which “researchers gradually assemble local linkages among neighboring levels of analysis in a bit-by-bit fashion.” (Lilienfeld, 2007, p. 266) These notions do not try to reduce psychology to biology or to assert causal relations between psychology and biology. Without offering a full mechanism, they are not fully satisfactory, but they make room to proceed: “Mechanistic explanations at each level are partial and constructed piecemeal with a focus toward actual experimental investigation, without overarching concerns that they be fit into grand, large-scale scientific theories; hence, there is no desideratum to provide a complete account of everything that happens.” (C. Wright & Bechtel, in press) This echoes the earlier position of Hempel (1966), adapted to include psychological phenomena: “…mechanism is perhaps best construed, not as a specific thesis or theory about the character of [psychological or] biological processes, but as a heuristic maxim, as a principle for the guidance of research” (p. 106).
Cacioppo, Berntson, and Nussbaum (2008) provided a recent articulation of a long-appealing view in which “…psychological processes represent emergent properties of a [spatially] widely distributed set of component [neural] processes” (p. 62). They proposed the following:
We may well need a new lexicon of constructs that are neither simply anatomical (e.g., Brodmann area 6 vs. Brodmann area 44) nor psychological (e.g., attention, memory), as we usher in a new era of psychological theory in which what constitutes elemental component processes (functional elements) are tied to specific neural mechanisms (structural elements) and in which the properties of interrelated networks of areas may indeed be more than the sum of the parts. (p. 66; see also C. Wright & Bechtel, in press, on emergent properties and D. Ross & Spurrett, 2004a, on skepticism about the concept)
If that is to be a viable path for the field, we are desperately in need of those new constructs. The levels of analysis notion and its cousins do not appear sufficient to shoulder the work.
Does One Phenomenon Implement Another?
While faulting a number of terms characterizing the relationship between psychology and biology, the term implement was repeatedly used. Working from Fodor’s (1968) distinction between contingent and necessary identity, Miller (1996; Miller & Keller (2000) recommended implement as a way to characterize the psychology–biology relationship—viewing cognition and emotion as implemented in neural systems but not reducible to them. This relationship would be the same as that of an algorithm spelled out in software and implemented in hardware.3 There might be an immeasurable variety of ways to generate a random-number series, so the notion of a random-number generator is a hypothetical construct, but no random numbers would arise until a particular algorithm is implemented in hardware. Similarly, there would be no depressed person without a corporeal person to be depressed. Every instance of depression might involve some chemical imbalance—perhaps even a consistent sort of chemical imbalance, perhaps providing a common, contingent identity. But even a very consistent chemical imbalance would not entail a necessary identity between (definitively psychological) depression and biochemistry. This notion of implementation avoids naive reductionism. So, how does this implementation occur? Once again, what are the mechanisms?
The implementation notion as a characterization of the relationship between psychological and biological events is both safe and unsatisfactory because it claims and offers little. Similarly, psychological events have sometimes been described as epiphenomena of biological events. Neural events are sometimes said to support psychological events. These construals do not appear to be problematic, but they also say nothing about mechanism, so they do not resolve present concerns. One can have theories about either software or hardware without paying any attention to the other domain. A core appeal of the concept of a Turing machine is its hardware independence. A scholar can do perfectly good theorizing about software or psychology without in the least considering the silicon or carbon hardware that might implement it. Circuit-board feasibility or biological plausibility is not a precondition of theorizing about software or psychological algorithms. In fact, it may often be crucial to push such theorizing well beyond what seems feasible to implement, in part to provide inspiration and guidance to those who develop the implementations. With that independence, it becomes clear that not only s there no necessary relationship between the software and the hardware but ne can employ the distinction without any comprehension of how to get from one to the other. Nevertheless, specifics of the psychology–biology bridging mechanisms are sorely needed in biological research on psychopathology, if the Decades of the Brain are not to lead us any farther astray.
The term implementation provides no hint of mechanism, in terms of how hardware or software (biochemistry or depression) cause each other. Thus, the notion of implementation does not deliver. It may be an appealing construal of what hardware does with software or what the brain and immune and endocrine and autonomic systems do about psychology, but it is not an account of the translation from software to hardware or from psychological phenomena to biological phenomena. Neither is the functionalism sometimes proposed, where what is psychological is conceived as being the function of what is biological (Churchland & Churchland, 1982; Fodor, 1968; Kozak & Miller, 1982; Lycan, 1982; Miller & Kozak, 1993; D. Ross & Spurrett, 2004b; Teitelbaum & Pellis, 1992). The “how” is where we are blind—blinded by our hopes for leverage over human capacity and illness and by our excitement about the recent march of technology. The notion of implementation as a candidate for characterizing psychology–biology relationships is inadequate, as are all other concepts reviewed here. Implementation, support, epiphenomenon, and functionalism have the virtue of not ignoring important boundaries and distinctions and might suffice if we were give up the goal of accounting for (or even just allowing) causation to occur between biology and psychology, but such causation seems to be a premise of the Decades of the Brain.
Whether it is a necessary premise is questionable. D. Ross and Spurrett (2004b) advocated a functionalism that does not rely on a conventional notion of causation from below and argued that we should look for causation (or, perhaps with less baggage, explanation, or even just the discovery of regularities in nature) in higher level (if one likes the levels metaphor) or more global dynamics as much as we do in lower level, underlying dynamics. Redhead (1990) went further, arguing against needing a concept of causation in science at all. The implication for the present critique is that there are a variety of reasons to question a biological-reductionism approach to causation that dismisses psychological phenomena and seeks to replace them with biological phenomena. Meanwhile, the notions of implementation, support, and their modest cousins seem to be the best we can do for now. In any case, let us choose our verbs carefully, mindful of the baggage they bring (the less baggage, the better).
Misunderstanding Functional Brain Localization
Aspects of the foregoing critiques apply to much of the basis for recent enthusiasm about exciting advances in neuroimaging methods.4 The phrase “localization of function,” very common in the neuroimaging literature, is fraught with peril. Low amplitude of the P300 component of the event-related brain potential (ERP), measured from EEG, is one of the most firmly established biological findings in schizophrenia (Bramon, Rabe-Hesketh, Sham, Murray, & Fangou, 2004; Ford, 1999), and there is considerable consensus on the functional significance of P300, considered in psychological terms (Donchin & Coles, 1988). There is much less consensus about which neural generator(s) produce the electrical activity or about what (distinct?) functions those generators serve across the diverse paradigms that elicit P300. In many cases, neural sources are difficult or impossible to identify with confidence from scalp EEG alone. However, combining imaging modalities such as EEG, MEG, optical methods, and MRI can deliver impressive spatial and temporal localization. EEG or MEG coupled with structural magnetic resonance imaging (sMRI) can achieve spatial localization as good as any other available standard noninvasive method, including fMRI as it is commonly used (though not equal to state-of-the-art fMRI; Miller et al., 2007a). If we understand the distinct functional significance of various neural generators of P300, and if only some generators are compromised in schizophrenia, this can inform us about the nature of not just the biological deficits in schizophrenia but cognitive and affective deficits. This is the case even if we have not fully worked out the neural circuitry that produces (or underlies) P300. Thus, functional interpretations of P300 may tell us things—psychological things—that we do not get from traditional psychological measures. Conversely, what we know about cognitive and affective deficits can inform us about the function of the different neural generators, not only in patients but in general.
Nevertheless, such neuroimaging phenomena do not underlie and are not the basis of the psychological phenomena that define the functions invoked in P300 tasks. Although we may posit that neural generators implement psychological functions, it must be understood that a psychological function does not have location in space (Fodor, 1968; Miller, Engels, & Herrington, 2007b). The now wildly popular goal of spatial localization of psychological functions in the brain is simply not an option (for supporting discussion, see Bennett & Hacker, 2003; Braitenberg, 1984; Fodor, 1968; Kotchoubey, 2005; Miller, 1996; Miller et al., 2007a, 2007b; Miller & Keller, 2000; Teitelbaum & Pellis, 1992;C.A. Ross & Pam, 1995).
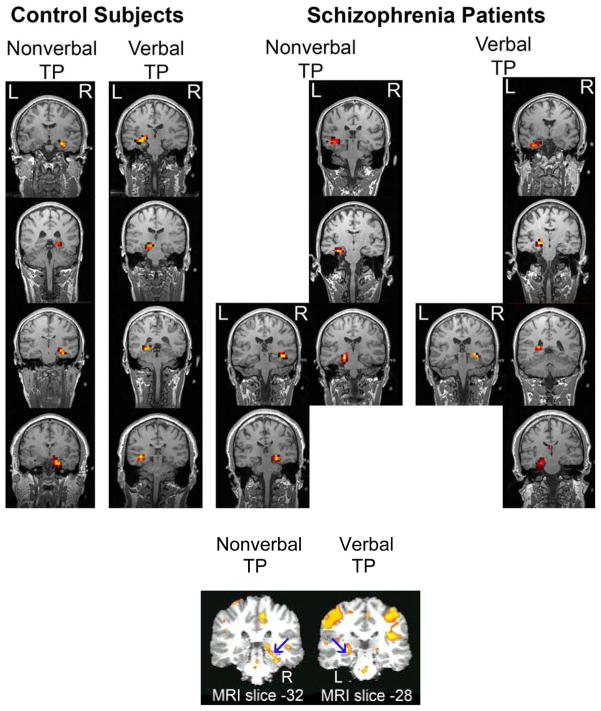
To make this case by example, memory deficits are well established in schizophrenia (e.g., Heinrichs & Zakzanis, 1998). But a memory encoding deficit in schizophrenia cannot be located in a specific brain region. My colleagues and I have provided consistent evidence of a lateralized hippocampal deficit in schizophrenia involving relational memory, using a combination of MEG and sMRI to locate deep brain activity (Hanlon et al., 2003, 2005, 2007; Miller, 2008). The findings were replicated with new participants run on a different MEG machine, using a different MEG source localization algorithm, and cross-validated spatially with a different functional imaging method (fMRI; see Fig. 1). The MEG portion of the work also provided information on the time course of the neural abnormality at a granularity conventional fMRI cannot provide. But this program of research has not demonstrated that the memory deficit is located in the hippocampus. Memory deficits are not the sort of thing that are located anywhere in space. Memory deficits are functional impairments that are conceived in cognitive, computational, and overt behavioral terms, not in biological terms.
Figure 1.
Illustration of localization of task-specific and hemisphere-specific hippocampal activity during nonverbal and verbal variants of a transverse-patterning (TP) task in four nonpatient and four patient individuals. Upper panel: MEG-based localization (each row is one subject). Controls showed consistent lateralization as a function of task. Patients showed less consistent activation. Lower panel: fMRI-based localization, in which blue arrows point to hippocampal activation, lateralized as a function of task (combined analysis for three nonpatients and four patients). Figure is adapted from Hanlon et al. (2007).
The dominant discourse convention in the Decades of the Brain, however, says otherwise. “Cognitive neuroscience…begins with localization within the brain of various cognitive abilities…. It has now become possible to localize mental functions to particular sets of regions….” (Kandel & Squire, 1992, pp. 143–144). There are two problems in these statements from a Nobel Prize winner and a past president of the Society for Neuroscience. The lesser problem is the implication that scientists were not able to associate specific functions with specific brain regions until recently. But this has been possible, in various forms, for decades. One sees this type of “Scientists are now able to…” characterization of scientific progress in the popular press all the time. It misleads the public to think that we are finally on the verge of a decisive breakthrough—often the decisive breakthrough in some area—when in fact most progress is incremental.
The more important problem with the 1992 statement is the claim that we can localize function at all. As argued above, mental events are not the sort of thing that has a spatial location. What we can do (increasingly often and increasingly well) is localize in space a portion of the tissue that seems differentially associated with mental events. “What we can do is correlate a person’s thinking of this or that with localized brain activity…. But this does not show that the brain is thinking, reflecting or ruminating; it shows that such-and-such parts of a person’s cortex are active when the person is thinking, reflecting or ruminating” (Bennett & Hacker, 2003, p. 83; emphasis in original). We cannot spatially localize those functions themselves: “…it makes scant sense to identify the mind with the brain…” (Bennett & Hacker, 2003, p. 105). Functions do not have location.
Poldrack (2008) decried cognitive neuroscientists’ “facile leap to localizationist conclusions” (p. 1). Unfortunately, counting on localizing things that cannot have a location is not confined to the scholarly literature. A social psychology paper in Science ran two interacting participants in MRI scanners simultaneously, with the key fMRI finding that, as trust developed between the two participants, caudate nucleus activation occurred earlier in the trial (King-Casas et al., 2005). In all respects the authors spoke with appropriate caution, but the university press release referred to the caudate activation as “the trust signal” and cited the study as having discovered “where trust decisions occur in the brain” (www.bcm.edu/fromthelab/vol04/is3/05apr_n1.htm, accessed 4/24/05). The popular media set up the study as groundbreaking by claiming that “Trust is a complex phenomena, one that many scientists would think incapable of being studied” (Fountain, 2005, p. A20), but the Science paper said no such thing, claiming much more modestly that trust “would seem to be a difficult part of social cognition to probe rigorously in a scientific experiment” (King-Casas et al., 2005, p. 78). The same popular press report stated that the “…scientists are reporting today that they have succeeded in visualizing feelings of trust developing in a specific region of the brain” (p. A19). So, neuroimaging can localize, in the brain, a psychological phenomenon such as trust? No. Again, fortunately, King-Casas et al. made no such untenable claim.
Under the headline “Area responsible for ‘self-control’ found in the human brain” appeared a story claiming that “The area of the brain responsible for self-control—where the decision not to do something occurs after thinking about doing it—is separate from the area associated with taking action, scientists say in the August 22 issue of the Journal of Neuroscience” (www.physorg.com/news106936688.html accessed March 4, 2010). It is unimaginable in modern cognitive neuroscience, however, that there is a single brain region responsible for self-control.
The rampant misconstrual in the popular press of what neuroimaging studies show is drawing increasing critical attention. Weisberg, Keil, Goodstein, Rawson, and Gray (2008) wrote of “The seductive allure of neuroscience explanations” even to the point of systematically misleading readers. McCabe and Castel (2008) demonstrated that scientific papers are found to be more convincing if they include brain images and concluded that “brain images are influential because they provide a physical basis for abstract cognitive processes, appealing to people’s affinity for reductionistic explanations of cognitive phenomena” (p. 343). The following is from a prominent complaint signed by 17 scholars (Aron et al., 2007) objecting to a New York Times Op-Ed piece:
“The article claimed that it is possible to directly read the minds of potential voters by looking at their brain activity while they viewed presidential candidates…. As cognitive neuroscientists who use the same brain imaging technology, we know that it is not possible to definitively determine whether a person is anxious or feeling connected simply by looking at activity in a particular brain region. This is so because brain regions are typically engaged by many mental states, and thus a one-to-one mapping between a brain region and a mental state is not possible. …we are distressed by the publication of research in the press … that uses flawed reasoning to draw unfounded conclusions about topics as important as the presidential election.”
Trust decisions and political attitudes do not occur in the brain. Decisions, feelings, perceptions, delusions, memories do not have a spatial location. We image brain events: electromagnetic, hemodynamic, and optical. We do not image, and cannot localize in space, psychological constructs. We can make inferences about the latter from the former, using bridge principles that connect observable data and hypothetical constructs. But the latter are not the former. “After all, we now have [neuroimaging] machines that can literally watch the mind at work.” (Watters, 2010). This is not true: EEG, MEG, fMRI, etc. watch the brain at work. What inferences we want to make about the mind based on such data are our constructions, not our observations.5
A (Not So) Special Case: Calling Psychopathology Genetic
Aspects of the foregoing critiques apply to recent enthusiasm about prospects for research on the human genome. The work of some genetic mechanisms seems at present best understood as a simple, monolithic unfolding, the straightforward path of a single gene or set of genes, essentially like Mendel and his peas (let us use gene here to mean any non-null set of genes that for present purposes functions as a unit—a convenient red herring). We often hear reference to “the gene for” some characteristic or behavior, such as blood type or creativity or Alzheimer’s or mania (e.g., “a genetic basis for” psychiatric disorder, “the genes underlying psychiatric disorders”; Abdolmaleky, Thiagalingam, & Wilcox, 2005, pp. 149, 150; “free will genes” and “the molecular details underlying consciousness”, L. Ziga, www.physorg.com/news186830615.html). Often the implication is more than that a gene or set of genes does not have just a nontrivial (perhaps central, perhaps even necessary or sufficient) causal role, but that the relevant genetic story is essentially the entire story.
In fact, however, the story is not so simple, even when it is a lot simpler than it probably is for psychopathology. There might be a single, dominant gene for Type A blood, but to have Type A blood one must have blood, which we do not attribute to that same gene, and to have blood there must be water, which we do not attribute to genes at all. For a particular gene to work (i.e., to matter), there must be other genes and there must also be things that are not genetic, in two senses. Some things are not genetic, in the sense that water is not genetic: It contains no genes, nor does its existence depend on genetic mechanisms. Some things are not genetic in a much more complex sense, which this discussion focuses on and which places severe and unpopular but coherent limits on the meaning of “genetic mechanism”, the apprehension of which is necessary for avoiding the naive reductionism that has become pervasive in cognitive, affective, and clinical neuroscience.
At stake are both substantive, conceptual material about the relationship between psychological and biological phenomena and pragmatic or even political issues about scientific priorities, including research funding priorities and health-care policy. Berenbaum (1995) compellingly addressed the substantive issue:
Although genes will never be sufficient to explain schizophrenia, it is conceivable that a gene or small set of genes will be found to be necessary for the development of schizophrenia. Even if this turns out to be the case, however, the identified gene or set of genes would not constitute an explanation of schizophrenia. The inability of a gene to explain schizophrenia is illustrated in the model of schizophrenia proposed by Meehl (1990). Meehl posits that there is a single major gene that is necessary, but not sufficient, for the development of schizophrenia. Meehl, however, clearly distinguishes between (a) the schizogene; (b) schizotaxia, which he describes as the ‘genetically determined [neural] integrative defect, predisposing to schizophrenia’…; (c) schizotypy, which he describes as a form of personality that develops in all or nearly all schizotaxic individuals; and (d) schizophrenia, which is the psychotic decompensation exhibited by a minority of schizotypes…. Just as infection by the HIV virus is not sufficient to explain AIDS, no gene will ever be sufficient to explain schizophrenia. (pp. 190–191)
The rapidly growing scientific and popular literature on the human genome has promoted the indefensible belief that genes can and eventually will provide an essentially sufficient explanation of psychological dysfunction (Miller et al., 2007a). But we know better (Johnson, Turkheimer, Gottesman, & Bouchard, 2009):
When there are both genetic and environmental differences, most of the mechanisms through which genes exert their causal influences on behavior are not the straightforward one gene–one (bit of) trait association one learns about in high-school biology. Instead, much gene expression is contingent on the presence of other gene products, environmental circumstances, and prior levels of gene expression, sometimes even in prior generations. … even highly heritable traits can be strongly manipulated by the environment… This means that little can be gleaned from any particular heritability estimate. (p. 218)
At some point the enormous momentum manifested in breathless proclamations such as “Now that we have the genome…” and “When we find the gene for…” needs to give way to more nuanced realizations: Environments (broadly conceived) are turning our genes on and off (or dialing them up and down) on a daily, even hourly basis and sometimes damaging our DNA or fostering its repair (Adachi, Kawamura, & Takemoto, 1993; Dimitroglou et al., 2003; Padgett & Glaser, 2003). One’s genes are not the immutable cause typically assumed. It follows that the typical diathesis-stress model, wherein genes are the diathesis and environment is the stressor, can be inverted. Of greater consequence, the debate between nature as main effect and nurture as main effect is over (or should be; Nelson & Gottesman, 2005). Furthermore, at least in mental illness and perhaps in most of psychology, it is becoming clear that the individual-differences action is generally in Gene × Gene interactions, Gene × Environment interactions, and gene–environment correlations, not in main effects (e.g., Gould & Gottesman, 2006; Kendler, 2005a, 2009; Miller et al., 2007a; Moffitt et al., 2006), even for differences between monozygotic twins (Haque, Gottesman, & Wong, 2009). It is also becoming clear that much of the contribution of environment to those Gene × Environment interactions, such as experience-dependent changes in gene function (Champagne & Mashoodh, 2009, p. 127), will be in what behavior geneticists called “unshared variance” (i.e., specific to the individual; McGue, 1999; Turkheimer, 2000).
Walker (2000) outlined the cycle by which psychological environment can affect gene expression, a story available for some time (e.g., reviews by Meany, 2001, and Sapolsky, 1996) but still not widely known:
The chain of events typically involves an environmental event that triggers a neurohumoral response that alters (turns on or off) the transcription of RNA and, thereby, the production of proteins that control other cellular and systematic processes, which, in turn, may affect behavior. …perhaps more than any other field of study, basic research on gene expression has elucidated the critical role of experience and behavior. It is somewhat ironic that advances in molecular genetics may prove to have been a major impetus to increased status for behavioral science. (p. 3)
In light of these considerations, what does a common term such as genetic basis (e.g., Cowan, Kopnisky, & Hyman, 2002) mean for psychopathology, and what does it rule out? A close parallel to the critique earlier about the concept of neural basis applies fully here. In addition to that logical case against such terms, the empirical story about the role of genes in mental illness appears particularly bleak. Not that there is no role—it is clear that there is a substantial role. But it will not be simple to identify, let alone manipulate.
Twin and adoption studies provide compelling evidence of significant genetic effects in virtually all major psychiatric disorders (Kendler, 2005a) and, indeed, throughout psychology (Johnson et al., 2009; Turkheimer, 2000). Yet no specific gene has been identified for any major psychiatric disorder, despite many candidate genes and many studies (Abdolmaleky et al., 2005). In mental illness, “…genetics are only a small part of the story” (Andreasen, 1984, p. 254). Kendler (2005a) provided a compelling case against virtually any simple genetic story in mental illness. He argued that the very notion of “the gene for [some particular mental illness]” is untenable:
…experts agree that for those disorders studied in genome-wide linkage scans of reasonable size and quality - especially schizophrenia, bipolar illness, panic disorder, and eating disorders - conclusive evidence has accumulated that even moderately rare genes of Mendellian-like effect do not exist. (p. 1245)
…current evidence suggests that many genes that influence risk for psychiatric disorders will not be diagnostically specific in their effect…. (p. 1247)
While we find it easy to use the phrase ‘X is a gene for Y,’ it feels quite odd to say ‘A is an environment for B.’ For example, a large body of empirical work supports the hypothesis that severe life events are important environmental risk factors for major depression. The magnitude of the association between such events and the subsequent depressive episode is far greater than that observed for any of the genes that we have reviewed here. Yet, who has heard the phrase ‘a romantic breakup is an environment for depression’? I suggest that we feel comfortable with ‘X is a gene for Y’ and not ‘A is an environment for B’ because we implicitly assume that genes have a privileged causal relationship with the phenotype not shared by environmental factors. However, empirical evidence does not support the position that genes code specifically for psychiatric illness while the environment reflects nonspecific ‘background effects’. (p. 1248, emphasis added).
The impact of individual genes on risk for psychiatric illness is small, often nonspecific, and embedded in causal pathways of stunning complexity. … Although we may wish it to be true, we do not have and are not likely to ever discover ‘genes for’ psychiatric illness. (p. 1250)
It is important to repeat that the critique is not that there are no genes involved in psychopathology. The critique is that typical statements about “genes for” carry an implication of explanatory sufficiency, as in “Once we have the gene for…” or “Now that we have the genome,” implying that identifying relevant genes will suffice for understanding, prevention, and intervention.
Turkheimer (2000) offered a particularly striking case in reflecting on just what the nature of the gene contribution to psychopathology is likely to be. He argued that a large part of it is going to turn out to be in the Gene × Environment interactions (not main effects of genes), with much of the environment appearing in the person-specific (“unshared”) variance. This is not an argument against genes mattering—genes surely matter greatly. It is an argument against our readily being able to nail down the contributions to the mechanisms and against common assumptions in such research to date and in popular-press coverage of it.
The concept of emergenesis (Lykken, McGue, Tellegen, & Bouchard, 1992) is a wonderful example of a rich class of potential genetic (or Gene × Environment) mechanisms that superficially do not follow a Mendelian model. The basic notion is that characteristics or behaviors with a substantial genetic contribution need not “run in families.” If a characteristic or behavior is driven by a rare confluence of multiple genes, the genetic contribution can be real—even very high—yet so rarely manifested in the lineage as to not seem genetic in the usual (simplistic) sense. Add to that Turkheimer’s point about the often obscure contribution that environment will make to Gene × Environment effects, and we have a lesson in humility about discovering specific genetic contributions to psychological phenomena, even though we are convinced of their significance.
The previously discussed Oxley et al. (2008) Science paper about political views and physiological responses did not directly assess genotype (or amygdala function) but nevertheless suggested a genetic causal contribution to political views: “…given that political and social attitudes are heritable and that amygdala activity has also been traced to genetics, genetic variation relative to amygdala activity could affect both physiological responses to threat and political attitudes…” (p. 1669). This appears to be a potentially valid line of argument. The striking thing about it is that it was included in the paper, particularly in the absence of a parallel suggestion about environmental or Gene × Environment interaction or (more interestingly) gene–environment correlation contributions. Why did genes end up in this story? Not because such a role is plausible. An environment contribution is just as plausible. Why cite the one and not the other or, better yet, their combination? “Data about genes that may increase risk for a given disorder will also help unravel the physiological mechanisms involved” (Insel, 2010, p. 50). Certainly, but why not say “unravel the psychological and physiological mechanisms involved”? When the Director of NIMH slights mental phenomena, it has an impact.
It is powerfully appealing to speak in simple terms (“the gene for X” or “Y is heritable”), as if the issue is binary and not dimensional and dynamic nor varying across populations, environments, or time. Yet heritability is not defined for genes. It is defined for genes in a particular population in a particular environment (Johnson et al., 2009). Turkheimer, Haley, Waldron, D’Onofrio, and Gottesman (2003) reported that the heritability of IQ at age 7 varied with socioeconomic status, being essentially zero in impoverished families, whereas poverty is associated with a larger effect of genes on physical health (Johnson & Krueger, 2005). O.S.P. Davis, Haworth, and Plomin (2009) reported a two- to threefold change in heritability of the latent intelligence factor g in a large twin cohort over the short time span from early childhood to middle childhood.
If asking “is g heritable?” means “is g heritable at all, in at least some contexts?”, then the answer is “sure.” But lots of things are heritable in that sense. It is not a very interesting sense. On what does the heritability depend? And what are the mechanisms of the contributions of genes to normal and abnormal psychological function? Presumably the change in heritability over a few years in the O.S.P. Davis et al. sample was not due to changes in what genes the children carried. Very likely, it was also not due to environment alone. Their combination in various forms matters. What are the mechanisms by which genes and environments cause behavior, if indeed causation is a sensible way to describe the relationship of genes, environments, and behavior? Not every study can tackle every question, but so many modern reports are written as if to dismiss so many crucial questions. When we frame things in terms of “the gene for X”, we distract from any plausible role for anything psychological in psychopathology.
The same neglect of contributions from anything other than simple Mendelian genetic effects is readily apparent in popular media. From the New York Times Magazine (Dobbs, 2007): “…genes (or their absence) do not hard-wire people for certain behaviors. There is no gene for understanding calculus. But genes do shape behavior and personality, and they do so by creating brain structures and functions that favor certain abilities and appetites more than others.” There is every indication that environment, Gene × Environment interactions, and gene–environment correlations also shape behavior and do so in part by shaping brain structures and functions. Why are they not cited here as well? As Kendler (2005a) explained, disapprovingly, “because we implicitly assume that genes have a privileged causal relationship with the phenotype” (p. 1248).
Dean (2007) in the New York Times: “…as evolutionary biologists and cognitive neuroscientists peer ever deeper into the brain, they are discovering more and more genes, brain structures and other physical correlates [of] feelings like empathy, disgust and joy” (p. D8). Finding correlates is fine, but the passage continues: “That is, they are discovering physical bases for the feelings from which moral sense emerges—not just in people but in other animals as well.” The phrase “That is” is notable, in that it implies that finding correlates is the same as finding “physical bases.” Just what a physical basis is and why finding it is significant are not discussed. Of course, the present contention is that there is no physical basis for psychological phenomena. There can be a contingent identity, but what could physical basis mean that makes basis the right term? Reductionism looms around every corner.
A regular New York Times columnist lamented this problem without realizing how regularly it arises in his own newspaper:
“…it occurred to me that while we postmoderns say we detest all-explaining narratives, in fact a newish grand narrative has crept upon us willy-nilly and is now all around. … Scarcely a month goes by when Time or Newsweek doesn’t have a cover article on how our genes shape everything from our exercise habits to our moods. Science sections are filled with articles on how brain structure influences things like lust and learning….” (Brooks, 2007, p. A14)
This “grand narrative” is indeed pervasive and both intellectually and politically seductive.
As noted above, it is well established that genes get upregulated and downregulated by environmental events (and by genes and by Gene × Environment interactions), in some cases many times a day. Why is this not widely known, even among relevant scientists, let alone journalists and their readers? It is not hard to grasp, unless one is blinded by premises of a naive biological determinism, with the genome underlying and inexorably driving everything else.
Once we accept that basically everything—not only schizophrenia and intelligence, but also marital status and television watching—is heritable, it becomes clear that specific estimates of heritability are not very important. The omnipresence of genetic influences does not demonstrate that behavior is ‘‘less psychological’’ or ‘‘more biologically determined’’ than had originally been thought; rather it shows that behavior arises from factors intrinsic as well as extrinsic to the individual. The real implications of heritability lie not in questions of relative biological determinism but in revealing the need to understand both the mechanisms through which the individual, whether consciously or not, directs his or her own life course and his or her power to do so. (Johnson et al., 2009, p. 220)
People can disagree about what suffices to demonstrate causality (e.g., Johnson et al., 2009; Pearl, 2009; D. Ross & Spurrett, 2004b, 2007; West & Thoemmes, 2010) or even about “the equivocal nature of the concept of causation itself” (D. Ross & Spurrett, 2004b, p. 619). Redhead (1990, p. 145) observed that there is no consensus among philosophers about the nature of causation. The present concern is not the logical conditions for deducing that a causal relationship likely exists. The present concern is that it has become commonplace to assert naively reductionist causation in the absence of discovery of anything approaching an adequate mechanism of that causation. Claims that mental illness is genes or biochemistry, or that it is essentially determined by them, have become rampant. We sorely need to identify the psychological mechanisms, the biological mechanisms, and the full chain of their relationship(s) before taking a stand on how much of the chain is psychological or biological (or genetic vs. environmental vs. Gene × Environment), before placing bets on where the best points of intervention are, and before making massively skewed commitments of research and health-care resources driven by such bets. At present, absent the mechanisms, our field makes an awful lot of assumptions about mechanisms (especially of psychopathology) when only mere correlations are available for the most part. And, as stated earlier, it should be remembered that, when one is trying to understand inherently psychological phenomena, having only the relevant biological mechanisms is, at best, very incomplete.
Intellectual, Clinical, and Policy Costs
When pressed, many in our field would insist that they are not naive reductionists and that they do not mean that depression is only biochemical or that schizophrenia is only genetic. Then why say or imply such things? At least two factors contribute, beyond the pull (discussed by France et al., 2007) of the pharmaceutical economy.
First, there is very considerable outside interest-group pressure on NIH to cast mental illness in narrowly biological ways (Deacon & Lickel, 2009). For some years highly regarded patient advocacy groups have pressed for a narrowed focus on biological factors, often fostering the same naive reductionism critiqued above. From the Web site of the National Alliance for Research on Schizophrenia and Affective Disorders (NARSAD): “Schizophrenia … is a severe, chronic, and generally disabling brain disease.” (www.narsad.org/?q=node/9/disorder). NIMH’s Web site discusses schizophrenia as one among “other physical illnesses” (www.nami.org/Template.cfm?Section=By_Illness&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=54&ContentID=23036).6
This pressure7 is unquestionably well intentioned but misguided, and it is often motivated in part by the assumption that biological construals of mental illness reduce stigma. Such a prediction would make sense if people tend to be held less responsible for their biology than for their psychology. Why that should be the case is not apparent: Although such a notion of differential responsibility is commonplace, it is not obvious that we have less control over our biology than over our psychology. The genes one has are not one’s responsibility, but we have considerable control over their interaction with the environment, and as argued above, that interaction is where the action is in psychopathology.
In any case, Deacon and Lickel (2009) reviewed evidence that “blaming the victim” is no longer widely practiced with respect to mental illness and that what stigma remains has not been reduced by educating the public to attribute it to biological causes outside the individual’s control. Deacon and Baird (2009) showed that biological explanations can actually foster pessimism about prognosis and psychosocial treatment. Furthermore, R. Wright (1987), Pinker (2009), and others have written of the huge legal and social-policy problems such a stance creates and of the pervasive confusion and injustice that results from legal8 and policy positions that are inconsistent on this important issue of responsibility. Compare (a) “…no one is biologically responsible for their actions.” (L. Ziga, www.physorg.com/news186830615.html) and (b) “The decision to handle mental conditions biologically is as moral a decision as any other” (Menand, 2010).
A second source of pressure on NIMH and NIDA to embrace naive biological reductionism is internal. They are a small minority among (and competing with) numerous other NIH Institutes and Centers, the center of gravity for which are disorders traditionally conceived as biological. Given the widespread premise that biological science is more respectable and more fruitful than psychological science,9 NIMH and NIDA place themselves at a political disadvantage to the extent that they publicize that their primary phenomena are psychological. There are a variety of off-the-record indications that NIMH and NIDA staff have a much more sophisticated understanding of the psychology biology relationship, in both theory and data, than what the public faces of these two institutes convey. To the extent that they show those cards, they risk losing leverage for funding and policy direction.
Acknowledging these very real and substantial pressures on NIMH and NIDA leadership, a variety of significant consequences for clinical research and intervention arise from miscasting the psychology–biology relationship. In the psychopathology and treatment research literatures, a common but unfortunate assumption is that dysfunctions conceived biologically require biological interventions and that those conceived psychologically require psychological interventions (Miller, 1996; Taitano & Miller, 1998). “While episodes of illness are sometimes triggered by unfortunate life events, the basic causes lie in the biology of the brain. The best way to treat these biological abnormalities…is to correct the underlying physical abnormality, usually through the use of somatic therapy.” (Andreasen, 1984, p. 249) If the premise is that depression is a chemical imbalance, it is understandable that one might assume that a chemical intervention is warranted. Yet the best way to alter one system may sometimes be a direct intervention in another system. Even, for example, if catecholamines were the best place to intervene in depression (which one might believe without assuming that depression is a chemical imbalance), it does not follow that a direct biological intervention in that system would be optimal for an individual (Kagan, 2007; Lilienfeld, 2007; Miller, 1996). As noted above, studies of pharmacological treatment and/or psychotherapy for anxiety have demonstrated that psychotherapy appears to cause changes in EEG (Borkovec et al., 1998), that cognitive behavior therapy normalizes hypoactive anterior cingulate cortex (Goldapple et al., 2004), and that medication and psychotherapy appear to have similar effects on PET-assessed brain activity (Baxter et al., 1992). Drug abuse clearly involves chemistry, yet psychotherapy has been found to be more effective than medication in treatment of drug abuse (Carroll & Onken, 2005).
Often, even in high-level research circles (such as a recent American College of Neuropsychopharmacology conference), one hears discussion of treatment of a mental disorder in monolithic terms, without explicit consideration of the various kinds of functional disabilities that occur (e.g., see the discussion of cognitive issues in depression in Levin, Heller, Mohanty, Herrington, & Miller, 2007), for which different kinds of adjunctive psychological interventions (e.g., social skills training, job training, cognitive rehabilitation) might well be indicated, even if the treatment plan leads with medication. Given a premise that mental illnesses are “brain disorders” and the inference that only medication is appropriate (which the present article argues are two separate errors), promising behavioral intervention approaches might not be pursued. Yet in schizophrenia, for example, effect sizes tend to be larger for behavioral interventions aimed at expressed emotion (Hooley, 2007) than for new medications.
There are at least two distinct aspects to the promise of expressed emotion or cognitive rehabilitation treatments as adjuncts to medication. First, medication may help normalize an important circuit, but psychological training may still be necessary to restore real-world function (as physical therapy may be needed to restore muscle strength after surgery). Thus, psychological intervention may be needed to reveal and achieve the full value of the medication. A second and more subtle reason to target psychological aspects of treatment, even if one assumes a primary role for medication, is that one may have to address many aspects of a patient’s skills and environment in order to determine the nature and size of a medication effect. Psychological interventions addressing expressed emotion, social support, and cognitive rehabilitation could reduce variance that would otherwise adversely affect (and lead us to underestimate the potential of) the medication outcome.
Aside from such implications for treatment research, the miscasting of the psychology–biology relationship endangers basic behavioral and biobehavioral research, which is valuable on its own and for potential contributions to clinical efforts. As an example, Teitelbaum and Pellis (1992) noted a very problematic intellectual and policy trend evident early in the first Decade of the Brain:
…the study sections of government funding agencies … demand that physiological psychologists use increasingly more molecular technologies to produce information about more and more molecular aspects of nervous tissue. This does not build psychology…. This also forces physiological psychologists to borrow molecular (and, often, irrelevant) technologies that they have not developed, while at the same time, they are not creating new methods for the description, analysis, and resynthesis of behavior (i.e., pure function). This is a prescription for a secondhand science. (p. 6)
This errant direction follows from the confusions reviewed above, such as believing that the biological is more fundamental than the psychological, or that psychopathology is genetic.
“The neuroscience basis for predictions about the data and the selection/interpretation of findings is not strong. It seems more at a psychological level of thinking.” That is the entire text of the primary weakness an NIH reviewer cited in a colleague’s recent NIMH grant application to study schizophrenia. Why is a psychological level of thinking a weakness? The reviewer did not offer a case that the research questions or clinical phenomena would be better served by a project more narrowly focused on neuroscience phenomena. It simply appears to be a premise, for this reviewer, that a psychological level of thinking is a bad thing. That such biases are not rare is surely one of the resocialization consequences of the Decades of the Brain.
In fact, that resocialization effort is ongoing and increasingly institutionalized. “When assessing the overall scientific merit of an application, reviewers should remember that their ultimate task is to judge the likelihood the proposed research will have a substantial impact on advancing our understanding of biological systems” —this in an email (Scarpa, personal communication, October 10, 2006), forwarded to countless grant reviewers, from the Director of the NIH Center for Scientific Review to all Scientific Research Administrators who run NIH grant-review committees and handle most regular grant applications seeking funding from NIMH (note that the “M” stands for “Mental”, not “Biological”) and NIDA. Alas, some of those reviewers sit on an NIH review committee titled “Neural Basis of Psychopathology, Addictions and Sleep Disorders Study Section” (cms.csr.nih.gov/peerreviewmeetings/csrirgdescriptionnew/bdcnirg/npas.htm).
The cover of the 2008 Training report of the National Advisory Mental Health Council (a top-level NIMH entity) Workgroup on Research (www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/reports/investing-in-the-future.pdf) is all white coats, a pipette, a microscope, and structural MRI pictures around diverse, young, professional faces. There are no images suggesting that people are the entities that have mental illness, nothing of the lives they live, nothing suggesting that NIMH staff interact with them, no hint of face-to-face assessment or psychotherapy or of the social context or social cost of mental illness. Not wanting to judge a report by its cover, looking inside one finds that the root or stem “psycholog” occurs exactly once in the 49-page document, outside of a few individuals’ titles, a single organization’s name, and a single table column heading. (By comparison, “psychiatr” occurs 14 times outside of proper names, Web addresses, etc. Still quite rare.) It would seem to be a document created by the National Institute of Chemical Health.
How far is this Decades of the Brain resocialization going? What used to be called cognitive testing in NIH grant applications is now often called neurocognitive testing (though the tests are the same). Sometimes even “bio” is no longer good enough: What was biofeedback for decades is now called neurofeedback, and bioethics somehow is inadequate for the allegedly new field of neuroethics. And for the average citizen, “Early evidence of the dangers of hands-free phone use shows that just talking on the phone reduces activity in the part of the brain responsible for driving by 37 percent” (News & Notes from State Farm, June 2009). There are a host of problems with such a statement in a mailing to customers from a leading insurance company. The problem most relevant here is the claim that there is a single part of the brain responsible for driving. Such statements systematically miseducate the public about the nature of brain function, its relationship to psychological function and dysfunction, and the potential of research on and intervention in that relationship. This is how we educate voters, exacerbating the internal and external political pressures on NIMH and NIDA leadership noted above. The scientific and health-care policy implications are immense.
Unfortunately, the evolution of behavioral science and its contributions in many domains have not received the public recognition they deserve. One consequence is that policymakers still give short shrift in budget allocations to behavioral science research. Now that it has proven its quality and its contributions to the major issues of the day, behavioral science deserves the same respect and support given to any scientific field that has come of age. (Leshner, 2007, p. 953)
The current ideology is so entrenched it is difficult to persuade state or federal legislators to allocate public funds for the prevention of psychopathology if they are told that neglect, poverty, and abuse [rather than, say, genes] place children at risk for the development of symptoms of anxiety, anger, or depression. (Kagan, 2007, p. 367)
The second consecutive NIMH Director to state that “mental disorders are brain disorders” (Thomas Insel, as quoted by Bruce, 2009) may not see how such statements undermine psychological approaches to mental illness:
Dr. Insel … stated that the outcome data showing quality-of-life improvements [from cognitive behavior therapy in schizophrenia] were extraordinarily impressive and asked why there has not been more publicity in this area. He also questioned why the NIMH is not funding more studies examining the effects of CBT [cognitive behavior therapy] on symptom reduction and quality-of-life improvement in individuals with schizophrenia. (Bruce, 2009, p. 42)
But we do know why: Recall the directive to NIH grant reviewers to privilege “research [that] will have a substantial impact on advancing our understanding of biological systems.” (Scarpa, personal communication, October 10, 2006)
Now after what has been in effect a second Decade of the Brain, a lot of the cows are already out of the barn with respect to the assumptions and headspace of basic and clinical neuroscientists, funding priorities at NIH, taxpayer understanding of what is on the horizon, etc. Rather than bemoan the past, we need to adapt to its consequences. “…the rapid pace of scientific advances in the biological sciences (and the funding that will accompany them) augurs a radically different future for psychological science—one in which new findings in genetics, cell biology, and neuroscience will exert more effects on our future empirical and theoretical work than most of the current state of our own [psychological] science” (Cuthbert, 2007, p. 18). Fortunately, Cuthbert did not foresee neuroscience swallowing psychology because “…most theories in neuroscience can only be grounded by reference to the functional perspectives that a science of behavior can provide” (Cuthbert, 2007, p. 18). To achieve that grounding, researchers must focus on getting public comprehension, budget priorities, and health-care policy back in balance.
One small but favorable change in the professional side of psychology is the rewording of one criterion for accreditation of clinical psychology doctoral programs by the American Psychological Association. Whereas for some time programs were required to teach material on the “biological bases of behavior, the wording is now “biological aspects of behavior” (see www.apa.org/ed/accreditation/ssdoctor09.pdf). This is not merely a pullback from untenable reductionism, it is a characterization of (at least some) biological events as lying within the realm of behavior (and thus of psychology). How long it will take for this change to ripple through dozens of state laws requiring extensive classroom coverage of such material for licensure as well as through NIMH policy and practice is difficult to predict.
It is not as if biological interventions are way ahead of psychological interventions for mental illness or advancing faster. Newer antipsychotics are no more effective than first-generation medications; neither are newer antidepressants more effective than older tricyclic antidepressants (Insel, 2010; for supporting citations see Deacon & Lickel, 2009). A growing clinical research literature makes clear that, at least pooled across individuals in a sample, a combination of pharmacological and psychotherapeutic interventions is clearly superior to either alone, with prospects for much more such evidence on the way (e.g., de Quervain, Aerni, Schelling, & Roozendaal, 2009; March et al., 2007; Thase et al., 1997). Some evidence suggests that psychotherapy effect sizes are often larger than those for medication (e.g., Shedler, 2010), though effects vary with symptom severity (Fournier et al., 2010). Of the unfortunately small subset of people with significant depression or anxiety who receive formal treatment (Gonzalez et al., 2010), relatively few receive a coordinated combination of psychotherapy and medication. The mental health care delivery system is doing right by a strikingly small proportion of the people we know how to help. Failing to provide treatment of either type appears to be a serious failure of the system. Allegiance to indefensible claims such as “depression is a chemical imbalance” or “schizophrenia is a brain disease” biases providers (and those who pay them, and those who set policy for payers) toward systematic overmedication (yet undertreatment). Blanket denunciation of medication is equally unfounded (Warner, 2010). These practices are damaging to individuals and costly to society.
The judgment of the research literature that combined treatment is best does not mean that every individual warrants combined treatment. Such a judgment is entirely compatible with some individuals benefiting much more from medication and others much more from psychotherapy. The literature is not yet there to guide optimal matching of person to treatment type. Were one concerned about long-term mental health care costs, one would be highly motivated to fund research on that issue. Unfortunately, under the guise of cost reduction, health care policies often merely shift costs into the future (minimally to a subsequent fiscal year and thereby hopefully to a different payer) via underdiagnosis and overmedication, leaving important issues untreated.10
Patient benefit aside, repeated hospitalization for problems for which we have good outpatient treatments is expensive. More comprehensive assessment and intervention might be more costly in the short run but cheaper in the long run. Why is studying this not a top research priority? If depression is just a chemical imbalance, and if drugs are the only way that a chemical imbalance can be addressed (two separate faulty assumptions), it is no wonder we have a dysfunctional mental health system. Assessment, prevention, and intervention are sorely (and expensively!) truncated by assumptions that, in part, are associated with the Decades of the Brain.
Dilemmas, Prospects, and Recommendations
How is it that psychological events can drive biological events, and vice versa? Or do they do so at all? No compelling answer is on the horizon. It should be clear that “working out the mechanisms” cannot be solely a matter of working out the relevant biology. Psychological mechanisms obviously need to be part of any full story about psychological phenomena, including psychopathology, and the contact point(s) between the psychological mechanisms and the biological mechanisms need to be identified and explicated. The contention of this article is that scientific and clinical progress is held up, and policy choices are severely skewed, by our tendency to cast psychological and biological phenomena in terms that preclude or obscure causal mechanisms connecting them or other relationships between them. We do this in two distinct ways: by treating one class of phenomena as interchangeable with or entirely reducible to the other, and by treating them dualistically, as if they exist in wholly different realms with no worked-out relationship. Neither is good science.
The primary concern here is naive reductionism, in the form of the now pervasive assumption that psychological phenomena, including psychopathology, can be fully accounted for in terms of biological events. Sometimes the assumption is that the phenomena can be fully accounted for in principle, though not yet in practice, and that the means will surely be forthcoming. Other times it seems that we believe that we can already do a satisfactory reduction. These more and less cautious forms of reductionism are both untenable.
Bennett and Hacker (2003), D. Ross and Spurrett (2004b), and others have provided extensive treatments of this problem. The present focus is not on providing a decisive logical analysis of the domains of biological and psychological phenomena as a basis for determining the nature or mechanism(s) of their relationship but rather on foregrounding the problematic assumptions and language of current basic and clinical neuroscience regarding these phenomena and their relationships. As argued above, these discourse conventions have major implications for how we conceive the phenomena, how we design experiments to study them, how we intervene to treat or prevent psychopathology, and how we set priorities for allocation of scientific and clinical resources in the training of scientists and clinicians, in the funding of them, and in deciding where our institutions should invest and how we should serve those in need.
The foregoing discussion has provided a sampling of problematic assumptions, terms, and policy implications but has not provided a fully satisfying alternative way to conceive psychology–biology relationships and relevant mechanisms. It is not clear to me (a) what the best (most coherent, most generative) way is to conceive the psychology–biology relationship and (b) how far biological phenomena can fruitfully go in enriching our understanding of psychological phenomena, including psychopathology. Fortunately, examples are available that demonstrate that one can do first-rate science, and talk about it, without making the mistakes of the dominant discourse convention. “Determining whether overactivations are neural correlates of processes that are beneficial, detrimental, or inconsequential to cognitive function is the crux of many research efforts in the cognitive neuroscience of aging…” (Reuter-Lorenz & Cappell, 2008, p. 177). No logical faux pas there. A claim of correlation between cognitive function and neural activation is not very strong, but that is most commonly all our neuroimaging data say. We manipulate one and measure the other, and we find that they covary. We could get quite far examining such correlations without declaring causation. The modest but logically careful “integrative explanatory pluralism” advocated by Kendler (2005b), Lilienfeld (2007), and others seems to be our best strategy at present.
Is the term underlying always problematic? Reuter-Lorenz and Cappell (2008) provided an example of appropriate usage by staying within biological events: “Transcranial magnetic stimulation (TMS) … temporarily disrupts the underlying neural signals…” (p. 177). This is a claim about a biological intervention causing biological consequences. At no point does the paper claim that biological phenomena account for (or underlie) psychological phenomena. Ditto a review of EEG asymmetry and emotion: “The specification of the neural substrates and processes underlying specific measures of EEG asymmetry in a given paradigm can constrain and inspire” theory and experimentation (Cacioppo, 2004, p. 240). Edgar et al. (2008) spoke of “a deficit in the ability of the brain to respond to novel stimuli by synchronizing the phase of ongoing oscillatory activity may be an important mechanism underlying the reported evoked potential abnormalities in schizophrenia” (p. 821). In both cases, there is no logical problem in thinking of neural events underlying EEG, as the scalp signal is believed to be essentially a summation of more atomic neuroelectric events (e.g., Whittingstall & Logothetis, 2009). The scalp EEG signal is a biological intervening variable. Conversely, Gehring, Bryck, Jonides, Albin, and Badre (2003) provided an example of appropriate usage of “underlying” among psychological events, stating that “The present study represents an effort to identify the underlying causes of the [attentional] switching effect…” (p. 573). The authors discussed, as candidate causal mechanisms, psychological phenomena such as priming and inhibition. Thus, they studied a psychological effect, which they construed to have psychological causes. They used brain measures (ERPs) to make psychological inferences but not to explain (away) a psychological phenomenon in terms of biological phenomena. In reviewing diverse neuroimaging studies, Dolan (2002) wrote about “The psychological consequences and mechanisms underlying the emotional modulation of cognition…” (p. 1191). Here again, psychological events are appropriately construed as underlying psychological events. Poldrack (2006) stated, “The goal of cognitive psychology is to understand the underlying mental architecture that supports cognitive functions” (p. 59)—again, psychological underlies psychological. Rushworth, Behrens, Rudebeck, and Walton (2007; emphasis added) discussed:
the component processes that underlie reinforcement guided decision making, such as the representation of reinforcement expectations, the exploration, updating and representation of action values, and the appreciation that choices are guided not just by the prospect of reward but also by the costs that action entails. Evidence is emerging to suggest that the anterior cingulate and orbitofrontal cortex make distinct contributions to each of these aspects of decision making. (p. 168)
They thus suggest that there is an important relationship between psychological and biological phenomena, but they do not suggest a type of relationship that the present analysis has argued is problematic. (They do not suggest a specific relationship at all, but such modesty is all they have grounds for. If only such modesty were more common, as we rarely have grounds for more than that.)
In all of these cases, there are neither logical nor practical obstacles to laying out the entire causal chain between the pairs of phenomena discussed, as each nomological net consists entirely of either psychological or biological events. These are just a few examples of the many ways in which basic and clinical neuroscientists are moving ahead without entrapment in untenable assumptions and without fostering bad science, bad clinical practice, and bad policy.
Without resorting to naive reductionism nor to dualism, we can agree that biology associated with psychopathology includes abnormal neural network structure and function, with genes (operating in genetic and environmental contexts) contributing to altered neural connectivity (Harrison & Weinberger, 2005; Meehl, 1962) and with symptoms observed across the full spectrum of language expression, central and peripheral physiology, and overt behavior (Lang, 1968, 1978). Given such a premise, conventional diagnosis based on self-report and overt behavior is strikingly limited by largely overlooking biological data (ironically so, given how heavily “biological” psychiatry has tried to become in recent decades).
The recently released draft of portions of the Diagnostic and Statistical Manual of Mental Disorders (fifth edition; DSM-V) improves ever so slightly on that, stating that mental disorder is “A behavioral or psychological syndrome or pattern that occurs in an individual … That reflects an underlying psychobiological dysfunction.” (Stein et al., 2010, p. 3; also available at www.dsm5.org/ProposedRevisions) So, the phenomenon itself is psychological, not biological, but there is a necessary (though unspecified) role for biology to play in the story. The authors explained as follows: “The term ‘psychobiological’ emphasizes the extent to which these different types and levels of dysfunction are intertwined in reality, and we therefore recommend incorporating it into the criterion” (p. 5). Because “psychobiological” and “intertwined” are not further explicated in that paper, no specific stand is taken on the role of or relationship between psychological and biological mechanisms. By (slight) contrast, in the DSM-IV (American Psychiatric Association, 2000) mental disorder is “a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual” that is “a manifestation of a behavioral, psychological or biological dysfunction in the individual” (p. xxxii). Like the DSM-V, that wording says that mental disorder itself is psychological, but it does not require a specifically “psychobiological” dysfunction. Biology is just an option in a list of domains of dysfunction, not a necessary part of the story.
The improvement in the DSM-V draft is thus in asserting that there must be some contact between psychology and biology in conceptualizing mental dysfunction; the DSM-V is not ready to take a stand on the particulars. That caution reflects what the clinical research literature has actually achieved, and it is (correctly) far more circumspect than the naive biological reductionism in much recent literature. In its definition of mental disorder, the DSM-V clearly rejects the “depression as a chemical imbalance” / “mental illness is a brain disorder” stance. On the contrary, it respects the burgeoning evidence for psychosocial factors in mental illness, especially their importance in fostering and evaluating meaningful improvement (Ro & Clark, 2009), such as cognition and even social cognition performance in evaluating medication efficacy (e.g., Carter et al., 2009; Nuechterlein et al., 2008; Vauth, Rüsch, Wirtz, & Corrigan, 2004).
Biology and psychology often are set up as competitors for scientific legitimacy, head space, and research funding. The present contention is not in favor of a psychological explanation of cognition, emotion, or psychopathology instead of a biological explanation. There is no doubt that there are systematic chemical imbalances associated with at least some cases of depression and that systematic brain disease is associated with at least some cases of schizophrenia—these contingent identities may provide important leverage points for psychological and biological theory, assessment, prevention, and intervention. But we should not frame biology and psychology in a way that forces a choice between those kinds of explanations or attempts to juxtapose or blur them without spelling out a coherent relationship between them. The still-ascendant hyperbiological bias represented by the declaration of the Decade of the Brain is no wiser and no more fruitful than the hyperpsychological bias of the psychoanalytic, behaviorist, and cognitive movements that preceded it.
We can avoid turf battles by approaching the relationship between the psychological and the biological as first fundamentally theoretical and logical, not merely a matter of data (Bennett & Hacker, 2003; Jessor, 1958). Working out the biology will not make psychology obsolete, any more than impressive advances in behaviorism or cognitive science or informatics have rendered biology obsolete. We do not have to choose. But if we pursue only biological explanation, psychological phenomena will remain unexplained, and psychological dysfunction will remain poorly treated.
A fundamental tenet of modern Western science is that dualism is not an option, where dualism assumes more than one distinct reality, such as mental and physical realities. Some scholars hope to avoid dualism by merely blurring psychology and biology together or asserting that the latter is all there is to the former. But Bennett and Hacker (2003) stated as follows:
We have tried to demonstrate, by reference to a variety of theories of distinguished contemporary cognitive neuroscientists, that conceptual error, far from being eradicated by a superficial rejection of various forms of Cartesian dualism, is widespread. It affects and infects the cogency of the questions addressed, the character of the experiments devised to answer them, the intelligibility of the descriptions of the results of these experiments, and the coherence of the conclusions derived from them. (p. 409)
Neither does functionalism entail dualism (D. Ross & Spurrett, 2004b). To avoid dualism, we must avoid taking seriously any of a host of metaphors and euphemisms, many reviewed in this article, in which psychology and biology “interact” (having two distinct domains in a position to interact implies separate realities, hence dualism), “underlie,” are “linked” or “tied to” each other, etc. We need to flesh out and make explicit our notions of the relationship between psychology and biology. Perhaps the psychological and the biological are logically distinct domains of explanation without the respective phenomena actually being physically distinct. Or perhaps psychological and biological concepts are not merely different terms for the same phenomena (with interreducible meanings)—psychological and biological explanations are not explanations of the same things. This possibility can be entertained without embracing dualism. No one accuses computer scientists of dualism due to distinguishing software and hardware or algorithm and implementation.11 Meanwhile, until we do have consensus on such a choice, individual scholars should be explicit about the choice their work makes.
Fundamentally psychological concepts will require fundamentally (though perhaps not exclusively) psychological explanations. Stories about biological phenomena can richly inform, but not replace, those explanations. When psychological events unfold in humans, they are implemented in biology, and those implementations are clearly important to study as well, both in their own right and to foster psychological research and clinical intervention. But conceptualizations limited to biology will not suffice for the psychological phenomena central to psychopathology. The present discussion is not yet one more call for more and better theory. It is a request that we stop speaking and thinking as if we already have adequate theories about psychology–biology relationships and to use and develop more careful construals of those relationships. Relatively neutral terminology such as implement and modest but generative concepts such as integrative explanatory pluralism, discussed earlier in this article, seem to be the best we have to offer as a way to move forward at present.
Cognitive, affective, and clinical neuroscience may eventually find peace on this issue. The question of the relationship between psychological and biological phenomena might be resolved the way physics has (so far) resolved the relationship of particles and waves.12 Neither underlies the other. Neither explains (or explains away or reduces) the other. Neither is more fundamental, the substrate, the foundation, or the basis. Although finding neither fully satisfying, physicists decided that each concept has value (organizing and predicting some of the data, not all), that they can coexist in the same field without forcing different camps, and that pursuit of one more than the other is not the better science, even though it is fine to devote a particular line of research (or a career) to one or the other. Why do neuroscientists, especially clinical neuroscientists studying psychopathology, feel the need to choose?
Will we ever identify and flesh out a causal chain that continues uninterrupted from psychology to biology or from biology to psychology? The answer may depend on how we construe the events we seek to account for (Bennett & Hacker, 2003). The foregoing critique faults common shortcuts that simply declare psychological events to be biological or assume a naive reductionism, whether to neurons or to genes. It is okay (and probably quite valuable) for a subset of the field to put aside the psychological phenomena that define schizophrenia, depression, and other mental disorders and to attend only to the associated biology. It is not okay to claim that doing so is an adequate path toward explaining or treating the psychological phenomena. The serious intellectual, clinical, and policy costs of such a claim were discussed earlier in the article. It was also noted that psychological phenomena do not have a spatial location in the brain and that explanations of brain phenomena are not explanations of psychological phenomena. But we can make important inferences about psychological constructs by studying the brain (see Poldrack, 2006, 2008, for discussion of inference based on neuroimaging methods, and Kozak & Miller, 1982, for a more general treatment of such psychophysiological inference).
What we can infer depends on the quality and scope of the available theories that explicitly and mechanistically relate psychological and biological phenomena. A major goal of such research is understanding, preventing, and treating mental illness. Altering someone’s neurochemistry (whether by pharmacological or psychological intervention) is not the proper goal. It is surely sometimes a critical means of reaching the goal, which, for mental disorders, is altering psychology. As noted above, we have both psychological and pharmacological interventions that are effective, on average, for people with clinical depression, particularly when used in combination. But we are largely unable to predict which type of psychotherapy, which medication, or which combination will work best for a given individual. Not only do we need better treatments, we need better prevention methods and better treatment-matching methods, with the resources deployed to deliver them. Defining away or denigrating the core psychological aspects of mental illness will not address those needs.
Until the present tide turns toward a broader vision of mental illness, we must be vigilant against indefensible but popular and pervasive claims that mental illness is simply a brain disorder, a chemical imbalance, or a genetic problem. Naive reductionism unfortunately abounds in the neuroimaging literature and in the popular press. But a mental disorder need not be triggered by, due to, or explained by brain pathology any more than a software bug must be a consequence of hardware failure. Even if the specific etiology (Meehl, 1973) of a psychological disorder were to include brain mechanisms (or gene expression affecting brain mechanisms) in the causal chain, it is possible that the brain mechanism (or gene expression) is itself driven by psychological events (Lilienfeld, 2007; Moffitt et al., 2006). Essential to promoting the contributions of biological measures to assessment, prevention, and treatment of mental illness is remembering that psychological symptoms are the prize. No advance in biological conjecture or measurement and no redefinition of terminology will alter that.
After, in effect, two Decades of the Brain and finding ourselves on the brink of a third (Miller, 2009), we now routinely speak as if neural events are causal for psychological phenomena. Such causal language is at least premature and frequently misleading. Three contentions have been explored here: the dominant discourse in modern cognitive, affective, and clinical neuroscience assumes that we know how psychology–biology causation works when we do not; there are serious intellectual, clinical, and policy costs to pretending we do (even if the pressures to do so are understandable); and crucial scientific and clinical progress will be stymied as long as we frame psychology, biology, and their relationship in currently dominant ways. The Decade of the Brain necessarily had limits, because science constantly strives for parsimony, simplifying the picture to abstract what it can. We throw away data every time we compute a mean or a trend. We do so to make problems and theories and data more tractable, and we see how far we can get. When we find the limit, we are supposed to revise and try again—sometimes incrementally, sometimes with a more dramatic shift (Kuhn, 1962). The present critique does not fault the now-aging notion of the Decade of the Brain for what it was, but some limits have become clear. Let us revise and move on.
Acknowledgments
This work was supported by the National Institute of Mental Health (P50 MH079485, R01 MH61358, T32 MH19554), the Department of Psychology of the University of Illinois at Urbana-Champaign, and the Zukunftskolleg of the University of Konstanz. The author thanks Ron A. Amundson, Howard Berenbaum, Bruce N. Cuthbert, Patricia J. Deldin, Thomas Elbert, Kara D. Federmeier, Richard Jessor, Michael J. Kozak, Jenika B. McDavitt, Russell A. Poldrack, Brigitte Rockstroh, Rebecca Levin Silton, and Edelyn Verona for comments on earlier drafts and Irving I. Gottesman and Wendy Heller for consultation.
Footnotes
The following are terminological clarifications. First, this article refers to overt events, observable by generic external observers, as scientific data. The terms empirical and empirical data are avoided out of deference to a prominent historical meaning of empirical that is quite distinct from anything publicly observable. The British empiricists, such as Locke, Berkeley, and Hume, generally believed that empirical data are those one obtains privately, through one’s senses. They are inherently private data, not public, and thus lack the status of data in Western science, which must be public in order to be (legitimate scientific) data. Relative to that tradition, the currently common term empirical data, referring to scientific data, is typically used in error. Second, psychology is commonly used to refer to overt (public) behavior, inner/mental (nonpublic) events, or both. Kozak and Miller (1982) argued that these uses of the term place psychology in two very different positions with respect to scientific data, with consequences for the role of psychological phenomena in scientific theorizing. Briefly, overt behavior is public and thus fits the conventional sense of “data” in Western science. Inner/mental events, not being public, may serve as data in one’s private life (such as for the British Empiricists), but they may not serve as conventional scientific data, because they are not publicly observable. Mental events, treated as latent or hypothetical constructs (MacCorquodale & Meehl, 1948; discussed later in the article), can be inferred from public events, which include language expression, physiology, or overt behavior (Lang, 1968, 1978). It is possible for a scientific psychology to include mental events, but it is not possible to treat them as scientific (public) data. Third, psychophysiology subsumes virtually all of human cognitive, affective, and clinical neuroscience (as well as portions of behavioral medicine). Occasionally in the hemodynamic neuroimaging literature, there is an assumption of a distinction between methods such as fMRI and psychophysiology, such as “Opportunity for a dynamic and integrative research experience combining fMRI, psychophysiology, and behavioral approaches” in a recent Web-posted job ad. That is like shopping for apples and fruit. Any neuroimaging work that includes psychological independent variables falls squarely within the definition of psychophysiology. A still widely recognition definition was published in the first issue of the senior journal in the field, Psychophysiology: “any research in which the dependent variable is a physiological measure and the independent variable a ‘behavioral’ one should be considered psychophysiological research” (Stern, 1964, p. 90; also see Davidson, 1998; Miller, 2000, 2009; and Miller et al., 2007a). Fourth, in shorthand, this article speaks as if cognition and emotion are fully distinct, but it can be argued that they should not be conceptualized as such, on both psychological and biological grounds (Miller, 1996; Pessoa, 2008). Finally, too often in the psychological literature, the “model” offered is just a list of elements that a model might include. A proper model (C. Wright & Bechtel, in press) is not just a list of psychological and/or neural elements but a specification of relations between them. This article emphasizes the lack of adequate specification of those relations.
“NIMH appears to endorse the incongruous position that (a) mental disorders are the product of a disordered brain, and (b) there is no diagnostically useful laboratory test capable of demonstrating a brain abnormality [in mental illness], nor will such a test likely ever exist” (Deacon & Lickel, 2009, p. 113).
The behavior-therapy-driven/cognitive-training-driven neural plasticity demonstrated by Candia et al. (2003) and McNab et al. (2009) discussed earlier suggests that even the software-hardware analogy is somewhat limited for present purposes, because generally we do not think of software modifying hardware, as can happen in neural plasticity.
Full disclosure: I direct a multimodal imaging center, am an active user of EEG, MEG, fMRI, and structural magnetic resonance imaging, and am a believer in the promise of these methods.
For further discussion of problems with the concept of localization of psychological function, see Willingham and Dunn (2003). Beck (2010, this issue), Racine, Bar-Ilan, and Illes (2005), McCabe and Castel (2008), and Van Horn and Poldrack (2009) presented a more extensive critique of the misrepresentation of neuroimaging results in popular media.
More disclosure: My lab has benefited from research funding from NIMH, NIDA, and NARSAD.
As this article was being completed, NARSAD announced a fund-raising initiative, the “Campaign for the Decade of Brain and Behavior Research” (www.narsad.org/?q=node/341/press-release-details/11214). This high-profile broadening of the agenda to include behavior is to be applauded. It takes nothing away from the already compelling case for the contribution of biological factors to mental illness, while nevertheless making room for the longer established contribution of psychological factors to mental illness.
Scott and Steinberg (2009) cited research on the psychological and neural immaturity of adolescents as a basis for arguing against allowing sentences of life without parole. The present perspective would be that neural immaturity, by itself, should be irrelevant to legal policy, as the latter deals with purely psychological phenomena (overt behavior, state of mind, intent, etc.). However, neural immaturity could be relevant in judging psychological immaturity, to the extent one has articulated a view about the relationship between psychological and biological phenomena that provides a basis for making inferences about psychology on the basis of brain data.
One can only speculate how fruitful psychological research would prove to be were decades of the financial and head-space resources devoted to biological research, including privately and publicly funded drug development, available to psychology.
In the acute psychiatric inpatient unit where I teach a diagnostic practicum, I often see a patient discharged after a very brief intervention directed at the acute behavior that got him/her hospitalized, without full attention to the larger set of stressors or disorders that set the stage for that acute behavior (and, often, will do so again). When the practicum began in 1990, staff outside our practicum almost never asked about or heard about any history of physical, emotional, or sexual trauma. We did so routinely, and patients frequently told my students that they were first to whom they had ever disclosed their trauma history. Many patients qualified for, but had never received, a diagnosis of posttraumatic stress disorder (PTSD). (In line with our experience, a PTSD false negative rate of 98% was documented in other psychiatric facilities by Mueser et al., 1998.) We found that this additional diagnosis was warranted in many cases of major depressive disorder and borderline personality disorder. But people typically get hospitalized for acute risk behavior, such as suicidal ideation or attempts. They are often medicated heavily and discharged quickly (well before genuine antidepressant medication effects are likely), without treatment for the PTSD or for the complex personality and behavioral adaptations to trauma that can underlie the symptoms. Perhaps they continue their antidepressant medication, perhaps not. But a number return soon enough because of acute behavior likely related to untreated (and undiagnosed) issues. This inpatient unit does a fine job given its scope and resources. I assure my students that the villain is not the unit, which is not conceived, staffed, or funded to be a comprehensive mental health treatment system. No other entity is either, so the job does not get done. Patients return, and costs accrue. The patients continue to suffer, even though we know how to treat them.
A comparison to a pair of concepts from the signal-processing literature is helpful (Edgar, Stewart, & Miller, 2005). Oscillatory phenomena that unfold over time (such as EEG data) or space (such as MRI data) are sometimes usefully displayed or analyzed as data along a temporal or spatial axis and other times in terms of sinusoidal frequencies that do not have a temporal or spatial axis in the same sense. Crucially, these are understood to be alternative representations of the same phenomenon. A bit of arithmetic can derive one from the other, so each has the status of an intervening variable with respect to the other. It would not make sense to ask whether a time-domain construal of a phenomenon underlies or is more fundamental than a frequency-domain construal of it. Some portions of the two domains are closely related, but other portions are distinct and not intertranslatable or reducible. For example, one can ask about the magnitude of a signal at a single point in time, but one cannot ask about its frequency at a single point in time. We can distinguish time and frequency domains without embracing dualism (and I reject dualism categorically), and we can do the same for psychology and biology.
Thanks to physicist Susan Lemieux for this example (personal communication, April 2, 2009).
Declaration of Conflicting Interests
The author declared that he had no conflicts of interest with respect to his authorship or the publication of this article.
References
- Abdolmaleky HM, Thiagalingam S, Wilcox M. Genetics and epigenetics in major psychiatric disorders: Dilemmas, achievements, applications, and future scope. American Journal of Pharmacogenomics. 2005;5:149–160. doi: 10.2165/00129785-200505030-00002. [DOI] [PubMed] [Google Scholar]
- Adachi S, Kawamura K, Takemoto K. Oxidative damage of nuclear DNA in liver of rats exposed to psychological stress. Cancer Research. 1993;58:4153–4155. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- American Psychological Association. APA launches decade of behavior. Monitor on Psychology. 1998 February;29(2) Retrieved February 14, 2008, from www.apa.org/monitor/feb98/behave.html.
- Amundson RA. EvoDevo as cognitive psychology. Biological Theory. 2006;1:10–11. [Google Scholar]
- Andreasen NC. The broken brain: The biological revolution in psychiatry. New York: Harper & Row; 1984. [Google Scholar]
- Aron A, Badre D, Brett M, Cacioppo J, Chambers C, Cooles R, et al. Politics and the brain. New York Times. 2007 November 14; Retrieved from http://www.nytimes.com/2007/11/14/opinion/lweb14brain.html.
- Aue T, Lavelle LA, Cacioppo JT. Great expectations: What can fMRI research tell us about psychological phenomena? International Journal of Psychophysiology. 2009;73:10–16. doi: 10.1016/j.ijpsycho.2008.12.017. [DOI] [PubMed] [Google Scholar]
- Baxter LR, Schwartz JM, Bergman KS, Szuba MP, Guze BH, Mazziotta JC, et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Archives of General Psychiatry. 1992;49:681–689. doi: 10.1001/archpsyc.1992.01820090009002. [DOI] [PubMed] [Google Scholar]
- Beck DM. The appeal of the brain in the popular press. Perspectives in Psychological Science. 2010;5:xxx–xxx. doi: 10.1177/1745691610388779. [DOI] [PubMed] [Google Scholar]
- Bennett MR, Hacker PMS. Philosophical foundations of neuroscience. Malden, MA: Blackwell; 2003. [Google Scholar]
- Berenbaum H. Toward a definition of schizophrenia. In: Miller GA, editor. The behavioral high-risk paradigm in psychopathology. New York: Springer-Verlag; 1995. pp. 181–196. [Google Scholar]
- Borkovec TD, Ray WJ, Stober J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Behaviour Research and Therapy. 1998;22:561–576. [Google Scholar]
- Braitenberg V. Vehicles. Cambridge, MA: MIT Press; 1984. [Google Scholar]
- Bramon E, Rabe-Hesketh S, Sham P, Murray RM, Fangou S. Meta-analysis of the P300 and P50 waveforms in schizophrenia. Schizophrenia Research. 2004;70:315–329. doi: 10.1016/j.schres.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Brooks D. New York Times. 2007. Apr 15, The age of Darwin; p. A14. [Google Scholar]
- Bruce SE. The NIMH professional coalition for research progress 2008 report. Behavior Therapist. 2009;32:41–42. [Google Scholar]
- Cacioppo JT. Feelings and emotions: Roles for electrophysiological markers. Biological Psychology. 2004;67:235–243. doi: 10.1016/j.biopsycho.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG, Nusbaum HC. Neuroimaging as a new tool in the toolbox of psychological science. Current Directions in Psychological Science. 2008;17:62–67. [Google Scholar]
- Candia V, Wienbruch C, Elbert T, Rockstroh B, Ray WJ. Effective behavioral treatment of focal hand dystonia in musicians alters somatosensory cortical organization. Proceedings of the National Academy of Sciences, USA. 2003;100:7942–7946. doi: 10.1073/pnas.1231193100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. American Journal of Psychiatry. 2005;162:1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter CS, Barch DM, Gur R, Gur R, Pinkham A, Ochsner K. CNTRICS final task selection: Social cognitive and affective neuroscience-based measures. Schizophrenia Bulletin. 2009;35:153–162. doi: 10.1093/schbul/sbn157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champagne FA, Mashoodh R. Genes in context: Gene–environment interplay and the origins of individual differences in behavior. Current Directions in Psychological Science. 2009;18:127–131. [Google Scholar]
- Churchland PS. Neurophilosophy: Toward a unified science of the mind-brain. Cambridge, MA: MIT Press; 1986. [Google Scholar]
- Churchland PM, Churchland PS. Functionalism, qualia, and intentionality. In: Biro JI, Shahan RW, editors. Mind, brain, and function: Essays in the philosophy of mind. Norman: University of Oklahoma Press; 1982. pp. 121–145. [Google Scholar]
- Cohen NJ, Eichenbaum H. Memory, amnesia, and the hippocampal system. Cambridge, MA: MIT Press; 1993. [Google Scholar]
- Cohen S, Janicki-Deverts D. Can we improve our physical health by altering our social networks? Perspectives on Psychological Science. 2009;4:375–378. doi: 10.1111/j.1745-6924.2009.01141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cone JD. Confounded comparisons in triple response mode assessment research. Behavioral Assessment. 1979;1:85–95. [Google Scholar]
- Cowan WM, Kopnisky KL, Hyman SE. The human genome project and its impact on psychiatry. Annual Review of Neuroscience. 2002;25:1–50. doi: 10.1146/annurev.neuro.25.112701.142853. [DOI] [PubMed] [Google Scholar]
- Cuthbert BN. Discontent in investigation: Plus ça change, plus c’est la même chose? Applied and Preventive Psychology. 2007;12:15–18. [Google Scholar]
- Dalgleish T. The emotional brain. Nature Reviews Neuroscience. 2004;5:582–589. doi: 10.1038/nrn1432. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Affect, cognition and hemispheric specialization. In: Izard CE, Kagan J, Zajonc R, editors. Emotion, cognition and behavior. New York: Cambridge University Press; 1984. pp. 320–365. [Google Scholar]
- Davidson RJ. Review of Psychophysiology: The mind–body perspective. Psychophysiology. 1998;35:352–355. [Google Scholar]
- Davis M. Neural systems involved in fear-potentiated startle. In: Davis M, Jacobs BL, Schoenfeld RI, editors. Annals of the New York Academy of Sciences: Vol. 563. Modulation of defined neural vertebrate circuits. New York: New York Academy of Sciences; 1989. pp. 165–183. [Google Scholar]
- Davis OSP, Haworth CMA, Plomin R. Dramatic increase in heritability of cognitive development from early to middle childhood. Psychological Science. 2009;20:1301–1308. doi: 10.1111/j.1467-9280.2009.02433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deacon BJ, Baird G. The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Clinical and Social Psychology. 2009;28:415–435. [Google Scholar]
- Deacon BJ, Lickel JJ. On the brain disease model of mental disorders. Behavior Therapist. 2009;32:113–118. [Google Scholar]
- Dean C. Science of the soul? “I think, therefore I am” is losing force. New York Times. 2007 June 26;:D8. [Google Scholar]
- Deldin PJ, Keller J, Gergen JA, Miller GA. Right-posterior face-processing anomaly in depression. Journal of Abnormal Psychology. 2000;109:116–121. doi: 10.1037//0021-843x.109.1.116. [DOI] [PubMed] [Google Scholar]
- Dennett DC. Making sense of ourselves. In: Biro JI, Shahan RW, editors. Mind, brain, and function: Essays in the philosophy of mind. Norman: University of Oklahoma Press; 1982. pp. 63–81. [Google Scholar]
- de Quervain DJF, Aerni A, Schelling G, Roozendaal B. Glucocorticoids and the regulation of memory in health and disease. Frontiers in Neuroendocrinology. 2009;30:358–370. doi: 10.1016/j.yfrne.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Dimitroglou E, Zafiropoulou M, Messini-Nikolaki N, Doudounakis S, Tsilimigaki S, Piperakis SM. DNA damage in a human population affected by chronic psychogenic stress. International Journal of Hygiene and Environtal Health. 2003;206:39–44. doi: 10.1078/1438-4639-00187. [DOI] [PubMed] [Google Scholar]
- Dobbs D. The gregarious brain. New York Times Magazine. 2007 July 8; Retrieved from http://www.nytimes.com/2007/07/08/magazine/08sociability-t.html.
- Dodge K. Mechanisms of gene-environment interaction effects in the development of conduct disorder. Perspectives on Psychological Science. 2009;4:408–414. doi: 10.1111/j.1745-6924.2009.01147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan RJ. Emotion, cognition, and behavior. Science. 2002;298:1191–1194. doi: 10.1126/science.1076358. [DOI] [PubMed] [Google Scholar]
- Donchin E, Coles MGH. Is the P300 component a manifestation of cognitive updating? Behavioral and Brain Sciences. 1988;11:357–427. [Google Scholar]
- Edgar JC, Hanlon FM, Huang MX, Weisend MP, Thoma RJ, Carpenter B, et al. Superior temporal gyrus spectral abnormalities in schizophrenia. Psychophysiology. 2008;45:812–824. doi: 10.1111/j.1469-8986.2008.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar JC, Stewart JL, Miller GA. Digital filtering in EEG/ERP research. In: Handy TC, editor. Event-related potentials: A handbook. Cambridge, MA: MIT Press; 2005. pp. 85–113. [Google Scholar]
- Engels AS, Heller W, Mohanty A, Herrington JD, Banich MT, Webb AG, Miller GA. Specificity of regional brain activity in anxiety types during emotion processing. Psychophysiology. 2007;44:352–363. doi: 10.1111/j.1469-8986.2007.00518.x. [DOI] [PubMed] [Google Scholar]
- Engels AS, Heller W, Spielberg JM, Warren SL, Sutton BP, Banich MT, Miller GA. Co-occurring anxiety influences patterns of brain asymmetry in depression. Cognitive, Affective, and Behavioral Neuroscience. 2010;10:141–156. doi: 10.3758/CABN.10.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felmingham K, Kemp A, Williams L, Das P, Hughes G, Peduto A, Bryant R. Changes in anterior cingulate and amygdala after cognitive behavior therapy of posttraumatic stress disorder. Psychological Science. 2007;18:127–129. doi: 10.1111/j.1467-9280.2007.01860.x. [DOI] [PubMed] [Google Scholar]
- Fodor JA. Psychological explanation. New York: Random House; 1968. [Google Scholar]
- Ford JM. The broken P300 and beyond. Psychophysiology. 1999;36:667–682. [PubMed] [Google Scholar]
- Fountain H. New York Times. 2005. Study of social interactions starts with trust; p. A20. [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J. Antidepressant drug effects and depression severity: A patient-level meta-analysis. Journal of the American Medical Association. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- France CM, Lysaker PH, Robinson RP. The “chemical imbalance” explanation for depression: Origins, lay endorsement, and clinical implications. Professional Psychology: Research and Practice. 2007;38:411–420. [Google Scholar]
- Gehring WJ, Bryck RL, Jonides J, Albin RL, Badre D. The mind’s eye, looking inward? In search of executive control in internal attention shifting. Psychophysiology. 2003;40:572–585. doi: 10.1111/1469-8986.00059. [DOI] [PubMed] [Google Scholar]
- Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S, et al. Modulation of cortical-limbic pathways in major depression: Treatment-specific effects of cognitive behavior therapy. Archives of General Psychiatry. 2004;61:34–41. doi: 10.1001/archpsyc.61.1.34. [DOI] [PubMed] [Google Scholar]
- Gonzalez HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: Too little for too few. Archives of General Psychiatry. 2010;67:37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould TD, Gottesman II. Psychiatric endophenotypes and the development of valid animal models. Genes, Brain and Behavior. 2006;5:113–119. doi: 10.1111/j.1601-183X.2005.00186.x. [DOI] [PubMed] [Google Scholar]
- Hanlon FM, Euler MJ, Bantz RL, Lundy SL, Thoma RJ, Weisend MP, et al. Assessment of lateralized hippocampal function in schizophrenia; Paper presented at the 20th International Congress on Schizophrenia Research; Colorado Springs, CO. 2007. Mar, [Google Scholar]
- Hanlon FM, Miller GA, Thoma RJ, Irwin J, Jones A, Moses SN, et al. Distinct M50 and M100 auditory gating deficits in schizophrenia. Psychophysiology. 2005;42:417–427. doi: 10.1111/j.1469-8986.2005.00299.x. [DOI] [PubMed] [Google Scholar]
- Hanlon FM, Weisend MP, Huang M, Lee RR, Moses SN, Paulson KM, et al. A noninvasive method for observing hippocampal function. NeuroReport. 2003;14:1957–1960. doi: 10.1097/00001756-200310270-00015. [DOI] [PubMed] [Google Scholar]
- Haque FN, Gottesman II, Wong AHC. American Journal of Medical Genetics: Part C. Seminars in Medical Genetics. 2009;151C:136–141. doi: 10.1002/ajmg.c.30206. [DOI] [PubMed] [Google Scholar]
- Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: On the matter of their convergence. Molecular Psychiatry. 2005;10:40–68. doi: 10.1038/sj.mp.4001558. [DOI] [PubMed] [Google Scholar]
- Heinrichs RW. The primacy of cognition in schizophrenia. American Psychologist. 2005;60:229–242. doi: 10.1037/0003-066X.60.3.229. [DOI] [PubMed] [Google Scholar]
- Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12:426–445. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- Hempel CG. Philosophy of natural science. Englewood Cliffs, NJ: Prentice-Hall; 1966. [Google Scholar]
- Herrington JD, Heller W, Mohanty A, Engels A, Banich MT, Webb AW, Miller GA. Localization of asymmetric brain function in emotion and depression. Psychophysiology. 2010;47:442–454. doi: 10.1111/j.1469-8986.2009.00958.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington JD, Mohanty A, Koven NS, Fisher JE, Stewart JL, Banich MT, et al. Emotion-modulated performance and activity in left dorsolateral prefrontal cortex. Emotion. 2005;5:200–207. doi: 10.1037/1528-3542.5.2.200. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: Version III-The final common pathway. Schizophrenia Bulletin. 2009;35:549–562. doi: 10.1093/schbul/sbp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SE. NIMH during the tenure of Director Steven E. Hyman, MD: The now and future of NIMH. American Journal of Psychiatry. 1998;155(Suppl):36–40. [PubMed] [Google Scholar]
- Hyman SE. Addiction: A disease of learning and memory. American Journal of Psychiatry. 2005;162:1414–1422. doi: 10.1176/appi.ajp.162.8.1414. [DOI] [PubMed] [Google Scholar]
- Insel TR. Faulty circuits. Scientific American. 2010 April;302(4):44–51. doi: 10.1038/scientificamerican0410-44. [DOI] [PubMed] [Google Scholar]
- Jessor R. The problem of reductionism in psychology. Psychological Review. 1958;65:170–178. [Google Scholar]
- Johnson W, Krueger RF. Higher perceived life control decreases genetic variance in physical health: Evidence from a national twin study. Journal of Personality and Social Psychology. 2005;88:165–173. doi: 10.1037/0022-3514.88.1.165. [DOI] [PubMed] [Google Scholar]
- Johnson W, Turkheimer E, Gottesman II, Bouchard TJ., Jr Beyond heritability: Twin studies in behavioral research. Current Directions in Psychological Science. 2009;18:217–220. doi: 10.1111/j.1467-8721.2009.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagan J. A trio of concerns. Perspectives on Psychological Science. 2007;2:361–376. doi: 10.1111/j.1745-6916.2007.00049.x. [DOI] [PubMed] [Google Scholar]
- Kandel ER, Squire LR. Cognitive neurosciences: Editorial overview. Current Opinion in Neurobiology. 1992;2:143–145. doi: 10.1016/s0959-4388(96)80067-5. [DOI] [PubMed] [Google Scholar]
- Keller J, Nitschke JB, Bhargava T, Deldin PJ, Gergen JA, Miller GA, Heller W. Neuropsychological differentiation of depression and anxiety. Journal of Abnormal Psychology. 2000;109:3–10. [PubMed] [Google Scholar]
- Kendler KS. “A gene for…”: The nature of gene action in psychiatric disorders. American Journal of Psychiatry. 2005a;162:1243–1252. doi: 10.1176/appi.ajp.162.7.1243. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Toward a philosophical structure for psychiatry. American Journal of Psychiatry. 2005b;162:433–440. doi: 10.1176/appi.ajp.162.3.433. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Psychiatric genetics: A current overview. Invited lecture presented at the annual meeting of the Society for Research in Psychopathology; Minneapolis, MN. 2009. Sep, [Google Scholar]
- Kety SS, Rosenthal D, Wender PH, Schulsinger F. The types and prevalence of mental illness in the biological and adoptive families of adopted schizophrenics. In: Rosenthal D, Kety SS, editors. The transmissions of schizophrenia. Oxford, United Kingdom: Pergamon; 1968. pp. 345–362. [Google Scholar]
- King-Casas B, Tomlin D, Anen C, Camerer CF, Quartz SR, Montague PR. Getting to know you: Reputation and trust in a two-person economic exchange. Science. 2005;308:78–83. doi: 10.1126/science.1108062. [DOI] [PubMed] [Google Scholar]
- Kolassa IT, Elbert T. Structural and functional neuroplasticity in relation to traumatic stress. Current Directions in Psychological Science. 2007;16:321–325. [Google Scholar]
- Kopnisky KL, Cowan WM, Hyman SE. Levels of analysis in psychiatric research. Development and Psychopathology. 2002;14:437–461. doi: 10.1017/s0954579402003036. [DOI] [PubMed] [Google Scholar]
- Korzybski A. Science and sanity: An introduction to non-Aristotelian systems and general semantics. 4. Lakeville, CT: International Non-Aristotelian Library; 1958. [Google Scholar]
- Kosslyn SM, Cacioppo JT, Davidson RJ, Hugdahl K, Lovallo WR, Spiegel D, Rose R. Bridging psychology and biology: The analysis of individuals in groups. American Psychologist. 2002;57:341–351. [PubMed] [Google Scholar]
- Kosslyn SM, Koenig O. Wet mind: The new cognitive neuroscience. New York: Free Press; 1992. [Google Scholar]
- Kotchoubey B. Neuroscience through the looking glass. Journal of Psychophysiology. 2005;19:232–237. [Google Scholar]
- Kozak MJ, Miller GA. Hypothetical constructs versus intervening variables: A reappraisal of the three-systems model of anxiety assessment. Behavioral Assessment. 1982;14:347–358. [Google Scholar]
- Kramer AF, Erickson KI. Aerobic exercise effects on cognitive and neural plasticity in older adults. British Journal of Sports Medicine. 2009;43:22–24. doi: 10.1136/bjsm.2008.052498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn TS. The structure of scientific revolutions. Chicago: University of Chicago Press; 1962. [Google Scholar]
- Lang PJ. Experimental studies of desensitization therapy. In: Wolpe J, editor. The conditioning therapies. New York: Holt, Rinehart, & Winston; 1964. pp. 38–53. [Google Scholar]
- Lang PJ. Fear and behavior: Problems in treating a construct. In: Shlien JM, editor. Research in psychotherapy. Vol. 3. Washington, DC: American Psychological Association; 1968. pp. 90–102. [Google Scholar]
- Lang PJ. Anxiety: Toward a psychophysiological definition. In: Akiskal HS, Webb WL, editors. Psychiatric diagnosis: Exploration of biological criteria. New York: Spectrum; 1978. pp. 265–389. [Google Scholar]
- LeDoux JE. Emotion: Clues from the brain. Annual Review of Psychology. 1995;46:209–235. doi: 10.1146/annurev.ps.46.020195.001233. [DOI] [PubMed] [Google Scholar]
- Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–47. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- Leshner AI. Behavioral sciences comes of age. Science. 2007;316:953. doi: 10.1126/science.1144897. [DOI] [PubMed] [Google Scholar]
- Levin RL, Heller W, Mohanty A, Herrington JD, Miller GA. Cognitive deficits in depression and functional specificity of regional brain activity. Cognitive Therapy and Research. 2007;31:211–233. [Google Scholar]
- Lilienfeld SO. Cognitive neuroscience and depression: Legitimate versus illegitimate reductionism and five challenges. Cognitive Therapy and Research. 2007;31:263–272. [Google Scholar]
- Luchins DJ. At issue: Will the term brain disease reduce stigma and promote parity for mental illnesses? Schizophrenia Bulletin. 2004;30:1043–1048. doi: 10.1093/oxfordjournals.schbul.a007119. [DOI] [PubMed] [Google Scholar]
- Lycan WG. Psychological laws. In: Biro JI, Shahan RW, editors. Mind, brain, and function: Essays in the philosophy of mind. Norman: University of Oklahoma Press; 1982. pp. 9–38. [Google Scholar]
- Lykken DT, McGue M, Tellegen A, Bouchard TJ., Jr Emergenesis: Genetic traits that may not run in families. American Psychologist. 1992;47:1565–1577. doi: 10.1037//0003-066x.47.12.1565. [DOI] [PubMed] [Google Scholar]
- MacCorquodale K, Meehl PE. On a distinction between hypothetical constructs and intervening variables. Psychological Review. 1948;55:95–107. doi: 10.1037/h0056029. [DOI] [PubMed] [Google Scholar]
- March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. The treatment for adolescents with depression study (TADS) Archives of General Psychiatry. 2007;64:1132–1144. doi: 10.1001/archpsyc.64.10.1132. [DOI] [PubMed] [Google Scholar]
- Marr D. Vision: A computational investigation into the human representation and processing of visual information. New York: Freeman; 1982. [Google Scholar]
- Marshall PJ. Relating psychology and neuroscience: Taking up the challenges. Perspectives in Psychological Science. 2009;4:113–125. doi: 10.1111/j.1745-6924.2009.01111.x. [DOI] [PubMed] [Google Scholar]
- McCabe D, Castel A. Seeing is believing: The effect of brain images on judgments of scientific reasoning. Cognition. 2008;107:343–352. doi: 10.1016/j.cognition.2007.07.017. [DOI] [PubMed] [Google Scholar]
- McGue M. The behavioral genetics of alcoholism. Current Directions in Psychological Science. 1999;8:109–115. [Google Scholar]
- McNab F, Varone A, Farde L, Jucaite A, Bystritsky P, Forssberg H, Klingberg T. Changes in cortical dopamine D1 receptor binding associated with cognitive training. Science. 2009;323:800–802. doi: 10.1126/science.1166102. [DOI] [PubMed] [Google Scholar]
- Meany MJ. Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annual Review of Neuroscience. 2001;24:1161–1192. doi: 10.1146/annurev.neuro.24.1.1161. [DOI] [PubMed] [Google Scholar]
- Meehl PE. Schizotaxia, schizotypy, schizophrenia. American Psychologist. 1962;17:827–838. [Google Scholar]
- Meehl PE. Specific genetic etiology, psychodynamics, and therapeutic nihilism. In: Meehl PE, editor. Psychodiagnosis: Selected papers. Minneapolis: University of Minnesota Press; 1973. pp. 182–199. [Google Scholar]
- Meehl PE. Theoretical risks and tabular asterisks: Sir Karl, Sir Ronald, and the slow progress of soft psychology. Journal of Consulting and Clinical Psychology. 1978;46:806–834. [Google Scholar]
- Meehl PE. Toward and integrated theory of schizotaxia, schizotypy, and schizophrenia. Journal of Personality Disorders. 1990;4:1–99. [Google Scholar]
- Meehl PE. What’s in a taxon? Journal of Abnormal Psychology. 2004;113:39–43. doi: 10.1037/0021-843X.113.1.39. [DOI] [PubMed] [Google Scholar]
- Menand L. Head case: Can psychiatry be a science? New Yorker. 2010 March 1; Retrieved April 17, 2010, at www.newyorker.com/arts/critics/atlarge/2010/03/01/100301crat_atlarge_menand.
- Miller GA. Presidential address: How we think about cognition, emotion, and biology in psychopathology. Psychophysiology. 1996;33:615–628. doi: 10.1111/j.1469-8986.1996.tb02356.x. [DOI] [PubMed] [Google Scholar]
- Miller GA. Editorial. Psychophysiology. 2000;37:1–4. [PubMed] [Google Scholar]
- Miller GA. Another quasi-thirty years of slow progress. Applied and Preventive Psychology: Current Scientific Perspectives. 2004;11:61–64. [Google Scholar]
- Miller GA. Localization for hippocampal abnormality: Hunting deep structures with MEG. Paper presented at the 4-D Neuroimaging 3rd Annual International Users Group Meeting; Barcelona, Spain. 2008. Jul, [Google Scholar]
- Miller GA. How we think about cognition, emotion, and biology in psychopathology: 14 years later. Paper presented in the Past Presidents Symposium at the annual meeting of the Society for Psychophysiological Research; Berlin, Germany. 2009. Oct, [Google Scholar]
- Miller GA, Ebert L. Conceptual boundaries in psychophysiology. Journal of Psychophysiology. 1988;2:13–16. [Google Scholar]
- Miller GA, Elbert T, Sutton BP, Heller W. Innovative clinical assessment technologies: Challenges and opportunities in neuroimaging. Psychological Assessment. 2007a;19:58–73. doi: 10.1037/1040-3590.19.1.58. [DOI] [PubMed] [Google Scholar]
- Miller GA, Engels AS, Herrington JD. The seduction of clinical science: Challenges in psychological and biological convergence. In: Treat TA, Bootzin RR, Baker TB, editors. Psychological clinical science: Papers in honor of Richard McFall. Mahwah, NJ: Erlbaum; 2007b. pp. 53–74. [Google Scholar]
- Miller GA, Keller J. Psychology and neuroscience: Making peace. Current Directions in Psychological Science. 2000;9:212–215. [Google Scholar]
- Miller GA, Kozak MJ. A philosophy for the study of emotion: Three-systems theory. In: Birbaumer N, Öhman A, editors. The structure of emotion: Physiological, cognitive and clinical aspects. Seattle, WA: Hogrefe & Huber; 1993. pp. 31–47. [Google Scholar]
- Moffitt TE, Caspi A, Rutter M. Measured gene-environment interactions in psychopathology. Perspectives on Psychological Science. 2006;1:5–27. doi: 10.1111/j.1745-6916.2006.00002.x. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Reid MW. Life stress and major depression. Current Directions in Psychological Science. 2009;18:68–72. [Google Scholar]
- Mueser KT, Goodman LB, Trubetta SL, Rosenberg SD, Osher FC, Vidaver R, Auciello P. Trauma and posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 1998;66:493–499. doi: 10.1037//0022-006x.66.3.493. [DOI] [PubMed] [Google Scholar]
- Nelson CA, Gottesman II. A piece of a neuroscientist’s mind. Science. 2005;307:1204. [Google Scholar]
- Nisbett RE, Wilson T. Telling more than we can know: Verbal reports on mental processes. Psychological Review. 1977;84:231–259. [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS consensus cognitive battery: Part 1. Test selection, reliability, and validity. American Journal of Psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Oxley DR, Smith KB, Alford JR, Hibbing MV, Miller JL, Scalora M, et al. Political attitudes vary with physiological traits. Science. 2008;321:1667–1670. doi: 10.1126/science.1157627. [DOI] [PubMed] [Google Scholar]
- Padgett DA, Glaser R. How stress influences the immune response? Trends in Immunology. 2003;24:444–448. doi: 10.1016/s1471-4906(03)00173-x. [DOI] [PubMed] [Google Scholar]
- Pearl J. Causal inference in statistics: An overview. Statistics Surveys. 2009;3:96–146. [Google Scholar]
- Pessoa L. On the relationship between emotion and cognition. Nature Reviews Neuroscience. 2008;9:148–158. doi: 10.1038/nrn2317. [DOI] [PubMed] [Google Scholar]
- Pinker S. My genome, my self. New York Times Magazine. 2009 January 11; Retrieved from http://www.nytimes.com/2009/01/11/magazine/11Genome-t.html?sq=My%20genome,%20my%20self&st=cse&adxnnl=1&scp=1&adxnnlx=1280862021-fX+xUOPAe1Pa5ji6Ha9m9Q.
- Poldrack RA. Can cognitive processes be inferred from neuroimaging data? Trends in Cognitive Sciences. 2006;10:59–63. doi: 10.1016/j.tics.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Poldrack RA. The role of fMRI in cognitive neuroscience: Where do we stand? Current Opinion in Neurobiology. 2008;18:1–5. doi: 10.1016/j.conb.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Popov T, Jordanov T, Rockstroh B, Elbert T, Merzenich MM, Miller GA. Specific cognitive training normalizes auditory sensory gating in schizophrenia: A randomized trial. Biological Psychiatry. 2011;69:465–471. doi: 10.1016/j.biopsych.2010.09.028. [DOI] [PubMed] [Google Scholar]
- Racine E, Bar-Ilan O, Illes J. fMRI in the public eye. Nature Reviews Neuroscience. 2005;6:159–164. doi: 10.1038/nrn1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redhead M. Explanation. In: Knowles D, editor. Explanation and its limits. Cambridge University Press; 1990. pp. 135–152. [Google Scholar]
- Reuter-Lorenz PA, Cappell KA. Neurocognitive aging and the compensation hypothesis. Current Directions in Psychological Science. 2008;17:177–182. [Google Scholar]
- Ro E, Clark LA. Psychosocial functioning in the context of diagnosis: Assessment and theoretical issues. Psychological Assessment. 2009;21:313–324. doi: 10.1037/a0016611. [DOI] [PubMed] [Google Scholar]
- Rose RM. Embodying the mind: A brief history of the science integrating mind and body. NeuroImage. 2009;47:785–786. doi: 10.1016/j.neuroimage.2009.02.022. [DOI] [PubMed] [Google Scholar]
- Ross CA, Pam A. Pseudoscience in biological psychiatry: Blaming the body. New York: Wiley; 1995. [Google Scholar]
- Ross D, Spurrett D. The cognitive and behavioral sciences: Real patterns, real unity, real causes, but no supervenience. Behavioral and Brain Sciences. 2004a;27:637–647. [Google Scholar]
- Ross D, Spurrett D. What to say to a sceptical metaphysician: A defense manual for cognitive and behavioral scientists. Behavioral and Brain Sciences. 2004b;27:603–627. doi: 10.1017/s0140525x04000147. [DOI] [PubMed] [Google Scholar]
- Ross D, Spurrett D. Notions of cause: Russell’s thesis revisited. British Journal for the Philosophy of Science. 2007;58:45–76. [Google Scholar]
- Ruscio J, Ruscio AM. Clarifying boundary issues in psychopathology: The role of taxometrics in a comprehensive program of structural research. Journal of Abnormal Psychology. 2004;113:24–38. doi: 10.1037/0021-843X.113.1.24. [DOI] [PubMed] [Google Scholar]
- Rushworth MFS, Behrens TEJ, Rudebeck PH, Walton ME. Contrasting roles for cingulate and orbitofrontal cortex in decisions and social behaviour. Trends in Cognitive Sciences. 2007;11:168–176. doi: 10.1016/j.tics.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM. Why stress is bad for your brain. Science. 1996;273:749–750. doi: 10.1126/science.273.5276.749. [DOI] [PubMed] [Google Scholar]
- Satel S. Mind over manual. New York Times. 2007 September 13;:A23. [Google Scholar]
- Schauer M, Elbert T, Gotthardt S, Rockstroh B, Odenwald M, Neuner F. Wiederfahrung durch psychotherapie modifiziert geist und gehirn [Re-experiencing by psychotherapy modifies mind and brain] Verhaltenstherapie. 2006;16:96–103. [Google Scholar]
- Schienle A, Schaefer A, Stark R, Vaitl D. Long-term effects of cognitive behavior therapy on brain activation in spider phobia. Psychiatry Research: Neuroimaging. 2009;172:99–102. doi: 10.1016/j.pscychresns.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Schreiner SA., Jr Truly, madly, deeply. New York Times. 2006 February 20;:A19. [Google Scholar]
- Scott ES, Steinberg L. The young and reckless. New York Times. 2009 November 14;:A21. [Google Scholar]
- Shedler J. The efficacy of psychodynamic psychotherapy. American Psychologist. 2010;65:98–109. doi: 10.1037/a0018378. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Phillips KA, Bolton D, Fulford KWM, Sadler JZ, Kendler KS. What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychological Medicine. 2010;40:1–7. doi: 10.1017/S0033291709992261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern JA. Toward a definition of psychophysiology. Psychophysiology. 1964;1:90–91. doi: 10.1111/j.1469-8986.1964.tb02626.x. [DOI] [PubMed] [Google Scholar]
- Taitano K, Miller GA. Neuroscience perspectives on emotion in psychopathology. In: Flack W, Laird J, editors. Emotion in psychopathology: Theory and research. New York: Oxford; 1998. pp. 20–44. [Google Scholar]
- Teitelbaum P, Pellis SM. Toward a synthetic psychology. Psychological Science. 1992;3:4–20. [Google Scholar]
- Thase ME, Friedman ES, Biggs MM, Wisniewski SR, Trivedi MH, Luther JF, et al. Cognitive therapy versus medication in augmentation and switch strategies as second-step treatments: A STAR*D report. American Journal of Psychiatry. 2007;164:739–752. doi: 10.1176/ajp.2007.164.5.739. [DOI] [PubMed] [Google Scholar]
- Turkheimer E. Three laws of behavior genetics and what they mean. Current Directions in Psychological Science. 2000;9:160–164. [Google Scholar]
- Turkheimer E, Gottesman II, Goldsmith HH. Commentary. Human Development. 1995;38:142–153. [Google Scholar]
- Turkheimer E, Haley A, Waldron M, D’Onofrio B, Gottesman II. Socioeconomic status modifies heritability of IQ in young children. Psychological Science. 2003;14:623–628. doi: 10.1046/j.0956-7976.2003.psci_1475.x. [DOI] [PubMed] [Google Scholar]
- Van Horn JD, Poldrack RA. Functional MRI at the crossroads. International Journal of Psychophysiology. 2009;73:3–9. doi: 10.1016/j.ijpsycho.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Praag HM. Can stress cause depression? Progress in Neuro-psychopharmacology & Biological Psychiatry. 2004;28:891–907. doi: 10.1016/j.pnpbp.2004.05.031. [DOI] [PubMed] [Google Scholar]
- Vauth R, Rüsch N, Wirtz M, Corrigan PW. Does social cognition influence the relation between neurocognitive deficits and vocational functioning in schizophrenia? Psychiatry Research. 2004;128:155–165. doi: 10.1016/j.psychres.2004.05.018. [DOI] [PubMed] [Google Scholar]
- Volkow ND. What do we know about drug addiction? American Journal of Psychiatry. 2005;162:1401–1402. doi: 10.1176/appi.ajp.162.8.1401. [DOI] [PubMed] [Google Scholar]
- Walker E. Behavioral science and biological reductionism. Psychopathology Research. 2000;11:1–3. [Google Scholar]
- Warner J. The wrong story about depression. [accessed 01/27/10.];New York Times. 2010 January 9; Retrieved from www.nytimes.com/2010/01/09/opinion/09warner.html.
- Watters E. The Americanization of mental illness. [accessed 01/11/10.];New York Times. 2010 January 10; Retrieved from www.nytimes.com/2010/01/10/magazine/10psyche-t.html.
- Weisberg DS, Keil FC, Goodstein J, Rawson E, Gray JR. The seductive allure of neuroscience explanations. Journal of Cognitive Neuroscience. 2008;20:470–477. doi: 10.1162/jocn.2008.20040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West SG, Thoemmes F. Campbell’s and Rubin’s perspectives on causal inference. Psychological Methods. 2010;15:18–37. doi: 10.1037/a0015917. [DOI] [PubMed] [Google Scholar]
- Whittingstall K, Logothetis NK. Frequency-band coupling in surface EEG reflects spiking activity in monkey visual cortex. Neuron. 2009;64:281–289. doi: 10.1016/j.neuron.2009.08.016. [DOI] [PubMed] [Google Scholar]
- Willingham DT, Dunn EW. What neuroimaging and brain localization can do, cannot do, and should not do for social psychology. Journal of Personality and Social Psychology. 2003;85:662–671. doi: 10.1037/0022-3514.85.4.662. [DOI] [PubMed] [Google Scholar]
- Wright C, Bechtel W. Mechanisms and psychological explanation. In: Thagard P, editor. Handbook of the philosophy of science: Vol. 4. Philosophy of psychology and cognitive science. New York: Elsevier; in press. [Google Scholar]
- Wright R. Alcohol and free will. New Republic. 1987 December 14;:14–16. [Google Scholar]
- Zuckerman M. Vulnerability to psychopathology: A biosocial model. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Zweig J. Your money and your brain. Money Magazine. 2007 September;:104–109. [Google Scholar]