Abstract
Topiramate is a sulfa-derivative antiepileptic drug which is also used for other indications such as essential tremor. A 79-year-old male was admitted to our center due to acute bilateral painless decline of vision. One month before admission, he had experienced essential tremor and treatment with topiramate 50 mg/day and propranolol 40 mg/day. Best-corrected visual acuity was 20/800 OD and 20/600 OS. Both eyes had normal anterior chamber depths and irides. Intraocular pressure was 10 mm Hg in the right eye and 11 mm Hg in the left eye. Retinal examination showed notable choroidal detachments in all quadrants of the periphery, which were confirmed by ultrasonography. Refraction showed no myopic shift. The administration of topiramate was discontinued as a potential causative agent for this condition. During follow-up, choroidal detachment and visual acuity gradually resolved. In this study, we described the first case of isolated massive choroidal detachment induced by topiramate.
Key Words: Topiramate, Choroidal detachment, Side effect, Sulfa derivative
Introduction
Topiramate is a sulfa-derivative antiepileptic drug which is also used for other indications such as migraine, personality disorders, weight loss, neuropathic pain and, recently, essential tremor [1, 2]. The pharmacodynamic picture of this drug generally reflects the modulation of voltage-gated sodium and calcium channels, increase of GABAergic inhibition, blockage of glutamate receptors and mild carbonic anhydrase inhibition [3]. To date, several side effects of this drug are reported, of which ophthalmic manifestations are of special importance. The most clinically significant ophthalmic side effects are angle-closure glaucoma, myopic shift, diplopia and nystagmus. The precise mechanisms responsible for such adverse effects are, however, not completely understood [4].
Serous choroidal detachment (transudation of fluid into the suprachoroidal space) may be due to globe hypotony of any etiology or exudation of serum caused by inflammation or other causes [5]. Choroidal detachment is generally known as a probable complication of sensitized eyes following surgery. Typically, these cases are concurrently treated with ocular hypotensive drugs [6]. Moreover, there are some instances in which the occurrence of choroidal detachment is not explainable by common mechanisms [5].
To our knowledge, massive choroidal detachment following the administration of topiramate has never been described in previous case reports. The purpose of this report was to illustrate the clinical and paraclinical features of a patient who experienced the above-mentioned adverse event. We also aimed to discuss the possible pathogenic links of topiramate by comparing the features of our case with those of cases previously reported in the literature.
Case Report
A 79-year-old male was admitted to our center for further evaluation of acute bilateral painless decline of vision. The patient's past clinical history included 80 mg/day aspirin intake due to unstable angina for 11 years. He denied any past history of smoking or addiction.
On neurological examination, mental status was found to be normal. The patient had no significant neurological disorder until 1 month before admission, when he experienced essential tremor. As a result, treatment with topiramate 50 mg/day and propranolol 40 mg/day was started 2 weeks before his admission due to ophthalmic symptoms. This treatment was prescribed by a neurologist.
He underwent uncomplicated cataract surgery 11 years ago for the right eye and 9 years ago for the left eye, and both eyes had intraocular lenses. He had no clinical history of glaucoma surgery or anti-glaucoma medications.
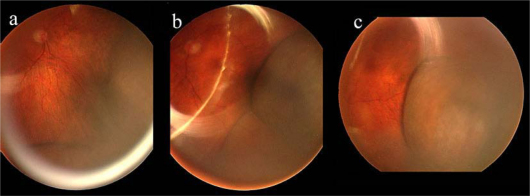
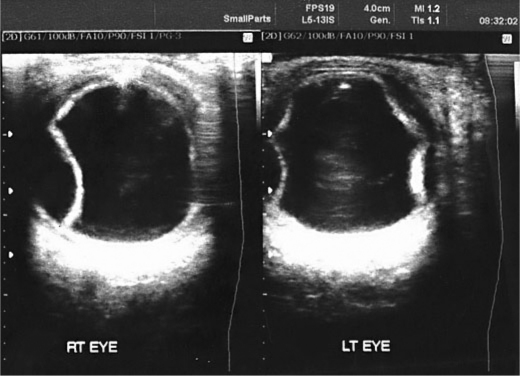
On ophthalmologic examination, best-corrected visual acuity was 20/800 OD and 20/600 OS. The eyelids showed meibomian gland dysfunction. Both eyes showed mild hyperemia and had normal anterior chamber depths and irides. Pupillary reactions to light and near stimuli were normal, and no pupillary afferent defect was present. Ocular motility was normal. Intraocular pressure was 10 mm Hg in the right and 11 mm Hg in the left eye. Anterior vitreous examination showed no abnormality. Retinal examination revealed posterior pole drusen compatible with mild dry age-related macular degeneration and notable choroidal detachments in all quadrants of the periphery (fig. 1), which were confirmed by ultrasonography (fig. 2). Refraction showed no myopic shift.
Fig. 1.
Fundus photographies of both eyes showing massive choroidal detachment. a Right eye. b, c Left eye.
Fig. 2.
B scan ultrasonography confirming massive choroidal detachment in both eyes.
The administration of topiramate was discontinued as a potential causative agent for this condition; however, we did not reduce the dosage of propranolol. We continued monitoring the patient's status daily. Within 3 days, visual acuity improved to 20/200 OD and 20/60 OS. This improvement continued until day 7, when visual acuity gradually exceeded to 20/25 OD and 20/30 OS. By the end of day 7, choroidal detachment resolved as well.
Discussion
We described the first case of isolated massive choroidal detachment induced by topiramate. However, it is worth noting that in a study by the National Registry of Drug-Induced Ocular Side Effects, 9 cases of suprachoroidal effusion were concisely mentioned regardless of the severity of their complication. The data on these subjects were extracted from the records of the World Health Organization or other related/similar organizations [4]. Nevertheless, to the best of our knowledge, neither precise features of these cases, e.g. the severity of effusion, were published elsewhere, nor any of them were specified to present massive choroidal detachment.
A review of the ophthalmology literature reveals that, to date, there are several reports describing bilateral angle closure following topiramate intake [4, 7, 8, 9]. Our patient did not exhibit myopic changes or a shallow anterior chamber, although such side effects have been frequently observed with the use of this drug.
The term ‘ciliochoroidal effusion syndrome’ was first proposed by Ikeda et al. [10] to describe the phenomena induced by topiramate and other sulfa derivatives. This syndrome represents a category of symptoms including ciliochoroidal effusion, forward displacement of the lens-iris diaphragm and, consequently, angle narrowing and myopic shift. Accordingly, in our case choroidal effusion without development of angle closure or myopic shift could be due to lack of crystalline lens.
As mentioned previously, the main cause of choroidal detachment is generally believed to be ocular hypotony following surgical procedures [6]. In our literature review, we could identify an interesting case by Doherty et al. [11] that shares decisive common features with ours. This patient was reported to manifest bilateral choroidal detachment after administration of topical dorzolamide. Taking together, four main similarities are worth noting: (1) both patients had a past history of uncomplicated cataract surgery; (2) intraocular pressure was within normal limits in both patients; (3) dorzolamide and topiramate are both sulfa-derivative drugs, and (4) similar to dorzolamide which is a carbonic anhydrase antagonist, topiramate is also suggested to be ‘a mild carbonic anhydrase inhibitor’ [3]. Accordingly, the authors concluded that the cause of choroidal detachment is not always hypotony and postulated that it may also be due to hypersensitivity to dorzolamide. Our case provides further evidence in favor of this hypothesis, and this raises the question whether the cause of choroidal detachment in our case was hypersensitivity to topiramate as this is a sulfa-derivative drug as well. From another point of view, it is well known that carbonic anhydrase antagonists can cause choroidal detachment [12], and this may explain why the administration of dorzolamide and topiramate results in this adverse effect.
As a conclusion, we propose that the administration of topiramate and perhaps other sulfa-derivative drugs might be eligible to be added as a differential diagnosis of choroidal detachment.
Disclosure Statement
The authors have no conflicts of interest.
References
- 1.Mirza N, Marson AG, Pirmohamed M. Effect of topiramate on acid-base balance: extent, mechanism and effects. Br J Clin Pharmacol. 2009;68:655–661. doi: 10.1111/j.1365-2125.2009.03521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadeghi R, Ondo WG. Pharmacological management of essential tremor. Drugs. 2010;70:2215–2228. doi: 10.2165/11538180-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 3.Kjellström S, Bruun A, Isaksson B, Eriksson T, Andréasson S, Ponjavic V. Retinal function and histopathology in rabbits treated with Topiramate. Doc Ophthalmol. 2006;113:179–186. doi: 10.1007/s10633-006-9027-8. [DOI] [PubMed] [Google Scholar]
- 4.Fraunfelder FW, Fraunfelder FT, Keates EU. Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology. 2004;111:109–111. doi: 10.1016/j.ophtha.2003.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Elagouz M, Stanescu-Segall D, Jackson TL. Uveal effusion syndrome. Surv Ophthalmol. 2010;55:134–145. doi: 10.1016/j.survophthal.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Alexander P, Ramirez-Florez S. Hypotony and choroidal detachment as a complication of travoprost after trabeculectomy surgery. Eye (Lond) 2008;22:736–737. doi: 10.1038/eye.2008.58. [DOI] [PubMed] [Google Scholar]
- 7.Banta JT, Hoffman K, Budenz DL, Ceballos E, Greenfield DS. Presumed topiramate-induced bilateral acute angle-closure glaucoma. Am J Ophthalmol. 2001;132:112–114. doi: 10.1016/s0002-9394(01)01013-3. [DOI] [PubMed] [Google Scholar]
- 8.Rhee DJ, Goldberg MJ, Parrish RK. Bilateral angle-closure glaucoma and ciliary body swelling from topiramate. Arch Ophthalmol. 2001;119:1721–1723. [PubMed] [Google Scholar]
- 9.Dehghani A, Rezaei L, Peyman A. Acute myopia and angle closure glaucoma associate with topiramate use: a case series. Am J Case Rep. 2010;11:271–273. [Google Scholar]
- 10.Ikeda N, Ikeda T, Nagata M, Mimura O. Ciliochoroidal effusion syndrome induced by sulfa derivatives. Arch Ophthalmol. 2002;120:1775. doi: 10.1001/archopht.120.12.1775. [DOI] [PubMed] [Google Scholar]
- 11.Doherty MD, Wride NK, Birch MK, Figueiredo FC. Choroidal detachment in association with topical dorzolamide: is hypotony always the cause? Clin Experiment Ophthalmol. 2009;37:750–752. doi: 10.1111/j.1442-9071.2009.02113.x. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg S, Gallily R, Bishara S, Blumenthal EZ. Dorzolamide-induced choroidal detachment in a surgically untreated eye. Am J Ophthalmol. 2004;138:285–286. doi: 10.1016/j.ajo.2004.02.070. [DOI] [PubMed] [Google Scholar]