Abstract
Research emanating from the field of developmental science indicates that initial risk factors for substance use disorder can be evident in early childhood. One dominant developmental pathway connecting these initial risk factors with subsequent substance use disorders focuses on the central role of disinhibited or externalizing behaviors. In the current paper, we delineate a second pathway that focuses on problems with emotion regulation associated with internalizing symptomatology. Several studies indicate that internalizing symptoms in early and middle childhood predict substance involvement in adolescents and young adulthood. We describe a risk model that traces the potential developmental markers of this internalizing pathway to substance use disorders and that identifies a population potentially vulnerable to this risk process, namely children of alcoholic parents. We consider the relation between the internalizing pathway and the more widely researched externalizing pathway. We then conclude with a discussion of the implications of this model for prevention efforts. In this manner, we strive for a translational goal, linking our existing understanding of internalizing processes and substance use disorders with our efforts to develop effective prevention programs.
Keywords: Substance Use, Depression, Anxiety, Developmental Pathway, Alcohol
Multiple disciplines contribute to our growing understanding of alcohol and substance use disorders. Within this field, developmental science emphasizes the early etiological processes that contribute to, yet precede, the onset and escalation of alcohol and drug use. Findings guided by this perspective show that alcohol and drug use itself may begin much earlier in development than when onset is typically studied (i.e., mid-childhood versus adolescence; Donovan et al., 2004) and that the roots of these behaviors are likely evident for some individuals in early childhood (Zucker, 2008). These findings have implications for preventive interventions, guiding when these programs may be most effective and identifying the types of developmental processes that these programs may most successfully target (Dunn, Mezzich, Tolan, Szapocznik, & Sambrano, 2007; Ialongo et al., 2006).
Developmental Psychopathology provides a framework for integrating developmental science with the study of how problem behaviors, such as substance use disorders (SUDs), emerge over development (e.g., Cicchetti, Matthysse, Levy, Kagan, & Benes, 1996; Zucker, Cicchetti, & Cohen, 2006). Researchers applying the Developmental Psychopathology framework to the study of SUDs have increasingly emphasized the importance of identifying developmental pathways leading to SUDs. However, few developmental pathways emanating from early childhood, rather than later in development, are currently articulated in the literature.
In the current paper, we review evidence supporting the need to further study one such early emerging pathway, the internalizing pathway to SUDs. We then describe a high-risk population potentially vulnerable to following this pathway, namely children of alcoholic parents. Relying on the tenets of the Developmental Psychopathology framework, we next describe the theoretical processes underlying the internalizing pathway. We consider the relation between the internalizing pathway and the more widely researched externalizing pathway. We then conclude with a discussion of the implications of this model for prevention efforts. In this manner, we strive for a translational goal, linking our existing understanding of internalizing processes and SUDs with our efforts to develop effective prevention programs.
The case for pursuing an internalizing pathway to SUDs
Although developmental pathways emanating from early childhood that lead to SUDs are rarely articulated in the literature, one notable exception is the antisocial or externalizing pathway. The externalizing pathway is posited to first emerge as difficult temperament in infancy which is followed in childhood by externalizing symptoms (e.g., aggression and conduct problems), an early onset of substance use, escalations in antisocial behavior and the eventual onset of SUDs (Tarter et al., 1999; Zucker et al., 2006). The core behavioral problems of this pathway thus typically reflect behavioral disinhibition, “an inability to inhibit socially undesirable or restricted actions” (p. 326, Iacono, Malone, & McGue, 2008). Although multiple factors may propel youth down this trajectory, current models emphasize interactions between an underlying liability for behavioral disinhibition (due to genetic and neurobiological factors) and a high-risk environment (due to the impact of parent antisociality on impaired parenting, disruptive or impoverished contexts, and deviant peer networks) as core to risk formation (e.g., Hussong, Curran, & Chassin, 1998; Zucker et al., 2006).
In support of this pathway, externalizing symptoms are highly correlated with substance use, particularly in adolescence (Hussong et al., 1998; King, Iacono, & McGue, 2004; Steele, Forehand, Armistead, & Brody, 1995). Moreover, recent behavioral genetics studies suggest that externalizing symptoms and substance use share a common genetic diathesis for disinhibited behavior (Iacono, 2008).1 Evidence for other aspects of this theoretical model has also begun to emerge (see Zucker et al., 2006). Thus, the externalizing pathway may well be a dominant pathway of risk for SUDs. This line of research has important implications for prevention, with accumulating evidence showing support for prevention and treatment programs that address deficits or introduce protective factors relevant to the externalizing pathway (e.g., Henggeler, Clingempeel, Brondino, & Pickrel, 2002; Lochman et al., 2007).
Perhaps given the dominance of the externalizing pathway, current research poorly defines alternative developmental pathways emanating from early childhood that lead to subsequent SUDs. This is a clear limitation of the field. As defined within the Developmental Psychopathology framework, the concept of equifinality indicates that many disorders are reached through multiple pathways and children may follow different pathways to reach these similar outcomes (Cicchetti & Rogosch, 1996).
In the case of SUDs, evidence for potential equifinality comes from at least two sources. First, a large body of research documents the salience of individual differences in understanding the etiology of alcoholism (e.g., Cox et al., 2001; Zucker et al., 2006). These differences suggest that various risk processes are differentially relevant across subgroups of individuals. For example, the extent to which alcohol serves to dampen physiological stress responses varies systematically across individuals and is greater among those with a family history of alcoholism (Sher & Walitzer, 1986; Sher, Grekin, & Gross, 2007). These findings indicate that pathways incorporating a physiological vulnerability for using alcohol to manage stress are potentially more salient for children of alcoholic parents than for their peers. A broad array of such risk and protective factors contribute to the development of substance involvement (Hawkins, Catalano, & Miller, 1992). The common finding that individual differences are important in the prediction of adolescent substance use indicates that youth vary in the etiological factors leading to SUDs and thus perhaps in their development pathways to these disorders.
Second, epidemiological data suggest limitations to relying on the externalizing model alone to capture developmental pathways for SUDs. For instance, in the National Epidemiological Study of Alcohol and Related Conditions, approximately 12% of adults meeting criteria for an AUD and 28% of those doing so for a drug use disorder in the past 12-months evidenced antisocial personality disorder, a predicted outcome of long-term deviant behavior associated with the externalizing pathway (Grant, Stinson, Dawson, Chou, Ruan et al., 2006). This represents a 5–12 fold increase in the odds of having an antisocial personality disorder among those with, versus without, a SUD. Nonetheless, less than a third of adults with a SUD show the expected pattern of comorbidity associated with the externalizing pathway. Other developmental pathways are clearly needed to understand additional trajectories leading to substance involvement and disorder.
In models of adult alcoholism, the antisocial form of alcoholism associated with the externalizing pathway is but one of two dominant subtypes of alcoholism that is defined via patterns of comorbidity (Babor, 1996; Zucker et al., 2006). An alternate is Depressive or Negative Affect Alcoholism. The developmental pathway leading to this form of alcoholism remains poorly articulated in the literature. Several factors may underlie this lack of research attention, some of which relate to early conceptualizations of a Depressive Alcoholism subtype (Cloninger, 1987; Cloninger, Sigvardsson, Gilligan, & von Knorring, 1988; Cloninger, Sigvardsson, & Bohman, 1996). For example, Depressive Alcoholism was long considered more common in women than in men and research efforts pertaining to “female alcoholism” have lagged behind those pertaining to “male alcoholism” (Wilsnack & Wilsnack, 1997). Recent studies show elevated rates of negative affect-related disorders (i.e., depression or anxiety) in men with versus men without alcohol use disorders, although comorbidity rates of negative affect and substance use disorders remain higher in women (Kessler, Crum, Warner, & Nelson, 1997). Moreover, Depressive Alcoholism was posited to be of late-onset (Cloninger et al., 1996) and thus not of central interest to studies of adolescents and young adults, the period targeted by most research on the development of SUDs. However, recent findings are inconsistent concerning whether the age of onset for SUDs differentiates Antisocial and Negative Affect SUDs as once supposed (e.g., Epstein, Labouvie, McCrady, Jensen, & Hayaki, 2002; Gratzer et al., 2004; Radouco-Thomas, Boivin, Chabot, & Marquis, 1986).
A primary reason why developmental pathways associated with Negative Affect Alcoholism remain understudied is that associations between depression and SUDs are weaker than are those between antisociality and SUDs. Mood and anxiety disorders (independent of those defined as ‘induced’ by alcohol and drug use) show a 2.8 and 1.9 fold increase, respectively, among adults with (versus without) a 12-month diagnosis of a substance use disorder (Grant, Stinson, Dawson, Chou, Dufour et al., 2006). This results in estimates of between 18 and 20% of adults with a substance use disorder also evidencing a mood or anxiety disorder. This risk is higher for substance dependence (4.2–4.5 fold increase) versus abuse (1.4–1.9), though still more modest than the risk for antisocial personality disorder (8.2 and 18.5 for abuse and dependence, respectively) found in parallel studies with this sample (i.e., NESARC; Grant, Stinson, Dawson, Chou, Dufour et al., 2006). Moreover, studies of adolescents predicting substance use outcomes consistently show a stronger effect of externalizing symptoms as opposed to internalizing symptoms (e.g., Hussong et al., 1998; King et al., 2004). In light of these findings, some researchers question the centrality of depression and negative affect as an explanatory mechanism for SUDs.
Other factors reducing research interests in the role of internalizing, as opposed to externalizing, mechanisms in substance use include challenges associated with measurement. Measures of internalizing symptoms are typically less reliable (particularly at younger ages) and show lower rates of inter-reporter agreement than those targeting externalizing symptoms (De Los Reyes & Kazdin, 2008). In addition, heterogeneity within measures of internalizing symptoms that reflect different forms of affective symptoms may have greater negative repercussions for the study of SUDs than heterogeneity within measures of externalizing symptoms. In general, various forms of externalizing symptoms all serve to increase risk for SUDs (Iacono, Malone, & McGue, 2008b). However, some forms of internalizing symptoms may actually reduce this risk (e.g., separation anxiety in late childhood; Kaplow, Curran, Angold, & Costello, 2001) whereas others may increase it (e.g., depression in adolescence) but only at certain ages (e.g., anxiety in later adolescence, Sung, Erkanli, Angold, & Costello, 2004).
Despite these challenges, pursuit of an internalizing pathway is of keen interest in the study of SUDs for several reasons. First, several studies report prospective prediction of adolescent alcohol involvement from childhood internalizing problems. For example, studies by Zucker and colleagues (Zucker, Chermack, & Curran, 2000) of high-risk youth show effects of internalizing symptoms in children as young as ages 2–5 on substance use in early adolescence. Moreover, community based samples also find that early indicators of internalizing symptoms in early- to mid-childhood (e.g., symptoms of anxiety and depression and inhibited temperament) predict substance involvement into late-adolescence and early adulthood (Caspi et al., 1996; Caspi, Moffitt, Newman, & Silva, 1996; Kellam, Ensminger & Simon, 1980).
Second, clinical studies indicate that self-medication, a key mechanism posited to link affective disruption and substance use, is self-reported in treatment samples as a primary reason for addiction and is commonly targeted by treatment programs (McMahon, Kouzekanani, DeMarco & Kusel, 1992). Third, reformulations of the self-medication model identify vulnerable sub-groups for whom the effect of depression on SUDs is larger than previously found in the population at large. This suggests that the internalizing pathway may be particularly relevant in explaining SUDs for a subset of individuals (Cooper, Russell, Skinner, Frone, & Mudar, 1992; Kushner, Sher, Wood, & Wood, 1994; Kushner et al., 1994). Fourth, comorbidity rates of affective and anxiety disorders with SUDs are among the highest reported with any psychiatric disorder, particularly within treatment settings (Costello, Erkanli, Federman, & Angold, 1999; Merikangas et al., 1998; Skinstad & Swain, 2001). Fifth, evidence for Negative Affect Alcoholism as a subtype is growing, and thus understanding the pathways through which this endpoint is reached and whether this finding generalizes to other SUDs is needed (e.g., Mezzich et al., 1993; Nurnberger, Foroud, Flury, Meyer, & Wiegand, 2002).
And, finally, we believe that understanding an internalizing pathway to SUDs is also important for developing effective preventive interventions. Knowledge about this pathway can inform the development of early intervention and prevention programs for SUDs, targeting youth as early as preschool when risk may be more malleable and intervention more successful. Because most early prevention work focuses on risk associated with externalizing processes, the explication of an internalizing pathway may also suggest novel targets of risk for an early age period. Although we believe that this internalizing pathway will be relevant for understanding processes leading to SUDs in a broad array of adolescents, we also believe that this pathway may be most evident within an established high risk sub-population, namely children of alcoholics.
The salience of parent alcoholism
Children of alcoholic parents (COAs) are among the highest risk groups for evidencing AUDs and other SUDs (e.g., Chassin, Pitts, DeLucia, & Todd, 1999; Sher, 1991). Of increasing research focus are the reasons underlying COAs’ risk for these disorders. In particular, recent efforts have provided the field with a growing understanding of the genetic and neurobiological contributors to AUDs (e.g., Hasin, Hatzenbuehler, & Waxman, 2006; Schuckit, 2000). With respect to Negative Affect Alcoholism in particular, the search for genetic mechanisms remains an active area of study. Currently, family linkage and twin studies demonstrate modest co-transmission for internalizing disorders (primarily depression) and alcoholism (Kendler, Neale, Heath, & Kessler, 1994; Merikangas, Leckman, Prusoff, Pauls, & Weissman, 1985; Zucker et al., 2006).2 In addition, summarizing results from the Collaborative Study on the Genetics of Alcoholism, Nurnberger et al. (2002) reported evidence consistent with examining Negative Affect Alcoholism as a unique phenotype. Specifically, they report a higher rate of comorbid depression and alcoholism among probands of families with a higher prevalence of this same comorbidity as opposed to families with a higher prevalence of alcoholism alone. This finding spurred genetic analyses identifying two markers on chromosome 1 that indicate linkage between alcohol and depression (spectrum) disorders. Together, these findings indicate the potential for some overlap in the genetic diathesis for alcoholism and internalizing disorders. Thus, some COAs may have greater genetic vulnerability for internalizing disorders that is shared with that for alcoholism and this comorbidity may be greatest in children whose parents demonstrate Negative Affect Alcoholism.
However, genetically-informed studies indicate that environmental factors also play a significant role in the development of SUDs and AUDs (e.g., Caspi et al., 2005; Dick et al., 2007; Dick et al., 2007; Rose, Dick, Viken, & Kaprio, 2001). Many of these candidate environmental risk factors are more prevalent among COAs, and these factors likely underlie the broad-based emotional and behavioral impairments more evident in COAs than in their peers. By ages 2–3 and through young adulthood, COAs show greater internalizing and externalizing symptoms than do their peers (Hussong et al., 2007; Hussong, Flora, Curran, Chassin, & Zucker, 2008). COAs also show higher rates of problems in school (e.g., poorer academic performance; McGrath, Watson, & Chassin, 1999) and in their peer relationships (e.g., lower rates of social competence in childhood and greater risk of deviant peer affiliations in adolescence; Chassin, Curran, Hussong, & Colder, 1996; Hussong, Zucker, Wong, Fitzgerald, & Puttler, 2005). Most notably, COAs show a substantially greater risk for alcohol and drug use disorders in young adulthood. COAs initiate substance use earlier, increase their rates of use more quickly, and show a faster escalation from initiation to alcohol use disorders than do children of non-alcoholic parents (Chassin et al., 1996; Chassin et al., 1999; Hussong, Bauer, & Chassin, 2008). By young adulthood, 53% of COAs evidence an AUD as compared to 25% of non-COAs. Moreover, rates of drug, affective, and anxiety disorders are approximately 21, 24 and 25% among COAs compared to 9, 12 and 18% among their peers, respectively (Chassin et al., 1999).
Not surprisingly, these elevated rates of disturbance make COAs a high-service utilization population, with COAs over-represented in mental health and special education services. Notably, nearly 80% of children in families in the child welfare system are affected by substance abuse (Child Welfare League of America, 2004). Recent estimates indicate that 11 percent of all children live in families where one or more parents abuse alcohol or other drugs (Child Welfare League of America, 2004), making COAs both a substantial and multi-risk population deserving of effective preventive interventions. For these reasons, targeting COAs as a vulnerable group is among the top health priorities identified by the Surgeon General in a 2007 call to action to prevent and reduce underage drinking (US DHHS, 2007). Despite this clear need, few empirically evaluated prevention programs target COAs.
The early emergence and stability of emotional and behavioral problems among COAs underscores the utility of a developmental perspective in explaining when and how some of these youth will come to evidence SUDs. Growing evidence suggests that the roots of this process are evident for some individuals as early as birth. This is most evident among those infants who experienced prenatal exposure to alcohol, tobacco or other drugs and the subsequent challenges associated with Fetal Alcohol Effects/Syndrome (Kodituwakku, Kalberg, & May, 2001; Streissguth et al., 2004; Testa, Quigley, & Eiden, 2003).3 However, research shows an early pattern of risk behavior in young children of alcoholic parents who avoided prenatal exposure to substances for their children. For example, analyses of two community samples showed that COAs without prenatal exposure began to evidence elevated internalizing symptoms and externalizing symptoms as early as age 2, with risk for symptomatology remaining high and stable into adulthood (Hussong et al., 2007; Hussong et al., 2008). To date, the few prevention programs that have been empirically evaluated target COAs between middle childhood and adulthood (see Price & Emshoff, 1997), after these emotional and behavioral problems have had years to stabilize.
In the current paper, we describe a developmental model that may guide the creation of prevention programs targeting younger children living with alcoholic parents. We focus this model on risk for the internalizing pathway to SUDs which may be especially salient in children of parents who evidence affective disturbance and alcoholism, either comorbidly at the individual parent level (e.g., in the form of Negative Affect Alcoholism) or as co-occurring risks within the family context (e.g., families where fathers have an AUD and mothers have a Major Depressive Disorder). Although we expect that the processes implicated here that define and explain the internalizing pathway are especially evident in COA families, we posit that these mechanisms are not limited to COA families but may occur more broadly for youth from a variety of family backgrounds.
What might an internalizing pathway look like?
We articulate an internalizing pathway to Negative Affect SUDs that incorporates early antecedents and developmentally-varying markers of progression toward this endpoint. We use the concept of a pathway as defined in the tree metaphor of Sroufe (1990), such that a pathway defines a course of development that is followed by a subgroup of children. Such pathways are not deterministic; we do not expect all children showing early indicators of progress on the internalizing pathway to eventually develop a Negative Affect SUD. Rather, the internalizing pathway includes the potential for moderating influences which serve to propel children along different dividing branches up the tree either toward resilience or toward sustained or increasingly maladaptive behavior. Thus, we expect that children who begin to travel along an internalizing pathway early in life will eventually evidence a wide array of outcomes ranging from normal to abnormal. However, in this paper, we begin with a simple description of one set of adjoining branches through the tree that define a pathway of increasing maladaptation, leading to the eventual development of a Negative Affect SUD.
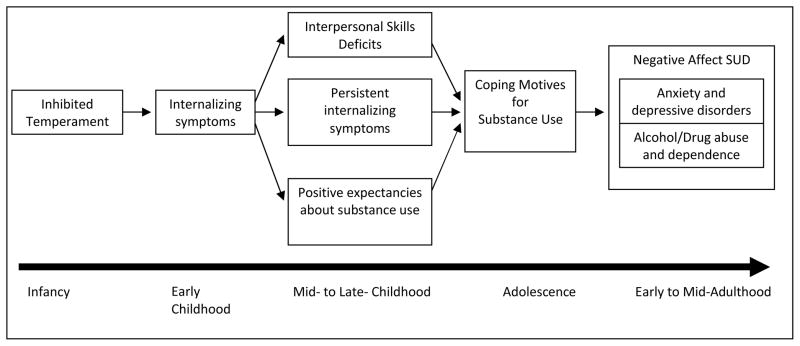
This internalizing pathway consists of an ongoing set of interactions between risk, protective (serving to decrease risk), and vulnerability (serving to increase risk) factors that lead to SUDs. The core of this model is a set of predictions about how risk for Negative Affect SUDs manifests differently at varying ages. These predictions may reflect mediated associations among risk indicators over time but are perhaps better conceptualized as the heterotypic continuity of Negative Affect SUDs. Within the Developmental Psychopathology framework, heterotypic continuity occurs when a single underlying construct is expressed in varying forms across development (Costello, Foley, & Angold, 2006). Evidence for heterotypic continuity in the internalizing pathway to SUDs comes from Costello et al. (2003) who found relatively greater evidence for heterotypic continuity among internalizing disorders and SUDs than among other forms of adolescence disorder. In articulating the potential markers or expressions of Negative Affect SUDs over development below, we emphasize what may be unique indicators of Negative Affect SUDs rather than indicators of SUDs more generally (see Figure 1).
Figure 1.
Internalizing Pathway to Negative Affect Substance Use Disorders
Beginning in infancy
Based on theories of internalizing disorders in young children and developmental formulations of SUDs (Fox, Henderson, Marshall, Nichols, & Ghera, 2005; Kagan, Reznick, & Gibbons, 1989; Rubin & Mills, 1991; Tarter et al., 1999), we posit that this pathway first manifests in infancy as a behaviorally inhibited or highly reactive temperament. Behavioral inhibition has been defined as “a restrained, cautious, avoidant reaction to unfamiliar persons, objects, events, or places” (p. 163; Kagan, 2008) and is considered an enduring, biologically mediated feature of temperament. Previous studies show a consistent link between behavioral inhibition in infancy and increasing internalizing symptoms during childhood (Colder, Mott, & Berman, 2002; Colder, Chassin, Stice, & Curran, 1997). Moreover, observer ratings of child behavior also show greater behavioral inhibition among COAs than among their peers (Hill, Lowers, Locke, Snidman, & Kagan, 1999).4 Findings from observational ratings strengthen this conclusion because they indicate that parents from alcoholic families are not simply over-reporting their children’s behavioral inhibition, as might be hypothesized based on findings of biased parental reports of children behavior associated with other forms of parent psychopathology (e.g., Forehand & McCombs, 1988).
Studies showing that these early temperament markers predict later substance use further support the salience of early behavioral inhibition for the internalizing pathway to SUDs. For example, Ensminger, Juon and Fothergill (2002) found that first grade boys (though not girls) who were both shy and aggressive had higher risk for drug use in adulthood. Similarly, Caspi et al. (1996) found that inhibited (fearful, shy, and easily upset) three-year-olds, compared to their peers, had higher rates of depression and, for boys, alcohol-related problems at age 21. Other studies also demonstrate that indices of internalizing behavior between ages 3 and 10 are predictive of more alcohol-related problems and disorder in mid-adolescence to early adulthood (Hawkins et al., 1992, 1999; Zucker, Fitzgerald et al., 2000; Mayzer et al., 2001, 2002).
Obviously, not all behaviorally inhibited infants will progress toward substance use and eventual disorder. Rather, we expect that progression involves the emergence of internalizing symptoms in the pre-school and early childhood years. Stable behavioral inhibition over time, particularly when paired with physiological indices of fear responses to novel stimuli, increases subsequent risk for internalizing symptoms (particularly anxiety, but also depression) in childhood (Gladstone & Parker, 2006; Hirshfeld, Rosenbaum, Biederman, & Bolduc, 1992; Kagan, Snidman, Zentner, & Peterson, 1999). Moreover, children of depressed parents show greater risk for early behavioral inhibition and internalizing symptoms (Rosenbaum et al., 2000). This same risk for greater internalizing symptoms is also seen in children of depressed (or Negative Affect) alcoholic parents versus children of alcoholic parents without depression and children of non-alcoholic parents (Hussong et al., 2008). Thus, we posit that the early stages of the internalizing pathway to SUDs are marked by behavioral inhibition and emerging internalizing symptoms from infancy into early childhood and we expect that children of parents with Negative Affect SUDs may be particularly vulnerable to this pathway.
Early to mid- childhood
A growing literature identifies the concomitants of internalizing symptoms in early childhood (Rubin & Mills, 1991). Notably, the social reticence accompanying behavioral inhibition in toddlers is associated with risk for peer rejection and self-perceptions of lower social competence in early childhood, particularly in girls (Nelson, Rubin, & Fox, 2005). 5 These temperament and social factors then set the stage for a self-defeating cognitive style about social events that further exacerbates risk for internalizing symptoms and leads to social withdrawal. As such, behaviorally inhibited infants are at a greater risk for internalizing symptoms as toddlers, which in turn increases their risk for social withdraw and other forms of interpersonal skill deficits at the point of school entry.
Many of these concomitants are consistent with early risk markers for eventual substance use in adolescence, particularly those that indicate continued and even escalating problems with emotional and social adjustment. Challenges associated with social interaction may lead children with greater internalizing symptoms over time to become socially rejected and isolated as they progress through the school years (Lillehoj, Trudeau, Spoth, & Wickrama, 2004). Although the relation between social withdraw in early childhood and later substance use has not been directly explored in the literature, peer rejection in the grade school years is associated with later internalizing symptoms in adolescence (Coie, Lochman, Terry, & Hyman, 1992). Moreover, the early emerging socio-cognitive processing style associated with internalizing symptoms and social withdrawal may further entrench and even exacerbate risk for increasing internalizing symptoms through the middle childhood years. Based on these findings, we posit that the early manifestations of the internalizing pathway to SUDs include high behavioral inhibition (in infancy), elevated internalizing symptoms (including both anxiety and depression, emerging with toddlerhood), and subsequent increases in peer rejection, social withdrawal and disengagement (exacerbated at school entry).
Late childhood and adolescence
We expect that development toward Negative Affect SUDs more specifically, rather than SUDs more generally, occurs during late childhood and is marked by three factors namely, positive expectations for the effects of alcohol and drug use, interpersonal skill deficits that lead to associations with deviant peers or to social withdraw and the desire to self-medicate, and coping motives for substance use. The first of these indices thus concerns the growing expectation that alcohol use will reduce distress associated with internalizing symptoms. Although younger children generally endorse more beliefs about the undesirable than positive or enhancing effects of alcohol, this balance of positive to negative beliefs changes both with age and drinking experience (Dunn & Goldman, 1998; O’Connor, Fite, Nowlin, & Colder, 2007). However, even in young children, some youth indicate that they hold such tension reduction or coping expectations for alcohol use even as they enter adolescence (as consistent with evidence in Colder et al., 1997 and Cooper, Frone, Russell, & Mudar, 1995). Such beliefs, as with any positive expectation for drinking, are predictive of greater alcohol use in adolescence (Reese, Chassin, & Molina, 1994). These positive beliefs about drinking are stronger in children of alcoholic fathers (Colder et al., 1997) and may indeed mediate COAs’ risk for substance involvement (Brown, Tate, Vik, Haas, & Aarons, 1999, though also see Colder et al., 1997). Moreover, expectancies and drinking motives are more strongly related to drinking among high school students from alcoholic versus non-alcoholic families (Mann, Chassin, & Sher, 1987). Thus, the development of such positive expectancies for alcohol use, particularly for the reduction of negative affect, are posited to partly mediate the relation between early childhood internalizing symptoms and subsequent risk for alcohol and drug use.
A second factor impacting progression along the internalizing pathway to SUDs during middle childhood and adolescence is interpersonal skill deficits. Specifically, we posit that the extent to which youth act upon their positive expectation about the effects of alcohol and drug use by initiating and escalating substance use is in part driven by their social context. Adolescents who are relatively more withdrawn or disengaged from their peers (perhaps as a function of prolonged internalizing symptoms) may actually initiate substance use somewhat later than their peers. Consistent with this possibility are findings from Kaplow et al. (2001) showing that young teens with a separation anxiety disorder delayed the onset of substance use compared to their peers whereas teens with a generalized anxiety disorder had an earlier onset of substance use. As such, social withdraw may act to delay the onset of substance use into adolescence, given that many opportunities for substance use occur within a peer setting (Hussong, 2000).
Although social withdraw may delay the onset of substance use, it is not likely to decrease the overall risk for substance involvement by late adolescence. Motivated, distressed youth are indeed likely to find avenues for accessing and using substances. This may be particularly true for socially withdrawn COAs who have easier access to alcohol in the home. Consistent with this hypothesis, COAs report drinking alone more frequently than do their peers (Chalder, Elgar, & Bennett, 2006). Adolescents who drink alone may indeed eventually show increased risk for Negative Affect SUDs as drinking alone in adolescence may well be associated with the motive of self-medication, or drinking to relieve stress, and with a greater risk for alcohol-related problems (Cooper, 1994; Cooper, Russell, Skinner, & Windle, 1992).
These effects of social withdraw, however, likely apply only to a minority of our target youth as not all teens with a history of internalizing symptoms will withdraw from their peers. Yet, a history of internalizing symptoms may still leave children progressing along the internalizing pathway with the interpersonal skills deficits that they bring into adolescence. Rather than leading to social withdrawal, these interpersonal deficits may simply steer these youth away from mainstream peer associations, leaving them to find acceptance with more deviant peers. Due to shifting peer contexts, opportunities for social interaction in marginalized groups of peers engaging in deviant behavior provide these socially awkward youth with peer acceptance. At the same time, such groups increase risk for engaging in deviant activities, such as substance use (as articulated by self-derogation theory, Kaplan, 1980 and social context theory, Dishion, Duncan, Eddy, & Fagot, 1994). For most youth, then, we expect to see the onset of substance use by mid-adolescence as social opportunities supportive of use expand and rates of depression are maintained (for boys) or increase (for girls; Angold, Costello, & Goodyer, 2001).
A third factor impacting whether adolescents progress along the internalizing pathway to SUDs is drinking motives. Specifically, adolescents following the internalizing pathway to SUDs may develop strong motives to use substances as a means of coping or reducing tension. Such motives may emerge from earlier coping expectancies for substance use (Kuntsche, Knibbe, Engels, & Gmel, 2007). Three factors may in part impact the strength of these motives. First, coping motives are associated with internalizing symptoms (Rafnsson, Jonsson, & Windle, 2006; Tubman, Wagner, & Langer, 2003) and a long history of internalizing symptoms may underlie these motives in youth traveling the internalizing pathway and seeking to mitigate continued distress. Second, deviant peer groups may also reinforce these motives, given evidence for the social transmission and reinforcement of not only substance use behaviors but also coping motives associated with heavy substance use (Hussong, 2003). And, third, individual differences in the extent to which alcohol actually functions to physiologically reduce tension and stress also may impact this risk. Notably, COAs experience greater reductions than do children of non-alcoholic parents in their physiological stress response when they use alcohol (particularly when they use heavily) versus when they are sober (Sher & Levenson, 1982; Sher et al., 2007). Alcohol, in particular, may then be a more effective short-term coping strategy for COAs and this may in turn increase their coping motives for drinking.
Importantly, such coping motives for drinking predict a more problematic course of substance use in general (Carpenter & Hasin, 1999; Cooper et al., 1995). With progression of the addictive process, affect-related cues for drinking and coping motives may become classically conditioned and part of a sub-conscious process (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). This, in turn, further entrenches the relation between affective and substance use disorders, such that the two become interdependent in a single addictive cycle. Thus, with adolescence, we posit that progression along the internalizing pathway is marked by (a) increasing coping expectancies and motives for substance use, (b) initiation of use either with the goal of self-medication by drinking alone or with the goal of peer acceptance by drinking with deviant peers, and (c) escalation in use to SUDs in adulthood to the point of addiction, particularly for COAs.
Developmental Progression
Collectively, these processes then define an internalizing pathway that emerges at birth and continues, given supportive risk mechanisms, into adulthood. The markers of progression along this pathway emphasize internalizing and affect regulation processes as related, eventually, to SUDs. The manner in which progression occurs along this pathway is then characterized by three concepts from developmental psychopathology. First, many of these risk processes are expected to be bi-directional. For example, increasing experience with alcohol may bolster coping motives in adolescence, particularly for COAs who show greater tension reduction benefits from alcohol as compared to their peers (Sher & Levenson, 1982). The resulting increase in substance use in turn increases negative mood (Hussong, Hicks, Levy, & Curran, 2001), elevating risk for substance-induced depression and both pharmacological (e.g., via withdrawal symptoms) and non-pharmacological influences (e.g., through coping with secondary stressors that are the consequences of use) on affect disturbance (Sher et al., 2007).
Second, these risk processes are also expected to be developmentally cumulative. Thus, by late adolescence, we posit that these youth will show continued internalizing symptoms, poor social functioning, positive expectancies and coping motives for substance use, and moderate to heavy substance use (likely, in part, as a means of self-medication). These adolescent risk factors in turn mediate the relation between temperament and internalizing symptoms in childhood and Negative Affect SUDs in adulthood. With young adulthood, mechanisms underlying dependence and addiction (e.g., Baker et al., 2004) may begin to function as the previously separable behaviors of internalizing symptoms and substance use become fused into a single form of problem behavior. Adolescents showing all of these markers of progression along this pathway are expected to be at greatest risk for Negative Affect SUDs with the transition to adulthood.
Third, we expect that the course (or rate of change) of pathway markers and the overall level of these markers are important in predicting the level of risk that youth face for Negative Affect SUDs. Specifically, we posit that an accelerated progression along this pathway (i.e., faster escalations in internalizing symptoms, earlier onset of substance use, more rapid development of coping motives and expectancies) will interact with overall levels of pathway markers (i.e., high levels of internalizing symptoms, substance use and coping motives and expectancies) to predict greater risk for Negative Affect SUDs.
In sum, we describe an alternative pathway to the more typically studied externalizing model for SUDs that we refer to as the internalizing pathway. In this model, we identify the markers that identify progression along the internalizing pathway ranging from the emergence of behavioral inhibition in infancy and toddlerhood to the development of Negative Affect SUDs in young adulthood. By identifying markers of progression along this pathway, we articulate a model marked by heterotypic continuity in problem manifestation.
The relation between internalizing and externalizing pathways
The internalizing model in Figure 1 describes a pathway of risk that is likely most evident in those children who eventually form a Negative Affect SUDs. However, the processes underlying this pathway are not necessarily restricted to children with this outcome. Rather, we posit that this is a more general risk process that varies in the extent to which it contributes to risk for any form of SUD across individuals. Thus, the emphasis of this model is on the risk mechanism rather than on the specific SUD outcome.
One implication of this assumption is that the externalizing and internalizing pathways are not necessarily orthogonal; rather they define different risk processes leading to SUDs that may at times be overlapping. In other words, emerging risk for SUDs is governed for some children by processes underlying both the internalizing and externalizing pathway and these may indeed be processes that put youth at risk for SUDs more generally rather than Negative Affect SUDs in particular. One example of this overlap comes from research on anger management and aggression in which cognitive-behavioral interventions to manage anger (and increase social problem solving skills) in aggressive boys reduced risk for substance use at one year follow-up (Lochman & Wells, 2003). These risk processes for SUDs are consistent with those acknowledged in the externalizing pathway. Likewise, to the extent that children who have problems with anger management also show problems regulating other forms of emotion (e.g., fear and sadness), the processes relating anger management to subsequent SUDs may also be implicated in the internalizing pathway. Thus, some of the risk processes defining the internalizing and externalizing pathways may at times overlap in the lifecourse of an individual child.
However, this is not to say that the internalizing pathway simply defines a set of risk processes that are subsumed by the externalizing model. Rather, risk processes underlying the internalizing pathway are unique in that the internalizing pathway (a) emphasizes the role of emotion-regulation within the development of self-regulation as central to early risk for SUDs, (b) defines self-medication as a central process translating deficits in self-regulation into substance-related behaviors and risk for addiction specifically, and (c) focuses on the Negative Affect form of SUDs as a salient outcome. With these emphases, the internalizing pathway defines markers of developmental progression along a trajectory identified by these three hallmarks of internalized SUDs (i.e., emotion regulation deficits in early childhood, self-medication with substance use onset typically in adolescence, and the onset of Negative Affect SUDs in early adulthood).
It is important to note that this emphasis on the unique contributions of internalizing processes to SUDs may appear to be in contrast to existing studies in which internalizing symptoms contribute little to the prediction of substance use in adolescence once risk associated with externalizing symptoms is considered (e.g., Hussong et al., 1998). As previously noted, this finding has led some to question the practical importance of internalizing symptoms as an indicator of risk for substance involvement. However, the unique contributions of internalizing and externalizing symptoms may be difficult to detect in adolescence (Serrano, Bauer, Curran, & Hussong, 2008). First, we have found that the unique effects of internalizing symptoms are only apparent at more severe levels of use or for more severe drugs of abuse (Hussong, Curran, Lee et al., 2008; Hussong, Bauer, Serrano, et al., 2008). Second, comorbidity rates of internalizing and externalizing symptoms peak in adolescence as compared with childhood and adulthood, and such high rates of co-occurrence may obscure the unique effects of internalizing symptoms during adolescence. This makes detection of internalizing processes as defined solely by the marker of internalizing symptoms difficult during adolescence. In contrast, we take a developmental perspective that defines the risk associated with internalizing symptoms as a history of behaviors characterized by the internalizing pathway rather than simply rates of internalizing symptoms in adolescence. As such, we posit that internalizing symptoms that onset early and persist into adulthood may be a unique predictor of substance involvement and disorder after controlling for co-occurring externalizing symptoms.
In addition to the possible overlap at times in the processes underlying the internalizing and externalizing pathways, we also recognize the potential for externalizing symptoms themselves to mediate the risk between early internalizing symptoms and substance involvement in adolescence. Several theories account for the development of externalizing symptoms secondary to internalizing symptoms, with the failure to form healthy relationships and deficits in social development serving to increase this comorbidity (Oland & Shaw, 2005). Moreover, both social context theory (Dishion et al., 1994) and the self-derogation model (Kaplan, 1980) suggest that the same social forces posited to propel youth with internalizing symptoms toward substance use (i.e., gaining acceptance but also peer support for deviance in a marginalized peer group) may act to increase deviant behavior more generally. As such, we also predict that for some youth externalizing symptoms may serve as a final common pathway to substance involvement, mediating the relation between childhood internalizing symptoms and substance use in later adolescence (Zucker, 2006). Thus, progression along the internalizing pathway to SUDs does not preclude the presence of externalizing symptomatology, particularly during adolescence. Rather, the internalizing pathway instead emphasizes emotion-based risk processes as underlying the emergence of externalizing symptoms and SUDs.
That said, we also posit that a subgroup of youth engage in SUDs consistent with the internalizing pathway without evidencing processes associated with the externalizing pathway. In fact, the extent to which youth experience internalizing and externalizing related processes for their SUDs likely exists on a continuum, with each set of processes dominant for different youth and perhaps at different points in their individual development. This raises the possibility that externalizing symptoms themselves may serve to moderate risk for substance involvement associated with the internalizing pathway. Negative Affect SUDs specifically may be more evident in youth with ‘pure’ forms of internalizing symptoms because their use is more centrally motivated by coping efforts. Although several studies of adolescents fail to support a moderating hypothesis (Capaldi, 1991; Capaldi & Stoolmiller, 1999; Miller-Johnson, Lochman, Coie, Terry, & Hyman, 1998), others find that internalizing is only predictive of substance use in the absence of externalizing symptoms (Dierker, Vesel, Sledjeski, Costello, & Perrine, 2007). For example, using an experience sampling method assessing daily negative affect and drinking in rising 9th graders over a 21 day period, we found that only those youth low in conduct problems were more likely to drink on days characterized by greater indicators of internalizing symptoms (Hussong, Gould, & Hersh, 2008).
In short, we anticipate that the internalizing pathway is not necessarily orthogonal to processes underlying the development of externalizing symptoms as related to SUDs. Rather, we expect that (a) independent contributions of internalizing and externalizing symptoms may only be evident outside of those developmental periods of high symptom co-occurrence (adolescence), (b) that the internalizing pathway may contribute to the ubiquity of externalizing symptoms during adolescence, with externalizing symptoms serving to mediate the relation between early emerging internalizing symptoms and subsequent SUDs, and (c) that the presence of externalizing symptoms may alter or moderate risk for progression along the internalizing pathway toward eventual Negative Affect SUDs. What distinguishes the internalizing pathway from the externalizing pathway is an emphasis on emotional dysregulation and the emergence of self-medication as the core features of the underlying disorder (i.e., Negative Affect SUDs). Thus, in the internalizing pathway, externalizing symptoms serve to propel or slow progression toward eventual Negative Affect SUDs, a specific form of SUDs with a unique psychological motivational structure and perhaps genetic liability.
What might we learn about prevention efforts based on the internalizing pathway?
Drawing on Rutter (1987), the development of any underlying etiological model may guide the development of effective prevention efforts by identifying those risk and vulnerability factors in need of redress as well as those protective factors that may be bolstered. In addition, we recognize clear prevention implications in our approach to understanding the development of AUDs and SUDs within a developmental framework. Our primary goal was to outline a model allowing us to identify progression of an underlying risk process that is eventually evident as Negative Affect SUDs (i.e., the internalizing pathway, Figure 1). This conceptualization of how internalizing symptoms contribute to the development of Negative Affect SUDs, particularly in COAs, offers a way to identify a target population, period of development for intervention, and risk process ripe for preventive intervention.
First, as in other areas of prevention, one lesson offered by the emerging literature showing that risk for the internalizing pathway emerges early in life is simply that earlier prevention efforts are needed (Ialongo et al., 2006). To date, no prevention programs have been developed and empirically evaluated to determine whether interventions in the preschool-period can effectively mitigate COAs’ risk. In addition to being a period when COAs are first evidencing risk for negative outcomes, the preschool years are an ideal developmental period for intervention because (a) such risk behaviors as aggression may become reinforced and more difficult to change if not addressed prior to school entry when the systemic repercussions of such behaviors may also impact children and (b) the rapid developmental changes that accompany this period offer families multiple opportunities to adapt to the child’s needs and reorganize how they function as a unit.
Second, a clear case can be made that COAs are at particular risk for progression along the internalizing pathway toward Negative Affect SUDs. Although we suspect that children who are exposed to both mood disorders and SUDS through their parents (e.g., a parent with depressed, alcoholism or a family with an alcoholic father and depressed/anxious mother) may be especially at risk for progression along the internalizing pathway, we also expect that the processes outlined here may be relevant for understanding the role of affective processes in risk for SUDs in families with an alcoholic parent more generally.
A third clear implication is that internalizing symptoms may be a useful target for early prevention efforts. Evidence suggests that the relation between parent alcoholism and child internalizing symptoms is weaker than that between parent alcoholism and child externalizing symptoms (Chassin, Rogosch, & Barrera, 1991; Edwards, Leonard, & Das Eiden, 2001). Nonetheless, previous studies consistently support COAs’ greater risk for internalizing symptoms compared to children of non-alcoholic parents, with COAs as young as 18 months showing elevated parent-reports on internalizing symptoms (Colder et al., 1997). Similar results come from studies focusing on early and middle childhood (Puttler, Zucker, Fitzgerald, & Bingham, 1998; Tubman, 1993). Studies by Chassin and colleagues (Chassin et al., 1991; Chassin et al., 1999) show that adolescent COAs have higher maternal reports of internalizing symptoms than their peers, and that this risk continues into young adulthood when COAs show higher rates of affective and anxiety disorders.
Conclusions
Our goal was to define an internalizing pathway to SUDs, particularly Negative Affect SUDs, which is guided by the extant literature and integrated through the tenants underlying the Developmental Psychopathology framework. The internalizing pathway outlines a process of heterotypic continuity to identify the early emergence of a risk process underlying Negative Affect SUDs and to track its progression over development. The pathway holds implications for target populations, periods of development, and risk processes, and thus informs the development of preventive interventions. However, the development of these prevention programs requires a greater degree of specificity than the current model provides. Being able to identify when (the pre-school years), who (children of alcoholic parents) and what distal factors to target (internalizing symptoms), begs the question of what risk processes underlie these target factors and how we might most effectively interrupt them. These needs define a research agenda that connects our understanding of broad developmental pathways leading to psychopathology with the demands of early preventive programs designed to alter the lifecourse of children at risk for following such detrimental pathways.
Footnotes
Despite the dominant trend to thus conceptualize all SUDs as part of a disinhibited phenotype linked to a single common genetic liability, other research has suggested that genetic structures related to risk for SUDs may vary depending on the form (use versus disorder), developmental timing (adolescence versus adulthood) and trajectory (stable prolonged use over adolescence versus deceleration; e.g., Dick, 2008) of the use. Thus defining the informative phenotypes of SUDs for identifying genetic liability remains an active area of research and the role of Negative Affect forms of SUDs, later defined, as potentially unique remains an active question of study.
See endnote 1 for comment on genetic liability and Negative Affect SUDs.
Note that we focus on mechanisms that do not require fetal alcohol exposure or effects and we generally do not consider the special circumstances of children with these disorders in this manuscript.
These parents also rate their children as more stubborn/persistent in their temperaments as well as externalizing symptoms (Edwards, Leonard, & Eiden, 2001).
The study of gender differences in the relations among internalizing symptoms, stress and substance involvement is a large and contradictory literature. Although we recognize the potential salience of gender differences within the internalizing pathway to SUDs that we posit here, we also recognize that integrating and applying this literature within the current model is beyond the scope of our paper.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb.
References
- Angold A, Costello EJ, Goodyer IM. The depressed child and adolescent. 2. New York, NY US: Cambridge University Press; 2001. The epidemiology of depression in children and adolescents; pp. 143–178. [Google Scholar]
- Babor TF. The classification of alcoholics: Typology theories from the 19th century to the present. Alcohol Health & Research World. 1996;20(1):6–17. [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111(1):33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tate SR, Vik PW, Haas AL, Aarons GA. Modeling of alcohol use mediates the effect of family history of alcoholism on adolescent alcohol expectancies. Experimental and Clinical Psychopharmacology. 1999;7(1):20–27. doi: 10.1037//1064-1297.7.1.20. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: I. familial factors and general adjustment at grade 6. Development and Psychopathology. 1991;3:277–300. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. prediction to young-adult adjustment. Development and Psychopathology. 1999;11(1):59–84. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS. Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal of Studies on Alcohol. 1999;60:694–704. doi: 10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: Longitudinal evidence of a gene X environment interaction. Biological Psychiatry. 2005;57(10):1117–1127. doi: 10.1016/j.biopsych.2005.01.026. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53(11):1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Chalder M, Elgar FJ, Bennett P. Drinking and motivations to drink among adolescent children of parents with alcohol problems. Alcohol and Alcoholism. 2006;41(1):107–113. doi: 10.1093/alcalc/agh215. [DOI] [PubMed] [Google Scholar]
- Chassin L, Curran PJ, Hussong AM, Colder CR. The relation of parent alcoholism to adolescent substance use: A longitudinal follow-up study. Journal of Abnormal Psychology. 1996;105(1):70–80. doi: 10.1037//0021-843x.105.1.70. [DOI] [PubMed] [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100(4):449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108(1):106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Child Welfare League of America. Substance abuse, families, and recovery. Report. 2004. 2004 children’s legislative agenda. [Google Scholar]
- Cicchetti D, Matthysse S, Levy DL, Kagan J, Benes FM. Psychopathology: The evolving science of mental disorder. New York, NY US: Cambridge University Press; 1996. Developmental theory: Lessons from the study of risk and psychopathology; pp. 253–284. [Google Scholar]
- Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Development and Psychopathology. 1996;8(4):597–600. [Google Scholar]
- Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236(4800):410–416. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Sigvardsson S, Bohman M. Type I and type II alcoholism: An update. Alcohol Health & Research World. 1996;20(1):18–23. [PMC free article] [PubMed] [Google Scholar]
- Cloninger CR, Sigvardsson S, Gilligan SB, von Knorring A. Genetic heterogeneity and the classification of alcoholism. Advances in Alcohol & Substance Abuse. 1988;7(3):3–16. doi: 10.1300/J251v07n03_02. [DOI] [PubMed] [Google Scholar]
- Coie JD, Lochman JE, Terry R, Hyman C. Predicting early adolescent disorder from childhood aggression and peer rejection. Journal of Consulting & Clinical Psychology. 1992;60(5):783–792. doi: 10.1037//0022-006x.60.5.783. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L, Stice EM, Curran PJ. Alcohol expectancies as potential mediators of parent alcoholism effects on the development of adolescent heavy drinking. Journal of Research on Adolescence. 1997;7(4):349–374. [Google Scholar]
- Colder CR, Mott JA, Berman AS. The interactive effects of infant activity level and fear on growth trajectories of early childhood behavior problems. Development and Psychopathology. 2002;14(1):1–23. doi: 10.1017/s0954579402001013. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6(2):117–128. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions - a motivational model of alcohol-use. 1995. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101(1):139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4(2):123–132. [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: Effects of timing and sex. Journal of Clinical Child Psychology. 1999;28(3):298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Foley DL, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(1):8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Cox WM, Yeates GN, Gilligan PAT, Hosier SG, Heather N, Peters TJ, et al. International handbook of alcohol dependence and problems. New York, NY US: John Wiley & Sons Ltd; 2001. Individual differences; pp. 357–374. [Google Scholar]
- De Los Reyes A, Kazdin AE. When the evidence says, ‘yes, no, and maybe so’: Attending to and interpreting inconsistent findings among evidence-based interventions. Current Directions in Psychological Science. 2008;17(1):47–51. doi: 10.1111/j.1467-8721.2008.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick D. Gene environment interplay in the development of alcohol problems: From twins studies to GWAS and back. A presentation at the Carolina Consortium on Human Development at the University of North Carolina; Chapel Hill. 2008. Nov, [Google Scholar]
- Dick DM, Pagan JL, Viken R, Purcell S, Kaprio J, Pulkkinen L, et al. Changing environmental influences on substance use across development. Twin Research and Human Genetics. 2007;10(2):315–326. doi: 10.1375/twin.10.2.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierker LC, Vesel F, Sledjeski EM, Costello D, Perrine N. Testing the dual pathway hypothesis to substance use in adolescence and young adulthood. Drug and Alcohol Dependence. 2007;87(1):83–93. doi: 10.1016/j.drugalcdep.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Duncan TE, Eddy JM, Fagot BI. The world of parents and peers: Coercive exchanges and children’s social adaptation. Social Development. 1994;3(3):255–268. [Google Scholar]
- Donovan JE, Leech SL, Zucker RA, Loveland-Cherry CJ, Jester JM, Fitzgerald HE, et al. Really underage drinkers: Alcohol use among elementary students. Alcoholism: Clinical and Experimental Research. 2004;28(2):341–349. doi: 10.1097/01.alc.0000113922.77569.4e. [DOI] [PubMed] [Google Scholar]
- Dunn ME, Goldman MS. Age and drinking-related differences in the memory organization of alcohol expectancies in 3rd-, 6th-, 9th-, and 12th-grade children. J Consult Clin Psychol. 1998;66(3):579–85. doi: 10.1037//0022-006x.66.3.579. [DOI] [PubMed] [Google Scholar]
- Dunn MG, Mezzich AC, Tolan P, Szapocznik J, Sambrano S. Preventing youth substance abuse: Science-based programs for children and adolescents. Washington, DC US: American Psychological Association; 2007. Development in childhood and adolescence: Implications for prevention research and practice; pp. 21–40. [Google Scholar]
- Edwards EP, Leonard KE, Das Eiden R. Temperament and behavioral problems among infants in alcoholic families. Infant Mental Health Journal. 2001;22(3):374–392. doi: 10.1002/imhj.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensminger ME, Juon HS, Fothergill KE. Childhood and adolescent antecedents of substance use in adulthood. Addiction. 2002;97(7):833–844. doi: 10.1046/j.1360-0443.2002.00138.x. [DOI] [PubMed] [Google Scholar]
- Epstein EE, Labouvie E, McCrady BS, Jensen NK, Hayaki J. A multi-site study of alcohol subtypes: Classification and overlap of unidimensional and multidimensional typologies. Addiction. 2002;97(8):1041–1053. doi: 10.1046/j.1360-0443.2002.00164.x. [DOI] [PubMed] [Google Scholar]
- Forehand R, McCombs A. Unraveling the antecedent-consequence conditions in maternal depression and adolescent functioning. Behaviour Research and Therapy. 1988;26(5):399–405. doi: 10.1016/0005-7967(88)90073-3. [DOI] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: Linking biology and behavior within a developmental framework. Annual Review of Psychology. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- Gladstone GL, Parker GB. Is behavioral inhibition a risk factor for depression? Journal of Affective Disorders. 2006;95(1):85–94. doi: 10.1016/j.jad.2006.04.015. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Alcohol Research & Health. 2006;29(2):107–120. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the united states: Results from the national epidemiologic survey on alcohol and related conditions. Alcohol Research & Health. 2006;29(2):121–130. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Gratzer D, Levitan RD, Sheldon T, Toneatto T, Rector NA, Goering P. Lifetime rates of alcoholism in adults with anxiety, depression, or co-morbid depression/anxiety: A community survey of ontario. Journal of Affective Disorders. 2004;79(1):209–215. doi: 10.1016/S0165-0327(02)00355-5. [DOI] [PubMed] [Google Scholar]
- Hasin D, Hatzenbuehler M, Waxman R. Genetics of substance use disorders. In: Miller WR, Carroll KM, Miller WR, Carroll KM, editors. Rethinking substance abuse: What the science shows, and what we should do about it. New York, NY US: Guilford Press; 2006. pp. 61–77. [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Kosterman R, Abbott R, Hill KG. Preventing adolescent health-risk behaviors by strengthening protection during childhood. Archives of Pediatrics and Adolescent Medicine. 1999;153:226–234. doi: 10.1001/archpedi.153.3.226. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Clingempeel WG, Brondino MJ, Pickrel SG. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(7):868–874. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- Hill SY, Lowers L, Locke J, Snidman N, Kagan J. Behavioral inhibition in children from families at high risk for developing alcoholism. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(4):410–420. doi: 10.1097/00004583-199904000-00013. [DOI] [PubMed] [Google Scholar]
- Hirshfeld DR, Rosenbaum JF, Biederman J, Bolduc EA. Stable behavioral inhibition and its association with anxiety disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31(1):103–111. doi: 10.1097/00004583-199201000-00016. [DOI] [PubMed] [Google Scholar]
- Hussong AH. The settings of adolescent alcohol and drug use. Journal of Youth and Adolescence. 2000;29(1):107–119. [Google Scholar]
- Hussong AM. Social influences in motivated drinking among college students. Psychology of Addictive Behaviors. 2003;17(2):142–150. doi: 10.1037/0893-164x.17.2.142. [DOI] [PubMed] [Google Scholar]
- Hussong A, Bauer D, Chassin L. Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. Journal of Abnormal Psychology. 2008;117(1):63–78. doi: 10.1037/0021-843X.117.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Bauer D, Serrano D, Curran PJ, Chassin L, Sher KJ, Zucker RA. Externalizing, not internalizing, symptoms identifies periods and persons at risk for alcohol use in high-risk family contexts: A cross-study analysis. A poster presented at the annual meeting for the Research Society on Alcoholism; Washington, DC. 2008. Jul, [Google Scholar]
- Hussong AM, Curran PJ, Chassin L. Pathways of risk for accelerated heavy alcohol use among adolescent children of alcoholic parents. Journal of Abnormal Child Psychology. 1998;26(6):453–466. doi: 10.1023/a:1022699701996. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Curran PJ, Lee T, Wirth RJ, Chassin LA, Sher KJ, Zucker RA. Symptomatology Identifies Periods and Persons at Risk for Illicit Drug Use in High-Risk Family Contexts: A Cross-Study Analysis. A poster presented at the annual meeting for the Society for Prevention Research; San Francisco, CA. 2008. May, [Google Scholar]
- Hussong AM, Flora DB, Curran PJ, Chassin LA, Zucker RA. Defining risk heterogeneity for internalizing symptoms among children of alcoholic parents. Development and Psychopathology. 2008;20(1):165–193. doi: 10.1017/S0954579408000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Gould LF, Hersh MA. Conduct problems moderate self-medication and mood-related drinking consequences in adolescents. Journal of Studies on Alcohol and Drugs. 2008;69(2):296–307. doi: 10.15288/jsad.2008.69.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology. 2001;110(3):449–461. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Zucker RA, Wong MM, Fitzgerald HE, Puttler LI. Social competence in children of alcoholic parents over time. Developmental Psychology. 2005;41(5):747–759. doi: 10.1037/0012-1649.41.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: Entry points for an antisocial pathway to alcoholism. Journal of Abnormal Psychology. 2007;116(3):529–542. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:325. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Ialongo NS, Rogosch FA, Cicchetti D, Toth SL, Buckley J, Petras H, Neiderhiser J. A developmental psychopathology approach to the prevention of mental health disorders. In: Cicchetti D, Cohen D, editors. Developmental psychopathology, vol 1: Theory and method. 2. Hoboken, NJ US: John Wiley & Sons Inc; 2006. pp. 968–1018. [Google Scholar]
- Kagan J. Behavioral inhibition as a risk factor for psychopathology. In: Beauchaine TP, Hinshaw SP, Beauchaine TP, Hinshaw SP, editors. Child and adolescent psychopathology. Hoboken, NJ US: John Wiley & Sons Inc; 2008. pp. 157–179. [Google Scholar]
- Kagan J, Reznick JS, Gibbons J. Inhibited and uninhibited types of children. Child Development. 1989;60(4):838–845. [PubMed] [Google Scholar]
- Kagan J, Snidman N, Zentner M, Peterson E. Infant temperament and anxious symptoms in school age children. Development and Psychopathology. 1999;11(2):209–224. doi: 10.1017/s0954579499002023. [DOI] [PubMed] [Google Scholar]
- Kaplan HB. Deviant behavior in defense of self. New York: Academic Press; 1980. [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. Journal of Clinical Child Psychology. 2001;30(3):316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kellam SG, Ensminger ME, Simon MB. Mental health in first grade and teenage drug, alcohol, and cigarette use. Drug and Alcohol Dependence. 1980;5:273–304. doi: 10.1016/0376-8716(80)90003-4. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Heath AC, Kessler RC. A twin-family study of alcoholism in women. American Journal of Psychiatry. 1994;151(5):707–715. doi: 10.1176/ajp.151.5.707. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the national comorbidity survey. Archives of General Psychiatry. 1997;54(4):313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99(12):1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kodituwakku PW, Kalberg W, May PA. The effects of prenatal alcohol exposure on executive functioning. Alcohol Research & Health. 2001;25(3):192–198. [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, Gmel G. Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. Journal of Studies on Alcohol and Drugs. 2007;68(1):76–85. doi: 10.15288/jsad.2007.68.76. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Wood MD, Wood PK. Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research. 1994;18(4):852–860. doi: 10.1111/j.1530-0277.1994.tb00050.x. [DOI] [PubMed] [Google Scholar]
- Lillehoj CJ, Trudeau L, Spoth R, Wickrama KAS. Internalizing, social competence, and substance initiation: Influence of gender moderation and a preventive intervention. Substance use & Misuse. 2004;39(6):963–991. doi: 10.1081/ja-120030895. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Wells KC. Effectiveness of the coping power program and of classroom intervention with aggressive children: Outcomes at a 1-year follow-up. Behavior Therapy. 2003;34(4):493–515. [Google Scholar]
- Lochman JE, Wells KC, Murray M, Tolan P, Szapocznik J, Sambrano S. Preventing youth substance abuse: Science-based programs for children and adolescents. Washington, DC US: American Psychological Association; 2007. The coping power program: Preventive intervention at the middle school transition; pp. 185–210. [Google Scholar]
- Mann LM, Chassin L, Sher KJ. Alcohol expectancies and the risk for alcoholism. Journal of Consulting & Clinical Psychology. 1987;55(3):411–417. doi: 10.1037//0022-006x.55.3.411. [DOI] [PubMed] [Google Scholar]
- Mayzer R, PUttler LI, Wong MM, Fitzgerald HE, Zucker RA. Predicting early onset of first alcohol use from behavior problem indicators in early childhood. Alcoholism: Clinical and Experimental Research. 2002;26(Suppl):124A. [Google Scholar]
- McGrath CE, Watson AL, Chassin L. Academic achievement in adolescent children of alcoholics. Journal of Studies on Alcohol. 1999;60:18–26. doi: 10.15288/jsa.1999.60.18. [DOI] [PubMed] [Google Scholar]
- McMahon RC, Kouzekanani K, DeMarco LA, Kusel SJ. Cognitive motivations for drinking among alcoholics: Factor structure and correlates. American Journal of Drug and Alcohol Abuse. 1992;18:477–487. doi: 10.3109/00952999209051043. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Leckman JF, Prusoff BA, Pauls DL, Weissman MM. Familial transmission of depression and alcoholism. Archives of General Psychiatry. 1985;42(4):367–372. doi: 10.1001/archpsyc.1985.01790270057006. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Auilar-Gaziola S, et al. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the international consortium in psychiatric epidemiology. Addictive Behaviors. 1998;23(6):893–908. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Mezzich A, Tarter R, Kirisci L, Clark D, Buckstein O, Martin C. Subtypes of early age onset alcoholism. Alcoholism: Clinical & Experimental Research. 1993;17(4):767–770. doi: 10.1111/j.1530-0277.1993.tb00838.x. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: Substance use outcomes across adolescence. Journal of Abnormal Child Psychology. 1998;26(3):221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Nelson LJ, Rubin KH, Fox NA. Social withdrawal, observed peer acceptance, and the development of self-perceptions in children ages 4 to 7 years. Early Childhood Research Quarterly. 2005;20(2):185–200. [Google Scholar]
- Nurnberger JIJ, Foroud T, Flury L, Meyer ET, Wiegand R. Is there a genetic relationship between alcoholism and depression? Alcohol Research & Health. 2002;26(3):233–234. [PMC free article] [PubMed] [Google Scholar]
- O’Connor RM, Fite PJ, Nowlin PR, Colder CR. Children’s beliefs about substance use: An examination of age differences in implicit and explicit cognitive precursors of substance use initiation. Psychology of Addictive Behaviors. 2007;21(4):525–533. doi: 10.1037/0893-164X.21.4.525. [DOI] [PubMed] [Google Scholar]
- Oland AA, Shaw DS. Pure versus co-occurring externalizing and internalizing symptoms in children: The potential role of socio-developmental milestones. Clinical Child and Family Psychology Review. 2005;8(4):247–270. doi: 10.1007/s10567-005-8808-z. [DOI] [PubMed] [Google Scholar]
- Price AW, Emshoff JG. Breaking the cycle of addiction: Prevention and intervention with children of alcoholics. Alcohol Health & Research World. 1997;21(3):241–246. [PMC free article] [PubMed] [Google Scholar]
- Puttler LI, Zucker RA, Fitzgerald HE, Bingham CR. Behavioral outcomes among children of alcoholics during the early and middle childhood years: Familial subtype variations. Alcoholism: Clinical and Experimental Research. 1998;22(9):1962–1972. [PubMed] [Google Scholar]
- Radouco-Thomas S, Boivin D, Chabot F, Marquis P. Nosology and diagnosis of alcoholism, issues and perspectives in subtyping (DSM III) simple alcoholism and alcoholism associated with other psychopathologies. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 1986;10(2):129–134. doi: 10.1016/0278-5846(86)90066-7. [DOI] [PubMed] [Google Scholar]
- Rafnsson FD, Jonsson FH, Windle M. Coping strategies, stressful life events, problem behaviors, and depressed affect. Anxiety, Stress & Coping: An International Journal. 2006;19(3):241–257. [Google Scholar]
- Reese FL, Chassin L, Molina BS. Alcohol expectancies in early adolescents: Predicting drinking behavior from alcohol expectancies and parental alcoholism. J Stud Alcohol. 1994;55(3):276–284. doi: 10.15288/jsa.1994.55.276. [DOI] [PubMed] [Google Scholar]
- Rose RJ, Dick DM, Viken RJ, Kaprio J. Gene-environment interaction in patterns of adolescent drinking: Regional residency moderates longitudinal influences on alcohol use. Alcoholism: Clinical and Experimental Research. 2001;25(5):637–643. [PubMed] [Google Scholar]
- Rosenbaum J, Biederman J, Hirshfeld-Becker D, Kagan J, Snidman N, Friedman D, et al. A controlled study of behavioral inhibition in children of parents with panic disorder and depression. American Journal of Psychiatry. 2000;157(12):2002–2010. doi: 10.1176/appi.ajp.157.12.2002. [DOI] [PubMed] [Google Scholar]
- Rubin KH, Mills RS. Conceptualizing developmental pathways to internalizing disorders in childhood. Canadian Journal of Behavioural Science/Revue Canadienne Des Sciences Du Comportement. 1991;23(3):300–317. [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57(3):316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Schuckit MC. Genetics of the risk for alcoholism. The American Journal on Addictions. 2000;9(2):103–112. doi: 10.1080/10550490050173172. [DOI] [PubMed] [Google Scholar]
- Serrano D, Bauer DJ, Curran PJ, Hussong AM. Prediction of alcohol use trajectories by internalizing and externalizing behavior: simultaneous analysis of three longitudinal studies via the generalized linear mixed model. A poster presented at the Inaugural Meeting of the UNC-Duke Conference on Development and Psychopathology; Chapel Hill, NC. 2008. Feb, [Google Scholar]
- Sher KJ. Children of alcoholics: A critical appraisal of theory and research. Chicago, IL, US: University of Chicago Press; 1991. [Google Scholar]
- Sher KJ, Grekin ER, Gross JJ. Handbook of emotion regulation. New York, NY US: Guilford Press; 2007. Alcohol and affect regulation; pp. 560–580. [Google Scholar]
- Sher KJ, Levenson RW. Risk for alcoholism and individual differences in the stress-response-dampening effect of alcohol. Journal of Abnormal Psychology. 1982;91(5):350–367. doi: 10.1037//0021-843x.91.5.350. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS. Individual differences in the stress-response-dampening effect of alcohol: A dose-response study. Journal of Abnormal Psychology. 1986;95(2):159–167. doi: 10.1037//0021-843x.95.2.159. [DOI] [PubMed] [Google Scholar]
- Skinstad AH, Swain A. Comorbidity in a clinical sample of substance abusers. American Journal of Drug and Alcohol Abuse. 2001;27(1):45–64. doi: 10.1081/ada-100103118. [DOI] [PubMed] [Google Scholar]
- Sroufe A. Considering normal and abnormal together: The essence of developmental psychopathology. Development and Psychopathology. 1990;2:335–347. [Google Scholar]
- Steele RG, Forehand R, Armistead L, Brody G. Predicting alcohol and drug use in early adulthood: The role of internalizing and externalizing behavior problems in early adolescence. American Journal of Orthopsychiatry. 1995;65(3):380–388. doi: 10.1037/h0079694. [DOI] [PubMed] [Google Scholar]
- Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O’Malley K, Young JK. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of Developmental & Behavioral Pediatrics. 2004;25(4):228–238. doi: 10.1097/00004703-200408000-00002. [DOI] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug and Alcohol Dependence. 2004;75(3):287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Vanyukov M, Giancola P, Dawes M, Blackson T, Mezzich A, et al. Etiology of early age onset substance use disorder: A maturational perspective. Development and Psychopathology. 1999;11(4):657–683. doi: 10.1017/s0954579499002266. [DOI] [PubMed] [Google Scholar]
- Testa M, Quigley BM, Eiden RD. The effects of prenatal alcohol exposure on infant mental development: A meta-analytical review. Alcohol and Alcoholism. 2003;38(4):295–304. doi: 10.1093/alcalc/agg087. [DOI] [PubMed] [Google Scholar]
- Tubman JG, Wagner EF, Langer LM. Patterns of depressive symptoms, drinking motives, and sexual behavior among substance abusing adolescents: Implications for health risk. Journal of Child & Adolescent Substance Abuse. 2003;13(1):37–57. [Google Scholar]
- U. S. Department of Health and Human Services. The surgeon general’s call to action to prevent and reduce underage drinking. 2007. [PubMed] [Google Scholar]
- Wilsnack RW, Wilsnack SC. In: Gender and alcohol: Individual and social perspectives. Wilsnack RW, Wilsnack SC, Wilsnack RW, Wilsnack SC, editors. Piscataway, NJ US: Rutgers Center of Alcohol Studies; 1997. [Google Scholar]
- Zucker RA. Anticipating problem alcohol use developmentally from childhood into middle adulthood: What have we learned? Addiction. 2008;103:100–108. doi: 10.1111/j.1360-0443.2008.02179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Chermack ST, Curran GM. Alcoholism: A life span perspective on etiology and course. In: Sameroff A, Lewis M, Miller S, editors. Handbook of developmental psychopathology. 2. New York: Plenum Press; 2000. pp. 569–587. [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen D, editors. Developmental psychopathology, vol 3: Risk, disorder, and adaptation. 2. Hoboken, NJ US: John Wiley & Sons Inc; 2006. pp. 620–656. [Google Scholar]