Abstract
In the management of renal trauma, surgical exploration inevitably leads to nephrectomy in all but a few specialized centers. With current management options, the majority of hemodynamically stable patients with renal injuries can be successfully managed nonoperatively. Improved radiographic techniques and the development of a validated renal injury scoring system have led to improved staging of injury severity that is relatively easy to monitor. This article reviews a multidisciplinary approach to facilitate the care of patients with renal injury.
Key words: Renal injury, Nephrectomy, Blunt trauma, Angiogenesis, Embolization
Renal injury occurs in approximately 1% to 5% of all traumas1,2 and can be classified as blunt or penetrating according to the mechanism. Blunt injuries are usually secondary to high-energy collisions such as motor vehicle accidents (MVA), falls from a height, and contact sports, although significant injuries have been reported following trivial trauma in structurally abnormal kidneys. In the Australian state of Victoria,a 89 Grade ≥ 2 renal injuries were recorded in 2008, with blunt trauma accounting for 94.4%; 57.3% were Grade 2 injuries, 12.4% Grade 3, 25.8% Grade 4, and 4.5% Grade 5. MVAs and motorcycle accidents were the most common cause of injury, accounting for 48.3% of all renal injuries.3 Civilian penetrating injuries are uncommon in Australia, and typically of low velocity, such as stabbings. In military series and certain urban areas (eg, South Africa and North America), gunshot wounds are a significant cause of penetrating injuries. The majority of blunt renal trauma cases are associated with injury to other abdominal organs, but they are commonly low-grade injuries.4
In the management of renal trauma, surgical exploration inevitably leads to nephrectomy in all but a few specialized centers. Given the success of conservative management of other solid organ injuries, this approach has been increasingly applied to patients with renal trauma. With current management, the majority of hemodynamically stable patients with renal injuries are successfully managed nonoperatively. 5,6 Improved radiographic techniques and the development of a validated renal injury scoring system have led to improved staging of injury severity that is relatively easy to monitor. In addition, improved hemodynamic management of patients in specialized units has led to improved outcomes with nonoperative management.
Furthermore, selective treatment with interventional procedures in radiology has reduced the need for surgical intervention. Successful hemostasis with angiography and renal embolization has been achieved for patients with blunt and penetrating renal injuries.2,7,8
Initial Management
Resuscitation
The approach to management of patients with major abdominal trauma has been standardized according to set protocols with the development of structured advanced trauma life support (ATLS) guidelines, the development of policies for minimizing coagulopathy with massive transfusions, and the use of damage control surgery (DCS).
Initial management of an adult with major trauma or suspected renal injury follows ATLS guidelines. The principles of ATLS are to identify and treat the immediate life-threatening injuries first by the assessment of Airway, Breathing, Circulation, Disability, Exposure/Environment. Renal injuries may present in the primary survey as hypovolemic shock; however, most will be identified in the secondary survey after imaging.
The development of massive transfusion protocols in resuscitation has seen significant reductions in 24-hour mortality.6 They aim to reduce traumatic coagulopathy through the administration of fresh frozen plasma, platelets, and coagulation products, in addition to packed red blood cells (RBCs). At our institution, the protocol is activated on the release of 4 or more units of RBCs and/or anticipated massive transfusion.9 Products are replaced at a ratio of 4 units of RBCs to 2 units of fresh frozen plasma. Platelets are used to maintain levels greater than 50 × 109/L and the international normalized ratio is kept less than 2.0. Cryoprecipitate is considered if fibrinogen is less than 1.0 g/L.
Evidence regarding the effect of blood product ratio on mortality outcomes differs.10 Recent military experiences in Iraq and Afghanistan have seen the development of more aggressive massive transfusion protocols, with a ratio of 1:1:1 of RBCs, fresh frozen plasma, and platelets.11 Although there is a higher proportion of penetrating trauma in these populations, early evidence suggests that similar protocols may also be associated with improvements in early mortality and coagulopathy in civilian settings.12–14
DCS involves a staged surgical approach to injury identification and repair to minimize extensive procedures on unstable patients. DCS aims to reduce the lethal triad of acidosis, hypothermia, and coagulopathy by gaining early control of bleeding and contamination and preventing of further heat loss. However, a recent systematic review has questioned the benefit of such an approach.15
Grade
The Injury Severity Scale for the kidney is an anatomic-based description, developed by the American Association for the Surgery of Trauma (AAST) in 1989 to facilitate clinical research (Table 1), and it has been validated for clinical use.16 It classifies renal injuries into five grades in order of increasing severity. It is widely used and is a powerful predictor of clinical outcome.17,18 The grade directly correlates with the need for intervention, nephrectomy, dialysis, and mortality.17,19,20 Consequently, an accurate early assessment of grade is vital to determine management strategy. Figures 1 through 5 illustrate examples of each grade.
Table 1.
Kidney Injury Scale
| Grade | Description |
| 1 | Contusion or nonexpanding subcapsular hematoma without parenchymal laceration |
| 2 | Nonexpanding perirenal hematoma or laceration < 1 cm deep without urinary extravasation |
| 3 | Laceration > 1 cm deep without urinary extravasation |
| 4 | Laceration extending though renal cortex into collecting system or segmental renal artery or vein injury with contained hemorrhage or partial vessel laceration or vessel thrombosis |
| 5 | Shattered kidney or renal pedicle injury/avulsion of renal hilum |
Figure 1.
Grade 1 injury.
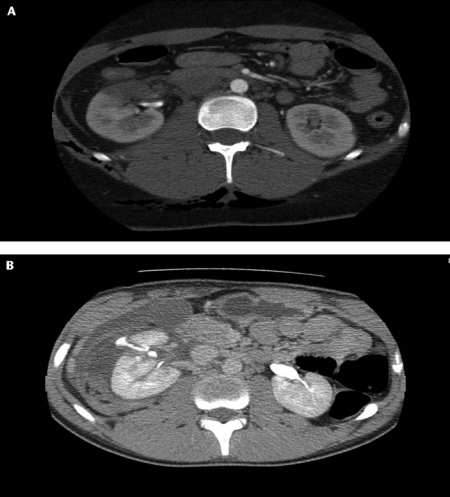
Figure 5.
(A) Grade 5 injury, shattered kidney. (B) Grade 5 injury with devascularized kidney. (C) Angiogram of Grade 5 injury with devascularized kidney.
Investigation
The majority of renal injuries are associated with injury of other abdominal organs. In the event of suspected blunt renal injury, the indications for imaging are visible hematuria, microscopic hematuria with systolic blood pressure < 90 mm Hg, the presence of major associated injuries, or a high index of suspicion based on mechanism of injury, such as a rapid deceleration injury.21 It is important to note that absence of hematuria does not exclude renal injury. Renal imaging should be performed in all patients with penetrating trauma to the torso where renal injury is suspected on the basis of entry or exit wounds.2
Ultrasound is routinely performed at the bedside in trauma patients as part of focused assessment by sonography in trauma to identify hemoperitoneum. It has a low sensitivity for the identification of retroperitoneal free fluid.22
Computed tomography (CT) is the gold standard for visceral imaging after blunt trauma.23 The arterial and portal venous phase can identify active extravasation, whereas delayed phase images assess the renal collecting system and ureteric continuity.24
If the patient progresses to emergency laparotomy without undergoing a CT scan, and a renal injury is identified, then a one-shot intravenous pyelogram can be performed at the time of surgery (using 2 mL/kg intravenous [IV] contrast).2 This not only assesses the degree of renal injury, but also confirms the presence of a functioning contralateral kidney.
Management
The Stable Patient
Patients with Grades 1 through 4 injuries can generally be managed conservatively. It is important, however, to appreciate that there are significant clinical differences between a Grade 4 laceration and a Grade 4 unstable vascular injury, and that the latter may necessitate intervention. Grade 5 injuries are more controversial, as traditional treatment involves intervention and possibly nephrectomy. However, successful conservative management has been reported and it is important to understand that there is a spectrum of Grade 5 injuries from the less severe (avascular kidneys with minimal hematoma) to more severe (burst kidney or uncontained pedicle avulsion).
Previously, exploratory laparotomy was recommended for all patients with penetrating renal injuries. However, nonoperative management has become more accepted for Grades 1 through 3 with penetrating renal injuries in the absence of associated intra-abdominal injury or hemodynamic instability.21,25
The Unstable Patient
Patients will often have significant concomitant injuries and will require operative intervention for those injuries (eg, pelvic stabilization, splenectomy, abdominal packing). Thus, care is often directed by specific trauma surgeons.
Indications for exploration in renal trauma are life-threatening hemorrhage, renal pedicle avulsion, or pulsatile/expanding retroperitoneal hematoma at the time of laparotomy. 6,25 In cases of active extravasation of IV contrast, the decision of whether to undergo surgical exploration or angioembolization must be based on the presence of concomitant injuries and the experience of the surgical team and radiologists. It is our experience that these injuries are now managed with embolization. Although injured kidneys may be salvaged in expert hands by gaining proximal vascular control and kidney reconstruction, patient safety is paramount and the usual result is nephrectomy. Vascular repair has been described in patients with a solitary kidney or bilateral injury, but it corresponds with poor outcomes and increased complication rates.25
The role of angiography and selective renal embolization in renal trauma is increasing and is an alternative treatment to laparotomy in patients who do not require immediate surgery.2 Successful hemostasis has been reported in Grade 4 injuries caused by both blunt and penetrating mechanisms. It has been associated with a 94.4% success rate in selected patients with blunt renal artery trauma of Grade 4 or 5.8 It is associated with reduced renal parenchymal injury and complications when compared with surgical management.26
Subsequent Management
Conservative management involves close reassessment and observation with serial estimations of hematocrit, initially twice daily. The patient should be kept to strict bed rest until the hematuria resolves. The role of antibiotics is not clear, but IV broad spectrum antibiotics should be used if there is suggestion of damage to the collecting system and urine leak.
Repeat abdominal CT imaging with a delayed phase is recommended between 36 and 72 hours after initial injury for Grades 3 through 5 blunt renal injury. For more minor grades of injury, repeat imaging is probably unnecessary. 27–29 We have evaluated the role of further repeat imaging after this time at our institution and found that it adds little if the patient remains stable.27 Thus, it is reasonable to repeat the imaging only if there is a change in the patient’s condition.
Complications
Urinary Extravasation
Urinoma formation (Figure 6) is the most common complication, occurring in 1% to 7% of all patients with renal trauma.30 Clinically, the development of sepsis or declining renal function raises suspicion of urinoma formation, which may be confirmed via CT.
Figure 6.
Urinoma formation after a Grade 5 injury.
Urinary extravasation resolves spontaneously in 76% to 87% of cases.6,28 Intervention may be required if there is a persistent leak or urine collection. The insertion of a retrograde stent or percutaneous nephrostomy typically aids resolution. 31 Percutaneous drainage of the urinoma is rarely necessary.
Infection
Perinephric abscesses (Figure 7) and infected urinomas may develop secondary to bacterial seeding or concomitant enteric or pancreatic injury. Management with percutaneous drainage is often successful, although open drainage of multiloculated collections is sometimes required.5
Figure 7.
Perinephric abscess after a Grade 4 injury.
Delayed Hemorrhage
Delayed hemorrhage is a common complication with deep lacerations of the renal cortex and medulla and is seen commonly in penetrating renal trauma, particularly stab injuries.6,28 Clinically, these patients may present with hematuria, falling hematocrit, or hemodynamic instability. It is often associated with pseudoaneurysm (Figure 8) or arteriovenous fistula formation. Delayed hemorrhage occurs in 13% to 25% of Grade 3 or 4 renal injuries that are managed expectantly; however, most cases are successfully treated with angioembolization.28,32
Figure 8.
(A) Pseudoaneurysm formation in a Grade 4 injury. (B) Angiogram of the same patient. (C) Angiogram of the same patient postembolization (note vasospasm in the proximal renal artery).
Devitalized Renal Segment
Injuries with nonviable renal segments can be managed conservatively; however, these injuries are associated with a higher complication rate and the need for delayed intervention.21,28 These patients require close monitoring.
Hypertension
Injury to the renal artery or compression of the kidney from hematoma/fibrosis is thought to lead to posttraumatic hypertension mediated by increased renin secretion in response to renal ischaemia. Incidence relates to the severity of renal injury, and patients with Grade 4 and 5 injuries should have periodic blood pressure monitoring in the long term. Nephrectomy is occasionally necessary to control renovascular hypertension refractory to medical management. Successful treatment with arterial stenosis repair or partial nephrectomy has been reported.28
Renal Insufficiency
The risk of renal impairment will depend on preexisting renal disease, age, presence of single kidney, and associated multiorgan failure. One study showed the risk of requiring dialysis was 0.46% in a large review of all grades of renal trauma.19 The need for dialysis was associated with increasing AAST grade and age older than 40 years. If just high-grade injuries are analyzed, the risk may be as high as 6%.33
Follow-Up
General recommendations include 3-month follow-up that comprises a physical examination, urinalysis, blood pressure measurement, and assessment of renal function.2 There are few published data regarding the role of follow-up imaging. Some centers advocate renography as quantitative assessment of renal function following Grade 4 and 5 injuries.28 Patients should have long-term monitoring for renovascular hypertension, especially those with high-grade injuries. Patients with concomitant injuries, such as colonic or pancreatic, will require individualized imaging to monitor and prevent related complications.
Conclusions
Renal injury may be a life-threatening event, but if handled correctly can be managed safely without the need for nephrectomy in most cases. Blunt trauma accounts for the majority of renal injuries, of which a greater proportion is a less severe injury grade. The majority of hemodynamically stable patients are successfully managed conservatively. Embolization is an alternative treatment option to control bleeding, particularly in patients who do not require intervention for concomitant injuries. A multidisciplinary approach coordinated by trauma service specialists facilitates the care of these patients in our institution.
Main Points.
In the management of renal trauma, surgical exploration typically leads to nephrectomy in all but a few specialized centers. Conservative management has been increasingly applied to patients with renal trauma due to the success this option has seen in handling other solid organ injuries.
The organ Injury Severity Scale for the kidney classifies renal injuries into five grades in order of increasing severity. It is widely used and is a powerful predictor of clinical outcome. The grade directly correlates with the need for intervention, nephrectomy, dialysis, and mortality.
The majority of renal injuries are associated with injury of other abdominal organs. In the event of suspected blunt renal injury, the indications for imaging are visible hematuria, microscopic hematuria with systolic blood pressure < 90 mm Hg, the presence of major associated injuries, or a high index of suspicion based on mechanism of injury, such as a rapid deceleration injury.
Indications for exploration in renal trauma are life-threatening hemorrhage, renal pedicle avulsion, or pulsatile/expanding retroperitoneal hematoma at the time of laparotomy. In cases of active extravasation of intravenous contrast, surgical exploration or angioembolization must be based on the presence of concomitant injuries and the surgical team’s experience.
Figure 2.
Grade 2 injury.
Figure 3.
Grade 3 injury.
Figure 4.
(A) Grade 4 injury with segmental renal injury. (B) Grade 4 injury with urine extravasation.
Footnotes
Estimated population of 5.2 million as of 31 December 2007 (Australian Bureau of Statistics).
References
- 1.Bent C, Iyngkaran T, Power N, et al. Urological injuries following trauma. Clin Radiol. 2008;63:1361–1371. doi: 10.1016/j.crad.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Pineiro L, Djakovic N, Plas E, et al. EAU guidelines on urethral trauma. Eur Urol. 2010;57:735–920. doi: 10.1016/j.eururo.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Victorian State Trauma Outcomes Registry (VSTOR) Victoria, Australia: Department of Human Services; [Google Scholar]
- 4.Kuo RL, Eachempati SR, Makhuli MJ, Reed RL., 2nd Factors affecting management and outcome in blunt renal injury. World J Surg. 2002;26:416–419. doi: 10.1007/s00268-001-0241-y. [DOI] [PubMed] [Google Scholar]
- 5.Santucci RA, Fisher MB. The literature increasingly supports expectant (conservative) management of renal trauma-a systematic review. J Trauma. 2005;59:493–503. doi: 10.1097/01.ta.0000179956.55078.c0. [DOI] [PubMed] [Google Scholar]
- 6.Broghammer JA, Fisher MB, Santucci RA. Conservative management of renal trauma: a review. Urology. 2007;70:623–629. doi: 10.1016/j.urology.2007.06.1085. [DOI] [PubMed] [Google Scholar]
- 7.McGuire J, Bultitude MF, Davis P, et al. Predictors of outcome in high grade renal injury. J Urol. 2011;185:187–191. doi: 10.1016/j.juro.2010.08.085. [DOI] [PubMed] [Google Scholar]
- 8.Chow SJ, Thompson KJ, Hartman JF, Wright ML. A 10-year review of blunt renal artery injuries at an urban level I trauma centre. Injury. 2009;40:844–850. doi: 10.1016/j.injury.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 9.Massive transfusion guidelines. Melbourne, Australia: The Alfred Hospital; 2009. [Google Scholar]
- 10.Riskin DJ, Tsai TC, Riskin L, et al. Massive transfusion protocols: the role of aggressive resuscitation versus product ratio in mortality reduction. J Am Coll Surg. 2009;209:198–205. doi: 10.1016/j.jamcollsurg.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 11.Dawes R, Thomas GO. Battlefield resuscitation. Curr Opin Crit Care. 2009;15:527–535. doi: 10.1097/MCC.0b013e32833190c3. [DOI] [PubMed] [Google Scholar]
- 12.Dente CJ, Shaz BH, Nicholas JM, et al. Improvement in early mortality and coagulopathy are sustained better in patients with blunt trauma after institution of a massive transfusion protocol in a civilian level 1 trauma centre. J Trauma. 2009;66:1616–1624. doi: 10.1097/TA.0b013e3181a59ad5. [DOI] [PubMed] [Google Scholar]
- 13.Fraga GP, Bansal V, Coimbra R. Transfusion of blood products in trauma: an update. J Emerg Med. 2010;39:253–260. doi: 10.1016/j.jemermed.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 14.Greer SE, Rhynhart KK, Gupta R, Corwin HL. New development in massive transfusion in trauma. Curr Opin Anaesthesiol. 2010;23:246–250. doi: 10.1097/ACO.0b013e328336ea59. [DOI] [PubMed] [Google Scholar]
- 15.Cirocchi R, Abraha I, Montedori A, et al. Damage control surgery for abdominal trauma. Cochrane Database Syst Rev. 2010;(1) doi: 10.1002/14651858.CD007438.pub2. CD007438. [DOI] [PubMed] [Google Scholar]
- 16.Moore EE, Shackford SR, Pachter HL, et al. Organ injury scaling: spleen, liver, and kidney. J Trauma. 1989;29:1664–1666. [PubMed] [Google Scholar]
- 17.Santucci RA, McAninch JW, Safir M, et al. Validation of the American Association for the Surgery of Trauma organ injury severity scale for the kidney. J Trauma. 2001;50:195–200. doi: 10.1097/00005373-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Shariat SF, Roehrborn CG, Karakiewics PI, et al. Evidence-based validation of the predictive value of the American Association for the Surgery of Trauma kidney injury scale. J Trauma. 2007;62:933–939. doi: 10.1097/TA.0b013e318031ccf9. [DOI] [PubMed] [Google Scholar]
- 19.Kuan JK, Wright JL, Nathens AB, et al. American Association for the Surgery of Trauma Organ Injury Scale for kidney injuries predicts nephrectomy, dialysis, and death in patients with blunt injury and nephrectomy for penetrating injuries. J Trauma. 2006;60:351–356. doi: 10.1097/01.ta.0000202509.32188.72. [DOI] [PubMed] [Google Scholar]
- 20.Davis KA, Reed RL , 2nd, Santaniello J, et al. Predictors of the need for nephrectomy after renal trauma. J Trauma. 2006;60:164–169. doi: 10.1097/01.ta.0000199924.39736.36. [DOI] [PubMed] [Google Scholar]
- 21.Alsikafi NF, Rosenstein DI. Staging, evaluation, and nonoperative management of renal injuries. Urol Clin North Am. 2006;33:13–19. doi: 10.1016/j.ucl.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 22.McGahan JP, Richards JR, Jones CD, Gersovich EO. Use of ultrasonography in the patient with acute renal trauma. J Ultrasound Med. 1999;18:207–213. doi: 10.7863/jum.1999.18.3.207. [DOI] [PubMed] [Google Scholar]
- 23.Kawashima A, Sandler CM, Corl FM, et al. Imaging of renal trauma: a comprehensive review. Radiographics. 2001;21:557–574. doi: 10.1148/radiographics.21.3.g01ma11557. [DOI] [PubMed] [Google Scholar]
- 24.Kawashima A, Sandler CM, Corriere JN, Jr, et al. Ureteropelvic junction injuries secondary to blunt trauma. Radiology. 1997;205:487–492. doi: 10.1148/radiology.205.2.9356633. [DOI] [PubMed] [Google Scholar]
- 25.Master VA, McAninch JW. Operative management of renal injuries: parenchymal and vascular. Urol Clin North Am. 2006;33:21–31. doi: 10.1016/j.ucl.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Hagiwara A, Sakaki S, Goto H, et al. The role of interventional radiology in the management of blunt renal injury: a practical protocol. J Trauma. 2001;51:526–531. doi: 10.1097/00005373-200109000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Davis P, Bultitude MF, Koukounaras K, et al. Assessing the usefulness of delayed imaging in routine followup for renal trauma. J Urol. 2010;184:973–977. doi: 10.1016/j.juro.2010.04.070. [DOI] [PubMed] [Google Scholar]
- 28.Santucci RA, Wessells H, Bartsch G, et al. Evaluation and management of renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004;93:937–954. doi: 10.1111/j.1464-4096.2004.04820.x. [DOI] [PubMed] [Google Scholar]
- 29.Malcolm JB, Derweesh IH, Mehrazin R, et al. Nonoperative management of blunt renal trauma: is routine early follow-up imaging necessary? BMC Urol. 2008;8:11. doi: 10.1186/1471-2490-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee YJ, Oh SN, Rha SE, Byun JY. Renal trauma. Radiol Clin North Am. 2007;45:581–592. doi: 10.1016/j.rcl.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Matthews LA, Smith EM, Spirnak JP. Nonoperative treatment of major blunt renal lacerations with urinary extravasation. J Urol. 1997;157:2056–2058. [PubMed] [Google Scholar]
- 32.Voelzke BB, McAninch JW. The current management of renal injuries. Am Surg. 2008;74:667–678. [PubMed] [Google Scholar]
- 33.Kansas BT, Eddy MJ, Mydlo JH, Uzzo RG. Incidence and management of penetrating renal trauma in patients with multiorgan injury: extended experience at an inner city trauma center. J Urol. 2004;172:1355–1360. doi: 10.1097/01.ju.0000138532.40285.44. [DOI] [PubMed] [Google Scholar]