Abstract
Background and Purpose
Individuals with critical illness experience dysfunction of many body systems including the neuromuscular system. Neuromuscular impairments result in a syndrome referred to as ICU-acquired weakness which may lead to difficulty with activities and participation. The purposes of this case series were to 1) describe safety and feasibility of physical intervention in individuals with ICU acquired weakness mechanically ventilated for at least 7 days; and 2) characterize physical therapist management and patient outcomes.
Case Description
Nineteen patients with ICU-acquired weakness who required mechanical ventilation for at least 7 days were enrolled over a 1-year period.
Intervention
Physical therapy (PT) was provided 5 day/wk for 30 minutes per session.
Outcomes
Outcome measures included manual muscle tests and item scores from the Functional Independence Measure (FIM). Participants completed 170 PT sessions. Only 20 sessions (12%) were stopped before 30 minutes. Seventeen participants survived to discharge; no PT-related adverse events occurred. At discharge, participants who went home showed a trend toward greater independence and strength compared to those who were discharged to another level of care. Median total hospital days was 28 for those discharged to home and 22 for those discharged to other level of care.
Discussion
This case series demonstrates safety and feasibility of PT intervention for patients with ICU-acquired weakness requiring mechanical ventilation for at least 7 days. The examination and intervention procedures are described and could be implemented with other similar individuals in the hospital setting. Future studies should investigate frequency and duration of physical intervention, both during hospitalization and post discharge.
Keywords: ICU-Acquired weakness, Physical Therapy
Introduction
Patients with critical illness often experience multi-organ dysfunction or failure, with the respiratory, renal, and cardiovascular systems affected most frequently. Because damage to these systems can be acutely life threatening, initial medical management has focused on stabilizing and remediating these body systems. To effectively manage critically ill patients, mechanical ventilation, vasopressive agents, and hemodialysis are frequently utilized. These interventions may limit patients' mobility and therefore their function. Impairments of the neuromuscular system can occur resulting in an under-recognized syndrome referred to as ICU-acquired weakness.1,2 Early detection and physical intervention may reduce the long-term consequences of ICU-acquired weakness with respect to activities and participation. 3-6
In survivors of critical illness, impairments of body systems other than the neuromuscular system typically improve prior to hospital discharge and approach predicted values by 6 months.7,8 In contrast, neuromuscular recovery takes longer and may be incomplete, even up to five years after hospitalization.7,9-12 Therefore, therapies are needed that can reduce the functional impact of neuromuscular morbidity.13 Physical interventions may be important in two ways: first through remediation of neuromuscular impairments during the recovery process and second, by reducing sequelae associated with deconditioning.
Three studies have reported the safety and feasibility of early mobility and physical therapy (PT) treatment of critically ill patients who required mechanical ventilation (MV).4,5,14 Bailey et al14 demonstrated feasibility of a protocol for treatment of patients in a respiratory ICU, including aggressive mobilization twice daily. These investigators conducted 1,449 sessions with 103 patients with fewer than 1% activity-related adverse events. Morris et al4 reported on patients who were enrolled within 48 hours of MV. These authors compared a protocol of PT 7 days per week versus standard of care (characterized as PROM and positioning initiated by nursing staff with a physical therapist consult as appropriate). Compared with the standard of care group, participants in the experimental protocol group were out of bed earlier, had more frequent physical therapy, and had similar complication rates. Schweickert et al5 compared a protocol consisting of early physical and/or occupational therapy plus early sedation withdrawal to standard of care for that facility. Physical therapy standard of care in the two participating facilities consisted of a physical therapist consult when the patient was deemed medically stable by the physician. Typically, this occurred after two weeks on MV. Significantly more of the participants in the experimental group returned to independent function compared with the control group (59% versus 35%; p = 0.02). Findings from all three studies support the benefits and safety of early physical intervention with critically ill individuals. However, these studies included individuals with a variety of diagnoses and time on MV, utilized different intervention approaches, and included a variety of outcome measures, some of which focused primarily on disease process and others on function;4,5,14 none of these studies fully described the PT protocols and the patients' functional outcomes. Hence, the available evidence is not sufficient to guide physical therapist intervention for acutely ill individuals in the ICU.
The purposes of this case series were to 1) describe safety and feasibility of participation in physical therapy intervention for individuals with ICU-acquired weakness who required MV for at least 7 days, and 2) characterize the examination and intervention procedures with sufficient detail that clinicians can implement a similar strategy.
Methods
Participants
From March 2008 to February 2009, 27 patients admitted to the ICU were prospectively enrolled in a pilot study to determine safety and feasibility of physical therapy intervention for patients with ICU-acquired weakness and to characterize PT management and patient outcomes. Participants were excluded if they were younger than 18 years or had any of the following: preexisting peripheral nervous system disease, cortical or brainstem lesion, fewer than two limbs in which strength could be tested, a language barrier that limited comprehension, acute myocardial infarction within the last 3 weeks, unstable angina, or history of concerning arrhythmias. This study was approved by the Colorado Multiple Institutional Review Board and informed consent was obtained for all participants prior to any procedures.
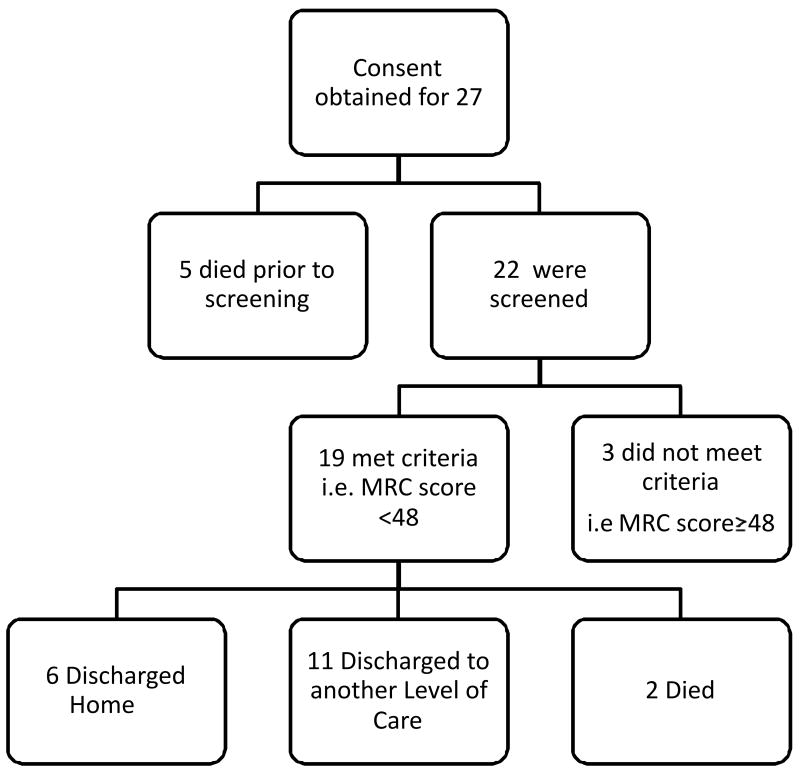
Twenty seven participants or their family members gave consent to participate in this study (Figure 1). Of these, 22 received an initial examination, 19 met the criteria for ICU-acquired weakness and 3 did not because they had Medical Research Council (MRC) scores of ≥48 out of 60 (indicating they did not have weakness; see below).1, 18-20 The 19 remaining participants were included in this case series.
Figure 1. Flow of participants through the stages of the study.
Initial Medical Examination
Muscle strength for 6 bilateral muscle groups was rated from 0 (no palpable contraction) to 5 (full force production) using the MRC scoring system.18 The muscle groups tested were shoulder and elbow flexors, wrist extensors, hip flexors, knee extensors, and ankle dorsiflexors for a total possible score of 60.18 The MRC scoring system has been validated and is reliable in individuals with both peripheral and central nervous system dysfunction as well as those with critical illness.18-20 A sum score of 48 is used to screen for ICU-acquired weakness.1,19,20
Evidence of delirium was determined by the Confusion Assessment Method for the ICU (CAM-ICU).21 The CAM-ICU detects delirium in ICU patients on MV. It uses nonverbal tasks including picture recognition, vigilance task, simple yes/no logic questions and simple commands to assess the presence or absence of delirium.22
Illness severity, organ failure, and muscle strength were assessed at study enrollment by the treating physician, using the Acute Physiology and Chronic Health Evaluations (APACHE) II, the Sepsis-related Organ Failure Assessment (SOFA), and the MRC score. The APACHE II consists of 12 physiology ratings plus age and chronic health status. Scores range from 0 – 71, with higher scores indicating greater severity of illness.15 Each three point increase in the APACHE II is associated with an increase in hospital mortality.16 The SOFA is a six item scale of organ dysfunction. Scores range from 0 – 24 with higher scores indicating greater dysfunction.17 A score of 3 – 4 indicates that at least 2 organs have failed. A score of >15 has a sensitivity of 31% and specificity of 99% for predicting mortality.17
Physical Therapy Procedures
Examination and Evaluation
As soon as participants were able to follow simple motor commands (e.g., open/close your eyes, “look at me”),19 a physical therapist performed an examination as outlined in Table 1. Vital sign responses were monitored throughout the examination. Based on the initial PT examination findings, the physical therapist determined an appropriate plan of care. The decision to begin early and intensive PT was based on medical stability, oxygen saturation, ventilation, and perfusion over the past 24 hours as well as the patient's cognitive ability to participate in the intervention. The elements of the plan of care were based on the participants's specific functional ability, areas of weakness, and mental status.
Table 1. Physical Therapy Examination Procedures.
| Component | Assessment strategy |
|---|---|
| Cognitive Status | Ability to follow these commands:
|
| Range of motion (ROM) | Passive and Active ROM23 |
| Strength | MMT using the method of Daniels and Worthingham24 for the following motions:
|
| Functional Status |
|
| Sitting Balance |
|
| Standing Balance |
|
ROM= range of motion, MMT= manual muscle test, FIM= functional index measure, LE= lower extremity, UE= Upper extremity
Decisions regarding intensity of PT treatment and treatment progression were based on physiological status (e.g., vital signs, oxygen saturation) as well as the participants's strength, functional abilities, and self-reported fatigue. This strategy, referred to as ‘response-dependent management’, is an important aspect of PT management for patients in the ICU.25 Response-dependent management refers to assessing physiological responses to increasing exercise/activity demands and using those data to determine whether to increase intensity of treatment, decrease the intensity, or terminate treatment. Using this strategy, the physical therapist can appropriately challenge patients with high levels of medical acuity. Thus, the likelihood of “over or under prescribing” is lessened.25
Implementation of PT examination and intervention took place in a team setting, including a physical therapist, nurse, respiratory therapist, and physician. The PT intervention required frequent communication with the nursing staff to determine which lines/tubes could be temporarily disconnected for mobility. The physical therapists managed the ventilator tubing but did not alter any settings.
PT Intervention
The primary components of the PT intervention included education, positioning, respiratory techniques, therapeutic exercise, and functional mobility retraining (see Table 2). PT was provided 5 times per week with a target of 30 minutes per session. For patient safety, a second person was available to assist with lines/tubes and for functional mobility. Guidelines for early termination of treatment sessions included participant reports of fatigue and physiological responses (e.g., hemodynamic instability, and/or declining pulmonary status). A protocol to handle adverse events was established; the physical therapist would terminate treatment, notify other members of the medical team, and complete an adverse event form. Adverse events were defined as desaturation less than 80%, systolic blood pressure < 90 mm Hg or > 200 mm Hg, fall to the floor, inadvertent extubation, or inadvertent removal of lines/tubes.
Table 2. Physical Therapy Intervention Techniques.
| Technique | Description |
|---|---|
| Breathing Strategies26 | |
|
| |
| Costophrenic assisted cough | Use of manual assistance over the lower ribs to assist with generation of force for a productive cough. |
|
| |
| Pursed Lip Breathing | “Breathing in through the nose to a count of “1,2” and out via pursed lips to a count of “1,2,3,4” |
|
| |
| Diaphragmatic Breathing | Have patient place one hand over umbilicus and one hand on upper chest (distal to clavicles). Instruct patient to increase excursion of hand over umbilicus with decreased movement of upper chest. Begin this task in a comfortable position; incorporate as appropriate while performing functional tasks. |
|
| |
| Scoop Technique | Use tactile cues to facilitate diaphragmatic breathing. A “slow stretch up and under the anterior thorax” Then ask the patient to “breathe into my hand”. |
|
| |
| Range of Motion Exercise | AAROM using PNF Diagonals23 |
|
| |
| Upper Extremity | PNF Diagonal 1 and 223 in both flexion and extension with manual contact over the agonist muscle groups performed in supine and sitting |
|
| |
| Lower Extremity | PNF Diagonal 1 and 223 in supine with manual contact over the agonist muscle groups. |
| In sitting: straight plane exercises of hip flexion, abduction and adduction, knee flexion/extension, and ankle dorsiflexion/plantarflexion. | |
| In standing, closed chain activities including squats, steps to the side, calf raises. | |
|
| |
| Patient Education | Education regarding safe mobility; home exercise program |
|
| |
| Functional Mobility Training | |
|
| |
| Bed mobility | Rolling side to side with rails and verbal cues initially and decreasing use of both bed rails and cues as patient increased in strength and endurance. |
| Sidelying to sit with incorporation of pacing breathing through the functional task. | |
|
| |
| Transfer Training | Once patient was able to maintain sitting balance at edge of bed with minimal A or less, sit to stand transfers were initiated from various bed heights. Transfers from bed to chair were also performed. |
|
| |
| Gait | Once patient demonstrated 3+ LE strength and the ability to maintain postural control with minimal A or less gait training with the least restrictive device was implemented. Initial floor surfaces included uncarpeted surfaces. |
AAROM= active assistive range of motion, PNF= proprioceptive neuromuscular facilitation, A= assistance, LE= lower extremity
Based on participant tolerance and strength, the PT intervention proceeded from activities in supine, to sitting, and then standing. The first intervention session focused on breathing, passive and active range-of-motion exercise (ROM) in supine and side lying. Depending on the participant's strength and endurance, functional activities also were initiated on day one (e.g., bed mobility, sitting, transfers). As activity tolerance improved, functional training increased. Criteria for progressing participants within or across sessions were based on the clinician's judgment of the participant's physiological response (e.g., oxygen saturation, HR, and blood pressure), neuromuscular and cognitive status, and participant subjective report of fatigue.
Outcome Measures
Outcomes were assessed using the following measures: Three tasks from the Functional Independence Measure (FIM) item scores, Five Time Sit to Stand Test (FTSST), Timed Up and Go (TUG), 2-Minute Walk Test (2MWT), Manual Muscle Test (MMT) summary scores, and discharge destination. The MMT-summary score was used rather than the MRC score because the MMT has the potential to pick up small but meaningful change in patients with ICU-acquired weakness.
Three functional tasks (bed mobility, transfers, and gait) were scored using components from the FIM27-30 which scores activities from 1 (total assist) to 7 (completely safe and independent). Although the total FIM has excellent reliability and validity, 27-30 the reliability of individual item scores has not been established. However, the total FIM contains items that often cannot be assessed in an ICU setting (e.g., chair and toilet transfers). A total score typically cannot be given; therefore other authors have similarly quantified the ratings for functional mobility tasks relevant for persons in the ICU.5,6
Tests of activity and balance included the FTSST, TUG, and the 2MWT. For the FTSST test, participants are asked to stand up and sit down five times as quickly as possible and the time required to complete the task is recorded. This test has established reliability,31,32 moderate discriminate properties for identifying individuals at risk for balance dysfunction and history of falls.33,34 For older subjects (age > 60 years) a cutoff point of 14.2 seconds reflects a 87% sensitivity and a 84% specificity for balance dysfunction.35 For individuals younger than 60 years old the cutoff point of 10 seconds has a sensitivity of 87% and specificity of 84% for predicting balance dysfunction.3
The TUG is a reliable and valid test evaluating a person's ability to rise from a chair, walk three meters, turn, and return to the sitting position.36 For community-dwelling elderly, TUG times of greater than 14 seconds correlates to increased fall risk with sensitivity (87%) and specificity (87%) for identifying individuals who fall.36,37 Times of <10 seconds for healthy community-dwelling women 20-80 have been reported.38 The 2MWT is commonly used to assess functional capacity and rehabilitation outcomes in a range of populations and especially in individuals with cardiac and pulmonary conditions.39-41 The 2MWT correlates with the more familiar 6MWT (r=0.94) and has high inter-rater reliability. 41 Manual muscle test (MMT) 42 was used to quantify strength for six upper extremity and seven lower extremity muscle groups (see Table 1). Reliability of MMT ranges from r=0.98 (shoulder flexion) to r=0.63 (knee flexion).43-45
Analysis
Outcomes were characterized using median scores, ranges, and frequency. For MMT, data are presented as median scores to characterize the groups (an average MMT score [MMT-summary] was calculated for each participant for the six upper extremity and 7 lower extremity muscle groups that were tested).
Results
Characteristics of the Sample
Median age of the 19 participants was 48 years (range 29-77). Ten of the participants (53%) were female (Table 3). Prior to hospitalization, all participants lived independently; four (21%) used home oxygen. Twelve participants (63%) were admitted to the Medical Intensive Care Unit (MICU) while 6 (32%) were admitted to the Surgical ICU (SICU). The most common admitting diagnoses were sepsis 6 (32%) and ARDS 5 (26%).
Table 3. Participant Baseline Characteristics.
| Characteristic | |
|---|---|
| Age median (range) | 48 (29-77) |
| Sex | (number (%)) |
| Male | 9 (47) |
| Female | 10 (53) |
| Primary Diagnosis | (number (%)) |
| Sepsis | 6 (32) |
| ARDS | 5 (26) |
| Other | 8 (42) |
| Co-Morbid Conditions | (number (%)) |
| Cardiovascular Disease | 6 (32) |
| Diabetes | 5 (26) |
| Liver Disease | 4 (21) |
| COPD | 3 (16) |
| Chronic Renal Failure-Hemodialysis | 2 (11) |
| Lung Transplant | 1 (5) |
| Cancer | 1 (5) |
| Primary Service | |
| MICU | 12 (63) |
| SICU | 6 (32) |
| NICU | 1 (5) |
| Assessment [possible range] | median (range) |
| APACHE II [0-71] | 15.5 (4-25) |
| SOFA [0-24] | 6 (2-18) |
| MRC Score [0-5] | 1.5 (1-4) |
ARDS = acute respiratory distress syndrome, COPD= chronic obstructive pulmonary disease, MICU= medical ICU, SICU = surgical ICU, NICU = neurological ICU, APACHE= Acute Physiology and Chronic Health Evaluations, SOFA= Sepsis-related Organ Failure Assessment, MRC=Medical Research Council Summary Score
The median APACHE II and SOFA score for the cohort were 15.5 and 6 respectively. At baseline, 12 (63%) of participants demonstrated delirium as determined by the CAM-ICU rating scale.21 The median number of hospital days at study enrollment was 13, and on average, PT was initiated two days after study enrollment. The median number of days on MV was 9 at both study enrollment and initiation of PT. Baseline MRC scores are shown in Table 3.
The individual participant's MMT-summary scores ranged from 1- 3.5, median score of 2.5, indicating sufficient weakness to preclude independent function. FIM scores ranged from 1- 4, with a median score of 2, indicating participants required maximal assistance. No participants were able to complete the higher level functional tests (e.g., TUG, FTSST, and 2MWT) at the time of baseline testing.
PT Interventions
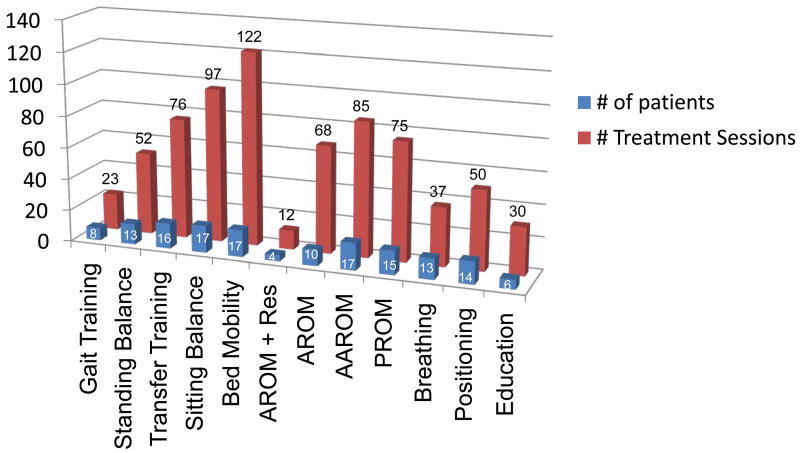
On average, the PT sessions were implemented 5 times per wk with a mean duration of 30 minutes. Specific treatments, the number of participants who received each treatment, and the total number of treatments (are illustrated in Figure 2). Seventeen patients (89%) participated in basic functional activities. Thirteen patients (68%) received education related to airway clearance and pacing of respiratory rate, and 8 patients (42%) engaged in gait training.
Figure 2. Frequency of application of the specific interventions.
Key: AAROM: active assisted range-of-motion, AROM: active range-of-motion, PROM: passive range-of-motion, Res: resisted range-of-motion,
With regard to feasibility, a total of 170 PT sessions were administered without any adverse events. Only 20 sessions (12%) were stopped before 30 minutes. The most common reason for terminating a treatment session early was ‘patient reported excessive fatigue’ (reported by 3 of the participants for a total of 10 sessions). For these three participants, we examined age, acuity of illness, time on ventilation, total hospital days, and muscle strength. No consistent pattern accounted for their frequent reports of fatigue. Indeed, some participants with the greatest weakness were able to complete all of the PT intervention sessions. Other reasons for terminating treatment sessions early included: patient refusal, and patient unable to respond to commands (2 each), and patient confusion, heart rate >160 bpm, and systolic BP drop of >20 mm Hg (1 each).
Outcomes and Discharge
Baseline and discharge status for strength and FIM scores for the 19 participants is summarized in Table 4. Seventeen participants survived to hospital discharge. Eleven survivors (65%) were discharged to another level of care, and six (35%) were discharged home. To further describe the sample, the data were stratified by those who were discharged home and those who went to another level of care (i.e., long term acute care or acute rehabilitation). Participants who were discharged home showed a trend toward higher initial MMT-summary and FIM scores. At initial examination, the participants discharged home were very similar to those discharged to another level of care (Table 5). However, at the time of hospital discharge those who went home were stronger (MMT-summary) and functioned with less assistance than those who went to another level of care.
Table 4. Outcome Data at Baseline and Discharge.
| Baseline | Discharge | |
|---|---|---|
| MMT (median (range)) | 2.5 (1-3.5) | 3 (1.5-4.5) |
| FIM (median (range)) | ||
| Bed Mobility | 2 (1-4) | 4 (1-6) |
| Transfers | 1 (1-4) | 4 (1-6) |
| Gait | 1 (1-4) | 3 (1-6) |
MMT=manual muscle test, FIM=functional independence measure
Note: data are for 17 survivors
Table 5. Outcome Measures According to Discharge Destination.
| Discharged Home (n=6) |
Discharged to Other Level of Care (n=11) |
|
|---|---|---|
| Median (range) | Median (range) | |
| MMT | ||
| Baseline | 2 (1-3.5) | 2.5 (1-3.5) |
| Discharge | 4 (3-4.5) | 3 (1-4.5) |
| FIM | ||
| Bed Mobility | ||
| Baseline | 2.5 (1-4) | 2 (1-4) |
| Discharge | 5 (5-7) | 4 (1-5) |
| Transfers | ||
| Baseline | 2 (1-4) | 1 (1-4) |
| Discharge | 5 (5-6) | 2 (1-4) |
| Gait | ||
| Baseline | 1 (1-3) | 1 (1-1) |
| Transfer | 6 (5-6) | 1 (1-5) |
MMT=manual muscle test, FIM=functional independence measure
Note: data are for 17 survivors
Changes over time also differed for the two groups. Individuals who went home had a median (range) study duration of 14.5 (7-30) days with a 2.5 to 5-point change in the FIM subscales and a 2-point improvement on the MMT. Individuals discharged to another level of care participated for a median (range) duration of 15 (7-30) days with a 1- to 2-point change on the FIM subscales and less than a 1-point change on the MMT (Tab. 5). Median total hospital days also differed for the two groups (28.5 and 22 respectively), although the range of days was comparable.
Only a few participants could perform higher level balance and functional tests at discharge. Four participants performed the FTSST; of these, one was discharged home and three were discharged to another level of care. One participant who was discharged home was able to perform the TUG and 2MWT. By the time of hospital discharge, 8 (47%) of the participants were able to walk. Of these, 6 (35%) were discharged home and 2 (12%) were discharged to another level of care.
Discussion
This case series describes safety and feasibility of PT intervention for patients with ICU-acquired weakness who required MV for at least 7 days. A total of 170 treatment sessions were implemented without any adverse events. This finding is similar to reports of other investigators,4,5,14 suggesting that the safety criteria implemented in this study and by others are appropriate. Furthermore, the intervention was well tolerated by the patients with only 12% of sessions terminated early. Based on the severity of illness, it was anticipated that some treatment sessions would be stopped early. It was surprising that so few participants needed to stop the treatment early.
Three participants accounted for the majority of the sessions that were stopped early. We found no consistent pattern explaining the early fatigue. Possibly the sample size was too small. Possibly, other issues contributed to the experience of these participants (e.g., depression, low motivation). Importantly, those participants with the greatest weakness did not preferentially require early termination of the intervention. One possible explanation was that the treatments were tailored to each participant, based on his or her physiological capability, and progressed according to moment-to-moment responses. These findings suggest that physical interventions can be implemented even with the weakest and most critically ill individuals.
The majority of participants were substantially limited in their ability to perform functional activities as indicated by a baseline median FIM score of 2 on three tasks: bed mobility, transfers and gait. Several higher level measures of balance and function also were used, however only a small number of participants were able to complete these additional tests by the time of hospital discharge. An alternative measure, the Physical Function ICU Test (PFIT)47-48, was made available after the beginning of this investigation. The PFIT includes 4 items: amount of assistance for sit to stand, strength for shoulder flexion and knee extension, marching in place, and an upper extremity endurance task of arm elevation to 90° shoulder flexion.47-48 This tool can be used clinically as an outcome measure and to guide exercise prescription. Future investigations may find it of benefit to include the PFIT as an outcome measure.
The PT interventions were similar to those in a recent report of PT practice in the US during acute care.49 Early in the case series, respiratory interventions were underutilized (Figure 2). However based on an understanding of the effect of MV on the diaphragm, it is clear that the respiratory system is likely affected and should be examined and treated. Specifically, after 18 hours of MV, Type I and Type II muscle fiber atrophy occurs along with contractile tissue dysfunction.50 Participants in this case series required MV for at least 7 days. Furthermore, three individuals had a co-morbid diagnosis of COPD with probable chronic changes of the diaphragm mechanics.51-52 The impact of respiratory interventions to assist with clearance and management of secretions, pacing of respiratory rate, and to decrease reliance on accessory muscles of breathing should be examined in future investigations.26 In this pilot study, only 13 participants received at least one session containing direct respiratory interventions. However, for patients on prolonged MV, we recommend screening the respiratory system to determine whether intervention is warranted.
Two physical therapists were available to implement each PT treatment session if needed, although most sessions were conducted with only one physical therapist. This contrasts with other mobility protocols used by Bailey4 and Morris,14 that used at least three people (RN, PT, CNA/Tech, RT) per treatment session. The lack of adverse events in our study suggests that PT interventions typically can be implemented with one (and occasionally two) individuals, making such interventions more feasible and realistic for widespread implementation.
Treatments started with participants in the supine position, and progressed to sitting and then to standing in this study and in other investigations.4,5,14 However, this progression may underestimate the patient's actual capacity. By fatiguing the patient during the least demanding tasks, it may not be possible to practice the more demanding and functionally relevant tasks. Therefore, it may be appropriate to begin the intervention with the more challenging and functionally meaningful tasks. Denehy and colleagues47-48 developed such a protocol in which patients perform the most demanding task firsts (e.g., marching in place). As time allowed, they proceeded to exercises that required less effort (e.g., supine activities). There are merits to both approaches and there is insufficient evidence to determine which is more efficacious.
Critically ill individuals clearly can tolerate earlier mobilization than typically occurs, potentially resulting in improved patient outcomes. Due to the extent of these patients' medical complexity, a team approach is necessary, including physicians, nurses, respiratory therapists, and physical therapists. Each professional brings his or her own expertise and perspective. Together the team can arrive at the best decisions regarding safe and effective interventions. Furthermore, when implementing physical interventions, the physical therapist needs to be aware of the full medical condition and findings from all other members of the team.
It is important to establish which participants are likely to benefit from early, aggressive physical intervention. As a first step to making this determination, and to set the stage for future investigations, we stratified the data according to those participants who were discharged home versus those who required further inpatient care. It was not possible to predict discharge destination of participants in each group based on physical function or MMT at baseline. It will be important to examine a variety of other indicators in a larger data set to determine whether it is possible to predict ultimate discharge destination.
With respect to patients discharged to settings other than the home, those in this investigation required more assistance for bed mobility and transfers and were non-ambulatory at initial assessment. This contrasts with data of Bailey et al14 as on average their patients ambulated within 1-2 days after respiratory ICU admission and walked more than 100 feet by day 3. Strength was not reported, but one can infer that they must have had greater than 3 muscle grade for lower extremity strength based on ability to walk. In the study by Schweickert and Hall,5 by the time of hospital discharge, 62% of patients in the treatment group and 40% of patients in the standard of care group did not require physical assistance for ambulation. In contrast approximately 32% of our cohort were ambulatory without physical assist (FIM level 5-7) at hospital discharge. However, Schweickert and Hall's cohort of patients required less time on MV, and PT was initiated on day 3 of MV. In contrast, on average our sample started PT nine days after MV, which may reflect a greater level of medical acuity.
When we compared characteristics of participants at discharge who went home with those who were discharged to another level of care, it appeared that the latter patients had greater weakness and were more limited functionally. The sample size in this investigation was too small to characterize the relationship between strength and functional limitations; however this issue should be evaluated in a larger study. It is important to note that many of the participants who were discharged home still had significant activity limitations and weakness. From reports by Herridge7, Heyland, 8 and Fletcher,11 participants surviving critical illness and/or ARDS continue to demonstrate limitations in function one year and some up to five years after discharge.
Future studies are needed which clearly characterize participants to establish characteristics of those participants who will benefit most from early, aggressive physical intervention; predictors for those who will be discharged home; how long weakness and functional loss persist among those discharged home; and how long physical intervention should continue.
Limitations
Several limitations should be acknowledged including the small sample size, lack of control group, floor effect of function and balance measures, and the unblinded assessors. Nevertheless, the findings provide important preliminary insight into participants' functional ability, strength and willingness to participate in PT while in the ICU. Furthermore, findings from this cohort were used to establish protocols for a large randomized controlled trial currently underway (NIH # NR-11051).
In summary, early activity, mobilization, and PT was safe and feasible for a cohort of participants with ICU-acquired weakness who were mechanically ventilated for 7 or more days. Although this study is preliminary and qualitative, it appears that patients who survive critical illness tolerate PT well and may require additional rehabilitation after hospital discharge. It is now imperative that future studies investigate the most efficacious types of PT, which includes identifying the most appropriate examination and outcome tools and defining optimal frequency and duration of intervention, both during hospitalization and after discharge home or to other levels of care.
References
- 1.Stevens R, Marshall S, Cornblath D, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med. 2009;37(10):S299–S308. doi: 10.1097/CCM.0b013e3181b6ef67. [DOI] [PubMed] [Google Scholar]
- 2.Schweickert W, Hall J. ICU-acquired weakness. Chest. 2007 May;131(5):1541–1549. doi: 10.1378/chest.06-2065. [DOI] [PubMed] [Google Scholar]
- 3.Khan J, Harrison T, Rich M, Moss M. Early development of critical illness myopathy and neuropathy in patients with severe sepsis. Neurology. 2006;67:1421–1425. doi: 10.1212/01.wnl.0000239826.63523.8e. [DOI] [PubMed] [Google Scholar]
- 4.Morris P, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008 Aug;36(8):2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 5.Schweickert W, Pohlman M, Pohlman A, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 May;373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zanni J, Korupolu R, Fan E, et al. Rehabilitation therapy and outcomes in acute respiratory failure: An observational pilot project. J Crit Care. 2009 Nov; doi: 10.1016/j.jcrc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003 Feb 20;348(8):683–693. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
- 8.Heyland DK, Groll D, Caeser M. Survivors of acute respiratory distress syndrome: relationship between pulmonary dysfunction and long-term health-related quality of life. Crit Care Med. 2005 Jul;33(7):1549–1556. doi: 10.1097/01.ccm.0000168609.98847.50. [DOI] [PubMed] [Google Scholar]
- 9.Herridge MS, Batt J, Hopkins RO. The pathophysiology of long-term neuromuscular and cognitive outcomes following critical illness. Crit Care Clin. 2008 Jan;24(1):179–199. x. doi: 10.1016/j.ccc.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF., Jr Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005 Feb 15;171(4):340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 11.Fletcher SN, Kennedy DD, Ghosh IR, et al. Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med. 2003 Apr;31(4):1012–1016. doi: 10.1097/01.CCM.0000053651.38421.D9. [DOI] [PubMed] [Google Scholar]
- 12.Herridge MS. Long-term outcomes after critical illness: past, present, future. Curr Opin Crit Care. 2007 Oct;13(5):473–475. doi: 10.1097/MCC.0b013e3282eff3af. [DOI] [PubMed] [Google Scholar]
- 13.Latronico N, Shehu I, Seghelini E. Neuromuscular sequelae of critical illness. Curr Opin Crit Care. 2005 Aug;11(4):381–390. doi: 10.1097/01.ccx.0000168530.30702.3e. [DOI] [PubMed] [Google Scholar]
- 14.Bailey P, Thomsen B, Spuhler V, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(1):139–145. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- 15.Knaus W, Draper E, Wagner D, Zimmerman J. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 16.Wong D, Knaus W. Predicting outcome in critical care: the current status of the APACHE prognostic scoring system. Can J Anaesth. 1991;38(3):374–383. doi: 10.1007/BF03007629. [DOI] [PubMed] [Google Scholar]
- 17.Vincent J, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 18.Kleyweg R, Van Der Meche F, Schmitz P. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle & Nerve. 1991;14(11):1103–09. doi: 10.1002/mus.880141111. [DOI] [PubMed] [Google Scholar]
- 19.De Jonghe B, Sharshar T, Lefaucheur JP, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002 Dec 11;288(22):2859–2867. doi: 10.1001/jama.288.22.2859. [DOI] [PubMed] [Google Scholar]
- 20.Ali NA, O'Brien JM, Jr, Hoffmann SP, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008 Aug 1;178(3):261–268. doi: 10.1164/rccm.200712-1829OC. [DOI] [PubMed] [Google Scholar]
- 21.Ely E, Inouye S, Bernard G, et al. Delirium in Mechanically Ventilated Patients. Validity and Reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) JAMA. 2001;286(21):2703–10. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 22.Plaschke K, von Haken R, Scholz M, et al. Comparison of the confusion assessment method for the intensive care unit (CAM-ICU) with the Intensive Care Delririum Screening Checklist (ICDSC) for delirium in critical care patients gives high agreement rate(s) Intensive Care Med. 2008;34(3):431–436. doi: 10.1007/s00134-007-0920-8. [DOI] [PubMed] [Google Scholar]
- 23.Kisner C, Colby L, editors. Therapuetic Exercise: Foundations and Techniques. 5th. Philadelphia: FA Davis Company; 2002. Resistance exercise for impaired muscle performance. [Google Scholar]
- 24.Hislop HJ, Montgomery J, editors. Daniels and Worthingham's Muscle Testing Techniques of Manual Examination. 7th. Philadelphia: WB Saunders Company; 2002. [Google Scholar]
- 25.Dean E. Mobilizing Patients in the ICU: Evidence and Principles of Practice. Acute Care Perspectives. 2008;17(1):1–9. 23. [Google Scholar]
- 26.Frownfelter D, Massery M. Facilitating ventilation patterns and breathing strategies. In: Frownfelter D, Dean E, editors. Cardiovascular and Pulmonary Physical Therapy Evidence and Practice. 4th. St. Louis: Mosby Elsevier; 2006. [Google Scholar]
- 27.Dodds T, Martin D, Stolov W, Deyo R. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74(5):531–36. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 28.Hsueh I, Lin J, Jeng J, Hsieh C. Comparison of the psychometric characteristics of the functional independence measure, 5 item Barthel index, and 10 item Barthel index in patients with stroke. J Neurol Neurosurg Psychiatry. 2002;73:188–90. doi: 10.1136/jnnp.73.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hobart J, Lamping D, Freeman J, et al. Which disability scale for neurologic rehabilitation? Neurology. 2001;57:639–644. doi: 10.1212/wnl.57.4.639. [DOI] [PubMed] [Google Scholar]
- 30.Sharrack B, Hughes R, Soudain A, Dunn The psychometric properities of clinnical rating scales used in multiple sclerosis. Brain. 1999;122(1):141–159. doi: 10.1093/brain/122.1.141. [DOI] [PubMed] [Google Scholar]
- 31.Lord S, Murray S, Chapman K, Munro B, Tiedemann A. Sit-to-Stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. J Gerontol A Biol Sci Med Sci. 2002;57(8):M539–M543. doi: 10.1093/gerona/57.8.m539. [DOI] [PubMed] [Google Scholar]
- 32.Howe T, Oldham J. Functional tests in elderly osteoarthritic subjects: variability of performance. Nurs Stand. 1995;9(29):35–38. doi: 10.7748/ns.9.29.35.s40. [DOI] [PubMed] [Google Scholar]
- 33.Mak M, Pang M. Parkinsonian single fallers versus recurrent faller: different characteristics and clinical features. Neurol. 2010 May 7; doi: 10.1007/s00415-010-5573-9. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 34.Gardner M, Buchner D, Robertson M, Campbell A. Practical implementation of an exercise-based falls prevention programme. Age and Ageing. 2001;30:77–83. doi: 10.1093/ageing/30.1.77. [DOI] [PubMed] [Google Scholar]
- 35.Whitney SL, Wrisley DM, Marchetti GF, Gee MA, Redfern MS, Furman JM. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther. 2005 Oct;85(10):1034–1045. [PubMed] [Google Scholar]
- 36.Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly patients. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 37.Shumway-Cook A, Brauer S, Woollacott M. Predicting the Probability for Falls in Community Dwelling Older Adults Using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 38.Isles RC, Choy NL, Steer M, Nitz JC. Normal values of balance tests in women aged 20-80. J Am Geriatr Soc. 2004;8:1367–1372. doi: 10.1111/j.1532-5415.2004.52370.x. [DOI] [PubMed] [Google Scholar]
- 39.Hamilton D, Haennel R. Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. J Cardiopulm Rehabil. 2000;20(3):156–164. doi: 10.1097/00008483-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Brooks D, Parsons J, Tran D, et al. The two-minute walk test as a measure of functional capacity in cardiac surgery patients. Arch Phys Med Rehabil. 2004 Sep;85(9):1525–1530. doi: 10.1016/j.apmr.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 41.Leung A, Chan K, Sykes K, Chan K. Reliability, validity, and responsiveness of a 2-min walk test to assess exercise capacity of COPD patients. Chest. 2006 Jul;130(1):119–125. doi: 10.1378/chest.130.1.119. [DOI] [PubMed] [Google Scholar]
- 42.Kendall F, McCreary E, Provance P, Rodgers M, Romani W. Muscles Testing and Function with Posture and Pain. 5th. Baltimore: Lippincott Williams and Wilkins; 2005. [Google Scholar]
- 43.Leggin B, Neuman R, Lannotti J, Williams G, Thompson E. Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. Shoulder Elbow Surg. 1996;5(1):18–24. doi: 10.1016/s1058-2746(96)80026-7. [DOI] [PubMed] [Google Scholar]
- 44.Wadsworth C, Krishnan R, Sear, Harrold J, Nielsen D. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther. 1987;67(9):1342–1347. doi: 10.1093/ptj/67.9.1342. [DOI] [PubMed] [Google Scholar]
- 45.Escolar D, Henricson E, Mayhew J, Florence J. Clinical evaluator relability for quantitative and manual muscle testings measures of strength in children. Muscle & Nerve. 2001;24(6):787–793. doi: 10.1002/mus.1070. [DOI] [PubMed] [Google Scholar]
- 46.Hough C, Steinberg K, Taylor Thompson B, Rubenfeld G, Hudson L. Intensive care unit-acquired neuromyopathy and corticosteroids in survivors of persistent ARDS. Int Care Med. 2009;35(1):63–68. doi: 10.1007/s00134-008-1304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Denehy L, Berney S, Skinner E, et al. Evaluation of Exercise Rehabilitation for Survivors of Intensive Care: Protocol for Single Blind Randomised Controlled Trial. The Open Critical Care Medicine Jounral. 2008;1:39–47. [Google Scholar]
- 48.Skinner EH, Berney S, Warrillow S, Denehy L. Development of a physical function outcome measure (PFIT) and a pilot exercise training protocol for use in intensive care. Crit Care Resusc. 2009 Jun;11(2):110–115. [PubMed] [Google Scholar]
- 49.Hodgin K, Nordon-Craft A, McFann K, Mealer M, Moss M. Physical therapy utilization in intensive care units: results from a national survey. Crit Care Med. 2009 Feb;37(2):561–566. doi: 10.1097/CCM.0b013e3181957449. quiz 566-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powers S, Kayazis A. Prolonged mechanical ventilation alters diaphragmatic structure and function. Crit Care Med. 2009;37(10):S347–S353. doi: 10.1097/CCM.0b013e3181b6e760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.De Troyer A. Effect of hyperinflation on the diaphragm. Eur Respir J. 1997;10:708–713. [PubMed] [Google Scholar]
- 52.Stubbings A, Moore A, Dusmet M, et al. Physiological properties of human diaphragm muscle fibres and the effect of of chronic obstructive pulmonary disease. J Physiol. 2008;586(10):2637–2650. doi: 10.1113/jphysiol.2007.149799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frownfelter D, Massery M. Facilitating ventilation patterns and breathing strategies. In: Frownfelter D, Dean E, editors. Cardiovascular and Pulmonary Physical Therapy Evidence and Practice. 4th. St. Louis: Mosby Elsevier; 2006. [Google Scholar]