Abstract
Avoidance coping (AVC) is common in individuals with posttraumatic stress disorder (PTSD) and in individuals with alcohol use disorder (AUD). Given that PTSD and AUD commonly co-occur, AVC may represent a risk factor for the development of comorbid post-traumatic stress and alcohol use. In this study, the relationship between AVC and PTSD symptoms (PTSS) was examined in individuals with versus without AUDs. Motor vehicle accident (MVA) victims were assessed 6-weeks post accident for AUD history (i.e. diagnoses of current/past alcohol abuse/dependence) and AVC. PTSS were assessed 6-weeks and 6-months post-MVA. All analyses were conducted on the full sample of MVA victims as well as on the subset of participants who were legally intoxicated (BAC ≥ 0.08) during the accident. It was hypothesized that the relationship between AVC and PTSS would be stronger in those individuals with an AUD history and especially strong in the subset of individuals who were legally intoxicated during the MVA. Results were largely supportive of this hypothesis, even after controlling for in-hospital PTSS, gender, and current major depression. Early assessment of AUD history and avoidance coping may aid in detecting those at elevated risk for PTSD, and intervening to reduce avoidance coping soon after trauma may help to buffer the development of PTSD+AUD comorbidity.
Keywords: Avoidance coping, Alcohol use disorder, Substance use disorder, Posttraumatic stress disorder (PTSD)
Posttraumatic stress disorder (PTSD) and substance use disorders (SUDs) commonly co-occur, with rates of PTSD ranging from 28–55% in individuals seeking treatment for alcohol/drug use (Coffey, Schumacher, Brady, & Cotton, 2007; Ouimette, Read, & Brown, 2005; Staiger, Melville, Hides, Kambouropoulos, & Lubman, 2009). The co-occurrence of PTSD and alcohol use disorders (AUDs) is particularly common, with epidemiological studies indicating that up to 52% of men and 28% of women with PTSD also meet lifetime criteria for alcohol abuse or dependence (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). This high prevalence is notable, given that comorbid individuals (PTSD+AUD) often use greater amounts of costly addiction treatment services (Brown, Stout, & Mueller, 1999), experience poor addiction treatment outcomes (Ouimette, Ahrens, Moos, & Finney, 1997), and report greater chronic health stressors (Tate, Norman, McQuaid, & Brown, 2007) than individuals with a single diagnosis. Given the high comorbidity of PTSD and AUD, as well as the synergistic impact of PTSD and AUD on impairment, a greater understanding of mechanisms linking the two disorders is needed so that appropriate and effective care can be administered to individuals experiencing PTSD+AUD.
Researchers have hypothesized that individuals with PTSD use substances such as alcohol to self-medicate or relieve psychological distress resulting from their trauma symptoms (Brady, Back, & Coffey, 2004; Brown & Wolfe, 1994; Stewart, Pihl, Conrod, & Dongier, 1998). Thus, psychological distress has been posited to be a key factor accounting for PTSD+AUD comorbidity. Empirical research seems to support this claim. For example, in a sample of Vietnam Veterans, PTSD symptoms (PTSS) positively correlated with alcohol use severity (McFall, Mackay, & Donovan, 1992). Similar findings were reported in a sample of community dwelling women who experienced childhood rape; in this study PTSS served as a mediator between childhood rape and alcohol use (Epstein, Saunders, Kilpatrick, & Resnick, 1998).
Stronger evidence for the role that psychological distress plays in the comorbidity of PTSD and alcohol use comes from a recent set of cue-based studies – in which the reactions of individuals with PTSD+SUD were recorded following exposure to either drug- or trauma-related cues. Using this paradigm, Coffey et. al. (2002) found that individuals with PTSD and either alcohol or cocaine dependence reported elevated levels of craving in response to both trauma imagery and in vivo drug cues, compared to craving ratings given in response to neutral cues. However, individuals with PTSD and alcohol dependence reported significantly greater distress and craving in response to these cues relative to those with PTSD and cocaine dependence suggesting that psychological distress may be a key motivating factor for substance use amongst those with PTSD+AUD. This same group of researchers has also found that more severe PTSS are associated with greater alcohol craving following trauma cue exposure (Saladin et. al., 2003) – particularly when those symptoms are secondary to childhood trauma (Schumacher, Coffey, & Stasiewicz, 2006). Finally, it has been demonstrated that the relationship between distress, alcohol craving, and trauma cue exposure weakens following PTSS reduction secondary to exposure based therapy (Coffey, Stasiewicz, Hughes, & Brimo, 2006). Thus, particularly for those with alcohol dependence and PTSD, it would seem that substance use is, at least in part, motivated by PTSS and the psychological distress experienced secondary to those symptoms. However, additional research is needed to identify potential factors that may be common to both PTSD and AUD that may partially account for the comorbidity of these disorders. Therefore, the present study sought to fill this need by examining avoidance coping – a variable that has been identified as a risk factor for both PTSD and AUD.
Avoidance coping (AVC) is a set of cognitive and behavioral reactions to stress characterized by passivity or disengagement from the source of distress (Moos & Holahan, 2003; Olff, Langeland, & Gersons, 2005; Ullman, Townsend, Filipas, & Starzynski, 2007; Wong, Looney, Michaels, Palesh, & Koopman, 2006). Cross-sectional research has found AVC to be related to drug use (Belding, Iguchi, Lamb, Lakin, & Terry, 1996), and AVC has been linked with a greater number of drinking problems in adults, especially in individuals who hold positive alcohol expectancies (Moos, Brennan, Fondacaro, & Moos, 1990; Cooper, Russell, Skinner, Frone, & Mudar, 1992). Similar findings have been observed in adolescents, with greater levels of AVC associated with greater alcohol consumption, alcohol-related problems, and tendencies to drink to cope with stress and a greater number of life stressors (Laurent, Catanzaro, & Callan, 1997). Longitudinal studies have found that decreases in AVC during drug use treatment predicted abstinence at 6-months in participants with opioid dependence, especially in those who presented to treatment with high levels of depression (Avants, Warbuton, & Margolin, 2000). Finally, lower levels of AVC have been shown to be associated with abstinence from alcohol 1-year following treatment (Timko, Finney, & Moos, 2005).
AVC is also consistently found to positively relate to PTSS in both cross-sectional (Bryant & Harvey, 1995; Ullman et. al., 2007) and longitudinal research, suggesting that AVC may serve as a risk factor for elevated PTSS in burn injury victims (Lawrence, Fauerbach, & Munster, 1996), veterans (Tiet, Rosen, Cavella, Moos, Finney, & Yesavage, 2006), and battered women (Krause, Kaltman, Goodman, & Dutton, 2008). Information-processing theories have been posited to explain the relationship between AVC and PTSD. Generally speaking, these theories propose that PTSD arises from a memory network that represents the traumatic event as threatening, unpredictable, and uncontrollable – ultimately leading to the execution of escape or avoidance behavior that typifies PTSS (Chemtob, Roitblat, Hamada, Carlson, & Twentyman, 1988; Foa & Kozak, 1986). Consequently, exposure to feared stimuli associated with the trauma is proposed to reduce PTSS through habituation and the integration of new information representing previously feared situations and trauma cues as safe. Avoidance of feared stimuli is thought to prevent habituation and integration, leading to the maintenance of PTSS (Creamer, Burgess, & Pattison, 1992; Foa, Steketee, & Rothbaum, 1989).
Given the links between alcohol use and AVC, it stands to reason that individuals with an AUD history may be more likely to engage in AVC, putting them at greater risk to develop PTSS following exposure to a traumatic event. Demonstration of support for this hypothesis is of importance, given that the modification of coping skills lends itself easily to intervention, accounting for its incorporation in both PTSD and AUD treatments (Foa & Rothbaum, 1998; Monti, Kadden, Rohsenow, Cooney, & Abrams, 2002). Thus, support for this hypothesis may identify one factor common to both PTSD and AUD that may be targeted in interventions that aim to prevent/treat these two disorders.
To elucidate the potential role of AVC in PTSD+AUD comorbidity, the present study sought to examine the association between AVC and PTSS experienced in response to an MVA in individuals with versus without a history of alcohol abuse or dependence. It was hypothesized that AVC would be associated with greater subsequent PTSS and that AVC and AUD history would interact such that the relationship between AVC and PTSS would be stronger for those with versus without an AUD history. In addition, individuals with BACs ≥ 0.08 during the MVA were examined in separate analyses, given that a high proportion of individuals with AUDs were anticipated to belong to this subset (Gómez-Talegón & Alvarez, 2006; Lapham et. al., 2001). Further, this subset was examined separately to reflect an objectively-identified group with likely more severe AUDs (e.g. characterized by more frequent alcohol use, alcohol related problems, etc.) (Eensoo, Paaver, Harro, & Harro, 2005). Analyses were conducted both crosssectionally – with AUD history, avoidance coping, and PTSS measured 6-weeks post-MVA – as well as prospectively – with AUD history and avoidance coping measured 6-weeks post-MVA and PTSS assessed 6-months post-MVA.
Methods
Participants
Three hundred fifty-six non-amnesic MVA victims (211 male, 145 female) admitted to a level-1 trauma center were recruited during their hospital stay. Follow-up assessments occurred at 6-weeks and 6-months post-accident. Ages ranged from 18–87 (M = 38.66, SD = 16.21), and approximately 88% were Caucasian, 10% were African American, 0.3% were Hispanic, and 1% reported other ethnicities. At the 6-week follow-up, 251 participants provided at least partial data, and at 6-months follow-up, 196 were retained.
Those retained at 6-weeks did not differ from those non-retained in terms of in-hospital PTSS scores (assessed via the Impact of Event Scale-Revised [IES-R]), age, or income (all ps > 0.05). However, a greater proportion of males and African Americans were lost to 6-week follow-up (ps < 0.05). Those retained at 6-months did not differ from those non-retained in terms of age or income (all ps > 0.05). However, a greater proportion of males, African Americans, and individuals with higher in-hospital IES-R PTSS were not retained (all ps < 0.05). In-hospital IES-R PTSS and gender were related to PTSS at 6-weeks and 6-months (assessed via the Clinician Administered PTSD Scale [CAPS] see Table 2), while the effects of race were non-significant at both 6-weeks and 6-months (all ps > 0.05). Thus, in-hospital IES-R PTSS and gender were included as covariates in all analyses. Furthermore, given the high comorbidity between depression and PTSD, current major depression was also included as a covariate in all analyses. Length of hospital stay (as assessed by the number of hours spent in hospital) and injury severity (as determined by Injury Severity Scores [Baker, O’Neill, Haddon, & Long, 1974]) were also considered as potential covariates, given the possibility that longer hospital stays due to more severe injuries may be associated with elevated PTSS. However, neither of these variables correlated with PTSS at either 6-weeks or 6-months (all p’s > 0.05). Thus, these variables were not included as covariates.
Table 2.
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | M | SD |
|---|---|---|---|---|---|---|---|---|
| 6-Week Follow Up (N=238) | ||||||||
| 1. IES-R PTSS | 3.49 | 2.25 | ||||||
| 2. Gender | 0.13* | 0.45 | 0.50 | |||||
| 3. Depression | 0.18** | 0.25*** | 0.13 | 0.34 | ||||
| 4. AUD | 0.07 | −0.17** | 0.01 | 0.31 | 0.46 | |||
| 5. AVC | 0.32*** | 0.11 | 0.28*** | 0.01 | 9.99 | 3.32 | ||
| 6. CAPS PTSS | 0.46*** | 0.25*** | 0.52*** | 0.23*** | 0.46*** | 25.76 | 20.89 | |
|
| ||||||||
| 6-Month Follow Up (N=182) | ||||||||
| 1. IES-R PTSS | 3.37 | 2.23 | ||||||
| 2. Gender | 0.16* | 0.48 | 0.50 | |||||
| 3. Depression | 0.29*** | 0.19** | 0.13 | 0.33 | ||||
| 4. AUD | 0.08 | −0.17* | 0.08 | 0.26 | 0.44 | |||
| 5. AVC | 0.38*** | 0.15* | 0.27*** | 0.01 | 9.92 | 3.36 | ||
| 6. CAPS PTSS | 0.46*** | 0.31*** | 0.58*** | 0.12 | 0.51*** | 20.84 | 19.38 | |
IES-R = Impact of Event Scale-Revised; AUD = alcohol use disorder history; AVC = avoidance coping; CAPS = Clinician-Administered PTSD Scale
Gender was dummy coded such that a value of 0 = male and a value of 1 = female
*p < 0.05, **p < 0.01, ***p < 0.001
BAC data (M = 0.16, SD = 0.08) were collected via medical chart review and were available for 78 (60 males, 18 females) participants. Of these 78, 63 (46 males, 17 females) had BACs greater than or equal to 0.08. At 6-weeks, 36 were retained and at 6-months, 21 were retained. Those retained at either the 6-week or 6-month follow-up did not differ from those non-retained at each time point in terms of in hospital IES-R PTSS, age, gender, income, or race (ps > 0.05). Examination of the raw data for the entire sample revealed that no more than 9% of the data for avoidance coping and no more than 6% of the data for the PTSD measures (i.e. 6% IES-R; 4% CAPS) were missing. In order to include data from all participants, imputation based upon an expectation maximization algorithm was used for these variables (Bentler, 2004). While only 1% of the depression data and 5% of the AUD data were missing, imputation was not conducted on these variables given the conceptual difficulties with imputing dichotomous diagnoses. Following imputation, complete data were available for 238 participants (131 male, 107 female) at 6-weeks and 182 participants (94 male, 88 female) at 6-months. In participants with BACs ≥ 0.08, data were available for 33 (22 males, 11 females) participants at 6-weeks and 19 (11 males, 8 females) participants at 6-months.
Procedures
The following procedures were approved by the Human Subjects Review Boards of Summa Health System, Akron General Medical Center, and Kent State University. MVA victims admitted to one of two level-1 trauma centers with Glasgow Coma Scale scores ≥ 14 were approached by the head trauma nurse. Participants were administered the Mini Mental Status Exam (MMSE; Folstein, Folstein, & McHugh, 1975) in order to determine ability to give informed consent. If a patient was deemed eligible, a researcher approached the patient, explained the study in detail, and obtained written informed consent. During the initial inhospital interview, demographic information was collected and the IES-R (Weiss & Marmar, 1997) was administered to assess initial PTSS.
Follow up assessments were conducted in participants’ homes by a Master’s level clinical psychology graduate student at 6-weeks and 6-months post-MVA. The time intervals associated with those follow up assessments were selected for practical, theoretical, and empirical reasons. In the larger-scale study from which the current data are analyzed, a 2-week follow up was conducted in order to assess for the presence of Acute Stress Disorder. Thus, a six-week follow up was selected as it allows participants to meet the PTSS duration criterion (Criterion E: One month) (American Psychiatric Association, 2000) without being overly burdensome to participants (by having a 2- and 4- week assessment). Furthermore, research indicates that for most individuals who experience a traumatic event, PTSS tend to dissipate over time (Blanchard et. al., 1996; Shalev, 2002). Thus, symptoms at 6-weeks are considered acute PTSS and, even at six weeks, many participants meeting acute PTSD criteria will tend to recover without intervention. The 6-month time point reflects chronic PTSS, and participants who are symptomatic at this point are not likely to recover without intervention. Empirically, similar time points are the standard for assessing PTSS in the trauma field (Bustamante, Mellman, David, & Fins, 2001; Murray, Ehlers, & Mayou, 2002; Resnick et. al., 2007; Vaiva et. al., 2006).
During the 6-week follow up assessment, participants were screened for alcohol abuse and d ependence, as well as current major depression using the Structured Clinical Interview for DSM-IV (SCID-IV: First, Gibbon, Spitzer, & Williams, 1996). In addition, PTSS were assessed with the CAPS (Blake et. al., 1995) and coping was assessed with the Brief Cope (Carver, 1997). At the 6-month follow up PTSS were assessed once again with the CAPS.
Measures
AUD History
The SCID-IV is a semi-structured clinical interview that is used to make diagnoses for DSM axis-I disorders (First, Gibbon, Spitzer, & Williams, 1996). The substance use modules of the SCID have demonstrated sufficient validity and reliability (Kranzler et. al., 1996; Skre, Onstad, Torgersen, & Kringlen, 1991). In the present study, the substance use modules were used to make diagnoses of past and current alcohol abuse and dependence. Given current research suggesting that addiction is best conceptualized as a chronic disease with symptoms that fluctuate with the passage of time (McClellan, Lewis, O’Brien, & Kleber, 2000; White, Boyle, & Loveland, 2002), those with past or current alcohol abuse or dependence were grouped together and classified as having an AUD history, while those without either of these diagnoses were classified as not having an AUD history.
Depression
The SCID-IV was also used to make diagnoses of current depression. The depression module of the SCID has been found to have good reliability (Riskind, Beck, Berchick, Brown, & Steer, 1987).
PTSS
The Impact of Event Scale-Revised (IES-R) is a 22-item self-report scale that was used to assess in-hospital PTSS in the present study (Weiss & Marmar, 1997). Adequate validity and reliability has been reported for the IES-R among MVA survivors (Beck et. al., 2008). Internal consistency estimates in the present study were found to be adequate at both 6-weeks (α = 0.88) and at 6-months (α = 0.89). In the current study the means of the intrusion, avoidance, and hyperarousal subscales of the IES-R were summed to obtain a global measure of PTSSl.
The Clinician-Administered PTSD Scale (CAPS) is a semi-structured clinical interview that was used to assess PTSD at 6-weeks and 6-months post-MVA in the present study (Blake et. al., 1995). The CAPS is considered the gold standard in trauma research and has been shown to have strong psychometric properties (Weathers, Keane, & Davidson, 2001). Interrater reliability for the CAPS in the current study was found to be strong at both 6-weeks (r = 0.98, p < 0.001) and 6-months (r = 0.97, p < 0.001). The CAPS can be used to obtain both a categorical diagnosis of PTSD, as well as a measure of continuous PTSS. In the present study, the CAPS was used to obtain current and lifetime categorical diagnoses of PTSD and current subsyndromal PTSD at 6-weeks and 6-months post-MVA. Consistent with prior research, subsyndromal PTSD was operationalized as meeting criteria for 2 of the 3 symptom clusters (Koren, Norman, Cohen, Berman, & Klein, 2005; Mellman, David, Bustamante, Fins, & Esposito, 2001). The CAPS was also used to obtain a continuous measure of PTSS experienced in response to the MVA at 6-weeks and 6-months post-MVA.
Avoidance Coping
The Brief Cope is a 28-item measure assessing 14 dimensions of coping (Carver, 1997). In the present study, participants were asked to rate the frequency with which they had been using each coping strategy since the MVA on a scale ranging from 1 (‘I haven’t been doing this at all’) to 4 (‘I have been doing this a lot’). Consistent with prior research, avoidance coping was assessed by taking the unweighted sum of the items comprising the self-distraction, denial, and behavioral disengagement subscales of the Brief Cope (Ullman, Filipas, Townsend, & Starzynski, 2007; Ullman et. al., 2007; Wong et. al., 2006). Internal consistency estimates in the present study were found to be adequate at both 6-weeks (α = 0.68) and at 6-months (α = 0.67).
Results
All analyses were conducted using SPSS 15.0 for Windows (SPSS Inc., 2006). Moderation analyses were conducted within a regression framework given the continuous level of the independent variable (avoidance coping) and the dichotomous nature of the moderator (AUD history) (Baron & Kenny, 1986). In addition, to ease interpretation of the results, all continuous predictors (i.e. AVC and IES-R PTSS) were standardized (i.e. z-transformed) prior to moderation analyses (Cohen, Cohen, West, & Aiken, 2003; Frazier, Tix, & Barron, 2004). Within regression, moderation is tested by first entering the main effects of the moderator and independent variables, after removing the effects of any control variables that are of interest. In the final step of the regression, the product term between the moderator and independent variable (e.g. AUD history x AVC) is entered. Moderation is said to be present when the product term is statistically significant over and above the additive effects of the main effects (Cohen et. al., 2003).
Descriptive Statistics
Diagnostic frequencies, means, standard deviations, and bivariate correlations for the study variables are presented in Tables 1 and 2. As can be seen from Table 1, consistent with predictions, a larger proportion of individuals with BACs ≥ 0.08 were diagnosed with alcohol abuse or dependence diagnoses relative to the full sample.
Table 1.
Frequencies for Alcohol Use Disorder, PTSD, Subsyndromal PTSD, and Major Depression Diagnoses a
| 6-Weeks | 6-Months | |||
|---|---|---|---|---|
| N | % | N | % | |
| Full Sample (N=238) | Full Sample (N=182) | |||
| Current AA | 9 | 3.8% | 7 | 3.8% |
| Past AA | 18 | 7.6% | 9 | 4.9% |
| Current AD | 8 | 3.4% | 3 | 1.6% |
| Past AD | 39 | 16.4% | 28 | 15.4% |
| Current PTSD | 25 | 10.5% | 14 | 7.7% |
| Lifetime PTSD | 42 | 17.6% | 32 | 17.6% |
| Current Sub-PTSD | 53 | 22.3% | 24 | 13.2% |
| Current Depression | 31 | 13.0% | 23 | 12.6% |
|
| ||||
| BAC Subsample (N=33) | BAC Subsample (N=19) | |||
| Current AA | 4 | 12.1% | 3 | 15.8% |
| Past AA | 4 | 12.1% | 2 | 10.5% |
| Current AD | 3 | 9.1% | 1 | 5.3% |
| Past AD | 14 | 42.4% | 8 | 42.1% |
| Current PTSD | 6 | 18.2% | 0 | 0.0% |
| Lifetime PTSD | 11 | 33.3% | 7 | 36.8% |
| Current Sub-PTSD | 10 | 30.3% | 2 | 10.5% |
| Current Depression | 2 | 6.1% | 2 | 10.5% |
AA = alcohol abuse; AD = alcohol dependence; PTSD = posttraumatic stress disorder; Sub-PTSD = subsyndromal posttraumatic stress disorder
Moderation Analyses: Full Sample
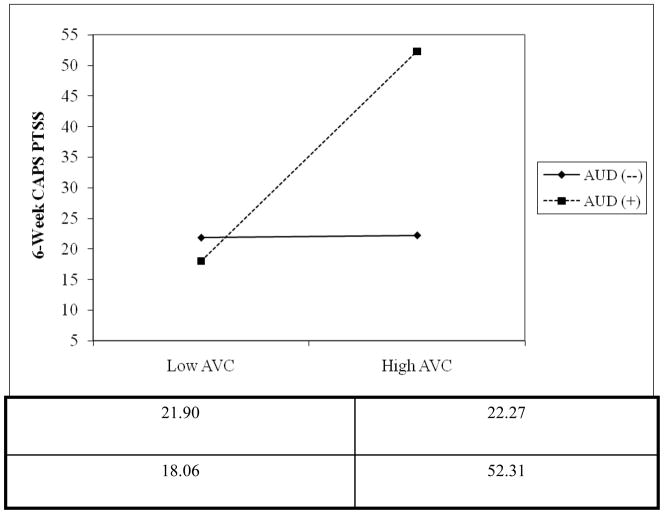
As can be seen in Table 3, consistent with our hypotheses, after controlling for IES-R PTSS scores, gender, and depression, AVC at 6-weeks was associated with greater CAPS PTSS scores at 6-weeks (β = 0.26, p < 0.001) and at 6-months (β = 0.30, p < 0.001). In the final step of the regression, when the product term was included in the model, moderation was observed at 6-weeks (β = 0.11, p < 0.05) but was present only at the trend level at 6-months (β = 0.10, p ≤ 0.10). To better understand the nature of the interaction observed at 6-weeks, a plot of predicted values for the dependent variable at each level of the moderator was constructed (Frazier, Tix, & Barron, 2004). Consistent with our predictions, examination of this plot suggested that while a positive relationship was observed between AVC and CAPS PTSS scores at 6-weeks at both levels of the moderator, greater AVC was associated with greater CAPS PTSS scores for those with an AUD history (see Figure 1).
Table 3.
Summary of Hierarchical Regression Moderation Analyses Examining the Interaction Between Alcohol Use Disorder History and Avoidance Coping in the Full Sample of MVA Victims a,b,c
| Step and Variables | B | SE B | 95% CI | β | ΔR2 |
|---|---|---|---|---|---|
| 6-Week Follow Up (N=238) | |||||
| Step 1 | |||||
| IES-R PTSS | 7.72 | 1.06 | 5.63, 9.81 | 0.37*** | |
| Gender | 3.94 | 2.16 | −0.31, 8.20 | 0.09+ | |
| Depression | 26.90 | 3.22 | 20.56, 33.24 | 0.43*** | 0.42*** |
| Step 2 | |||||
| IES-R PTSS | 5.79 | 1.01 | 3.81, 7.77 | 0.28*** | |
| Gender | 5.62 | 1.99 | 1.69, 9.55 | 0.13** | |
| Depression | 22.75 | 3.00 | 16.84, 28.66 | 0.37*** | |
| AUD | 10.41 | 2.07 | 6.33, 14.49 | 0.23*** | |
| AVC | 5.39 | 1.02 | 3.38, 7.40 | 0.26*** | 0.11*** |
| Step 3 | |||||
| IES-R PTSS | 5.93 | 1.00 | 3.96, 7.90 | 0.28*** | |
| Gender | 5.55 | 1.98 | 1.65, 9.45 | 0.13** | |
| Depression | 22.00 | 2.99 | 16.11, 27.90 | 0.35*** | |
| AUD | 10.34 | 2.05 | 6.29, 14.38 | 0.23*** | |
| AVC | 4.23 | 1.14 | 1.98, 6.48 | 0.20*** | |
| AUD x AVC | 4.79 | 2.18 | 0.49, 9.10 | 0.11* | 0.01* |
|
| |||||
| 6-Month Follow Up (N=182) | |||||
| Step 1 | |||||
| IES-R PTSS | 5.83 | 1.12 | 3.61, 8.04 | 0.30*** | |
| Gender | 6.54 | 2.19 | 2.23, 10.86 | 0.17** | |
| Depression | 26.83 | 3.39 | 20.13, 33.53 | 0.46*** | 0.46*** |
| Step 2 | |||||
| IES-R PTSS | 3.78 | 1.11 | 1.59, 5.96 | 0.19** | |
| Gender | 6.54 | 2.07 | 2.45, 10.63 | 0.17** | |
| Depression | 23.51 | 3.21 | 17.18, 29.84 | 0.40*** | |
| AUD | 4.15 | 2.32 | −0.42, 8.72 | 0.09+ | |
| AVC | 5.77 | 1.09 | 3.61, 7.93 | 0.30*** | 0.08*** |
| Step 3 | |||||
| IES-R PTSS | 3.89 | 1.10 | 1.71, 6.07 | 0.20** | |
| Gender | 6.49 | 2.06 | 2.42, 10.56 | 0.17** | |
| Depression | 23.45 | 3.19 | 17.15, 29.75 | 0.40*** | |
| AUD | 4.08 | 2.31 | −0.47, 8.63 | 0.09+ | |
| AVC | 4.82 | 1.23 | 2.39, 7.24 | 0.25*** | |
| AUD x AVC | 3.86 | 2.32 | −0.72, 8.44 | 0.10+ | 0.01+ |
CI = confidence interval; AUD = alcohol use disorder history; AVC = avoidance coping; IES-R = Impact of Event Scale-Revised; PTSS = posttraumatic stress symptoms
Gender was dummy coded such that a value of 0 = male and a value of 1 = female
+ p < 0.10, *p < 0.05, **p < 0.01, *** p < 0.001
Figure 1.
Plotted Means Illustrating Moderating Effect of AUD History by Avoidance Coping on 6-Week CAPS PTSS Amongst the Full Sample of MVA Victims (N = 238).
NOTE. AUD (+) = alcohol abuse or dependence history present; AUD (-) = alcohol abuse or dependence history absent; AVC = avoidance coping; CAPS = Clinician-Administered PTSS Scale; PTSS = posttraumatic stress symptoms
Moderation Analyses: BAC ≥ 0.08 Subset
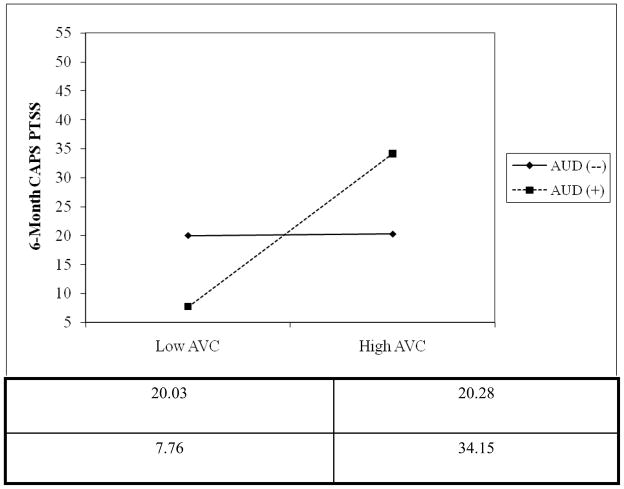
As can be seen in Table 4, when analyses were limited to the subset of MVA victims who were intoxicated at the time of the MVA, AVC at 6-weeks was related to CAPS PTSS scores at 6-weeks (β = 0.43, p < 0.05) but not at 6-months (β = 0.29, p = ns) after controlling for IES-R PTSS scores, gender, and depression. When the product term was included in the model, moderation was observed at both 6-weeks (β = 0.56, p < 0.05) and at 6-months (β = 0.55, p < 0.05). Examination of the plots of predicted values for the statistically significant interactions suggested that greater AVC at 6-weeks was associated with greater CAPS PTSS scores at 6-weeks and 6-months after controlling for IES-R PTSS scores, gender, and depression (see Figures 2 and 3).
Table 4.
Summary of Hierarchical Regression Moderation Analyses Examining the Interaction Between Alcohol Use Disorder History and Avoidance Coping in the BAC ≥ 0.08 Subset of MVA Victims a,b,c
| Step and Variables | B | SE B | 95% CI | β | ΔR2 |
|---|---|---|---|---|---|
| 6-Week Follow Up (N=33) | |||||
| Step 1 | |||||
| IES-R PTSS | 2.18 | 4.00 | −6.00, 10.35 | 0.10 | |
| Gender | 0.06 | 7.77 | −15.84, 15.96 | 0.001 | |
| Depression | 28.75 | 16.51 | −5.03, 62.52 | 0.33+ | 0.14 |
| Step 2 | |||||
| IES-R PTSS | −1.92 | 3.89 | −9.90, 6.07 | −0.09 | |
| Gender | 3.98 | 7.22 | −10.84, 18.81 | 0.09 | |
| Depression | 22.65 | 15.11 | −8.36, 53.66 | 0.26 | |
| AUD | 14.89 | 8.19 | −1.90, 31.69 | 0.30+ | |
| AVC | 9.22 | 3.64 | 1.74, 16.69 | 0.43* | 0.20* |
| Step 3 | |||||
| IES-R PTSS | 0.81 | 3.69 | −6.78, 8.41 | 0.04 | |
| Gender | 1.66 | 6.63 | −11.97, 15.29 | 0.04 | |
| Depression | 12.08 | 14.34 | −17.39, 41.56 | 0.14 | |
| AUD | 13.10 | 7.48 | −2.27, 28.47 | 0.27+ | |
| AVC | 0.18 | 4.82 | −9.73, 10.09 | 0.10 | |
| AUD x AVC | 16.94 | 6.57 | 3.44, 30.44 | 0.56* | 0.13* |
|
| |||||
| 6-Month Follow Up (N=19) | |||||
| Step 1 | |||||
| IES-R PTSS | 1.30 | 3.33 | −5.80, 8.41 | 0.09 | |
| Gender | −10.37 | 5.66 | −22.43, 1.70 | −0.35+ | |
| Depression | 36.70 | 11.55 | 12.08, 61.32 | 0.77** | 0.59** |
| Step 2 | |||||
| IES-R PTSS | −0.14 | 4.12 | −9.04, 8.76 | −0.01 | |
| Gender | −8.82 | 5.84 | −21.43, 3.80 | −0.30 | |
| Depression | 30.30 | 16.11 | −4.51, 65.11 | 0.63+ | |
| AUD | 4.66 | 7.02 | −10.50, 19.82 | 0.14 | |
| AVC | 4.33 | 3.55 | −3.33, 12.00 | 0.29 | 0.05 |
| Step 3 | |||||
| IES-R PTSS | 2.38 | 3.34 | −4.90, 9.66 | 0.16 | |
| Gender | −10.27 | 4.61 | −20.32, −0.23 | −0.35* | |
| Depression | 19.51 | 13.15 | −9.14, 48.16 | 0.41 | |
| AUD | 0.80 | 5.66 | −11.53, 13.13 | 0.02 | |
| AVC | 0.16 | 3.11 | −6.62, 6.93 | 0.01 | |
| AUD x AVC | 13.07 | 4.34 | 3.62, 22.52 | 0.55* | 0.15* |
CI = confidence interval; AUD = alcohol use disorder history; AVC = avoidance coping; IES_R = Impact of Event Scale-Revised; PTSS = posttraumatic stress symptoms
Gender was coded such a value of 0=male and a value of 1=female
+ p < 0.10, *p < 0.05, **p < 0.01, *** p < 0.001
Figure 2.
Plotted Means Illustrating Moderating Effect of AUD History by Avoidance Coping on 6-Week CAPS PTSS Amongst the BAC ≥ 0.08 Subset of MVA Victims (N =33).
NOTE. AUD (+) = alcohol abuse or dependence history present; AUD (-) = alcohol abuse or dependence history absent; AVC = avoidance coping; CAPS = Clinician-Administered PTSD Scale; PTSS = posttraumatic stress symptoms
Figure 3.
Plotted Means Illustrating Moderating Effect of AUD History by Avoidance Coping on 6-Month CAPS PTSS Amongst the BAC ≥ 0.08 Subset of MVA Victims (N =19).
NOTE. AUD (+) = alcohol abuse or dependence history present; AUD (-) = alcohol abuse or dependence history absent; AVC = avoidance coping; CAPS = Clinician-Administered PTSD Scale; PTSS = posttraumatic stress symptoms
Discussion
Prior research demonstrates that avoidance coping is common in individuals with AUDs and in individuals with PTSD, suggesting that it might be an important variable involved in PTSD+AUD comorbidity. Results from this study were supportive of this hypothesis. Specifically, the relationship between avoidance coping and PTSS was found to be greater for those with a history of alcohol abuse or dependence – relative to those without this history – in a sample of recent MVA victims. Furthermore, this relationship was present after taking into account the influence of several control variables. Thus, a stronger relationship between avoidance coping and PTSS in those with AUD history was observed even after the effects of inhospital PTSS, gender, and depression were removed. This is notable, given that both gender and depression are often strongly related to PTSD (Breslau, Davis, Peterson, & Schultz, 2000; Tolin & Foa, 2006). In addition, by controlling for in-hospital PTSS, the present results suggested that avoidance coping was associated with increased PTSS at subsequent time points over and above those symptoms present in-hospital, particularly in those with an AUD history. In the full sample, this relationship was observed at 6-weeks post-accident, as well as marginally at 6-months at the trend level. Furthermore, this relationship was present at both 6-weeks and 6-months post-accident in the subset of individuals legally intoxicated at the time of the accident.
The present study is consistent with prior research demonstrating the comorbidity of AUDs and PTSD and that a history of prior AUDs may be a risk factor for PTSD (Blanchard et. al., 1996). In addition, results from the present study extend previous research by suggesting that avoidance coping is a common mechanism linking the two disorders. Given the existence of valid, reliable alcohol screeners useful for primary care settings – such as the 4-item CAGE (Ewing, 1984) and the 10-item AUDIT (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) – the present results suggest that screening for alcohol use disorders in recently traumatized MVA victims, combined with an assessment of avoidance coping, may be an effective way to identify individuals at risk of developing PTSD. In addition, given evidence that avoidance coping is associated with both PTSD and alcohol use (Bryant & Harvey, 1995; Cooper et. al., 1992), the development of interventions that target avoidance coping in recently traumatized individuals with AUD may be efficacious in reducing both the use of substances such as alcohol and PTSD risk. Consequently, by targeting avoidance coping in such a manner, both the cost and impairment associated with the co-occurrence of AUD and PTSD may be curtailed.
Interpretation of the present results should be tempered in light of several limitations. First, a greater proportion of males, African Americans, and individuals with higher in-hospital PTSS as assessed by the IES-R were lost to follow-up. This differential attrition may limit the inferences that can be drawn from this study. Thus, it is unclear whether the results obtained generalize more broadly to both males and females, individuals of differing races/ethnicities, as well as individuals with higher levels of initial PTSS. Second, information on participants’ history of prior treatment for alcohol use disorders was not collected. Such information could have been used to determine participants’ alcohol use disorder severity. It is possible that those who have sought treatment in the past may suffer from more severe alcohol use disorders, which may in turn be related to a greater reliance on avoidance coping. Future studies should consider how alcohol use disorder severity may modify the results observed in the present investigation. Finally, the current study was based upon a sample of recent MVA victims who reported moderate levels of AVC and PTSS and may not generalize to more highly traumatized samples or victims of other types of traumatic events. While this may limit the ability to generalize the present results, inclusion of more symptomatic participants may also have strengthened the present results. Nevertheless, future research should seek to determine if the relationship between PTSS and AVC is stronger for those with AUD history using samples of individuals with varying trauma characteristics, and PTSS levels.
Despite these limitations, the results from this study are consistent with the idea that avoidance coping among MVA victims may be differentially related to PTSD depending upon an individual’s AUD history status. Given research suggesting that avoidance coping is associated with both PTSD and AUD, results from the current study suggest that avoidance coping could be associated with increased risk for PTSD following trauma in individuals with AUDs.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Avants SK, Warbuton LA, Margolin A. The influence of coping and depression on abstinence from illicit drug use on methadone-maintained patients. American Journal of Drug and Alcohol Abuse. 2000;26:399–416. doi: 10.1081/ada-100100252. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test. 2. World Health Organization; 2001. [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Long WB. The Injury Severity Score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck JG, Grant DM, Read JP, Clapp JD, Coffey SF, Miller LM, Palyo SA. The Impact of Event Scale-Revised: Psychometric properties in a sample of motor vehicle accident survivors. Journal of Anxiety Disorders. 2008;22:187–198. doi: 10.1016/j.janxdis.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 Structural Equations Program Manual. Encino, CA: Multivariate Software, Inc; 2004. [Google Scholar]
- Belding MA, Iguchi MY, Lamb RJ, Lakin M, Terry R. Coping strategies and continued drug use among methadone maintenance patients. Addictive Behaviors. 1996;21:389–401. doi: 10.1016/0306-4603(95)00069-0. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, Jones-Alexander J. One-year prospective follow-up of motor vehicle accident victims. Behavior Research Therapy. 1996;34:775–786. doi: 10.1016/0005-7967(96)00038-1. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13:206–209. [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection. Biological Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Wolfe J. Substance abuse and post-traumatic stress disorder comorbidity. Drug and Alcohol Dependence. 1994;35:51–59. doi: 10.1016/0376-8716(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors. 1999;13:115–122. [Google Scholar]
- Bryant RA, Harvey AG. Avoidant coping style and post-traumatic stress following motor vehicle accidents. Behaviour Research and Therapy. 1995;33:631–635. doi: 10.1016/0005-7967(94)00093-y. [DOI] [PubMed] [Google Scholar]
- Bustamante V, Mellman TA, David D, Fins AI. Cognitive functioning and the early development of PTSD. Journal of Traumatic Stress. 2001;14:791–797. doi: 10.1023/A:1013050423901. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chemtob C, Roitblat HL, Hamada RS, Carlson JG, Twentyman CT. A cognitive action theory of post-traumatic stress disorder. Journal of Anxiety Disorders. 1988;2:253–275. [Google Scholar]
- Cohen J, Cohen P, Aiken SG, West LS. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3. Mahweh, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Brady KT, Cotton BD. Changes in PTSD symptomatology during acute and protracted alcohol and cocaine abstinence. Drug and Alcohol Dependence. 2007;87:241–248. doi: 10.1016/j.drugalcdep.2006.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Stasiewicz PR, Hughes PM, Brimo ML. Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors. 2006;20:425–435. doi: 10.1037/0893-164X.20.4.425. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Creamer M, Burgess P, Pattison P. Reaction to trauma: A cognitive processing model. Journal of Abnormal Psychology. 1992;101:452–459. doi: 10.1037//0021-843x.101.3.452. [DOI] [PubMed] [Google Scholar]
- Eensoo D, Paaver M, Harro M, Harro J. Predicting drunk driving: Contributions of alcohol use and related problems, traffic behaviour, personality, and platelet monoamine oxidase (MAO) activity. Alcohol & Alcoholism. 2005;40:140–146. doi: 10.1093/alcalc/agh135. [DOI] [PubMed] [Google Scholar]
- Epstein JN, Saunders BE, Kilpatrick DG, Resnick HS. PTSD as a mediator between childhood rape and alcohol use in adult women. Child Abuse & Neglect. 1998;22:223–234. doi: 10.1016/s0145-2134(97)00133-6. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism: The CAGE questionnaire. Journal of the American Medical Association. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO. Treating the Trauma of Rape. New York: Guilford; 1998. [Google Scholar]
- Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behavior Therapy. 1989;20:155–176. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental stat: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology. 2004;51:115–134. [Google Scholar]
- Gómez-Talegón MT, Alvarez FJ. Road traffic accidents among alcohol-dependent patients: The effect of treatment. Accident Analysis and Prevention. 2006;38:201–207. doi: 10.1016/j.aap.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koren D, Norman D, Cohen A, Berman J, Klein EM. Increased PTSD rick with combat-related injury: A matched comparison study of injured and uninjured soldiers experiencing the same combat events. The American Journal of Psychiatry. 2005;162:276–282. doi: 10.1176/appi.ajp.162.2.276. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Kadden RM, Babor TF, Tennen H, Rounsaville BJ. Validity of the SCID in substance abuse patients. Addiction. 1996;91:859–868. [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress. 2008;21:83–90. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]
- Lapham SC, Smith E, C’de Baca J, Chang I, Skipper BJ, Baum G, Hunt WC. Prevalence of psychiatric disorders among persons convicted of driving while impaired. Archives of General Psychiatry. 2001;58:943–949. doi: 10.1001/archpsyc.58.10.943. [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Callan MK. Stress, alcohol-related expectancies and coping preferences: A replication with adolescents of the Cooper et. al. (1992) model. Journal of Studies on Alcohol. 1997;58:644–651. doi: 10.15288/jsa.1997.58.644. [DOI] [PubMed] [Google Scholar]
- Lawrence JW, Fauerbach J, Munster A. Early avoidance of traumatic stimuli predicts chronicity of intrusive thoughts following burn injury. Behaviour Research and Therapy. 1996;34:643–646. doi: 10.1016/0005-7967(96)00019-8. [DOI] [PubMed] [Google Scholar]
- McFall ME, Mackay PW, Donovan DM. Combat-related posttraumatic stress disorder and severity of substance abuse in Vietnam Veterans. Journal of Studies on Alcohol. 1992;53:357–363. doi: 10.15288/jsa.1992.53.357. [DOI] [PubMed] [Google Scholar]
- Mellman TA, David D, Bustamante V, Fins AI, Esposito K. Predictors of post traumatic stress disorder following severe injury. Depression and Anxiety. 2001;14:226–231. doi: 10.1002/da.1071. [DOI] [PubMed] [Google Scholar]
- Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams DB. Treating Alcohol Dependence: A Coping Skills Training Guide. New York: Guilford; 2002. [Google Scholar]
- Moos RH, Brennan PL, Fondacaro MR, Moos BS. Approach and avoidance coping responses among older problem and nonproblem drinkers. Psychology and Aging. 1990;5:31–40. doi: 10.1037//0882-7974.5.1.31. [DOI] [PubMed] [Google Scholar]
- Moos RH, Holahan CJ. Dispositional and contextual perspectives on coping: Toward an integrative framework. Journal of Clinical Psychology. 2003;59:1387–1403. doi: 10.1002/jclp.10229. [DOI] [PubMed] [Google Scholar]
- Murray J, Ehlers A, Mayou RD. Dissociation and post-traumatic stress disorder: Two prospective studies of road traffic accident survivors. British Journal of Psychiatry. 2002;180:363–368. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Gersons PR. The psychobiology of PTSD: Coping with trauma. Psychoneuroendocrinology. 2005;30:974–982. doi: 10.1016/j.psyneuen.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Ahrens C, Moos RH, Finney JW. Posttraumatic stress disorder in substance abuse patients: Relationship to 1-year posttraumatic outcomes. Psychology of Addictive Behaviors. 1997;11:34–47. [Google Scholar]
- Ouimette P, Read J, Brown PJ. Consistency of retrospective reports of DSM-IV criterion A traumatic stressors among substance use disorder patients. Journal of Traumatic Stress. 2005;18:43–51. doi: 10.1002/jts.20009. [DOI] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, Ruggiero KJ, Kilpatrick D. Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour Research and Therapy. 2007;45:2432–2447. doi: 10.1016/j.brat.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riskind JH, Beck AT, Berchick RJ, Brown G, Steer RA. Reliability of DSM III diagnoses for major depression and generalized anxiety disorder using the Structured Clinical Interview for DSM-III. Archives of General Psychiatry. 1987;44:817–820. doi: 10.1001/archpsyc.1987.01800210065010. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Drobes DJ, Coffey SF, Dansky BS, Brady KT, Kilpatrick DG. PTSD symptom severity as a predictor of cue-elicited drug craving in victims of violent crime. Addictive Behaviors. 2003;28:1611–1629. doi: 10.1016/j.addbeh.2003.08.037. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Coffey SF, Stasiewicz PR. Symptom severity, alcohol craving, and age of trauma onset in childhood and adolescent trauma survivors with comorbid alcohol dependence and posttraumatic stress disorder. The American Journal of Addictions. 2006;15:422–425. doi: 10.1080/10550490600996355. [DOI] [PubMed] [Google Scholar]
- Shalev AY. Acute stress reactions in adults. Biological Psychiatry. 2002;51:532–543. doi: 10.1016/s0006-3223(02)01335-5. [DOI] [PubMed] [Google Scholar]
- Skre I, Onstad S, Torgersen S, Kringlen E. High interrelated reliability for the Structured Clinical Interview for DSM-III-R Axis I (SCID-I) Acta Psychiatrica Scandinavica. 1991;84:167–173. doi: 10.1111/j.1600-0447.1991.tb03123.x. [DOI] [PubMed] [Google Scholar]
- SPSS for Windows, Rel. 15.0.0. Chicago: SPSS, Inc; 2006. [Google Scholar]
- Staiger PK, Melville F, Hides L, Kambouropoulos N, Lubman DI. Can emotion-focused coping help explain the link between posttraumatic stress disorder severity and triggers for substance use in young adults? Journal of Substance Abuse Treatment. 2009;36:220–226. doi: 10.1016/j.jsat.2008.05.008. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Pihl RO, Conrod PJ, Dongier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1998;23:797–812. doi: 10.1016/s0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Tate SR, Norman SB, McQuaid JR, Brown SA. Health problems of substance dependent veterans with and those without trauma history. Journal of Substance Abuse Treatment. 2007;33:25–32. doi: 10.1016/j.jsat.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Rosen C, Cavella S, Moos RH, Finney JW, Yesavage J. Coping, symptoms, and functioning outcomes of patients with posttraumatic stress disorder. Journal of Traumatic Stress. 2006;19:799–811. doi: 10.1002/jts.20185. [DOI] [PubMed] [Google Scholar]
- Timko C, Finney JW, Moos RH. The 8-year course of alcohol abuse: Gender differences in social context and coping. Alcoholism: Clinical and Experimental Research. 2005;29:612–621. doi: 10.1097/01.alc.0000158832.07705.22. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress. 2007;20:821–831. doi: 10.1002/jts.20290. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL. Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31:23–37. [Google Scholar]
- Vaiva G, Boss V, Ducrocq F, Fontaine M, Devos P, Brunet A, Laffargue P, Goudemand M, Thomas P. Relationships between posttraumat GABA plasma levels and PTSD at 1-year follow up. American Journal of Psychiatry. 2006;163:1446–1448. doi: 10.1176/ajp.2006.163.8.1446. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD. New York: Guilford Press; 1997. pp. 399–411. [Google Scholar]
- Wong M, Looney E, Michaels J, Palesh O, Koopman C. A preliminary study of peritraumatic dissociation, social support, and coping in relation to posttraumatic stress symptoms for a parent’s cancer. Psycho-Oncology. 2006;15:1093–1098. doi: 10.1002/pon.1041. [DOI] [PubMed] [Google Scholar]