Abstract
OBJECTIVE
We tested the hypothesis that elevated transferrin saturation is associated with an increased risk of any form of diabetes, as well as type 1 or type 2 diabetes separately.
RESEARCH DESIGN AND METHODS
We used two general population studies, The Copenhagen City Heart Study (CCHS, N = 9,121) and The Copenhagen General Population Study (CGPS, N = 24,195), as well as a 1:1 age- and sex-matched population-based case-control study with 6,129 patients with diabetes from the Steno Diabetes Centre and 6,129 control subjects, totaling 8,535 patients with diabetes and 37,039 control subjects.
RESULTS
In the combined studies, odds ratios in those with transferrin saturation ≥50% vs. <50% were 2.1 (95% CI 1.3–3.4; P = 0.003) for any form of diabetes; 2.6 (1.2–5.6; P = 0.01) for type 1 diabetes; and 1.7 (1.4–2.1; P = 0.001) for type 2 diabetes.
CONCLUSIONS
Elevated transferrin saturation confers a two- to threefold increased risk of developing any form of diabetes, as well as type 1 and type 2 diabetes separately.
Diabetes is a common late complication of hereditary hemochromatosis, an autosomal-recessive disease with lifelong iron accumulation in metabolically highly active tissues, primarily in the endocrine pancreas, the myocardium, the synovial membrane, the anterior pituitary lobe, and the liver (1). Diabetes as a consequence of hemochromatosis is characterized by insulin resistance and β-cell destruction (2), and the metabolic phenotype can therefore mimic type 2 diabetes and nonautoimmune type 1 diabetes (3).
The defects in insulin-producing and insulin-sensitive tissues are most likely caused by iron-dependent catalysis via the Fenton reaction of reactive oxygen radical species, which impair insulin signaling in skeletal muscle and liver and cause β-cell destruction due to an insufficient β-cell–deficient antioxidant defense (4). It is unclear, however, whether elevated transferrin saturation confers an increased risk of diabetes in the general population. Our aim was to test this hypothesis in three large populations (Supplementary Data online).
RESEARCH DESIGN AND METHODS
Details are provided in the Supplementary Data online.
Participants
The studies were approved by the appropriate institutional review boards and ethical committees. The investigation was conducted according to the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from participants. All participants were white and of Danish descent. There was no overlap of individuals between the three studies, thus allowing independent confirmation of findings. We included all attending individuals with eligible transferrin saturation.
General population studies
On the basis of the Danish Central Person Registration number, The Copenhagen City Heart Study (CCHS, N = 9,121; recruited 1991–1994) (5) and The Copenhagen General Population Study (CGPS, N = 24,195; recruited 2003–2007) (6) recruited participants randomly from the general population of Copenhagen, Denmark. The studies included a self-administered questionnaire, a physical examination, and blood samples.
Population-based case-control study
We recruited (2001–2007) consecutively 6,129 population-based patients with diabetes from Copenhagen County who attended the Steno Diabetes Centre.
Transferrin saturation
Transferrin saturation (percentage) was determined as iron levels (in micromoles per liter) divided by 2 × transferrin levels (in micromoles per liter) × 100. Transferrin was measured by turbidimetry, and iron levels were measured by colorimetry using a Konelab autoanalyzer (Thermo Fisher Scientific, Waltham, MA) and Hitachi 912 (Roche Diagnostics, Indianapolis, IN). Transferrin saturation >50% was chosen as suggestive of increased transferrin saturation, in accordance with accepted clinical practice (7–9). Transferrin saturation range was 2.8–236% (CCHS), 0.9–130% (CGPS), and 0.1–97% (population-based case-control study). Increased transferrin saturation was detected in 355, 346, and 361 individuals in the CCHS, CGPS, and in the population-based case-control study, respectively.
Diabetes end point definitions
A combination of ICD codes, self-reported diabetes (yes/no), information on antidiabetic medication, and a nonfasting glucose >11 mmol/L was used.
Statistics
Cox proportional hazards regression with age as timescale (i.e., left truncation) was used to estimate hazard ratios (HRs) with 95% CIs. The assumption of proportional hazards was tested with the use of Schoenfeld residuals, and no violations were observed. Analyses not stratified for sex were adjusted for sex. In the case-control study, conditional logistic regression models were used to estimate odds ratios (ORs) with 95% CI.
RESULTS
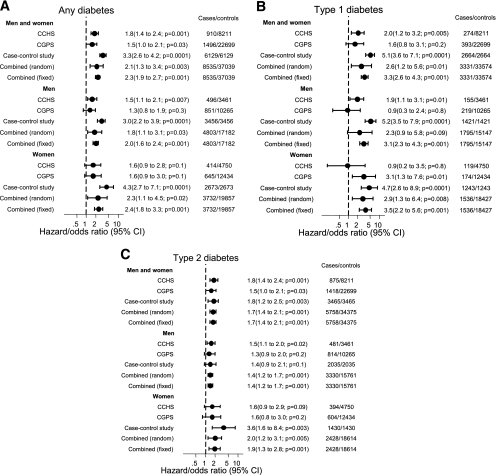
Details are provided in the Supplementary Data online. The HRs (95% CI) for any form of diabetes in individuals with transferrin saturation of ≥50% vs. <50% were 1.8 (1.4–2.4; P = 0.001) in CCHS and 1.5 (1.0–2.1; P = 0.03) in CGPS (Fig. 1A). In the case-control study, the OR (95% CI) for any form of diabetes in individuals with transferrin saturation of ≥50% vs. <50% was 3.3 (2.6–4.2; P = 0.0001). In the combined studies, OR in the meta-analysis under the random-effects model was 2.1 (1.3–3.4; P = 0.003) for any form of diabetes in those with transferrin saturation ≥50% vs. <50% (Fig. 1A); statistical heterogeneity was Q = 17 and P = 0.001. The ORs for type 1 and type 2 diabetes in the combined studies in the meta-analysis under the random-effects model were 2.6 (1.2–5.6; P = 0.01) and 1.7 (1.4–2.1; P = 0.001), respectively, in those with transferrin saturation ≥50% vs. <50% (Fig. 1B and C); statistical heterogeneity was Q = 15 and P = 0.001 for type 1 diabetes and Q = 0.7 and P = 0.7 for type 2 diabetes.
Figure 1.
Risk of diabetes according to transferrin saturation ≥50% vs. <50% in the CCHS, the CGPS, a case-control study, and combined. A: Any form of diabetes. B: Type 1 diabetes. C: Type 2 diabetes. The case-control study comprised patients with diabetes from the Steno Diabetes Centre in Copenhagen, and control subjects were ascertained as in the CGPS but from a different sample than those included in the CGPS-only study. Combined, there was no overlap of individuals among these three studies, thus allowing independent confirmation of findings. 95% CIs are shown. Heterogeneity for the combined results for men and women was Q = 17 and P = 0.001 for any form of diabetes, Q = 15 and P = 0.001 for type 1 diabetes, and Q = 0.7 and P = 0.7 for type 2 diabetes.
CONCLUSIONS
Details are provided in the Supplementary Data online. Here we demonstrated that transferrin saturation ≥50% was associated with a two- to threefold increased risk of developing any form of diabetes, as well as type 1 diabetes and type 2 diabetes separately. This is the first and largest population-based study that consistently demonstrates transferrin saturation as a risk marker of any form of diabetes, and of type 1 and type 2 diabetes separately, in three independent studies. There was no overlap of individuals between the three studies, thus allowing independent confirmation of findings.
Because the risk of developing diabetes observed in this study increased with the degree of iron overload for which there is a simple treatment (phlebotomy), 1–3% of diabetes cases in the general population and 7% of cases in a diabetes population likely could be resolved if patients received such a treatment earlier in life, equal to ∼300 patients/million in Denmark. These findings reinforce the importance of investigating iron overload in the differential diagnosis of secondary causes of diabetes and support arguments in favor of screening for iron overload in the general population. A health-economic analysis of the cost/benefit ratio of screening for elevated iron saturation in the general or in diabetic populations may help to determine the public health consequences of this study (e.g., advice against iron supplements), and whether large prospective intervention studies should be initiated to show causality between elevated transferrin saturation and diabetes.
Supplementary Material
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
C.E. contributed to the literature search and the study design, analyzed and interpreted data, wrote and edited the manuscript, and created the figures and tables. T.M.-P. contributed to the literature search and the study design, collected and interpreted data, and edited the manuscript. H.U.A. contributed to the study design, collected and interpreted the data, and edited the manuscript. A.T.-H. contributed to the study design, collected and interpreted the data, and edited the manuscript. M.F. collected the data and edited the manuscript. H.B. contributed to the study design, interpreted the data, and edited the manuscript. B.G.N. contributed to the literature search and the study design, collected the data, analyzed and interpreted the data, edited the manuscript, and created the figures and tables.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-0416/-/DC1
References
- 1.Pietrangelo A. Hereditary hemochromatosis—a new look at an old disease. N Engl J Med 2004;350:2383–2397 [DOI] [PubMed] [Google Scholar]
- 2.Hanson EH, Imperatore G, Burke W. HFE gene and hereditary hemochromatosis: a HuGE review. Human Genome Epidemiology. Am J Epidemiol 2001;154:193–206 [DOI] [PubMed] [Google Scholar]
- 3.Ellervik C, Mandrup-Poulsen T, Nordestgaard BG, et al. Prevalence of hereditary haemochromatosis in late-onset type 1 diabetes mellitus: a retrospective study. Lancet 2001;358:1405–1409 [DOI] [PubMed] [Google Scholar]
- 4.Oberley LW. Free radicals and diabetes. Free Radic Biol Med 1988;5:113–124 [DOI] [PubMed] [Google Scholar]
- 5.Ellervik C, Tybjærg-Hansen A, Grande P, Appleyard M, Nordestgaard BG. Hereditary hemochromatosis and risk of ischemic heart disease: a prospective study and a case-control study. Circulation 2005;112:185–193 [DOI] [PubMed] [Google Scholar]
- 6.Ellervik C, Tybjærg-Hansen A, Nordestgaard BG. Total mortality by transferrin saturation levels: two general population studies and a metaanalysis. Clin Chem 2011;57:459–466 [DOI] [PubMed] [Google Scholar]
- 7.Cartwright GE, Edwards CQ, Kravitz K, et al. Hereditary hemochromatosis. Phenotypic expression of the disease. N Engl J Med 1979;301:175–179 [DOI] [PubMed] [Google Scholar]
- 8.Edwards CQ, Griffen LM, Goldgar D, Drummond C, Skolnick MH, Kushner JP. Prevalence of hemochromatosis among 11,065 presumably healthy blood donors. N Engl J Med 1988;318:1355–1362 [DOI] [PubMed] [Google Scholar]
- 9.Olynyk JK, Cullen DJ, Aquilia S, Rossi E, Summerville L, Powell LW. A population-based study of the clinical expression of the hemochromatosis gene. N Engl J Med 1999;341:718–724 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.