Abstract
Background
Though spiritual care is associated with less aggressive medical care at the end of life (EOL), it remains infrequent. It is unclear if the omission of spiritual care impacts EOL costs.
Methods
Prospective, multi-site study of 339 advanced cancer patients accrued September 2002–August 2007 from an outpatient setting and followed until death. Spiritual care was measured by patients' reports that the healthcare team supported their religious/spiritual needs. EOL costs in the last week were compared among patients reporting their spiritual needs were inadequately supported versus those well-supported. Analyses adjusted for confounders (e.g., EOL discussions).
Results
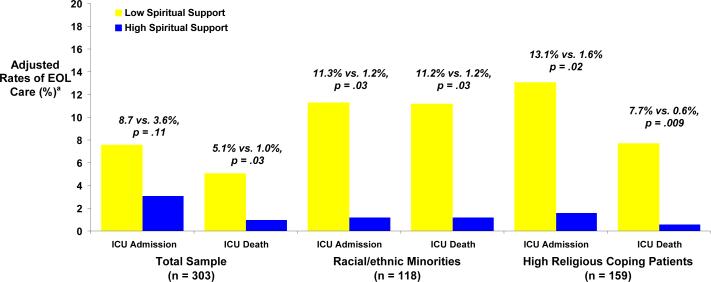
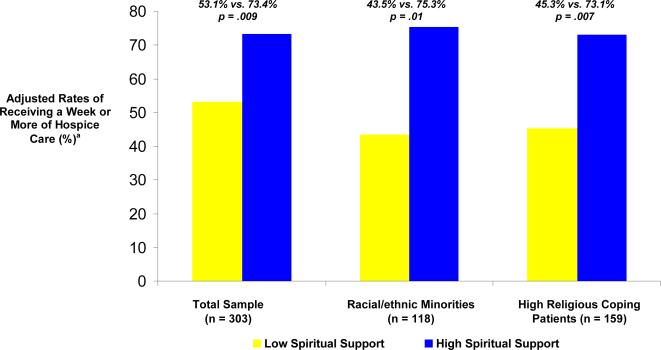
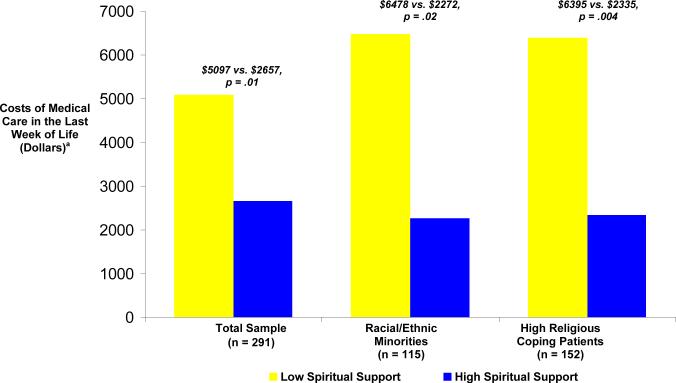
Patients reporting their R/S needs were inadequately-supported by clinic staff were less likely to receive a week or more of hospice (54% vs. 72.8%; p=.01) and more likely to die in an ICU (5.1% vs. 1.0%, p=.03). Among minorities and high religious coping patients, those reporting poorly supported R/S needs received more ICU care (11.3% vs. 1.2%, p=.03 and 13.1% vs. 1.6%, p=.02, respectively), less hospice (43.% vs. 75.3% ≥ a week of hospice, p=.01 and 45.3% vs. 73.1%, p=.007, respectively) and had increased ICU deaths (11.2% vs. 1.2%, p=.03 and 7.7% vs. 0.6%, p=.009, respectively). EOL costs were higher when patients reported their spiritual needs were inadequately supported ($4947 vs. $2833, p=.03), particularly among minorities ($6533 vs. $2276, p=.02) and high religious copers ($6344 vs. $2431, p=.005).
Conclusion
Cancer patients reporting their spiritual needs are not well-supported by the healthcare team have higher EOL costs, particularly among minorities and high religious coping patients.
INTRODUCTION
Spiritual care is recognition of the role of patient religion and/or spirituality (R/S) in illness and attention to R/S concerns as part of medical care. Spiritual care is an integral component of palliative care1 supported by data among patients with advanced illness demonstrating: (1) the importance of R/S in the illness experience,2–5 including its central role in preserving patient quality of life (QOL),6, 7 (2) frequent R/S concerns among these patients,2, 4, 5, 8 and (3) patients' expressed wishes for spiritual care as part of their medical care.7, 9
R/S is not only associated with patient QOL in the setting of advanced illness;6 recent data suggest that R/S also influences patient EOL care.10–12 For example, religiousness and religious coping (e.g., seeking God's support in confronting the stress of illness) are associated with preferences for3, 11, 13 and receipt of11 aggressive medical treatment (e.g., mechanical ventilation) at the EOL. The receipt of aggressive medical care at the EOL is an outcome with broad implications given its associations with heightened symptom burden and distress in patients,14 worse bereavement outcomes in surviving family members,14 and high costs.15
Results from the Coping with Cancer study demonstrate that spiritual care is associated with better patient QOL near death and reduced EOL medical care intensity10 but remains infrequent.3 These findings raise the questions: (1) Is the lack of spiritual care by the healthcare team associated with medical care costs at EOL; and (2) given higher rates of aggressive EOL care among racial/ethnic minorities15 and high religious coping patients,11 is insufficient attention to spiritual needs associated with greater EOL costs among these at-risk patient groups? We hypothesized that patients whose spiritual needs are not well-supported by the healthcare team would have increased EOL medical care costs, and that costs implications would be greatest among racial/ethnic minorities and high religious coping patients.
METHODS
Study Sample
Patients were recruited from September 1, 2002 to August 31, 2007 from seven outpatient sites: Dana-Farber Cancer Institute, Massachusetts General Hospital, Boston, Massachusetts; New Hampshire Oncology Hematology, Hookset, New Hampshire; Parkland Hospital, Simmons Comprehensive Cancer Center, Dallas, Texas; Veterans Affairs Connecticut Comprehensive Cancer Clinics, West Haven, Connecticut; and Yale University Cancer Center, New Haven, Connecticut. Eligibility criteria included an advanced cancer diagnosis with disease refractory to first-line chemotherapy; age ≥21 years; presence of an informal (non-paid) caregiver; and adequate stamina to complete the interview. Exclusion criteria for patient-caregiver dyads included patient or caregiver: meeting criteria for dementia or delirium by neurocognitive examination or inability to speak English or Spanish. All participants provided written, informed consent according to protocols approved by participating centers' human subjects committees.
Study Protocol
Research staff underwent a two-day training program in the protocol, chart extraction, and interviewing. Potential participants were identified from outpatient appointment schedules; recruitment did not include specific reference to R/S. Upon enrollment, patients participated in a baseline interview. Patients' medical records were reviewed to extract disease/treatment information. A second assessment was performed within three weeks after the participant's death, including chart extraction to obtain EOL care information and a post-mortem interview of a caregiver present during the final week of life.
Of 920 eligible patients approached, 658 (72%) participated. The most common reasons for nonparticipation included “not interested” (n=109) and “caregiver refuses” (n=35). There were no significant differences between non-participants and participants in gender, age, race, or education. At the time of completion of active study follow-up (August 28, 2008), 366 had died and a post-mortem interview was performed; 40 lacked complete post-mortem or spiritual care data, resulting in a final sample of 339 (93% of 366).
Baseline Measures
Spiritual care
Patients rated the degree to which their spiritual needs were met by the healthcare team. Spiritual care was dichotomized to low (spiritual needs supported not at all, to a small extent, and to a moderate extent) versus high (spiritual needs largely or completely supported) consistent with findings from our prior report.10 A detailed description of measures of spiritual care and religiousness are available in our prior report.10
Religious variables
Patients rated their religiousness and spiritual support received from religious communities. Pargament's validated religious coping questionnaire16 measured how patients utilize their religious beliefs to adapt to the stress of illness. Positive religious coping (e.g., “seeking God's love and care”) is the most common form of religious coping.11, 16 Negative religious coping is less common11 and often indicates existential distress.17 Given our previous report indicating greater aggressive EOL care in patients endorsing high (above the median score of 12) positive religious coping,11 positive religious coping was similarly dichotomized.
Other baseline variables
The previously-validated McGill Quality of Life questionnaire18, 19 was used to assess baseline patient QOL, existential well-being and social support. The patient-doctor relationship, history of an EOL discussion with a physician, presence of advance directives, EOL treatment preferences, and terminal illness awareness were also assessed. Age, gender, race/ethnicity (White; Black; Asian American, Pacific Islander, or Indian; Hispanic; or other dichotomized to White versus non-White), education (years), and insurance status were patient-reported. Karnofsky performance status was obtained by physician assessment.
End-of-life Care
End-of-life care
Hospice – a predictor of EOL costs20 and QOL14 among cancer patients – was recorded as none, <1 week, 1–4 weeks, 5–8 weeks, 9–12 weeks, or >12 weeks, and dichotomized to ≥1 week vs. <1week/no hospice (median split). Days of ICU care with and without mechanical ventilation – key determinants of EOL costs15 – were recorded and dichotomized as any vs. no ICU care (median split) in the last week. Location of death – another established aggressiveness EOL care measure21 known to impact costs22 – was recorded as ICU, non-ICU hospital, home, home with hospice, inpatient hospice, nursing home/long-term care facility and dichotomized to death in an ICU versus other locations. Receipt of resuscitation and chemotherapy in the last week of life was also recorded.
Costs of End-of-life Care
Medical care costs over the last seven days of life were estimated and adjusted to reflect costs as of January 1, 2010.23 ICU costs were based on published estimates (non-ventilated ICU care, day 1=$4646, day 2=$4149, day 3 or more=$3696/day; and ventilated ICU care, day 1=$7061, day 2=$5666, day 3 or more=$4946/day).24 If the number of ICU days was less than seven and the patient died in the hospital, the patient was considered to have been in a non-ICU hospital setting for the remaining days (estimated at $1803/day25), an assumption supported by data indicating that patients with an ICU stay require an average additional six days in the non-ICU hospital.24 Among patients receiving less than seven days of ICU care who died in a non-hospital setting, the remaining days and associated costs were split evenly between a non-ICU hospital setting25 and their death setting (cost estimates of those locations described below). Resuscitation costs were estimated for patients who did not have costs estimated by an ICU admission (as ICU/hospitalization costs include resuscitation costs) and were based on the Agency for Health Research and Quality Healthcare Utilization Project estimate ($10,464, average hospital stay of 4 days).26 The remaining three days were based on average medical costs in the last month of life ($339/day).15
Hospice costs were based on Center for Medicare and Medicaid Services (CMS) 2010 reimbursement rates (home hospice=$143/day and inpatient hospice=$636/day).27 EOL costs for patients receiving seven or more days of hospice were based on the inpatient or home hospice care daily costs. Patients receiving less than one week of hospice were considered to have 3.5 days of hospice with the remaining 3.5 days based on average daily costs in the last month of life.15 Among patients who did not receive hospice or aggressive care, costs were estimated according to their place of death. Patients dying in a hospital were considered to have 2.3 days of a hospital stay preceding their death per the Dartmouth Atlas estimates.28 The remaining 4.7 days were based on average daily costs in the last month.15 Among patients dying at home, all seven days were estimated by average daily costs in the last month of life.15 Patients dying in a long-term care facility were considered to have been in that facility for seven days given data indicating median stays are 142 days,29 with average costs based on average CMS reimbursement rates for 2010 ($399/day).30 Receipt of chemotherapy in the last week of life was estimated at $821 (25% of estimated $3281 per 4 weeks).31
Statistical Analysis
T-tests (continuous variables) and χ2 tests (ordinal and dichotomous variables) were used to compare baseline characteristics among those reporting high versus low spiritual support from the healthcare team. Logistic regression assessed the relationship between patient-reported spiritual care and receipt of ICU care in the last week of life, receipt of at least 1 week of hospice care, and of dying in an ICU. Analyses were adjusted for predictors of EOL care, including race,15, 32–34 EOL treatment preferences,14, 35 EOL discussion,14, 36 advance care planning,37 positive religious coping,11 and religiousness.3, 13 EOL care models were also adjusted for variables potentially related to spiritual care and EOL care, including education, health insurance status, recruitment site (Northern versus Southern sites), baseline existential well-being and social support, religious community spiritual support, the patient-physician relationship, and terminal illness awareness. Additional confounds considered were: age, gender, performance status, QOL, and negative religious coping; variables were retained when the p-value remained significant (p<.05) after controlling for other confounds. Multivariable models were repeated among racial/ethnic minorities and high religious coping patients. Hierarchical linear modeling with clustering by site was performed to further assess possible confounding by site. Final models were used to generate adjusted rates of any ICU care in the last week of life, receipt of 1 week or more of hospice, and death in an ICU. The same models were used to assess the relationship between patient-reported spiritual care and medical care costs in the last week of life, repeated as an ANOVA procedure with least square means to obtain adjusted cost estimates for the full sample, racial/ethnic minorities and high religious coping patients. Statistical analyses were performed with SAS version 9.1 (SAS Institute Inc, Cary, North Carolina). All reported p-values are two-sided and considered significant when less than .05.
RESULTS
Sample Characteristics
Baseline sample characteristics are shown in Table 1. Compared to patients reporting low support of their R/S needs, patients reporting high support of the R/S needs were more likely to be of non-white race/ethnicity, were less likely to have health insurance, were more religious, and endorsed greater positive religious coping. High spiritual support patients also reported greater existential well-being and social support. Recruitment site differed between the two groups, with high spiritual support patients being more frequently recruited from Parkland hospital and less frequently from Yale Cancer Center.
Table 1.
Baseline characteristics of the study sample by spiritual care from the health care team (N=339)a
| Total Sample (n=339) | Low Spiritual Support (n=252) | High Spiritual Support (n=87) | p | |
|---|---|---|---|---|
| Age, M (SD) | 58.3 (12.6) | 58.6 (12.5) | 57.3 (12.8) | .38 |
| Male, n (%) | 183 (54.0) | 140 (55.6) | 43 (49.4) | .32 |
| Non-white race, n (%)b | 126 (37.2) | 85 (33.7) | 41 (47.1) | .02 |
| Married, n (%) | 200 (59.5) | 154 (61.6) | 46 (53.5) | .19 |
| Education, years, M (SD) | 12.4 (4.0) | 12.6 (4.3) | 11.8 (4.1) | .09 |
| Health insurance, n (%) | 190 (57.1) | 153 (61.7) | 38 (44.2) | .005 |
| Karnofsky performance status, M (SD)c | 63.4 (15.8) | 64.1 (17.6) | 61 (18.9) | .13 |
| Recruitment Site | ||||
| Yale Cancer Center (CT), n (%) | 66 (19.6) | 61 (24.2) | 5 (5.9) | |
| Veterans Association of Connecticut Cancer Center (CT), n (%) | 13 (3.4) | 12 (4.8) | 1 (1.2) | |
| Simmons Comprehensive Cancer Center (TX), n (%) | 34 (10.1) | 24 (9.5) | 10 (11.8) | |
| Parkland Hospital (TX), n (%) | 152 (45.1) | 103 (40.9) | 49 (57.7) | |
| Dana-Farber Cancer Institute/Massachusetts General Hospital (MA), n (%) | 7 (2.1) | 7 (2.8) | 0 (0) | |
| New Hampshire Oncology Hematology (NH), n (%) | 65 (19.3) | 45 (17.9) | 20 (23.5) | <.001 |
| McGill Quality of life, M (SD)d | 45.2 (14.0) | 45.0 (15.1) | .90 | |
| Existential well-being, M (SD)d | 44.9 (10.4) | 47.8 (9.7) | .02 | |
| Social support, M (SD)d | 17.0 (3.5) | 18.1 (2.8) | .006 | |
| Religiousness, n (%) | ||||
| Not at all important | 38 (11.2) | 36 (14.3) | 2 (2.3) | |
| Somewhat important | 71 (20.9) | 64 (25.4) | 7 (8.0) | |
| Very important | 230 (67.9) | 152 (60.3) | 79 (89.8) | <.001 |
| Positive religious coping, M (SD)e | 11.1 (6.4) | 10.2 (6.5) | 13.7 (5.4) | <.001 |
| Negative religious coping, M (SD)f | 2.0 (3.5) | 1.8 (3.4) | 2.5 (3.9) | .14 |
| Spiritual support from religious communities, n (%) | ||||
| Not at all | 110 (32.5) | 101 (40.1) | 9 (10.2) | |
| To a small extent | 42 (12.4) | 39 (15.5) | 4 (4.6) | |
| To a moderate extent | 43 (12.7) | 34 (13.5) | 9 (10.2) | |
| To a large extent | 54 (15.9) | 35 (13.9) | 19 (21.6) | |
| Completely supported | 90 (26.6) | 43 (17.1) | 47 (53.4) | <.001 |
| End-of-life discussion with a physician | 124 (36.6) | 88 (34.9) | 37 (42.1) | .23 |
| Patient-physician relationship, M (SD)g | 4.8 (0.5) | 4.7 (0.5) | 4.9 (0.4) | .09 |
| Preference for aggressive treatment measures at end of life, n (%)* | 86 (28.6) | 66 (30.0) | 20 (24.4) | .34 |
| Terminal illness awareness, n (%) | 86 (28.6) | 111 (45.0) | 31 (37.6) | .22 |
| Advanced care planning, n (%) | 186 (54.9) | 143 (56.8) | 43 (49.4) | .24 |
Abbreviations: M – mean; SD – standard deviation
Missing data in <3% of patients for the following variables: health insurance status, Karnofsky performance status, recruitment site, quality of life, existential well-being, social support, religiousness, positive religious coping, negative religious coping, patient-physician relationship, and terminal illness awareness. Data regarding preferences for aggressive treatment measures at end of life available for 301 patients.
Minority race ethnicity patients include 66 Black, 55 Hispanic, and 5 other race patients.
A measure of functional status that is predictive of survival, where 0 is dead and 100 is perfect health.d‡A validated measure of quality of life with five domains: overall quality of life, physical, psychological, existential, and social support. Existential items and support items were removed and used as separate predictors.
McGill quality of life possible scores 0 to 70. Social support possible scores 0 to 20. Existential well-being possible scores 0 to 60.
A measure of positive religious appraisals in coping with illness (e.g., I've been seeking God's love and care), scale 0 to 21.
A measure of negative religious appraisals in coping with illness (e.g., I've been wondering whether God has abandoned me), scale 0 to 21.
Measure of patient-physician relationship (scale 0–5) assessing patient: trust in the physician, sense of being cared for as a “whole person”, sense of being respected, respect for the physician, and comfort asking questions about care.
Medical Care Received in the Last Week of Life
Patients died a median of 111 (interquartile range 54–249) days after the baseline interview. In the last week of life, 35 patients (10.3%) received ICU care, and 25 (7.4%) died in an ICU. Most (n=248, 73.1%) received hospice care at EOL, and 199 (58.7%) received a week or more of hospice care. Adjusted estimates of receipt of ICU care in the last week of life, death in an ICU, and 1 week or more of hospice care according to receipt of spiritual care are shown in Figures 1 and 2. In comparison to those reporting high spiritual support, patients reporting their religious/spiritual needs were poorly supported were less likely to receive a week or more of hospice care and were more likely to die in an ICU, with the impact being greatest among racial/ethnic minorities and high religious coping patients. Furthermore, both racial/ethnic minority and high religious coping patients had higher estimated rates of receiving ICU care in the last week of life when they reported their spiritual needs were poorly supported by the healthcare team.
Figure 1. Adjusted estimates of ICU admissions in the last week of life and of ICU deaths by provision of patient-reported spiritual care from the health care team in the complete sample, racial/ethnic minorities and high religious coping patients (N=303)b.
aSample reduced from 339 due to missing data; findings unchanged when analyses repeated with data imputed to mean values.
bEstimates were adjusted for education, race/ethnicity, baseline existential well-being, baseline social support, advance care planning, end-of-life discussion, health insurance status, patient-physician relationship, degree of positive religious coping, preferences for aggressive care, religiousness, spiritual support from religious communities, Northern versus Southern recruitment site, and terminal illness awareness. Models repeated with cluster analysis by site with findings unchanged.
Figure 2. Adjusted estimates of receiving a week or more of hospice care by patient-reported receipt of spiritual care from the health care team in the complete sample, among non-white race/ethnicity patients and high religious coping patients (N=303)b.
aEstimates were adjusted for education, race/ethnicity, baseline existential well-being, baseline social support, advance care planning, end-of-life discussion, health insurance status, patient-physician relationship, degree of positive religious coping, preferences for aggressive care, religiousness, spiritual support from religious communities, Northern versus Southern recruitment site, and terminal illness awareness. Models repeated with cluster analysis by site with findings unchanged.
bSample reduced from 339 due to missing data; findings unchanged when analysis repeated with data imputed to mean values.
Medical Care Costs in the Last Week of Life
Adjusted estimates of medical care costs in the last week of life according to patient-reported receipt of spiritual care are shown in Figure 3. The estimated difference in EOL care costs was $2441 [95% confidence interval (CI)= $488 to $4394] for patients reporting high support of their spiritual needs by the healthcare team as compared to those reporting receiving less spiritual support, with greater differences seen among racial/ethnic minorities ($4206, 95% CI= $544 to $7869) and high religious coping patients ($4060, 95% CI= $1331 to $6789).
Figure 3. Costs of medical care in the last week of life by patient-reported receipt of spiritual care from the health care team in the total sample and among non-white race/ethnicity and high religious coping patients (N=291)b.
aLeast square mean estimates of costs were adjusted for education, race/ethnicity, baseline existential well-being, baseline social support, advance care planning, end-of-life discussion, health insurance status, patient-physician relationship, degree of positive religious coping, preferences for aggressive care, religiousness, spiritual support from religious communities, Northern versus Southern recruitment site, and terminal illness awareness. Models repeated with cluster analysis by site with findings unchanged.
bSample reduced from 339 due to missing data; findings unchanged when analysis repeated with data imputed to mean values.
DISCUSSION
Spiritual care is a key component of palliative care1 that has previously been shown to improve the well-being of dying patients and facilitate their transitioning to less-aggressive, QOL-focused care at the EOL.10 However, spiritual support from the healthcare team remains infrequent in the care of terminally-ill patients.3 This study demonstrates that advanced cancer patients who report that their religious/spiritual needs are insufficiently supported by the healthcare team have increased medical costs in the final week of life. EOL costs among advanced cancer patients reporting low support of their religious/spiritual needs by the healthcare team were $2441 more on average as compared to those well-supported. Notably, low R/S support among racial/ethnic minority patients and high religious coping patients was associated with greater cost differences in the last week of life, on average $4206 more among minorities and $4060 more among high religious coping patients. These findings are robust considering adjustment for multiple potential confounding factors such as EOL discussions and geographic location. Hence, the frequent absence of spiritual care by the medical team3 – culturally-competent care mandated by national guidelines1 – is associated with decreased well-being of dying patients10, 38 and their families,14 and increased costs due to greater futile, aggressive care at the EOL.
Studies indicate that EOL costs are largely driven by aggressive measures, such as ICU care,15 whereas increased hospice is associated with lower healthcare costs.20 Provision of spiritual care appears to influence costs at the EOL by leading to greater hospice-utilization and facilitating earlier referrals to hospice while decreasing ICU care and deaths, particularly among patients known to be at greater risk for aggressive care – racial/ethnic minorities34, 39, 40 and high religious coping patients.11 R/S has been shown to play a key role in the experience of EOL2, 3 and in EOL decision-making,12 particularly among minorities.34, 39, 40 This study's demonstration that low patient-reported support of their spiritual needs is associated with increased aggressive care among minorities beyond the contribution of religious coping and religiousness, highlights the central role that R/S often plays in the experience of terminal illness among African-American40 and Latino patients.34 Attention to patients' R/S as part of medical care appears to assist terminally-ill patients in avoiding burdensome, aggressive medical care at the EOL. Potential causal mechanisms include facilitating resolution of spiritual needs and distress that would otherwise result in more aggressive and QOL-compromising care. Recognition of patient R/S as part of EOL care may also assist patients in transitioning away from a focus on extending life to a focus on spiritual priorities at the EOL, such as finding spiritual peace – a factor of primary importance to patients facing death7 that is associated with less aggressive care at EOL.41 Involving patients' R/S in medical decision-making may assist patients in recognizing less aggressive EOL care options that remain consistent with their R/S beliefs.
The implications of the provision of spiritual care to dying patients are noteworthy given that it represents higher quality EOL care1, 10 that, despite its presence in national care quality standards,1 frequently remains absent at the EOL.3 The projected economic impact is approximately $1.4 billion ($2441 × 562,340 annual cancer deaths42) for care delivered in the last week of life, or approximately 1.5% of direct cancer costs per year ($1.3 billion of $93.2 billion).42 Furthermore, this study's cost estimates only comprise cancer care in the last week of life; spiritual care could result in greater cost implications if other EOL clinical settings were included and examined over a longer time period. Whereas some hypothesize that ample supply of aggressive technologies creates unnecessary demand,28 our study suggests that medical demand is impacted by medical system engagement of underlying psychosocial issues that mediate EOL decision-making.
This study is limited by the fact that cost calculations were based on estimates present in the literature rather than medical claims data. However, by employing national cost averages that include unaccounted for items such as type of chemotherapy or laboratory costs, these estimates provide a justifiable approximation of the overall impact of spiritual care on US EOL medical care costs. Furthermore, costs calculations solely represent costs to medical payers and do not include costs to patients and their families, such as care-giving costs and lost employment revenue. Another limitation is the unclear content of the spiritual care patients reported receiving from their healthcare team. Data from our prior report assists in characterizing spiritual care, however. First, patients' ratings of support of their R/S needs are significantly associated with receiving pastoral care visits,10 supporting the convergent validity of the spiritual care measure and suggesting that pastoral care is a key aspect of spiritual care. Furthermore, while spiritual care from the healthcare team is associated with less intensive EOL care and reduced costs, receipt of pastoral care visits alone does not predict medical care received at the EOL.10 This finding is consistent with the fact that medical caregivers such as physicians and nurses are the primary health providers assisting patients in medical decision-making, and reinforces the multidisciplinary, collaborative approach to spiritual care outlined in recent guidelines.43 Additionally, patients' ratings of spiritual support from the healthcare team and their associations with EOL outcomes appear distinct from patients' perceptions of their relationships with their providers and of care communication, as the associations of spiritual support with EOL care and costs adjusted for the patient-physician relationship (5-item measure of trust, mutual respect, feeling viewed as a whole person, and comfort asking questions regarding care) and history of an EOL discussion with a physician. Interestingly, in contrast to patients' overwhelmingly positive perceptions of their medical care and care communication,44 a minority (26%) reported high support of their R/S needs by their care providers, further bolstering confidence that patients are identifying spiritual care as absent from their medical care and distinct from other aspects of medical care provision. Future studies are required to describe the specific content of spiritual care from the medical team and its impact on patient and family well-being, medical decision-making, and medical costs.
In conclusion, infrequent spiritual care by the healthcare team is associated with higher medical care costs during the final week of life, particularly among racial/ethnic minorities and high religious coping patients. These findings highlight the importance of spiritual care guidelines1 and of educating healthcare providers in their appropriate role in spiritual care provision.43 The integration of spiritual care into the care of dying patients holds promise to improve patients'10 and bereaved caregivers'14 well-being, while also avoiding healthcare costs due to futile, aggressive care at the EOL.
Acknowledgments
Funding/Support: Supported by Grant No. MHJ63892 from the National Institute of Mental Health and Grant No. CA 106370 from the National Cancer Institute (Prigerson), Fetzer Foundation (Prigerson and Paulk), and ASCO Young Investigator Award (Balboni).
Additional Contributions: We thank Heather Stieglitz, Ph.D, Maureen Clark, and Richard Timms, MD for material, administrative, or technical, support.
REFERENCES
- 1.National Consensus Project for Quality Palliative Care: Clinical practice guidelines for quality palliative care. Second Edition. 2009. [accessed June 28, 2010]. Available from URL: http://www.nationalconsensusproject.org/ [Google Scholar]
- 2.Alcorn SR, Balboni MJ, Prigerson HG, et al. “If God wanted me yesterday, I wouldn't be here today”: religious and spiritual themes in patients' experiences of advanced cancer. J Palliat Med. 2010;13(5):581–8. doi: 10.1089/jpm.2009.0343. [DOI] [PubMed] [Google Scholar]
- 3.Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol. 2007;25(5):555–60. doi: 10.1200/JCO.2006.07.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hui D, de la Cruz M, Thorney S, Parsons HA, Delgado-Guay M, Bruera E. The Frequency and Correlates of Spiritual Distress Among Patients With Advanced Cancer Admitted to an Acute Palliative Care Unit. Am J Hosp Palliat Care. doi: 10.1177/1049909110385917. [DOI] [PubMed] [Google Scholar]
- 5.Moadel A, Morgan C, Fatone A, et al. Seeking meaning and hope: self-reported spiritual and existential needs among an ethnically-diverse cancer patient population. Psychooncology. 1999;8(5):378–85. doi: 10.1002/(sici)1099-1611(199909/10)8:5<378::aid-pon406>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 6.Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8(5):417–28. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 7.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. Jama. 2000;284(19):2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 8.Astrow AB, Wexler A, Texeira K, He MK, Sulmasy DP. Is failure to meet spiritual needs associated with cancer patients' perceptions of quality of care and their satisfaction with care? J Clin Oncol. 2007;25(36):5753–7. doi: 10.1200/JCO.2007.12.4362. [DOI] [PubMed] [Google Scholar]
- 9.Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med. 1999;159(15):1803–6. doi: 10.1001/archinte.159.15.1803. [DOI] [PubMed] [Google Scholar]
- 10.Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010;28(3):445–52. doi: 10.1200/JCO.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phelps AC, Maciejewski PK, Nilsson M, et al. Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. Jama. 2009;301(11):1140–7. doi: 10.1001/jama.2009.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silvestri GA, Knittig S, Zoller JS, Nietert PJ. Importance of faith on medical decisions regarding cancer care. J Clin Oncol. 2003;21(7):1379–82. doi: 10.1200/JCO.2003.08.036. [DOI] [PubMed] [Google Scholar]
- 13.True G, Phipps EJ, Braitman LE, Harralson T, Harris D, Tester W. Treatment preferences and advance care planning at end of life: the role of ethnicity and spiritual coping in cancer patients. Ann Behav Med. 2005;30(2):174–9. doi: 10.1207/s15324796abm3002_10. [DOI] [PubMed] [Google Scholar]
- 14.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Jama. 2008;300(14):1665–73. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169(5):493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56(4):519–43. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 17.Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005;61(4):461–80. doi: 10.1002/jclp.20049. [DOI] [PubMed] [Google Scholar]
- 18.Cohen SR, Mount BM, Bruera E, Provost M, Rowe J, Tong K. Validity of the McGill Quality of Life Questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med. 1997;11(1):3–20. doi: 10.1177/026921639701100102. [DOI] [PubMed] [Google Scholar]
- 19.Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9(3):207–19. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 20.Emanuel EJ, Ash A, Yu W, et al. Managed care, hospice use, site of death, and medical expenditures in the last year of life. Arch Intern Med. 2002;162(15):1722–8. doi: 10.1001/archinte.162.15.1722. [DOI] [PubMed] [Google Scholar]
- 21.Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22(2):315–21. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 22.Rady MY, Johnson DJ. Admission to intensive care unit at the end-of-life: is it an informed decision? Palliat Med. 2004;18(8):705–11. doi: 10.1191/0269216304pm959oa. [DOI] [PubMed] [Google Scholar]
- 23.Archived Consumer Price Index Detailed Report Information. U.S. Bureau of Labor and Statistics; 2010. [accessed April 28, 2010]. http://www.bls.gov/cpi/cpi_dr.htm#2010. [Google Scholar]
- 24.Dasta JF, McLaughlin TP, Mody SH, Piech CT. Crit Care Med. 6. Vol. 33. 2005. Daily cost of an intensive care unit day: the contribution of mechanical ventilation; pp. 1266–71. [DOI] [PubMed] [Google Scholar]
- 25.Milbrandt EB, Kersten A, Rahim MT, et al. Growth of intensive care unit resource use and its estimated cost in Medicare. Crit Care Med. 2008;36(9):2504–10. doi: 10.1097/CCM.0b013e318183ef84. [DOI] [PubMed] [Google Scholar]
- 26.HCUPnet: A tool for identifying, tracking, and analyzing national hospital statistics. U.S. Department of Health and Human Services; [accessed April 28, 2010]. ( http://hcupnet.ahrq.gov/HCUPnet.jsp). Available from URL: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=AF35A093DFBB93CF&Form=SelLAY&JS=Y&Action=%3E%3ENext%3E%3E&_LAY=Researcher. [Google Scholar]
- 27.Center for Medicaid and State Operations Disabled and Elderly Health Programs Group . Correction to Annual Change in Medicaid Hospice Payment Rates. Department of Health and Human Services; Sep, 2009. [Acceessed April 28, 2010]. http://www.cms.hhs.gov/Hospice/downloads/hospicerates10correction.pdf. [Google Scholar]
- 28. [accessed March 1, 2010];The Dartmouth Atlas of Health Care. [Google Scholar]
- 29.Nursing Home Current Residents, Table 38. National Center for Health Statistics; 2008. [Accessed April 28, 2010]. http://www.cdc.gov/nchs/data/nnhsd/Estimates/nnhs/Estimates_Diagnoses_Tabl es.pdf. [Google Scholar]
- 30.Medicare Program . Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities for FY 2010. Department of Health and Human Services Center for Medicaid and Medicare Services; [Accessed April 28, 2010]. http://edocket.access.gpo.gov/2009/pdf/E9-18662.pdf. [Google Scholar]
- 31.Jacobson M, O'Malley AJ, Earle CC, Pakes J, Gaccione P, Newhouse JP. Does reimbursement influence chemotherapy treatment for cancer patients? Health Aff (Millwood) 2006;25(2):437–43. doi: 10.1377/hlthaff.25.2.437. [DOI] [PubMed] [Google Scholar]
- 32.Barnato AE, Chang CC, Saynina O, Garber AM. Influence of race on inpatient treatment intensity at the end of life. J Gen Intern Med. 2007;22(3):338–45. doi: 10.1007/s11606-006-0088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26(25):4131–7. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith AK, Sudore RL, Perez-Stable EJ. Palliative care for Latino patients and their families: whenever we prayed, she wept. Jama. 2009;301(10):1047–57. E1. doi: 10.1001/jama.2009.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cosgriff JA, Pisani M, Bradley EH, O'Leary JR, Fried TR. The association between treatment preferences and trajectories of care at the end-of-life. J Gen Intern Med. 2007;22(11):1566–71. doi: 10.1007/s11606-007-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prigerson HG. Socialization to dying: social determinants of death acknowledgement and treatment among terminally ill geriatric patients. J Health Soc Behav. 1992;33(4):378–95. [PubMed] [Google Scholar]
- 37.Loggers ET, Maciejewski PK, Paulk E, et al. Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol. 2009;27(33):5559–64. doi: 10.1200/JCO.2009.22.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–8. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23(3):267–74. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. Jama. 2000;284(19):2518–21. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 41.Mack JW, Nilsson M, Balboni T, et al. Peace, Equanimity, and Acceptance in the Cancer Experience (PEACE): validation of a scale to assess acceptance and struggle with terminal illness. Cancer. 2008;112(11):2509–17. doi: 10.1002/cncr.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. http://www.cancer.org/downloads/STT/500809web.pdf.
- 43.Puchalski C, Ferrell B, Virani R, et al. Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. J Palliat Med. 2009;12(10):885–904. doi: 10.1089/jpm.2009.0142. [DOI] [PubMed] [Google Scholar]
- 44.Jha AK, Orav EJ, Zheng J, Epstein AM. Patients' perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–31. doi: 10.1056/NEJMsa0804116. [DOI] [PubMed] [Google Scholar]