Abstract
Aims
Cannabis use adversely affects adolescents and interventions that are attractive to adolescents are needed. This trial compared the effects of a brief motivational intervention for cannabis use with a brief educational feedback control and a no-assessment control.
Design
Participants were randomized into one of three treatment conditions: Motivational Enhancement Therapy (MET), Educational Feedback Control (EFC) or Delayed Feedback Control (DFC). Those assigned to MET and EFC were administered a computerized baseline assessment immediately following randomization and completed assessments at the 3- and 12-month follow-up periods. Participants in the DFC condition were not assessed until the 3-month follow-up. Following the completion of treatment sessions, all participants were offered up to 4 optional individual treatment sessions aimed at cessation of cannabis use.
Setting
High schools in Seattle, WA, USA.
Participants
310 self-referred adolescents who smoked cannabis regularly.
Measurements
Main outcome measures included days of cannabis use, associated negative consequences, and engagement in additional treatment.
Findings
At the 3-month follow-up, participants in both the MET and EFC conditions reported significantly fewer days of cannabis use and negative consequences compared to DFC. Frequency of cannabis use was less in MET relative to EFC at 3 months, but did not translate to differences in negative consequences. Reduction in use and problems were sustained at 12-months but there were no differences between MET and EFC interventions. Engagement in additional treatment was minimal and not different by condition.
Conclusions
Brief interventions can attract and have positive impacts on adolescent cannabis users, but the mechanisms of the effects are yet to be identified.
Cannabis continues to be the most prevalent illicit drug used by adolescents and adults in many of the world’s regions. Rates of use among adolescents in the U.S. and Europe suggest cannabis consumption is a common experience among youth. Lifetime cannabis use rates among 15 and 16 year-olds in twelve European countries range from 7 to 44 percent with only three countries reporting rates below 22 percent (Hibell, et al., 2004). Lifetime use among U.S. 10th graders was 36 percent (Johnston et al., 2007). Data from the 2007 national survey of high school students in the U.S. indicate almost one-third of high school seniors (31.7%) used cannabis at least once in 2007, and daily use of cannabis was reported by 5.1% of high school seniors (the respective rates for high school sophomores were 24.6% and 2.8%) (Johnston, O’Malley, Bachman, & Schulenberg, 2008). Rates of use in the past 30 days were 14.2% and 18.8% for high school sophomores and seniors, respectively. Accessibility of cannabis remains high. The majority of seniors (84%) and sophomores (69%) reported having access to cannabis (Johnston, O’Malley, Bachman, & Schulenberg, 2008).
Both the Epidemiological Catchment Area (ECA; Anthony & Helzer, 1991) and the National Comorbidity Study (NCS; Anthony, Warner, & Kessler, 1994) estimate that slightly more than 4% of the population develops a dependency on cannabis - the highest prevalence rate of any illicit drug. Two national surveys conducted in the U.S. 10 years apart indicate the prevalence of DSM-IV abuse and dependence diagnoses has significantly increased despite rates of past year use having remained stable (Compton, Grant, Colliver, Glantz, & Stinson, 2004). Approximately 9% of those who have ever used cannabis meet criteria for a diagnosis of dependence at some time (Anthony et al., 1994), and the risk of dependence may be as high as 20–30% for those who have used cannabis more than a few times (Hall, Solowij, & Lemon, 1994). The risk of experiencing current cannabis dependence, given any smoking in the past year, is estimated to be greater for adolescents (aged 12 – 17 years) than for adults, 14% versus 7% respectively (Kandel, Chen, Warner, Kessler, & Grant, 1997). In addition, it appears that spontaneous remission of cannabis use is somewhat rare among regular adolescent cannabis users (Perkonigg et al, 1999; 2007).
Treatment admissions for cannabis have dramatically increased. Treatment admissions in the U.S. for primary cannabis dependence have increased from 7 percent in 1993 to 16 percent in 2003 (SAMHSA, 2004) and continues to be the most common illicit drug among those seeking substance abuse treatment (SAMHSA, 2008). Although rates vary by country, cannabis was the primary drug of abuse for 20 percent of all treatment cases in European Union countries (EMCDDA, 2009). Although more people are seeking treatment, they remain a minority in comparison to the number of users in the population. For example, it is estimated that there are 4 million cannabis users in the European Union who use daily or almost daily (EMCDDA, 2009). If all 65,000 cannabis treatment admissions were daily users, less than 2 percent of daily users were receiving treatment.
Controlled trials of interventions for adolescent cannabis users have been conducted and a large multi-site study found that a 5-session treatment combining Motivational Enhancement Therapy (MET) and Cognitive Behavioral Treatment (CBT) was as effective in reducing use and associated problems as longer family and systems-based interventions (Dennis, Godley, et al., 2004). However, the typical participant in this and other treatment trials focused on adolescent cannabis use has been coerced into treatment by parents, schools, or the legal system. The majority of adolescents in need of treatment do not self-refer and are not involved in treatment (Diamond, Leckrone, Dennis, & Godley, 2006; Titus, et al., 1999). A handful of studies have evaluated brief, MI-based interventions with adolescents who were not presenting to treatment. McCambridge and Strang (2004) recruited 200 weekly cannabis or stimulant users, ages 16 to 20, at postcompulsory colleges in the UK. Students were randomized to receive a one-session motivational interviewing (MI) session or assessment only control condition. Students who received MI reduced their use of cannabis, alcohol and cigarettes more than students in the control condition at a 3-month follow-up. A follow-up effectiveness study including 162 youth aged 16 to 18 failed to replicate a reduction in cannabis use (Gray, McCambridge, & Strang, 2005). However, the study was quasi-experimental and eligibility criteria were not limited to cannabis use, but instead included those who were smoking cigarettes daily, drinking alcohol weekly or using cannabis.
The Teen Marijuana Check-Up (TMCU), a motivational enhancement therapy (MET) intervention adapted from the Drinker’s Check-Up (Miller & Sovereign, 1989), is aimed at eliciting voluntary participation from cannabis using adolescents (Swan, et al., 2008). Two pre-post design pilot studies have evaluated the acceptability (Berghuis, et al., 2006; Martin, Copeland, & Swift, 2005) of this model in the United States and Australia. Both demonstrated that non-treatment seeking adolescents could be attracted to voluntarily participate in the TMCU and reductions in cannabis use were evident. A randomized clinical trial involving 97 high school students who used cannabis regularly was conducted to determine if the MET intervention could produce reductions in cannabis use greater than an assessment control condition (Walker, Roffman, Stephens, Berghuis, & Kim, 2006). Both conditions reported lower cannabis use at a 3-month follow-up assessment and the lack of differential effect between conditions raised questions about whether the pre-intervention assessment was sufficient to account for the behavior change. The assessment package in the study was carefully constructed to include questions involving both the positive and negative aspects of cannabis use, and the assessment in some respects was similar to a writing exercise to explore the pros and cons of cannabis use – a potential active ingredient in MI (LaBrie, Pedersen, Earleywine, & Olsen; 2006). Martin and Copeland (2008) found similar results with an Australian sample recruited from the general community. Both studies lacked a comparison condition to control for therapist contact and other nonspecific factors that may have contributed to outcomes. Due to the relatively short periods of follow-up in these studies (3 and 6 months), less is known about the durability of a MET intervention’s effect.
The present study was designed to extend this line of research by addressing several of the limitations in the prior trials. In a three group randomized clinical trial, brief MET was compared with an educational feedback control group that spent equivalent time with a counselor reviewing various effects of cannabis. A no-assessment delayed feedback group was also included to provide a control for assessment effects. Finally, we made additional cognitive-behavioral treatment available within the high schools in order to decrease barriers to treatment-seeking that may occur as a result of the interventions. In particular, we reasoned that if the MET intervention were successful in increasing motivation for change, then a subset of participants might be inclined to seek additional intervention that would augment the impact of the check-up. The main hypotheses were: 1) reductions in cannabis use and related consequences would be greater among MET participants than education or delayed feedback participants; 2) more MET participants would attend the additional cognitive behavioral treatment than participants in the educational condition; and 3) attendance of additional treatment would partially mediate the effect of MET on cannabis use and related outcomes.
Method
Participants
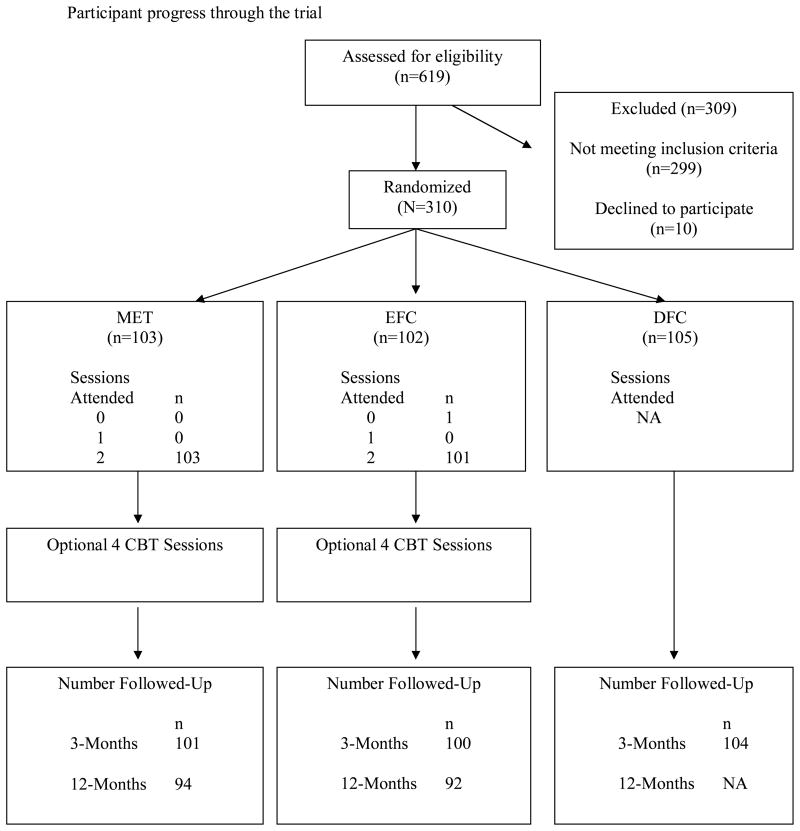
A target sample size of 300 was predicated on the goal of detecting a potential interaction between treatment condition and stage of change at the 3-month follow-up with an eta-squared effect size of .045 with power of .80 and assuming up to 10% attrition (Erdfelder, Faul, & Buchner, 1996). Inclusion criteria were: 1) age (14–19 years old), 2) grade level (9th through 12th) and 3) cannabis use (smoked 9 or more days in past 30). Individuals were excluded if they: 1) were not fluent in English, 2) had a thought disorder that precluded full participation, or 3) refused to accept randomization to condition. Of the 619 screened participants, 299 were ineligible (48.3%). The majority (98%) of ineligible participants had not used cannabis on at least 9 days in the past month. Of the 320 eligible for the study, all but 10 chose to participate (96.9%, See Figure 1). The 310 participants randomly assigned to treatment conditions averaged 16.0 years of age (SD = 1.24). Participants were mostly male (N = 188, 60.6%) and Caucasian (N = 203, 65.5%) with 10% African American, 13% multiracial, 3% Asian and Pacific Islander, and 5% other. Four percent of eligible participants were Hispanic or Latino. Approximately 52% (N = 161) of participants were in the 9th or 10th grades and 48% (N = 149) were in the 11th or 12th grades. Based on a stage of change algorithm completed at screening, 39% of the sample were in the precontemplation stage, 30% were in the contemplation stage, and 31% were in the preparation, action, or maintenance stages.
Figure 1.
Participant progress through the trial
Design
Participants were recruited from six local high schools in the Seattle, Washington school district with schools contributing 76, 72, 69, 42, 36, and 15 students to the final sample, respectively. Following screening and informed consent, participants were randomized to one of three treatment conditions: Motivational Enhancement Therapy (MET; n = 103), Educational Feedback Control (EFC; n = 102) or Delayed Feedback Control (DFC; n = 105). Randomization to condition was accomplished following stratification on stage of change (SOC: Precontemplation vs. Contemplation vs. Preparation/Action/Maintenance) and grade level (9th/10th vs 11th/12th) using tables of randomly permuted blocks. Randomization tables were constructed separately for each of the six high schools. Follow-up assessments were conducted at 3 and 12 months after the baseline assessment. Those assigned to MET and EFC completed baseline assessments immediately following randomization, whereas those randomized to DFC were not assessed further until the 3-month follow-up. Upon completion of the 3-month follow-up, participants in the DFC condition were offered their choice of the two active treatment conditions, but were not followed thereafter.
Recruitment and Screening Procedures
All procedures were approved by the University of Washington IRB. Participants were recruited through educational guest presentations delivered by project staff in high school classes, lunchtime recruitment tables, the distribution of flyers in the schools, and referrals from school staff. Presentations included discussion activities with students about common reasons that teens choose to smoke marijuana, brief overviews of some of the effects of marijuana on health and behavior, and finally a description of the study. Project publicity and presentations emphasized that the TMCU was a free, nonjudgmental, and confidential service for teens who would like information on their use of cannabis. It was emphasized that the TMCU was not a treatment program and that whether participants changed their cannabis use would be up to them. Recruitment occurred across three school years (2004–2005–2005–2006, and 2006–2007) and was timed such that each participant’s 3-month follow-up assessment was completed in the same school year as his/her recruitment. This also ensured that the 12-month follow-up assessment did not occur during the summer break.
In total, 349 classroom presentations were made during the recruitment period reaching approximately 7,148 students. At the conclusion of each presentation, all students in the class were asked to complete an anonymous questionnaire evaluating the content and process of the presentation. Students were told to sign their names on the evaluation questionnaire only if they were interested in participating. All questionnaires were collected directly by project staff and interested students were subsequently called out of class and administered a brief screening interview to determine eligibility. Procedures were developed at each school to ensure that the reason for being called out of class was unknown to classmates and school staff.
A total of 619 students completed the screening interview and most were self-referred following a classroom presentation (n = 231; 37%) or having discussed the study with a project staff member at a lunch time informational table (n=212; 34%). Other sources of referral were friends (n = 117; 19%), school staff (n = 35; 6%), and project advertisements (n = 28; 3%). All ineligible applicants were offered a single MET or EFC session and behavior change resources if they indicated interest. Eligible participants reviewed a consent form that explained all requirements of participation. Note that the need for parental consent was waived by the IRB based on the fact that adolescents in the state of Washington may legally seek treatment for substance abuse without parental consent. Once the consent form was signed the staff member called the research office, provided the blocking information, and then received the condition assignment. Those participants assigned to the MET and EFC conditions were told they would be called out of class in the next week to complete an initial assessment and begin the check-up. Those assigned to DFC were told they would be contacted in 3 months to complete the assessment and receive the check-up.
Assessment and Measures
Measures were administered by an Audio-Computer-Assisted Self-Interviewing (A-CASI) program at baseline and follow-ups. Computer-assisted technology has been demonstrated to be valid in assessing a variety of potentially sensitive behaviors in adolescents and adults (e.g., Davis, Hoffman, Morse, & Luehr, 1992; Webb, Zimet, Fortenberry, & Blythe, 1999; Turner, et al., 1998; McElrath, 1994; Erdman, Klein, & Greist, 1983).
Cannabis, alcohol, and drug use
Assessment of cannabis, alcohol and other drug use was based on 31 substance use questions taken from the GAIN-I (Global Appraisal of Individual Needs-I). The GAIN is a comprehensive, standardized bio-psycho-social assessment battery (Dennis, Titus, White, Unsicker, & Hodgkins, 2003; Dennis, 1999) used in the Cannabis Youth Treatment (CYT) project (Center for Substance Abuse Treatment, 2000a; Dennis, Titus, et al., 2002). Studies with both adults and adolescents have found this measure to have good reliability and validity (Dennis, Funk, Godley, Godley, & Waldron, 2004; Dennis, 1998). The 90-day assessment time frame utilized by the GAIN was modified in this study. Participants were asked to report the number of days using cannabis, alcohol, and other drugs over the past 60 days. They also reported on other quantity and frequency indices of use (most joints smoked in one day, typical times of day when cannabis is used, etc.). The primary dependent measure for cannabis use was the number of days cannabis was used in the 60 days prior to assessment.
Cannabis related consequences
Symptoms of cannabis abuse and dependence as described in DSM-IV were assessed through 17 items from the GAIN-I. Each symptom for DSM-IV abuse and dependence was converted into one or more questions to assess the presence of the symptom (e.g., withdrawal was assessed with two questions, with the first question focusing on the presence of any withdrawal symptoms and the second question focusing on any use to stop or avoid withdrawal symptoms). Participants were scored as having met a criterion if they positively endorsed any question assessing that criterion. The total numbers of abuse and dependence critieria met were computed separately. The Marijuana Problem Inventory (MPI; Johnson & White, 1989), a 23-item self-report questionnaire adapted from the Rutgers Alcohol Problem Index (RAPI; White and Labouvie, 1989) assessed the degree to which individuals experienced problem behaviors associated with cannabis use over the past 60 days. Items were rated on a 5-point scale (1 = never, 5 = more than 10 times) and the scale total score was calculated by adding the item scores. Cronbach’s alpha for the MPI ranged from .82 to .88 across time points.
Other treatment
Utilization of other treatment was assessed with items from the GAIN-I that assess recent inpatient, outpatient, and 12-step group treatment experiences related to cannabis, alcohol, other drugs, and emotional/psychological problems.
Additional items assessed cannabis use motives, self-efficacy for change, internalizing and externalizing behavior problems, life goals, and environmental risk factors but are not discussed further in this paper. Several of these measures were included in the assessment battery solely to generate feedback in the Personalized Feedback Report.
Intervention Conditions
The MET and EFC conditions each consisted of two 45–50 minute sessions scheduled approximately one and two weeks after the baseline assessment.
MET
The goal of the first session was to elicit the teen’s story of cannabis use, and to evoke motivation for change by eliciting reasons for using, reasons for abstaining, concerns they may have about their use and how they see cannabis fitting into their life currently and over the long-term. MI skills and techniques were utilized throughout. First, counselors would use open questions and reflective listening to develop rapport and gain an understanding of how cannabis fit into the teen’s life. Next, motivation and change talk were probed for, often utilizing a pros/cons of using exercise. Counselors would seek to develop discrepancy, typically asking the teen how they saw cannabis fitting into their future. Self-efficacy was explored and reinforced by the counselor. The session often ended with a summary of the discussion and a key question such as “What are you thinking at this point about your cannabis use?”
In the second session of the MET condition, the counselor introduced the personal feedback report (PFR), summarizing the individual sections to be discussed, and how the time together would be spent. The PFR was constructed from data collected in the baseline assessment and was comprised of the following sections: history of cannabis use; recent use patterns of cannabis, alcohol, and other drugs; normative data on cannabis; problems related to cannabis use; potential costs and benefits of reducing cannabis use; situational confidence in avoiding cannabis; and life goals. The PFR was printed in booklet format with graphics and accompanying descriptions of risk factors for developing problems with cannabis. The PFR and an accompanying “Understanding Your PFR” booklet were given to the teen and reviewed in the feedback session with the counselor utilizing motivational interviewing skills throughout.
EFC
The EFC condition involved two sessions with a counselor delivering a PowerPoint presentation on current research and facts about cannabis. This condition was highly structured and didactic, with the counselors avoiding MET techniques throughout. The first session began by eliciting questions the teen had about cannabis and orienting the teen to the educational nature of the intervention. PowerPoint sections on Cannabis Basics, Cannabis and the Brain, and Cannabis and the Lungs were then reviewed. The second session reviewed the following PowerPoint presentations: Sex and Pregnancy, Cannabis and Driving, and The Heart. If time permitted in either session, the participant chose additional content areas from the following topics to review: The Legalization Debate, Cannabis and the World, Legal Issues, and Cannabis and Medicine.
Cognitive-Behavioral Treatment
At the conclusion of session two for EFC and MET, all participants were informed that additional sessions were available for those who wanted help in stopping their cannabis use. The four optional 50-minute CBT sessions were delivered in an individual format. The Cannabis Youth Treatment study manual entitled “Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users: 5 Sessions” (Sampl & Kadden, 2001) was adapted such that the first CBT session was devoted to gaining rapport, setting treatment goals and reviewing a functional analysis of cannabis use. The second session focused on cannabis refusal skills. The third session emphasized strategies for enhancing the teen’s social support network and increasing pleasant activities. The final session was devoted to planning for emergencies and coping with relapse or set backs. Practice exercises and role-plays were used throughout each session to model particular skills. CBT sessions were delivered by a counselor different from the counselor who performed the MET or EFC sessions.
Counselor Training and Adherence
The interventions were delivered by bachelor’s and master’s level counselors. Consistent with the Check-up philosophy of the clinical interaction having “no pressure to change,” counselors in this project were referred to as health educators. A total of 10 counselors were trained by the first and third authors, two experienced MET/CBT therapists. Due to the duration of the trial, some staff turnover occurred and additional counselors were hired and trained to maintain a staff of three to five at all times. Each new counselor went through the same training procedures. Counselors first studied background readings on cannabis, motivational interviewing, and the specific intervention protocol manuals. In a series of weekly meetings, the trainers presented the intervention protocols and conducted role-play exercises with the counselors to develop skills in delivering the MET and EFC interventions. Once counselors were competent to administer the interventions, each counselor practiced the interventions with pilot participants and received feedback from the trainers who reviewed audiotapes of the intervention sessions. During the trial, counselors continued to meet as a group with the trainers on a weekly basis to review audiotapes, reinforce intervention skills, and discuss difficult cases in order to maintain adherence to the protocol. Audio tapes of both interventions were randomly reviewed throughout the duration of the study. These tapes were coded for adherence to the protocol and written feedback was provided to the counselors. If a counselor drifted too far from the protocol, individual meetings were held with the training staff to re-orient the counselor to the interventions and discuss any other problems that may have been occurring.
Tapes of the intervention sessions were coded by four research assistants trained to use the Motivational Interviewing Treatment Integrity coding system version 3.0 (MITI; Moyers, Martin, Manuel, Miller, & Ernst, 2007) to determine adherence to MET techniques and guidelines. Audiotapes of feedback sessions from 60 participants (30%) in the MET (n=40) and EFC (n=20) conditions were sampled such that equal numbers of first and second feedback sessions were coded within each condition. Intraclass correlations showed good to excellent agreement between raters with the exception of the frequency of MI Nonadherent counselor behavior (e.g., confrontation), which was suppressed due to very low frequency of these behaviors in either condition. Global ratings on a 5-point scale averaged from 4.30 to 4.85 for MET tapes for MITI scales assessing counselor empathy, evocation, direction, collaboration, and autonomy. Scale scores differed dramatically and significantly (ps <.001) from the corresponding ratings for the EFC condition (means ranged from 1.18 to 2.73). Similarly, all MITI behavior counts of MET-consistent behaviors differed significantly in the intended directions. These data indicated that MET was delivered with a high degree of fidelity and skill and that treatment conditions differed as intended.
Counselors received a similar training protocol for conducting the optional CBT sessions. Following a review of the treatment manual (http://www.kap.samhsa.gov/products/manuals/cyt/pdfs/cyt1.pdf), counselors role-played the various intervention sessions and then received feedback on their performances with pilot participants. Tape-reviews of sessions with participants were followed by supervisory feedback throughout the trial. However, there was no attempt to code therapist behavior during CBT sessions.
Follow-up Procedures
Follow-up assessments were scheduled 3-months and 12-months after the baseline assessment. Students were called out of class to complete the A-CASI-based assessments. For participants who were not available to complete the 12-month assessment in person (e.g., graduated seniors, dropouts, no longer in area, etc.), an internet-based assessment that directly mimicked the A-CASI program without audio assistance was created. In total, 14 participants were offered the assessment online and 12 completed it. Participants received gift cards following the two feedback sessions ($15), and at completion of the 3-month ($20) and 12-month ($40) follow-up assessments.
Results
Preliminary Analyses
At baseline assessment, the average participant had used cannabis on 39 of the past 60 days, reported more than three of the seven DSM IV dependence symptoms, and reported one of the four DSM IV abuse symptoms. Alcohol and other illicit drug use were less frequent. Approximately 13% of the sample had participated in cannabis treatment in the past. No significant differences were detected between conditions in demographics, baseline cannabis use, or SOC characteristics, suggesting that the randomization scheme was largely effective (see Table 1). However, there was a significant difference between groups on gender of participants (χ2 (2, n = 310) = 9.33, p < .01), such that there was a higher proportion of females in the DFC group (N = 53, 50.5%) as compared to MET (N = 31, 30.1%) and EFC (N = 38, 37.3%). Gender, therefore, was a covariate in all outcome analyses. There also was a significant difference between the MET and EFC conditions in days of other drug use reported at baseline, with MET participants reporting other drug use on about 3 out of the past 60 days and EFC participants reporting an average of 6 days of other drug use (F (1, 201) = 5.40, p < .05). Note that DFC participants were not assessed at baseline and other drug use for these participants was undetermined. Therefore, frequency of other drug use was a covariate in those analyses comparing only the MET and EFC conditions.
Table 1.
Baseline characteristics across conditions
| Variable | MET N = 103 |
EFC N = 102 |
DFC N = 105 |
Total Available | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Screening MJ Use (Days in Past 30 Days) | 19.74a | 6.71 | 19.74a | 7.22 | 19.09a | 7.28 | 19.52 | 7.06 |
| Age | 15.95a | 1.24 | 16.04a | 1.23 | 15.93a | 1.26 | 15.97 | 1.24 |
| Age of First MJ Use | 12.90a | 1.80 | 13.22a | 1.50 | N/A | N/A | 13.06 | 1.66 |
| Baseline MJ Use (Days in Past 60 Days) | 40.23a | 14.28 | 37.69a | 16.06 | N/A | N/A | 38.97 | 15.21 |
| Baseline MJ Dependence Symptoms | 3.37a | 2.07 | 3.45a | 2.11 | N/A | N/A | 3.41 | 2.09 |
| Baseline MJ Abuse Symptoms | 1.38a | 1.16 | 1.60a | 1.12 | N/A | N/A | 1.49 | 1.15 |
| Used MJ Before/During School* | 2.31a | 1.31 | 2.39a | 1.33 | N/A | N/A | 2.35 | 1.32 |
| Baseline Alcohol Use (Days in Past 60) | 10.17a | 10.50 | 10.98a | 11.44 | N/A | N/A | 10.58 | 10.96 |
| Baseline Other Drug Use (Days in Past 60) | 2.87a | 5.50 | 6.08b | 12.79 | N/A | N/A | 4.47 | 9.93 |
0=Never; 1=Less than 1 day per week; 2=One day per week; 3= 2–4 days per week; 4=5 days per week
Note. Values within a row that do not share the same superscript differ significantly at p < .05.
Follow-up rates were 98% at the 3-month follow-up and 91 % at the 12-month follow-up with no evidence of differences in attrition across treatment condition. Further, those lost to follow-up did not differ significantly on baseline variables. Transformations were used to improve the distributions of some variables, but results were the same as with the raw data. Hence the raw data results are presented below. All outcome analyses were conducted on an intent-to-treat basis with missing values replaced using a multiple expected maximization procedure.
Intervention Attendance and Perceptions
Feedback session completion rates were very high in both conditions, with 100% of MET participants and 99% of EFC participants completing both sessions. Contrary to predictions, the proportion of participants attending CBT sessions did not differ by condition (x2 (1, n = 205) = 0.408, p > .05), with 12.6% (N = 13) of MET participants and 9.8% (N = 10) of EFC participants attending at least one session. Similarly, there were no differences in the average number of CBT sessions attended by condition, either for the whole sample (F (1, 203) = 0.57, p > .05) or among those who attended any CBT sessions (MET = 3.23 of the 4 possible sessions; EFC = 3.00 sessions).
Questionnaires completed by participants following each feedback session showed that they felt listened to (98%), liked (81%), appreciated (92%), respected (96%), understood (89%), comfortable with the counselor (83%), and cared about (74%). Participants agreed that the counselors were not judgmental (94%) and did not use persuasion (93%). Participants reported being satisfied with their session (92%) and with the counselor (95%). Notably, there were no differences in these ratings by condition, with the exception that those in the EFC were more likely to endorse the usefulness of free information about cannabis. Overall, these data indicate the participants felt the sessions were a positive experience and that the EFC condition controlled for nonspecific therapeutic factors.
3-Month Outcomes
Table 2 shows cannabis use and cannabis-related problems across the baseline and follow-up assessments. For 3-month outcome analyses involving comparisons with the DFC condition, 3 (Condition: MET vs. EFC vs. DFC) × 3 (Stage of Change: Precontemplation vs. Contemplation vs. Preparation/Action/Maintenance) between-subjects general linear model analyses were conducted. Frequency of cannabis use reported during screening and gender were included as covariates. Results for the number of days of cannabis use in the past 60 days included a significant main effect for condition, F(2, 298) = 6.62, p < .01, eta-squared = .04. Participants in both the MET (p < .001) and EFC (p < .05) conditions reported significantly fewer days of cannabis use compared to DFC. However, frequency of cannabis use did not differ significantly between the MET and EFC conditions (p > .05).
Table 2.
Cannabis use and related problems during the past 60 days
| Treatment Condition | Assessment
|
|||||
|---|---|---|---|---|---|---|
| Baseline
|
3 months
|
12 months
|
||||
| M | SD | M | SD | M | SD | |
| Days of Cannabis Use | ||||||
| MET | 40.23a | 14.28 | 31.80a | 19.67 | 33.71a | 22.27 |
| EFC | 37.69a | 16.06 | 34.53ab | 19.78 | 34.24a | 21.08 |
| DFC | - | - | 37.46b | 18.99 | - | - |
|
| ||||||
| Number of Dependence Symptoms | ||||||
| MET | 3.37a | 2.07 | 2.70a | 2.01 | 2.74a | 1.99 |
| EFC | 3.45a | 2.09 | 3.02a | 2.00 | 2.92a | 2.11 |
| DFC | - | - | 3.77b | 1.95 | - | - |
|
| ||||||
| Number of Abuse Symptoms | ||||||
| MET | 1.38a | 1.16 | 1.05a | 1.04 | 1.10a | 0.95 |
| EFC | 1.59a | 1.11 | 1.30ab | 1.04 | 1.14a | 1.03 |
| DFC | - | - | 1.52b | 1.07 | - | - |
|
| ||||||
| Number of Cannabis Problems | ||||||
| MET | 18.47a | 13.47 | 14.68a | 10.39 | 13.08a | 10.35 |
| EFC | 19.13a | 12.31 | 14.24a | 10.18 | 14.14a | 10.32 |
| DFC | - | - | 21.58b | 12.95 | - | - |
Note. Values within an assessment point that do not share a superscript differ significantly at p < .05.
We also conducted 2 (Condition) × 3 (SOC) × 2 (Time: Baseline vs. 3-month) mixed-model analyses using only the MET and EFC conditions, because DFC participants did not complete the baseline assessment and we could not covary for baseline differences in other drug use in the preceding analysis. With baseline frequency of other drug use and gender included as covariates, a significant main effect of time, F (1,197) = 9.89, p < .01, eta-squared = .05, was qualified by a significant interaction effect of time by condition, F(1, 196) = 5.74, p < .05, eta-squared = .03, indicating that participants in MET showed a significantly larger reduction in cannabis use compared to EFC participants. In addition, there was a main effect of SOC, F (2,196) = 4.71, p < .01, eta-squared = .05. Participants in the Precontemplation and Contemplation stages reported more days of cannabis use (M = 38.02 and M = 38.30, respectively) than participants in the Preparation/Action/Maintenance stages (M = 31.31). These findings confirm that differences in baseline levels of other drug use were not a significant factor in the previous 3-condition analyses and, in fact, show greater reductions in cannabis use in MET relative to EFC when other drug use was controlled.
We repeated these same analyses for self-reported cannabis problems and dependence and abuse symptoms at the 3-month follow-up. In the 3-group between-subjects analyses there were significant main effects of condition on cannabis problems (F(2, 299) = 13.17, p < .001), dependence (F(2, 299) = 7.78, p < .001), and abuse (F(2, 299) = 4.86, p < .01) symptoms. As indicated in Table 2, pair-wise tests showed that MET participants reported significantly fewer problems, abuse, and dependence criteria relative to the DFC condition at 3 months (ps < .05). The EFC condition typically fell between the MET and DFC conditions on each measure and did not differ significantly from MET. EFC participants reported significantly fewer dependence symptoms and cannabis problems relative to DFC. Similarly, when we conducted the repeated measures models comparing baseline and 3-month indices of cannabis-related consequences in the MET and EFC conditions controlling for baseline other drug use and gender, we found significant effects of time for problems (F(1,197) = 8.97, p < .01), abuse symptoms (F(1,197 = 6.71, p < .01) and dependence symptoms (F(1,197) = 3.43, p = .06), but no significant condition by time interactions indicative of differential change in the two intervention conditions. For dependence symptoms and cannabis problems, main effects of SOC and interactions of SOC and time were significant. Although dependence symptoms and problems decreased in all groups, larger reductions in these negative consequences were seen in those participants categorized in the Preparation/Action/Maintenance stage of change relative to those in Precontemplation or Contemplation categories.
12-Month Outcomes
To examine the longer term effects of the interventions, 2 (Condition: MET vs. EFC) × 3 (SOC) × 3 (Time: Baseline, 3-months, 12-months) general linear model analyses were performed covarying for baseline levels of other drug use and gender. On the number of days of cannabis use in the past 60 days, there were significant main effects of time, F(2, 197) = 6.11, p < .01, eta-squared = .06, and SOC, F(2, 197) = 5.79, p < .01, eta-squared = .06. The condition by time interaction did not reach significance (F(2, 196 = 2.85, p = .06) and there were no other significant interaction effects. Baseline cannabis use decreased at 3-months and remained reduced at 12-months, but there was no significant difference by condition in the overall analysis (see Table 2). Participants in the Precontemplation (M = 37.80) and Contemplation (M = 37.45) stages of change reported more use than participants in the Preparation/Action/Maintenance stages (M = 30.13) across assessments.
Analyses of related negative consequences across all three assessments showed significant time effects for abuse symptoms (F(2,196) = 5.26, p < .01) and cannabis problem totals (F(2,196) = 4.53, p < .05). Significant reductions in these indices at the 3-month follow-up remained reduced at 12-months. The time effect in the overall analyses was not significant for dependence symptoms, but significant SOC by time interactions for dependence symptoms and cannabis problems again showed that the greatest reductions in these indices were for those in the Preparation/Action/Maintenance category.
Abstinence Rates
Complete point-prevalence abstinence for the 60 day period assessed at each follow-up was a fairly rare occurrence and did not differ significantly by condition. At 3 months, abstinence rates were 4% (MET), 2% (EFC), and 1% (DFC), χ2= 2.09, p > .05. At 12 months, abstinence rates were 12% (MET) and 5% (EFC), χ2 = 3.07, p > .05.
Mediational Hypothesis
The lack of differences between groups in CBT attendance precluded true meditational analyses, but the relationship between CBT attendance and frequency of cannabis use was explored. Partial correlations, controlling for baseline cannabis use, showed that CBT session attendance was associated with reduced cannabis use at 3-months (r = −.14, p < .05) and 12-months (r = −.18, p < .05).
Alcohol and Other Drug Use
Although not targeted by the interventions, we explored change in the frequency of alcohol and other drug use. There was no significant change in either behavior related to condition at either the 3- or 12-month follow-ups.
Discussion
The current study extends the existing research on intervening with adolescents who use cannabis. The TMCU was successful in attracting a large voluntary sample of cannabis using teens, many of whom were experiencing abuse and dependence symptoms and whose level of use was similar to those described among treatment populations (e.g., Dennis, et al., 2004). However, there was only partial support for the hypothesis that a brief MET intervention would have greater effects on reducing cannabis use in this population than an educational control condition, and what support there was disappeared by the 12-month follow-up. Both MET and EFC interventions were associated with significant reductions in cannabis use relative to a no-assessment, delayed intervention condition and these reductions appeared to be maintained at the 12-month follow-up. The reductions in cannabis use were accompanied by changes in associated negative consequences indicating that the interventions had a meaningful impact. Overall, there was little engagement with additional CBT sessions designed to augment the effect of the brief interventions, suggesting that future research with this model will need to find ways to strengthen its impact.
At the 3-month follow-up, both MET and EFC reduced cannabis compared with the no assessment, delayed intervention condition. There was some evidence of greater reductions in cannabis use in the MET group compared to EFC, but the differences were not great enough to be statistically significant in the less powerful between-subjects analyses. Similarly, on indices of negative consequences associated with cannabis use at 3-months, both MET and EFC tended to produce greater reductions than the delayed intervention condition and did not differ from each other. Further, there was no evidence that stage of change as measured by a simple algorithm interacted with treatment condition. There were predictable differences in the extent of cannabis use as a function of stage of change, with those who entered the project already preparing to change making the greatest reductions in indices of negative consequences. Although others have challenged the utility of the stage of change concept on both conceptual and empirical grounds (e.g., West, 2005), we might have expected those in the contemplation stage to have benefited most from the MET intervention. The failure to find such an effect adds to a growing literature of largely null results regarding stage of change and treatment matching.
At 12-months the reductions in cannabis use and related problems produced by both interventions were maintained, but there was no evidence of greater long-term change in the MET group. These findings are encouraging in that apparently meaningful reductions in cannabis use resulting from brief interventions were sustained over a relatively lengthy period of time. Greater effects may have been achieved had we been able to repeatedly interact with participants over time, especially in cases where participants had been unsuccessful in reducing use on their own or had experienced additional negative consequences of use.
There was limited use of the CBT sessions overall and no differences were found by treatment condition. This absence of differences was contrary to our predictions that the MET condition would foster more interest in treatment and consequently even greater change in cannabis use. The CBT sessions were presented as being for those who wanted to quit using cannabis, which may have created too large of a hurdle for these relatively ambivalent teen users. Describing additional treatment sessions as focused on ways of “reducing” marijuana use may make them more appealing. Further, the CBT sessions were offered only once, at the end of the second feedback session raising the question of whether repeated prompting would have allowed those who did not immediately see the need to change their minds later. It is also possible that the CBT acceptance rates were inflated in the EFC condition due to the lack of opportunity to talk about their own cannabis use in the initial didactic information sessions. Nevertheless, the absence of an effect on CBT involvement precluded exploration of a mediating effect of CBT on reductions in cannabis use. The small, but significant relationship between CBT attendance and subsequent reductions in cannabis use, argues for further research on in-school treatment availability.
There was evidence that the EFC condition had an effect on cannabis use at 3-months relative to the DFC condition, but the design did not allow us to know whether this effect was attributable to the baseline assessment received by EFC participants or the educational component of the intervention. The EFC condition was designed largely as an attentional control and ratings of sessions by independent coders clearly showed the intended differences in the types of interactions that occurred between the counselors and students. At the same time, student perceptions of the EFC counselors were positive and highly similar to those of the MET condition on measures of mutual respect, usefulness of the session, and the lack of coercion. Either these nonspecific treatment factors or the baseline assessment, therefore, may account for the similar findings. However, these findings, in conjunction with our earlier trial (Walker et al., 2006) that showed no significant differences in cannabis use between a MET condition and a delayed control that received a baseline assessment, add to a growing literature suggesting that assessment may be a significant contributor to the effects of brief interventions on substance use (Kypri, Langley, Saunders, & Cashell-Smith, 2006). Understanding assessment effects may be particularly important for work in school settings. For example, a computerized assessment as used in this study, could be an inexpensive intervention requiring little additional training of personnel. Future research should continue to explore the role assessment may play in promoting behavior change.
The lack of strong and consistent effects for MET as compared to an alternative brief intervention in this study requires comment. This is one of the only cannabis studies that has compared MET to a comparison brief intervention matched for dose and attention. Previous findings on MET with cannabis using youth have suggested MET may be superior to providing assessment only (McCambridge & Strang, 2004), but that study did not include a comparison brief intervention. Our findings suggest that MET may provide only a small increment in effect above and beyond another brief intervention (EFC). Given the time and expense required to train counselors adequately in MET, other brief feedback interventions may be more cost-effective and should be explored in future research.
A few limitations of this trial are noted. Biological validation of self-reported drug use was not used. The collection of urine in the schools while maintaining the confidentiality of participants would have been logistically difficult and was thought to be a barrier for a teen to participate in the TMCU. Given that self-reports of adolescent drug users have been found to be reliable and valid with similar assessment procedures (Lennox, Dennis, Ives, & White, 2006; Modisette, Hunter, Ives, Funk, & Dennis, 2009) and urine assays for cannabis metabolites are of limited utility when complete abstinence is not the outcome to be verified, we opted to exclude this from our assessment battery. We attempted to remove motives for misreporting of drug use through rapport building, a nonjudgmental attitude, emphasizing confidentiality, dissociating self-reports from project staff through the use of the A-CASI assessments, and assigning different counselors to prompt for follow-ups than conducted the participant’s feedback and CBT sessions. The reporting of frequent use by teens in this trial suggests that pressures to underreport were minimized. The provision of gift certificate incentives for completion of MET and EFC sessions may also be viewed as a limitation by artificially inflating interest in the TMCU. The answer to this question awaits additional research that does not include incentives for participation, but we note that the use of incentives is consistent with recent contingency management programs that support the utility of incentives for increasing treatment participation (Carroll et al., 2006; Sinha, et al, 2003). It may be that incentives are needed to reach certain populations and involve them in treatment and it may be cost-effective in the long run.
Taken as a whole, these results provide continued support for “check-up” models to promote voluntary participation of heavy cannabis using adolescents in schools in brief interventions designed to reduce use. However, contrary to the hypotheses, the findings largely did not clearly support the use of MET over an alternative brief intervention and utilization of additional treatment was minimal. Future research should address ways of augmenting the impact of these brief interventions, perhaps by including repeated check-ups over time.
Acknowledgments
This work was supported by a grant from the National Institute on Drug Abuse (RO1DA014296). We also wish to thank the participants who generously shared their experiences with us and to Allison O’Rourke, Gretchen Davis, Teryl Neil, Carolyn Speidel, Jennifer Katz, Jennifer McCormick, McKenzie Winters, Megan Holz, and Jennifer Higgins for their thoughtful and caring work on this project.
This research was supported by NIDA RO1DA014296. The authors have no conflicts of interest.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
Contributor Information
Denise D. Walker, Email: ddwalker@u.washington.edu, School of Social Work, University of Washington, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020
Robert Stephens, Department of Psychology, Virginia Tech 0436, Blacksburg, VA 24061
Roger Roffman, School of Social Work, University of Washington, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020
Josephine DeMarce, 1970 Roanoke Blvd, Psychology (116A4), Salem, VA 24153.
Brian Lozano, Department of Psychology, Virginia Tech 0436, Blacksburg, VA 24061.
Sheri Towe, Department of Psychology, Virginia Tech 0436, Blacksburg, VA 24061.
Belinda Berg, School of Social Work, University of Washington, Innovative Programs Research Group, 909 NE 43rd Street, Suite 304, Seattle, WA 98105-6020.
References
- Anthony JC, Helzer JE. Syndromes of drug abuse and dependence. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America. New York: Free Press, MacMillan; 1991. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substance, and inhalants: Basic finding from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology. 1994;2:244–268. [Google Scholar]
- Berghuis JP, Swift W, Roffman RA, Stephens RS, Copeland J. The Teen Cannabis Check-Up: Exploring Strategies for Reaching Young Cannabis Users. In: Roffman RA, Stephens RS, editors. Cannabis Dependence Its Nature, Consequences and Treatment. New York: Cambridge University Press; 2006. [Google Scholar]
- Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, Ford HL, Vitolo SA, Doebrick CA, Rounsaville BJ. The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. Journal of Consulting and Clinical Psychology. 2006;74:955–966. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Research. Substance Abuse and Mental Health Services Administration. Report to HW Clark, Director. Sep, 2000a. The Cannabis Youth Treatment (CYT) Experiment: Preliminary Findings. [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA: Journal of the American Medical Association. 2004;291(17):2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Davis LJ, Hoffman NG, Morse RM, Luehr JG. Substance use disorder diagnostic schedule (SUDDS) – the equivalence and validity of a computer-administered and an interviewer-administered format. Alcoholism-Clinical and Experimental Research. 1992;16:250–254. doi: 10.1111/j.1530-0277.1992.tb01371.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML. Global Appraisal of Individual Needs (GAIN) manual: Administration, scoring and interpretation, (Prepared with funds from CSAT TI 11320) Bloomington, IL: Lighthouse Publications; 1998. [Google Scholar]
- Dennis ML. Cannabis youth treatment (CYT) cooperative agreement: The need & the study. Talk presented at the CSAT Initiatives at the “Treatment of Adolescent Substance Abusers” panel; Rockville, MD. Feb, 1999. [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(suppl 2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley S, Diamond G, Tims F, Babor T, Donaldson J, Liddle H, Titus JD, Kaminer Y, Webb C, Hamilton N, Funk R. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, Diamond G, Donaldson J, Godley SH, Tims F, et al. The Cannabis Youth Treatment (CYT) Experiment: Rationale, study design, and analysis plans. Addiction. 2002;97(Supplement I):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Titus JC, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures. (Version) 5. Bloomington, IL: Chestnut Health Systems; 2003. Retrieved from www.chestnut.org/li/gain. [Google Scholar]
- Diamond G, Leckrone J, Dennis M, Godley SH. The Cannabis Youth Treatment Study: The Treatment Models and Preliminary Findings. In: Roffman RA, Stephens RS, editors. Cannabis dependence: Its nature, consequences, and treatment. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- EMCDDA. Annual Report 2009: The state of the drugs problem in Europe. European Monitoring Centre for Drugs and Drug Addiction; Lisbon: 2009. [Google Scholar]
- Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behavior Research Methods, Instruments, & Computers. 1996;28:1–11. [Google Scholar]
- Erdman H, Klein MH, Greist JH. The reliability of a computer interview for drug use/abuse information. Behavior Research Methods and Instrumentation. 1983;15(1):66–68. [Google Scholar]
- Gray E, McCambridge J, Strang J. The effectiveness of motivational interviewing delivered by youth workers in reducing drinking, cigarettes, and cannabis smoking among young people: Quasi-experimental pilot study. Alcohol and Alcoholism. 2005;40(6):535–539. doi: 10.1093/alcalc/agh199. [DOI] [PubMed] [Google Scholar]
- Hall W, Solowij N, Lemon J. The health and psychological consequences of cannabis use. Monograph Series No. 25. Canberra, Australia: Australian Government Publishing Service; 1994. [Google Scholar]
- Hibell B, Andersson B, Bjarnason T, Ahlstrom S, Balakireva O, Kokkevi A, Morgan M. The ESPAD report 2003: alcohol and other drug use among students in 35 European countries. Stockholm: Swedish Council for Information on Alcohol and Other Drugs; 2004. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2007 (NIH Publication No. 08-6418) Bethesda, MD: National Institute on Drug Abuse; 2008. [Google Scholar]
- Johnson V, White HR. An investigation of factors related to intoxicated driving behaviors among youth. Journal of Studies on Alcohol. 1989;50:320–330. doi: 10.15288/jsa.1989.50.320. [DOI] [PubMed] [Google Scholar]
- Kandel D, Chen K, Warner LA, Kessler RC, Grant B. Prevalence and demographic correlates of symptoms of last year dependence on alcohol, nicotine, marijuana and cocaine in the U.S. population. Drug and Alcohol Dependence. 1997;44:11–29. doi: 10.1016/s0376-8716(96)01315-4. [DOI] [PubMed] [Google Scholar]
- Kypri K, Langley JD, Saunders JD, Cashell-Smith ML. Assessment may conceal therapeutic benefit: Findings from a randomized controlled trial for hazardous drinking. Addiction. 2007;102:62–70. doi: 10.1111/j.1360-0443.2006.01632.x. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Pedersen ER, Earleywine M, Olsen H. Reducing heavy drinking in college males with the decisional balance: Analyzing an element of Motivational Interviewing. Addictive Behaviors. 2006;31:254–263. doi: 10.1016/j.addbeh.2005.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennox R, Dennis ML, Ives M, White MK. The construct and predictive validity of different approaches to combining urine and self-reported drug use measures among older adolescents after substance abuse treatment. American Journal on Addictions. 2006;15:92–101. doi: 10.1080/10550490601006089. [DOI] [PubMed] [Google Scholar]
- Martin G, Copeland J. The adolescent cannabis check-up: Randomized trial of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2008;34:407–414. doi: 10.1016/j.jsat.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Martin G, Copeland J, Swift W. The Adolescent Cannabis Check-Up: Feasibility of a brief intervention for young cannabis users. Journal of Substance Abuse Treatment. 2005;29:207–213. doi: 10.1016/j.jsat.2005.06.005. [DOI] [PubMed] [Google Scholar]
- McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multi-site cluster randomized trial. Addiction. 2004;99:39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- McElrath K. A comparison of two methods for examining inmates’ self-reported drug use. The International Journal of the Addictions. 1994;29:517–524. doi: 10.3109/10826089409047397. [DOI] [PubMed] [Google Scholar]
- Miller WR, Sovereign RG, editors. The check-up: A model for early intervention in addictive behaviors. Amsterdam: Swets & Zeitlinger; 1989. [Google Scholar]
- Modisette KC, Hunter BD, Ives ML, Funk RR, Dennis ML. NORMS including alpha, mean, N, sd, ICC for Adolescents (by demographics) and overall for Young Adults (18–25) and Adults (18+) using the CSAT 2008 V5 Dataset [Electronic version] Normal, IL: Chestnut Health Systems; 2009. Retrieved April 15, 2010 from http://chestnut.org/LI/Posters/Norms_by_Demog_2008dataset.xls. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0(MITI 3.0) Albuquerque, NM: University of New Mexico Center on Alcoholism, Substance Abuse and Addictions; 2007. [Google Scholar]
- Perkonigg A, Goodwin RD, Fiedler A, Behrendt S, Beesdo K, Lieb R, Wittchen H. The natural course of cannabis use, abuse and dependence during the first decades of life. Addiction. 2007;103:439–449. doi: 10.1111/j.1360-0443.2007.02064.x. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Lieb R, Hoefler M, Schuster P, Sonntag H, Wittchen HU. Patterns of cannabis use, abuse and dependence over time: Incidence, progression and stability in a sample of 1228 adolescents. Addiction. 1999;94:1663–1678. doi: 10.1046/j.1360-0443.1999.941116635.x. [DOI] [PubMed] [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users: 5 Sessions, Cannabis Youth Treatment (CYT) Series, Volume 1. (DHHS Publication No. SMA 01-3486) Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental health Services Administration; 2001. p. BKD384. [Google Scholar]
- Sinha R, Easton C, Renee-Aubin L, Carroll KM. Engaging young probation referred marijuana-abusing individuals in treatment: a pilot trial. American Journal of Addictions. 2003;12:314–323. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS): 1992–2002. National Admissions to Substance Abuse Treatment Services. (DHHS Publication No. SMA 04-3965) Rockville, MD: Department of Health and Human Services; 2004. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: National Findings (NSDUH Series H-34, DHHS Publication No. SMA 08-4343) Rockville, MD: 2008. [Google Scholar]
- Swan M, Schwartz S, Berg B, Walker D, Stephens R, Roffman R. The Teen Marijuana Check-Up: An In-School Protocol for Eliciting Voluntary Self-Assessment of Marijuana Use. Journal of Social Work Practice in the Addictions. 2008;8:284–302. doi: 10.1080/15332560802223305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Walker D, Roffman R, Stephens R, Berghuis J, Kim W. Motivational Enhancement Therapy for Adolescent Marijuana Users: A Preliminary Randomized Controlled Trial. Journal of Consulting and Clinical Psychology. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb PM, Zimet GD, Fortenberry D, Blythe M. Comparability of a computer-assisted versus written method for collecting health behavior information from adolescent patients. Journal of Adolescent Health. 1999;24:383–388. doi: 10.1016/s1054-139x(99)00005-1. [DOI] [PubMed] [Google Scholar]
- West R. Time for a change: Putting the Transtheoretical (Stages of Change) Model to rest. Addiction. 2005;100:1036–1039. doi: 10.1111/j.1360-0443.2005.01139.x. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]