Abstract
Introduction
The discovery that many tissues express the vitamin D receptor and are able to transform the 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D (active metabolite) has led to the hypothesis that vitamin D could have a role in the pathogenesis and prevention of diabetes mellitus. Accumulating evidence has linked vitamin D deficiency with immunological disturbance in type 1 diabetes mellitus. Several epidemiological studies have shown lower serum 25-hydroxyvitamin D concentrations in diabetic individuals compared to nondiabetic individuals.
Patients and methods
A total of 105 Lebanese patients with type 1 diabetes mellitus were recruited. Levels of HbA1c and vitamin D were recorded during two phases with phase 1 being the period from June–September 2009 and phase 2 from January–April 2009.
Results
Vitamin D levels at the end of sunny season (phase 2), reflecting the previous sunny months, were found to be higher than in the early summer season (phase 1) reflecting the previous cloudy months season, with a mean change of 0.70 ± 6.87 ng/mL (P = 0.029). HbA1c levels were higher in phase 2 than in phase 1 with an increase of 0.175% ± 1.46% (P = 0.113).
Conclusion
Vitamin D levels were higher at the end of the sunny season than at the end of cloudy season. HbA1c was also lower (but not significantly so) in the early summer season (cloudy months). There was a weak correlation between seasonal changes of vitamin D levels and the control of blood glucose as monitored by HbA1c in a cohort of Lebanese patients with type 1 diabetes mellitus.
Keywords: type 1 diabetes, vitamin D, HbA1c, seasonal variation
Introduction
Type 1 diabetes mellitus (T1DM) is a T-cell mediated autoimmune disease that results in the destruction of insulin producing beta cells in the pancreas requiring exogenous insulin for survival.1 The beta-cell destruction often begins during infancy and continues over many months or years. By the time T1DM is diagnosed, about 80% of the beta-cells have been destroyed.2 Although it is acknowledged to be an autoimmune disease, the causes are still considered to be unknown.3 Epidemiologic studies of T1DM have directed the search for possible genetic predispositions and related environmental factors that are still poorly defined.4 Some identified environmental risk factors operating early in life include enteroviral infections in pregnant women, older maternal age (39–42 years), preeclampsia, cesarean section delivery, increased birth weight, early introduction of cow’s milk proteins, and an increased rate of postnatal growth (weight and height).5,6 There is a need to find the cause of this chronic disease because there has been an increase its incidence over time. It is estimated that currently the incidence is increasing by 3% per year and this cannot be explained by genetic factors only.2 Several approaches have been tried to prevent T1DM but none of them have been shown to work, and the prevention of T1DM remains an objective for the future.7
Recent evidence has reported that vitamin D deficiency predisposes individuals to T1DM and T2DM. Several studies show that vitamin D has several effects on the immune system and insulin synthesis and secretion, therefore suggesting a role in the development of both types of diabetes. Studies have shown that diabetic individuals are more vitamin D deficient than nondiabetic individuals.8 Vitamin D deficiency is becoming a global public health problem although it is largely unrecognized.9–12 It has been estimated that 1 billion people worldwide have vitamin D deficiency or insufficiency.13
The aim of our study is to show that better glycemic control achieved in patients with T1DM during the sunny season compared to the cloudy season is related to change in the levels of serum 25-hydroxyvitamin D.4–6 Our second aim is to determine whether lower values of glycosylated hemoglobin (HbA1c) noted during the end of the cloudy season compared to the end of the sunny season is associated with higher levels of vitamin D.
Patients and methods
The study recruitment was done at the Chronic Care Center in Hazmieh, Lebanon. The center is a specialized institution for the treatment and follow-up of childhood chronic T1DM. A total of 105 Lebanese patients with T1DM were recruited. Patient characteristics are presented in Table 1. Level of 25-hydroxyvitamin D was assessed in the patients at two different phases: phase 1 from June–September 2009, reflecting the previous cloudy 6 months, and phase 2 from January–April 2009, reflecting the previous sunny 6 months. For each phase, the level of HbA1c was also recorded for each patient. Serum 25-hydroxyvitamin D levels for both phases were measured by using the radioimmunoassay immunodiagnostics system kit and HbA1c was determined by the high performance liquid chromatography method using a Variant kit (Bio-Rad Laboratories, Philadelphia, PA).
Table 1.
Participant characteristics
| Mean age (years) | 18.75 ± 6.35 |
| Mean duration of diabetes mellitus (years) | 7.9 ± 6.0 |
| Sex distribution (%) | 56.7% male, 43.3% female |
| Mean body mass index at baseline (kg/m2) | 23.2 ± 4.2 |
| Mean waist circumference (cm) | 82.2 ± 12.1 |
| Mean hip circumference (cm) | 96.8 ± 11.2 |
| Baseline fasting blood sugar (mg/dL) | 152.9 ± 91.4 |
The study protocol has been reviewed and approved by the Ethics Committee at the Chronic Care Center as well as the Institutional Review Board at the American University of Beirut. A signed informed consent was obtained from all patients.
Results
When analyzing for a trend of vitamin D and HbA1c change, vitamin D levels in phase 2 were found to be more elevated than in phase 1 with a mean change of 0.70 ± 6.87 ng/mL (P = 0.029). Similarly, HbA1c levels were higher in phase 2 than in phase 1 with an increase of 0.175% ± 1.46%. However this trend regarding blood sugar control was not significant (P = 0.113).
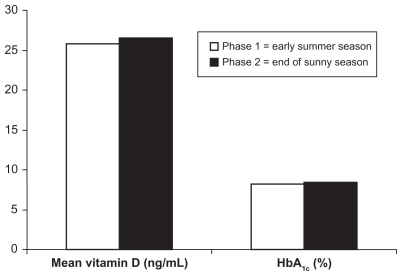
Both HbA1c and serum vitamin D levels were found to be higher during the early cloudy season (end of sunny season; phase 2) as opposed to early summer season (phase 1). When analyzing for a correlation, it was found to be very weak with the Spearman coefficient being −0.046 (P = 0.661). Thus it seems that both HbA1c and vitamin D levels tend to increase over the early cloudy season (end of sunny season) and decrease in the early summer season (Figure 1). It is important to note that this tendency did not reach significance for the HbA1c fluctuation.
Figure 1.
HbA1c and vitamin D levels in early summer season vs end of sunny season.
Discussion
The existence of vitamin D receptors in activated T lymphocytes, antigen-presenting cells (macrophages and dendritic cells), and thymus tissue raised the idea that 1,25-dihydroxyvitamin D (1,25(OH)2D) might function as an immunomodulator.14–16 The fact that immune cells (activated macrophages and dendritic cells in particular) also contain the enzyme 1-alpha-hydroxylase, which is necessary for the final activating step in the conversion of 25-hydroxyvitamin D to the metabolically active molecule, shows that these cells are able to synthesize and secrete 1,25(OH)2D which is able to target the immune system.8
In order to provide evidence that vitamin D affects the risk of developing T1DM, several studies have been done using animal models such as nonobese diabetic (NOD) mice. A study conducted by Mathieu et al reported that 1,25(OH)2D has been shown to reduce T1DM onset in NOD mice. He administrated 5 μg/kg of 1,25(OH)2D in the NOD mice and found that diabetes incidence in NOD mice at 200 days was reduced to 8% in the 1,25(OH)2D-treated group vs 56% in the control group.17 A study conducted by Zella et al reported that a vitamin D deficient state alone can potentiate diabetic onset in the NOD mouse. The authors also found that daily dietary supplementation with 2000 IU of 1,25(OH)2D prevents diabetes over 200 days regardless of vitamin D status before the study.18 They suggested that oral administration of 1,25(OH)2D or preferably a nonhypercalcemic analog would be clinically relevant for the prevention of T1DM in humans.16
In our study we aimed to show that an increase in vitamin D serum level is correlated to an improvement in glycemic control as shown in a decrease in HbA1c levels. Interestingly the vitamin D level was significantly higher at the end of the sunny season than in the summer season itself. The vitamin D levels reported by this study were taken in Lebanon at latitude 33°N and were lower than the ones reported by Greer in Australia (latitude 29°S) and by Littorin in Sweden (latitude 55–65°N).19,20 It seems that vitamin D levels in our study are affected by factors relevant to developing countries21 rather than purely on geographical/solar distribution considerations.22 In a national US study, it was found that the average American spent 93% of their 24-hour day indoors. Air conditioning, computers, video games, and extensive television programming are reasons behind the increasing time spent indoors with decrease in outdoor activities. Because of the current changes in lifestyles, humans are now more dependent on foods rich in vitamin D or oral vitamin D supplementation and less exposed to sunlight even in summer. 23 Remarkably in the sunniest areas of the world, vitamin D deficiency is also a major health problem. It was found that in Saudi Arabia, India, Turkey, New Zealand, Egypt, Hong Kong, China, Libya, Lebanon, Spain, Australia, San Diego, California, and the southeastern US 35%–80% of children are vitamin D deficient. We cannot always assume that just because there is more abundant sunlight outdoors vitamin D levels would be higher in summer season compared to winter.10 Nevertheless it is important to note that the study’s focus is not on the vitamin D absolute level but rather on its trend with seasonal change. Diabetes control as represented by HbA1c seems to be affected by seasonality with a mean rise of 0.175% ± 1.46%. These results did not reach statistical significance in our study but showed a trend for better control of glycemia during the end of the cloudy months.
In this study, however, no correlation could be found between diabetes control and variation of vitamin D level in a population of Lebanese with T1DM. Moreover, vitamin D levels tend to significantly increase at the end of the summer season and this is associated with better blood sugar control.
Future studies are needed with a larger sample size and a standardized questionnaire for the level of exercise, accuracy of insulin dosing, and timing of insulin injection. Such studies will provide more data on any possible relationship between vitamin D and diabetes pathogenesis and control.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.American Diabetes Association. Standards of medical care in diabetes– 2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: a systematic review and meta-analysis. Arch Dis Child. 2008;93(6):512–517. doi: 10.1136/adc.2007.128579. [DOI] [PubMed] [Google Scholar]
- 3.Mohr SB, Garland CF, Gorham ED, Garland FC. The association between ultraviolet B irradiance, vitamin D status and incidence rates of type 1 diabetes in 51 regions worldwide. Diabetologia. 2008;51(8):1391–1398. doi: 10.1007/s00125-008-1061-5. [DOI] [PubMed] [Google Scholar]
- 4.Sloka S, Grant M, Newhook LA. Time series analysis of ultraviolet B radiation and type 1 diabetes in Newfoundland. Pediatr Diabetes. 2008;9(2):81–86. doi: 10.1111/j.1399-5448.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- 5.Stene LC, Ulriksen J, Magnus P, Joner G. Use of cod liver oil during pregnancy associated with lower risk of Type I diabetes in the offspring. Diabetologia. 2000;43(9):1093–1098. doi: 10.1007/s001250051499. [DOI] [PubMed] [Google Scholar]
- 6.Soltesz G, Patterson CC, Dahlquist G EURODIAB Study Group. Worldwide childhood type 1 diabetes incidence – what can we learn from epidemiology? Pediatr Diabetes. 2007;8(Suppl 6):6–14. doi: 10.1111/j.1399-5448.2007.00280.x. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. International Diabetes Federation [homepage on the Internet] Geneva: World Health Organization; Feb 6, 2007. [Accessed August 2, 2011]. Available from: www.who.int/diabetes. [Google Scholar]
- 8.Mathieu C, Gysemans C, Giulietti A, Bouillon R. Vitamin D and diabetes. Diabetologia. 2005;48(7):1247–1257. doi: 10.1007/s00125-005-1802-7. [DOI] [PubMed] [Google Scholar]
- 9.Alemzadeh R, Kichler J, Babar G, Calhoun M. Hypovitaminosis D in obese children and adolescents: relationship with adiposity, insulin sensitivity, ethnicity, and season. Metabolism. 2008;57(2):183–191. doi: 10.1016/j.metabol.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 10.Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006;116(8):2062–2072. doi: 10.1172/JCI29449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lips P. Vitamin D physiology. Prog Biophys Mol Biol. 2006;92(1):4–8. doi: 10.1016/j.pbiomolbio.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353–373. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 13.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 14.Mathieu C, Badenhoop K. Vitamin D and type 1 diabetes mellitus: state of the art. Trends Endocrinol Metab. 2005;16(6):261–266. doi: 10.1016/j.tem.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Palomer X, Gonzalez-Clemente JM, Blanco-Vaca F, Mauricio D. Role of vitamin D in the pathogenesis of type 2 diabetes mellitus. Diabetes Obes Metab. 2008;10(3):185–197. doi: 10.1111/j.1463-1326.2007.00710.x. [DOI] [PubMed] [Google Scholar]
- 16.Luong K, Nguyen LT, Nguyen DN. The role of vitamin D in protecting type 1 diabetes mellitus. Diabetes Metab Res Rev. 2005;21(4):338–346. doi: 10.1002/dmrr.557. [DOI] [PubMed] [Google Scholar]
- 17.Mathieu C, Waer M, Laureys J, Rutgeerts O, Bouillon R. Prevention of autoimmune diabetes in NOD mice by 1,25 dihydroxyvitamin D3. Diabetologia. 1994;37(6):552–558. doi: 10.1007/BF00403372. [DOI] [PubMed] [Google Scholar]
- 18.Zella JB, McCary LC, DeLuca HF. Oral administration of 1,25 dihydroxyvitamin D3 completely protects NOD mice from insulin-dependent diabetes mellitus. Arch Biochem Biophys. 2003;417(1):77–80. doi: 10.1016/s0003-9861(03)00338-2. [DOI] [PubMed] [Google Scholar]
- 19.Greer RM, Rogers MA, Bowling FG, et al. Australian children and adolescents with type 1 diabetes have low vitamin D levels. Med J Aust. 2007;187(1):59–60. doi: 10.5694/j.1326-5377.2007.tb01130.x. [DOI] [PubMed] [Google Scholar]
- 20.Littorin B, Blom P, Schölin A, et al. Lower levels of plasma 25-hydroxyvitamin D among young adults at diagnosis of autoimmune type 1 diabetes compared with control subjects: results from the nationwide Diabetes Incidence Study in Sweden (DISS) Diabetologia. 2006;49(12):2847–2852. doi: 10.1007/s00125-006-0426-x. [DOI] [PubMed] [Google Scholar]
- 21.Arabi A, El Rassi R, El-Hajj Fuleihan G. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat Rev Endocrinol. 2010;6(10):550–561. doi: 10.1038/nrendo.2010.146. [DOI] [PubMed] [Google Scholar]
- 22.Moltchanova EV, Schreier N, Lammi N, Karvonen M. Seasonal variation of diagnosis of Type 1 diabetes mellitus in children worldwide. Diabet Med. 2009;26(7):673–678. doi: 10.1111/j.1464-5491.2009.02743.x. [DOI] [PubMed] [Google Scholar]
- 23.Wagner CL, Taylor SN, Hollis BW. Does vitamin D make the world go ‘round’? Breastfeed Med. 2008;3(4):239–250. doi: 10.1089/bfm.2008.9984. [DOI] [PMC free article] [PubMed] [Google Scholar]