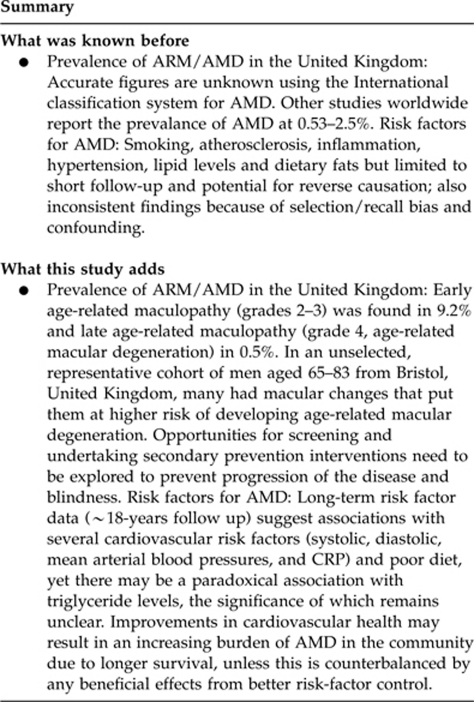
Abstract
Aims/Purpose
To determine the prevalence of age-related maculopathy (ARM) and age-related macular degeneration (AMD) in men aged 65–83 years living in the Speedwell region of Bristol, United Kingdom and identify modifiable risk factors.
Methods
A total of 2348 men recruited to the Speedwell prospective cohort study in 1979 were followed up in 1997 with an eye questionnaire and had retinal photographs that were assessed using the International Classification System for ARM.
Results
In all, 934 men (66.8% response rate) attended with a mean of 17.9 years (15.3–20.6 years) follow-up. Early ARM (grades 2–3) was found in 9.2% (95% confidence interval (CI) 7.4%, 11.4%) and late age-related maculopathy (grade 4, AMD) in 0.5% (95% CI 0.2%, 1.2%). The risk of ARM (grades 2–4) was increased with raised C-reactive protein and consumption of lard and solid fats, whereas triglyceride levels were associated with a lower risk. The latter were confirmed in multivariable analyses and in addition, haemodynamic measures also predicted risk (eg mean arterial pressure odds ratio (OR) per z-score 1.37, 95% CI 1.04, 1.79).
Conclusions
In a representative cohort of men aged 65–83 from Bristol, United Kingdom, many had macular changes that put them at higher risk of developing AMD. Various modifiable exposures were associated with an increased risk ARM/AMD. Opportunities for screening and undertaking secondary prevention interventions need to be explored to prevent progression of the disease and blindness.
Keywords: maculopathy, macular degeneration, prevalence, risk factors, cohort study, United Kingdom
Introduction
Age-related macular degeneration (AMD) is a progressive, late onset degenerative eye disease, and the most severe form of the group of abnormalities termed age-related maculopathy (ARM). It is the leading cause of permanent blindness in the elderly in the Western world.1 In the United Kingdom, it accounts for almost 42% of blindness occurring in those aged between 65–74 years, rising to 66% in those aged 75–84 years and 74% in those aged over 85 years.2 AMD is associated with a significant reduction in quality of life and functional independence in the elderly.3 As life expectancy in the developed world increases, the prevalence and incidence of blindness from this disease will undoubtedly rise unless preventive strategies or treatments are found. Several studies have examined the prevalence of ARM/AMD in the United Kingdom,4, 5, 6, 7, 8, 9, 10, 11, 12 but only two community-based studies have had a sample size of more than a thousand participants,13 and one was restricted to general practice patients over 75 years.14 Identifying those at high-risk of developing AMD is crucial in preventing irreversible visual impairment and blindness from this disease, and may lead to secondary/tertiary prevention strategies.
A number of epidemiological studies have reported a host of risk factors for ARM/AMD, the most consistent of which is smoking behaviour.15 Most of these associations are inconsistent and this may be in part due to chance, selection and recall bias, and different confounding structures. Prospective studies have the advantage of measuring risk factors before the development of the disease. These have shown positive associations with smoking,15, 16 atherosclerosis,17 systemic hypertension,18, 19 increased white cell count, gout and emphysema,20 increased dietary fat and lipid levels16 and an inverse association with a diet rich in fish.21, 22, 23, 24 All these studies examined risk factors within a relatively short latency period, which raises the concern that some associations may be because of reverse causation. In this study we have examined the prevalence of ARM and AMD in a population-based cohort of men from the United Kingdom who have been followed up for around 18 years as part of a cardiovascular cohort study. Our aim was to test whether previously observed associations, as well as novel risk factors were predictive of disease risk after a long latency period.
Methods
Study population
The Speedwell study invited all men aged 45–59 registered with the 16 general practitioners at two health centres in Speedwell, Bristol, England in 1979 to participate in a cohort study to examine cardiovascular risk factors. Full details of its design and aims have been published previously.25 During phase I (1979–1982), 2348 men (representing 92% of the target sample of 2550) underwent a clinical examination and data collection on general health, medical history, life-style and potential risk factors. Blood samples were taken in a fasting state between 5 and 9 hours. Following this, the surviving men were seen at intervals of ∼4 years comprising phases II, III, and IV. These subsequent phases collected data on new ischaemic heart disease and stroke events, repeated some baseline tests and added others. Data on dietary factors, including major food nutrients and individual food items were collected in phase II on a 25% random subsample of men (n=231). In 1997, 1420 men were sent questionnaires about their eye health and asked to participate in a study examining risk factors for ARM/AMD and cataract,26 which took place between June 1997 and December 1999.
Procedures for eye examination
Details of the eye examination have been published previously.26 Participants underwent a clinical examination including a brief history, visual acuity measurements and slit lamp examination. Eyes were then dilated with tropicamide 1% and phenylephrine 2.5%, unless contraindicated. Two 32° stereoscopic colour slide photographs centred on the macula were taken for each eye. Photography was followed by clinical examination of the posterior pole by indirect ophthalmoscopy using a Volk 78D lens.
Photographic grading
The International Classification System for ARM grading was used,27 which is based on the Wisconsin Age-related Maculopathy Grading system.28 We used the same stratification of ARM described by Klaver et al,29 whereby: 0—No ARM, 1a—Soft distinct drusen, 1b—Pigmentary irregularities, 2a—Soft, indistinct, or reticular drusen, 2b—Soft, distinct drusen with pigmentary irregularities, 3—Soft, indistinct, or reticular drusen with pigmentary irregularities, 4—Presence of atrophic or neovascular macular degeneration. Grade 4 is defined as AMD. Grading was carried out independently at the Rotterdam ARM grading centre by two trained graders. To minimise criterion shifts and inter-observer differences, images were regularly double-graded and disagreements were resolved by discussion to reach a consensus between graders. Using a grid system and grading tools, the graders were able to estimate drusen size and the area involved by drusen or retinal pigmentary changes. The number of drusen of each size both inside the grid and outside the grid, the size of the largest drusen, the most frequent size of drusen, and the percentage of confluence were recorded, as were the type of drusen: hard, soft, soft distinct, soft indistinct, reticular, and the percentage of area occupied by drusen in each of the three zones: central, inner, outer. Details of the participants' visual acuity, refractive error and previous retinal diseases were sent to the graders with the transparencies to allow attribution of the causes of lesions.
Pre-existing risk factor data
All risk factor data were taken from phase I (1979–1982) except for the dietary data, C-reactive protein (CRP) and D-dimer measures, which were taken from phase II (1985–1988) samples. Smoking habit was measured from a questionnaire and stratified into four groups: never smoked, ex-smoker, moderate smoking (including cigar/pipe and smoking between 1–14 cigarettes per day), and heavy smoking (>15 cigarettes per day). Total alcohol consumption (including weekly beer, wine, and sherry intake in units of ethyl alcohol) was estimated from a self-administered questionnaire given to every man for completion at home. Full details of this questionnaire have been published.30 A semi-quantitative food frequency questionnaire was used to acquire data on a wide variety of foodstuffs such as breads, meat, fruit, vegetables, snacks, dairy products, and cooking fats. This was carried out on a 25% random subsample (231 participants).
Resting blood pressures (BPs) were measured with a random zero sphygmomanonmeter. Cholesterol and triglyceride concentrations were measured with enzymatic procedures. The high density lipoprotein (HDL) fraction was isolated by precipitation of the low and very low-density lipoproteins (LDL, VLDL) with heparin and manganese chloride. LDL Cholesterol was estimated using the Friedewald formula whereby (LDL cholesterol)=(Total cholesterol)−(HDL cholesterol)−((Triglycerides)/2.2), where all concentrations are in mmol/l.31 Haemostatic factors, fibrinogen and white cell count were measured at baseline and methods for estimation have been published previously.32 Fibrinogen was measured by heat precipitation nephelometry. CRP was measured by a sensitive nephelometric assay (Behring, Siemens Healthcare, Camberley, UK) and D-dimer, with an ELISA (Biopool International Inc., Ventura, CA, USA).
Statistical methods
To provide greater statistical power, we have defined any subject with ARM grades 2–4 as cases as they either have AMD (grade 4) or are at a high risk of developing future AMD (2-year risk between 3–9%).29 We used ANOVA and χ2 tests to compare the means and proportions for the baseline descriptive data by AMD/case status. Data were log transformed were necessary and appropriate. All continuous variables were standardised (by subtracting the mean value and then dividing by the standard deviation) to create z-scores, which allows direct comparison of effect estimates. We used logistic regression analysis to estimate the odds ratio (95% confidence intervals (CIs) and P-values) as a proxy for the risk ratio, initially adjusting for age. A test for trend, as well as a heterogeneity test was carried out for ordinal variables. A P-value <0.05 was considered as providing evidence against the null hypothesis. Further multivariable analyses considered four models: (1) adjusting for age and social class as a non-specific confounder, (2) adjusting for age and the lifestyle variables of smoking and alcohol intake, (3) adjusting for age, metabolic and inflammatory factors: systolic blood pressure (SBP), total cholesterol, total triglycerides, BMI, blood glucose, and CRP. We examined the dietary variables from the food frequency questionnaire separately owing to the reduced sample size, and any positive associations were then adjusted for covariates that predicted in the univariable analyses but were not thought to be on the causal pathway.
Results
Of the 1420 men who were still part of the Speedwell Study in 1999 (see Table 1), 51 could not be reached and 26 died during the data collection phase resulting in 1343 eligible participants. Of these, 212 (15.8%) returned questionnaires only, 24 (1.8%) were seen in the eye clinic only and 925 (68.9%) were seen in the eye clinic and returned questionnaires.
Table 1. Stratification of ARM (0–4), worse eye, by age group in men with a gradable retinal photograph (n=934).
| Age group | ARM 0 | ARM 1 | ARM 2 | ARM 3 | ARM 4 | Total |
|---|---|---|---|---|---|---|
| 65–69 | 189 (53.6%) | 140 (39.8%) | 20 (5.7%) | 3 (0.9%) | 0 (0.0%) | 352 |
| 70–74 | 143 (41.9%) | 164 (48.1%) | 29 (8.5%) | 4 (1.2%) | 1 (0.3%) | 341 |
| 75+ | 111 (46.1%) | 96 (39.8%) | 23 (9.5%) | 7 (2.9%) | 4 (1.7%) | 241 |
| Total | 443 (47.4%) | 400 (42.8%) | 72 (7.7%) | 14 (1.5%) | 5 (0.5%) | 934 |
Abbreviation: ARM, age-related maculopathy.
Of the 949 men who attended the clinic, 14 (1.4%) had no retinal photographs taken, 6 (0.6%) had contraindications for example, shallow anterior chamber or iris clip lenses, 7 (0.7%) refused dilation and 1 (0.1%) was dilated but his photographs were lost. Eight (0.8%) had photographs of one eye only, 927 (97.6%) had retinal photographs of both eyes. Reasons for only one eye being photographed were significant corneal scaring, enucleation, iris clip lens, contraindication for dilatation, and cataract. Gradable retinal photographs of at least one eye were available for 934 (98.5%) clinic participants. The mean age of the subjects was 71.1 years (SD 4.2 years, inter-quartile range 67–74 years, range 64–79 years).
Prevalence data
Late ARM—grade 4 (classified as AMD using the Wisconsin Age-related Maculopathy Grading System28) was seen in five participants that is, 0.5% (95% CI 0.2%, 1.2%), all of whom had the condition unilaterally (three in the right eye and two in the left) with signs of early ARM in the other eye (Table 1). Three men aged 72, 76, and 79 in 1999 (who were not examined in the eye study, but had agreed to further follow up) were identified as having AMD from an electronic search of medical records increasing the rate of AMD to 0.9% (95% CI 0.4%, 1.7%). Early ARM (grade 2 and 3) was graded in 86 participants that is, 9.2% (95% CI 7.4%, 11.4%), and the prevalence of any maculopathy (ie ARM grades 1–4) was 52.6% (95% CI 48.0%, 57.4%).
Features of ARM
The worst eye was used in the analysis. Retinal pigment epithelium degeneration was found in 9.6% and hyperpigmentation in 10.4% of subjects. Overall 105 (11.3%) individuals had pigmentary abnormalities in at least one eye. The levels of hyperpigmentation and hypopigmentation were similar for each age group. Hard drusen and soft drusen less than 125 μm (C1), were the most frequent morphological types of drusen seen in all age groups. The largest drusen size gradually increased with age. For ‘large' drusen, that is, those greater than 125 μm (C1) in diameter, the prevalence was 5.1% for those aged 64–70, 7.0% for those 70–74, and 12.0% for those 75–80 (OR per unit age-group 1.09; 95% CI 1.03, 1.15, P=0.005). Confluent drusen (>50%) were found in 87 (9.3%), soft indistinct drusen in 23 (2.5%), reticular drusen in one (0.1%), and drusen occupying greater than 50% of central zone 5 (0.5%).
Risk factor data
The crude baseline characteristics of participants by case status (ARM grades 2–4) are shown in Table 2 and the age-adjusted odds ratios are in Table 3. At baseline, older men, lower total and VLDL triglycerides, CRP, increased use of lard and solid vegetable oil, or eating fried foods with solid fats all predicted an increased risk of maculopathy (Table 2), which was unlikely to be due to chance. The age-adjusted analysis revealed the same risk factors with the exception of VLDL triglycerides (Table 3). Surprisingly, heavy smokers in phase I had only a modestly elevated risk, which was consistent with chance. This result was not changed when we repeated the analysis using smoking data at phases II and III (results not shown). Associations for social class, alcohol intake, BP, BMI, blood glucose, white cell count, fibrinogen, and D-dimer levels were also consistent with chance variation.
Table 2. Baseline characteristics of participants according to AMD statusa.
| Characteristics | Controls grades 0–1 (n=843) | Cases grades 2–4 (n=91) | P-value |
|---|---|---|---|
| Age in years (mean, SD) | 71.0 (4.2) | 72.2 (4.1) | 0.02 |
| Social classb | 0.90 | ||
| Non-manual | 337 (40.0) | 37 (40.7) | |
| Manual | 506 (60.0) | 54 (59.3) | |
| BMI in kg/m2 (mean, SD) | 25.6 (3.0) | 25.9 (2.6) | 0.37 |
| Smoking habit | 0.90 | ||
| Never smoked | 174 (20.7) | 17 (18.7) | |
| Ex smoker | 329 (39.1) | 39 (42.9) | |
| Cigar/pipe/1–14 cigarettes per day | 171 (20.3) | 17 (18.7) | |
| >15 cigarettes per day | 168 (20.0) | 18 (19.8) | |
| Alcohol consumption | 0.63 | ||
| <1 unit per week | 211 (25.0) | 28 (30.8) | |
| ≥1 unit to ≤18 units per week | 208 (24.7) | 21 (23.1) | |
| >18 units to ≤60 units per week | 222 (26.3) | 24 (26.4) | |
| >60 units per week | 202 (24.0) | 18 (19.8) | |
| Haemodynamic measures in mm Hg (mean, SD) | |||
| Systolic | 135.2 (20.8) | 137.9 (20.8) | 0.24 |
| Diastolic | 85.4 (12.8) | 87.9 (11.6) | 0.08 |
| Pulse pressure | 49.9 (13.4) | 50.1 (14.3) | 0.89 |
| Mean arterial pressure | 102.0 (14.6) | 104.6 (13.8) | 0.11 |
| Blood lipids in mmol/l (mean, SD) | |||
| Total cholesterol | 5.8 (1.2) | 5.9 (1.1) | 0.78 |
| LDL cholesterol | 4.0 (1.1) | 4.1 (1.1) | 0.48 |
| HDL cholesterol | 1.1 (0.4) | 1.2 (0.4) | 0.32 |
| VLDL cholesterol | 0.9 (0.6) | 0.9 (0.8) | 0.55 |
| Total triglycerides | 1.6 (1.0) | 1.4 (0.7) | 0.04 |
| VLDL triglyceride | 0.9 (0.7) | 0.7 (0.6) | 0.05 |
| Glucose in mmol/l (mean, SD) | 5.0 (0.9) | 4.8 (0.5) | 0.11 |
| Inflammatory markers (mean, SD) | |||
| White cell count (109 cells/l) | 6.7 (1.8) | 6.8 (1.7) | 0.89 |
| Fibrinogen (g/l) | 1.4 (0.3) | 1.4 (0.2) | 0.68 |
| CRP (mg/l) | 2.3 (3.3) | 3.2 (4.4) | 0.03 |
| D-dimer (ng/ml) | 49.7 (57.9) | 43.7 (23.2) | 0.37 |
| Dietary intakec | |||
| Average family use of lard or solid vegetable oil | 0.04 | ||
| None | 70 (35.4) | 4 (15.4) | |
| 1–200 oz per week | 128 (64.6) | 22 (84.6) | |
| Frequency of eating home fried food using solid fats | <0.001 | ||
| <1 time a week | 115 (56.1) | 4 (15.4) | |
| 1–7 times a week | 90 (43.9) | 22 (84.6) | |
Abbreviations: SD, standard deviation; BMI, body mass index; LDL, low density lipoprotein; HDL, high density lipoprotein; VLDL, very low density lipoprotein; CRP, C-reactive protein.
Statistically significant data are highlighted in bold.
Data are given in no (%) unless otherwise indicated.
Social classes I, II, and III (non-manual); manual includes social classes III (manual), IV, V.
Dietary data were only collected on a random subset of 231 (25%) subjects in phase II (1984–1988).
Table 3. Univariable age-adjusted analysis of risk factors for cases (ARM grades 2–4).
| Risk factor | Odds ratio | Confidence interval | P-value |
|---|---|---|---|
| Age group | |||
| 45.6–50.9 | 1 | ||
| 51–54.9 | 1.58 | 0.84–2.97 | 0.15 |
| 55–58.5 | 2.57 | 1.38–4.79 | 0.003 |
| 58.6–63.6 | 2.23 | 1.14–4.34 | 0.02 |
| P-value for trend | 1.34 | 1.10–1.63 | 0.004 |
| Social class | |||
| Non-manual | 1 | ||
| Manual | 0.97 | 0.62–1.50 | 0.88 |
| Smoking habit | |||
| Never smoked | 1 | ||
| Ex smoker | 1.12 | 0.61–2.04 | 0.72 |
| Cigar/pipe/1–14 cigarettes per day | 0.95 | 0.47–1.94 | 0.90 |
| >15 cigarettes per day | 1.12 | 0.56–2.26 | 0.75 |
| P-value for trend | 1.01 | 0.82–1.26 | 0.91 |
| Alcohol consumption | |||
| <1 unit per week | 1 | ||
| ≥1 unit to ≤18 units per week | 0.81 | 0.44–1.49 | 0.50 |
| >18 units to ≤60 units per week | 0.82 | 0.46–1.47 | 0.51 |
| >60 units per week | 0.68 | 0.36–1.27 | 0.22 |
| P-value for trend | 0.89 | 0.73–1.08 | 0.25 |
| Haemodynamic measures | |||
| Systolic blood pressurea | 1.09 | 0.86–1.38 | 0.47 |
| Diastolic blood pressurea | 1.22 | 0.97–1.53 | 0.08 |
| Pulse pressurea | 0.93 | 0.72–1.21 | 0.61 |
| Mean arterial pressurea | 1.17 | 0.93–1.47 | 0.18 |
| BMIa | 1.10 | 0.86–1.40 | 0.45 |
| Blood lipids | |||
| Total cholesterola | 1.04 | 0.83–1.31 | 0.74 |
| LDL cholesterola | 1.10 | 0.87–1.38 | 0.43 |
| HDL cholesterola | 1.08 | 0.88–1.33 | 0.44 |
| VLDL cholesterola | 1.09 | 0.89–1.33 | 0.41 |
| Total triglyceridesa | 0.73 | 0.54–1.00 | 0.05 |
| VLDL triglyceridea | 0.76 | 0.57–1.02 | 0.07 |
| Glucosea | 0.62 | 0.37–1.06 | 0.08 |
| Inflammatory markers | |||
| White cell counta | 1.01 | 0.84–1.23 | 0.89 |
| Fibrinogen levelsa | 1.03 | 0.81–1.30 | 0.82 |
| CRPa | 1.33 | 1.00–1.77 | 0.05 |
| D-dimera | 0.74 | 0.42–1.31 | 0.31 |
| Dietary intake | |||
| Average family use of lard or solid vegetable oil | |||
| None | 1 | ||
| 1–200 oz per week | 3.27 | 1.07–10.01 | 0.04 |
| Frequency of eating home fried food using solid fats | |||
| <1 time a week | 1 | ||
| 1–7 times a week | 6.85 | 2.26–20.77 | 0.001 |
P-values less than 0.05 are highlighted in bold.
Values are standardised and z-scored.
Further multivariable logistic regression analyses showed that adjustment for social class (model 1) or for smoking and alcohol (model 2) made little difference to the results (table of data not shown). Mutual adjustment for the metabolic and inflammatory measures was performed to adjust for further potential confounders and/or intermediaries that may contribute to the development of AMD. When lifestyle measures (model 2: age, smoking, and alcohol) were adjusted in the analysis the associations of AMD with lower levels of triglycerides and raised CRP were attenuated (OR CRP: 1.33, 95% CI 0.99, 1.77, P=0.05; OR triglycerides: 0.73 95% CI 0.54, 1.00, P=0.05). Older age was predictably associated with AMD (OR for trend: 1.33, 95% CI 1.09, 1.62, P=0.006). When anthropometric and metabolic factors were adjusted together (model 3), the association of AMD and age was maintained (see Table 4). Higher baseline systolic, diastolic, and mean arterial BPs were shown to be associated with AMD with modest evidence against the null hypothesis. Again, higher serum total triglycerides were shown to be protective in the development of AMD.
Table 4. Multivariable analysis of risk factors for AMD cases (ARM grades 2–4), adjusting for systolic BP, CRP, total cholesterol, total triglyceride, BMI and blood glucose.
| Risk factor | Odds ratio | Confidence interval | P-value |
|---|---|---|---|
| Age group | |||
| 45.6–50.9 | 1 | ||
| 51–54.9 | 1.65 | 0.78–3.49 | 0.19 |
| 55–58.5 | 2.36 | 1.11–5.01 | 0.03 |
| 58.6–63.6 | 2.63 | 1.22–5.67 | 0.01 |
| P-value for trend | 1.37 | 1.09–1.73 | 0.007 |
| Social class | |||
| Non-manual | 1 | ||
| Manual | 0.82 | 0.50–1.36 | 0.45 |
| BMIa | 1.24 | 0.93–1.64 | 0.14 |
| Smoking habit | |||
| Never smoked | 1 | ||
| Ex smoker | 1.17 | 0.60–2.26 | 0.65 |
| Cigar/pipe/1–14 cigarettes per day | 0.75 | 0.33–1.72 | 0.49 |
| >15 cigarettes per day | 1.02 | 0.46–2.22 | 0.97 |
| Alcohol consumption | |||
| <1 unit per week | 1 | ||
| ≥1 unit to ≤18 units per week | 0.76 | 0.39–1.48 | 0.42 |
| >18 units to ≤60 units per week | 0.56 | 0.28–1.11 | 0.10 |
| >60 units per week | 0.59 | 0.29–1.19 | 0.14 |
| P-value for trend | 0.82 | 0.66–1.03 | 0.09 |
| Haemodynamic measures | |||
| Systolic blood pressurea | 1.34 | 1.01–1.76 | 0.04 |
| Diastolic blood pressurea,b | 1.35 | 1.03–1.77 | 0.03 |
| Pulse pressurea,b | 1.18 | 0.89–1.57 | 0.26 |
| Mean arterial pressurea,b | 1.37 | 1.04–1.79 | 0.02 |
| Blood lipids | |||
| Total cholesterola | 1.08 | 0.82–1.42 | 0.57 |
| LDL cholesterola | 0.89 | 0.43–1.87 | 0.77 |
| HDL cholesterola | 1.04 | 0.81–1.32 | 0.77 |
| VLDL cholesterola | 1.25 | 0.86–1.82 | 0.24 |
| Total triglyceridesa | 0.68 | 0.47–0.99 | 0.04 |
| VLDL triglyceridea | 0.70 | 0.44–1.11 | 0.13 |
| Glucosea | 0.60 | 0.32–1.11 | 0.11 |
| Inflammatory markers | |||
| White cell counta | 0.94 | 0.71–1.25 | 0.67 |
| Fibrinogena | 1.00 | 0.76–1.32 | 1.00 |
| CRPa | 1.28 | 0.93–1.75 | 0.13 |
| D-dimera | 0.72 | 0.39–1.34 | 0.30 |
P-values <0.05 are highlighted in bold.
Values are standardised and z-scored.
Blood pressure variables were not adjusted by systolic BP due to co-linearity.
Dietary data was analysed separately from the main analysis (because of the limited sample number). Lower concentrations of serum total triglycerides and VLDL triglyceride, as well as higher CRP remained predictive in this subgroup analysis. Consistent with the univariable analysis, a higher use of lard or solid fats and increased frequency of eating home fried food using solid fats were the only dietary variables shown to be associated with an increased prevalence of AMD in this model of multivariate analysis (OR lard: 3.19, 95% CI 1.04, 9.80, P=0.04; OR fried food: 8.35, 95% CI 1.96, 35.66, P=0.004).
Discussion
This is the second large population-based screening study of AMD in the United Kingdom. The prevalence of AMD in this study was lower than that reported in the Beaver Dam (BDES, 1.2%, males), Rotterdam (RS, 1.4%, males), Blue Mountains Eye Study (BMES) (1%, males), Chesapeake Bay Watermen (1.3%), the European eye study (EUREYE, 2.5%, males), the Eye diseases prevalence research group (Eye diseases PRG, 0.63–3.97%, white males), Cardiovascular health study (CHS, 1.4%, white males), and Melton Mowbray (1.9% exudative AMD, 1.9% GA),1, 4, 33, 34, 35, 36, 37, 38 but it is comparable to the Visual Impairment Project39 (VIP, 0.58%, males) and the Colorado-Wisconsin Study40 (0.53%, age-standardised to VIP study). In part this may be due to differences in grading between studies; however, the grading system used in our study was almost identical to that used in the RS. Although the average age in the Speedwell study was greater than several of the other studies (BDES 61.8 years, RS 69.0 years, BMES 66.1 years), we had an upper age limit of 83 years while in some of the other studies this was unrestricted. This might account for some of the difference, as the risk for AMD rises with age. A third possible issue is selection bias; men who did not attend may be more likely to have AMD (due to inability/disability to attend) or equally more willing to participate, if they have AMD (to seek medical attention), though our response rate of 86.4% for any clinical information and 70.7% for the eye examination is similar to other studies.35, 36 Virtually all the non-responders were contacted by phone or their medical records were checked. If we add the three men identified as having AMD from their clinical records to our estimate, the prevalence of 0.9% (95% CI 0.4%, 1.7%), although lower, is consistent with other estimates in the literature.
Hypopigmentation was seen in 9.6% of participants and hyperpigmentation in 10.4%. These figures are slightly higher than those found in the RS,35 VIP,41 or Colorado–Wisconsin40 studies but less than the BDES,34 BMES,33 and Melton Mowbray4 studies. Several studies have shown a greater risk of developing future AMD given the presence of these milder abnormalities.29, 42, 43, 44 Considering the increase in life expectancy due to age-specific reductions in cardiovascular mortality, more men will survive to develop AMD in the future with inevitable health consequences.
Potential risk factors for AMD
We found that age, higher blood levels of CRP and lower blood levels of triglycerides were associated with a higher risk of developing ARM/AMD. Following multivariable adjustment for metabolic factors, subjects with ARM/AMD also had higher baseline systolic, diastolic, and mean arterial BPs. The only dietary variables that potentially predicted the risk for developing ARM/AMD were higher intakes of lard or solid fats and fried food using solid fats.
In this study, socioeconomic status was not associated with ARM/AMD, similar to other studies21, 45, 46, 47 that have used educational level as a surrogate indicator of socioeconomic status.48, 49, 50 In contrast to previously published reports, this study showed no evidence that smoking at baseline was associated with ARM/AMD,15, 45, 51, 52, 53, 54, 55, 56 although this is not seen consistently across studies.19, 41, 57, 58 Pooled analysis of BDES, BMES and the Rotterdam study showed a threefold association of current smoking at baseline with the development of AMD,16 whereas the Nurses' health59 and the Physicians' health56 studies both observed positive dose-related associations between smoking and AMD. Analysis of data in later phases showed an age-related decline in smoking prevalence, however, this did not change our findings. We suspect that our negative findings most likely reflect a type II error or a healthy survivor effect, which will differ between populations because of variations in competing causes of death.
We found that baseline serum levels of CRP (measured in Phase II), a marker of systemic inflammation, was associated with ARM/AMD. This result strengthens the previously reported findings from prospective60, 61, 62 and cross-sectional studies63, 64, 65, 66 and supports the hypothesis that the pathogenesis of AMD may be inflammatory or immune-related. Drusen, one of the pathological hallmarks of AMD, contain inflammatory proteins such as fibrinogen, vitronectin, complement, and CRP.67, 68 This association, however, may reflect reverse causation despite the relatively long latency between exposure and outcome measures. Recent epidemiological work has failed to find associations between functional genetic variants associated with elevated CRP levels and coronary heart disease.69 Furthermore, adjustment for other metabolic factors attenuated this association, which is in agreement with another study,70 suggesting that either these factors may mediate the association or they both share a common antecedent.
Surprisingly, there was an inverse relationship between fasting serum triglyceride lipid levels and the VLDL subfraction with AMD risk, which is counterintuitive to the hypothesis that the pathogenesis of AMD is related to atherosclerosis.20 Other epidemiological studies have found either no,46, 71, 72, 73, 74 a positive association21 or an inverse association between serum lipids and ARM/AMD.16, 22, 38, 75, 76 More recent studies are difficult to interpret because of the wide-spread use of lipid-lowering medication, which may have a pharmacological effect independent of their effects on lipids. However, this cannot account for our findings as in the 1980s, few men would have been on lipid-lowering therapies and this predates the statin era. The reasons for these discrepancies are unclear. Furthermore, our study reports that an increased dietary intake of solid fats (lard, solid vegetable oils) and food fried in solid fats were independent risk factors in the development of AMD, despite no change in serum cholesterol levels or BMI. Other studies have shown similar results.23, 77, 78 This would be consistent with the idea that AMD, cardiovascular disease and atherosclerosis may share a similar pathogenesis, however, one must be cautious with such associations because of the possibility of residual confounding, as dietary intakes are strongly associated with other lifestyle and sociodemographic factors.
In this study, higher systolic, diastolic and mean arterial BPs were associated with an increased risk of ARM/AMD. Hypertension has been postulated as a risk factor for AMD through its deleterious functions on the choroidal circulation.20, 79 Similar associations have been found by others.38, 46, 47, 80, 81 However, other studies have failed to find an association,16, 45, 72, 73, 74, 81, 82, 83 and to our knowledge there are no reports of a reduction in risk of AMD in those being treated for hypertension.20, 45, 84
Strengths and limitations
This study has prospective risk factor data on a longer period than any other studies to the best of our knowledge. This greatly reduces the chance that any associations are secondary to reverse causation or ascertainment bias, whereby subjects with co-morbidity are more like to have ARM/AMD detected due to greater clinical surveillance. The generalisability of our findings are limited to Caucasian men though, as we note above many of our associations have been seen in other studies including women. Another major limitation is the relatively small number of cases that we had available for analysis. At 80% power and 5% significance, we could detect a doubling of the odds ratios or more but not more modest effects.
Conclusions
We have found that AMD and ARM are moderately common in an unselected sample of elderly white men living in South West England. Long-term risk factor data suggest associations with several cardiovascular risk factors and poor diet, yet there may be a paradoxical association with triglyceride levels, which remains unexplained. Improvements in cardiovascular health may result in an increasing burden of AMD in the community due to longer survival, unless this is counterbalanced by any beneficial effects from better risk-factor control. Long-term trend data on incidence rate will help confirm or refute a shared cardiovascular mechanism.
Acknowledgments
We would like to thank Research into Ageing and the National Eye Research Centre for funding this research and the Bristol Eye Hospital for providing suitable facilities for performing the eye examinations. We would like to acknowledge the assistance given by Hans Vingerling and Paulus de Jong in the preparation of data for analysis.
The authors declare no conflict of interest.
Footnotes
Ethics approval
The study was approved by the following research ethic committees: Frenchay Health Care Trust, United Bristol Health Care Trust and South and West Local Research Ethics committee.
References
- Congdon N, O'Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122 (4:477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- Bunce C, Wormald R. Causes of blind certifications in England and Wales: April 1999–March 2000. Eye. 2008;22 (7:905–911. doi: 10.1038/sj.eye.6702767. [DOI] [PubMed] [Google Scholar]
- Lotery A, Xu X, Zlatava G, Loftus J. Burden of illness, visual impairment and health resource utilisation of patients with neovascular age-related macular degeneration: results from the UK cohort of a five-country cross-sectional study. Br J Ophthalmol. 2007;91 (10:1303–1307. doi: 10.1136/bjo.2007.116939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson AJ, Sparrow JM, Duke AM, Thompson JR, Gibson JM, Rosenthal AR. Prevalence of age-related maculopathy at two points in time in an elderly British population. Eye. 1997;11 (Pt 3:301–314. doi: 10.1038/eye.1997.66. [DOI] [PubMed] [Google Scholar]
- Sparrow JM, Dickinson AJ, Duke AM, Thompson JR, Gibson JM, Rosenthal AR. Seven year follow-up of age-related maculopathy in an elderly British population. Eye. 1997;11 (Pt 3:315–324. doi: 10.1038/eye.1997.67. [DOI] [PubMed] [Google Scholar]
- Das BN, Thompson JR, Patel R, Rosenthal AR. The prevalence of eye disease in Leicester: a comparison of adults of Asian and European descent. J R Soc Med. 1994;87 (4:219–222. [PMC free article] [PubMed] [Google Scholar]
- Gibson JM, Rosenthal AR, Lavery J. A study of the prevalence of eye disease in the elderly in an English community. Trans Ophthalmol Soc UK. 1985;104 (Pt 2:196–203. [PubMed] [Google Scholar]
- Gray PJ. The prevalence of eye disease in elderly Bengalis in Tower Hamlets. J R Soc Med. 1996;89 (1:23–26. doi: 10.1177/014107689608900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey RH, Burns-Cox CJ, Hughes A. Blind and partial sight registration in Avon. Br J Ophthalmol. 1989;73 (2:88–94. doi: 10.1136/bjo.73.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JR, Du L, Rosenthal AR. Recent trends in the registration of blindness and partial sight in Leicestershire. Br J Ophthalmol. 1989;73 (2:95–99. doi: 10.1136/bjo.73.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wormald RP, Wright LA, Courtney P, Beaumont B, Haines AP. Visual problems in the elderly population and implications for services. BMJ. 1992;304 (6836:1226–1229. doi: 10.1136/bmj.304.6836.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augood CA, Vingerling JR, de Jong PT, Chakravarthy U, Seland J, Soubrane G, et al. Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE) Arch Ophthalmol. 2006;124 (4:529–535. doi: 10.1001/archopht.124.4.529. [DOI] [PubMed] [Google Scholar]
- Reidy A, Minassian DC, Vafidis G, Joseph J, Farrow S, Wu J, et al. Prevalence of serious eye disease and visual impairment in a north London population: population based, cross sectional study. BMJ. 1998;316 (7145:1643–1646. doi: 10.1136/bmj.316.7145.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans JR, Fletcher AE, Wormald RP. Age-related macular degeneration causing visual impairment in people 75 years or older in Britain: an add-on study to the Medical Research Council Trial of Assessment and Management of Older People in the Community. Ophthalmology. 2004;111 (3:513–517. doi: 10.1016/j.ophtha.2003.07.012. [DOI] [PubMed] [Google Scholar]
- Thornton J, Edwards R, Mitchell P, Harrison RA, Buchan I, Kelly SP. Smoking and age-related macular degeneration: a review of association. Eye. 2005;19 (9:935–944. doi: 10.1038/sj.eye.6701978. [DOI] [PubMed] [Google Scholar]
- Tomany SC, Wang JJ, van LR, Klein R, Mitchell P, Vingerling JR, et al. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology. 2004;111 (7:1280–1287. doi: 10.1016/j.ophtha.2003.11.010. [DOI] [PubMed] [Google Scholar]
- Vingerling JR, Dielemans I, Bots ML, Hofman A, Grobbee DE, de Jong PT. Age-related macular degeneration is associated with atherosclerosis. The Rotterdam Study. Am J Epidemiol. 1995;142 (4:404–409. doi: 10.1093/oxfordjournals.aje.a117648. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Tomany SC, Cruickshanks KJ. The association of cardiovascular disease with the long-term incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 2003;110 (6:1273–1280. doi: 10.1016/S0161-6420(03)00599-2. [DOI] [PubMed] [Google Scholar]
- Krishnaiah S, Das TP, Kovai V, Rao GN. Associated factors for age-related maculopathy in the adult population in southern India: the Andhra Pradesh Eye Disease Study. Br J Ophthalmol. 2009;93 (9:1146–1150. doi: 10.1136/bjo.2009.159723. [DOI] [PubMed] [Google Scholar]
- Klein R, Peto T, Bird A, Vannewkirk MR. The epidemiology of age-related macular degeneration. Am J Ophthalmol. 2004;137 (3:486–495. doi: 10.1016/j.ajo.2003.11.069. [DOI] [PubMed] [Google Scholar]
- The Eye Disease Case-Control Study Group. Risk factors for neovascular age-related macular degeneration Arch Ophthalmol 1992110(121701–1708. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Franke T. The relationship of cardiovascular disease and its risk factors to age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1993;100 (3:406–414. doi: 10.1016/s0161-6420(93)31634-9. [DOI] [PubMed] [Google Scholar]
- Cho E, Hung S, Willett WC, Spiegelman D, Rimm EB, Seddon JM, et al. Prospective study of dietary fat and the risk of age-related macular degeneration. Am J Clinl Nutr. 2001;73 (2:209–218. doi: 10.1093/ajcn/73.2.209. [DOI] [PubMed] [Google Scholar]
- Chua B, Flood V, Rochtchina E, Wang JJ, Smith W, Mitchell P. Dietary fatty acids and the 5-year incidence of age-related maculopathy. Arch Ophthalmol. 2006;124 (7:981–986. doi: 10.1001/archopht.124.7.981. [DOI] [PubMed] [Google Scholar]
- The Caerphilly and Speedwell Collaborative Group. Caerphilly and Speedwell collaborative heart disease studies J Epidemiol Community Health 198438(3259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocks N, Patel R, Sparrow J, Davey-Smith G. Prevalence of cataract in the Speedwell Cardiovascular Study: a cross-sectional survey of men aged 65–83. Eye. 2002;16 (3:275–280. doi: 10.1038/sj.eye.6700106. [DOI] [PubMed] [Google Scholar]
- Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol. 1995;39 (5:367–374. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- Klein R, Davis MD, Magli YL, Segal P, Klein BE, Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology. 1991;98 (7:1128–1134. doi: 10.1016/s0161-6420(91)32186-9. [DOI] [PubMed] [Google Scholar]
- Klaver CC, Assink JJ, van LR, Wolfs RC, Vingerling JR, Stijnen T, et al. Incidence and progression rates of age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci. 2001;42 (10:2237–2241. [PubMed] [Google Scholar]
- Yarnell JW, Fehily AM, Milbank JE, Sweetnam PM, Walker CL. A short dietary questionnaire for use in an epidemiological survey: comparison with weighed dietary records. Hum Nutr Appl Nutr. 1983;37 (2:103–112. [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18 (6:499–502. [PubMed] [Google Scholar]
- The Caerphilly and Speedwell Collaborative Group. Caerphilly and Speedwell collaborative heart disease studies J Epidemiol Community Health 198438(3259–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology. 1995;102 (10:1450–1460. doi: 10.1016/s0161-6420(95)30846-9. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99 (6:933–943. doi: 10.1016/s0161-6420(92)31871-8. [DOI] [PubMed] [Google Scholar]
- Vingerling JR, Dielemans I, Hofman A, Grobbee DE, Hijmering M, Kramer CF, et al. The prevalence of age-related maculopathy in the Rotterdam Study. Ophthalmology. 1995;102 (2:205–210. doi: 10.1016/s0161-6420(95)31034-2. [DOI] [PubMed] [Google Scholar]
- Bressler NM, Bressler SB, West SK, Fine SL, Taylor HR. The grading and prevalence of macular degeneration in Chesapeake Bay watermen. Arch Ophthalmol. 1989;107 (6:847–852. doi: 10.1001/archopht.1989.01070010869032. [DOI] [PubMed] [Google Scholar]
- Augood CA, Vingerling JR, de Jong PT, Chakravarthy U, Seland J, Soubrane G, et al. Prevalence of age-related maculopathy in older Europeans: the European Eye Study (EUREYE) Arch Ophthalmol. 2006;124 (4:529–535. doi: 10.1001/archopht.124.4.529. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Marino EK, Kuller LH, Furberg C, Burke GL, et al. Early age-related maculopathy in the cardiovascular health study. Ophthalmology. 2003;110 (1:25–33. doi: 10.1016/s0161-6420(02)01565-8. [DOI] [PubMed] [Google Scholar]
- Vannewkirk MR, Nanjan MB, Wang JJ, Mitchell P, Taylor HR, McCarty CA. The prevalence of age-related maculopathy: the visual impairment project. Ophthalmology. 2000;107 (8:1593–1600. doi: 10.1016/s0161-6420(00)00175-5. [DOI] [PubMed] [Google Scholar]
- Cruickshanks KJ, Hamman RF, Klein R, Nondahl DM, Shetterly SM. The prevalence of age-related maculopathy by geographic region and ethnicity. The Colorado-Wisconsin Study of Age-Related Maculopathy. Arch Ophthalmol. 1997;115 (2:242–250. doi: 10.1001/archopht.1997.01100150244015. [DOI] [PubMed] [Google Scholar]
- Vannewkirk MR, Weih L, McCarty CA, Taylor HR. Cause-specific prevalence of bilateral visual impairment in Victoria, Australia: the Visual Impairment Project. Ophthalmology. 2001;108 (5:960–967. doi: 10.1016/s0161-6420(01)00554-1. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Tomany SC, Meuer SM, Huang GH. Ten-year incidence and progression of age-related maculopathy: The Beaver Dam eye study. Ophthalmology. 2002;109 (10:1767–1779. doi: 10.1016/s0161-6420(02)01146-6. [DOI] [PubMed] [Google Scholar]
- Wang JJ, Rochtchina E, Lee AJ, Chia EM, Smith W, Cumming RG, et al. Ten-year incidence and progression of age-related maculopathy: the blue Mountains Eye Study. Ophthalmology. 2007;114 (1:92–98. doi: 10.1016/j.ophtha.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Knudtson MD, Meuer SM, Swift M, Gangnon RE. Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology. 2007;114 (2:253–262. doi: 10.1016/j.ophtha.2006.10.040. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Mukesh BN, Fu CL, Mitchell P, Wang JJ, Taylor HR. Risk factors for age-related maculopathy: the Visual Impairment Project. Arch Ophthalmol. 2001;119 (10:1455–1462. doi: 10.1001/archopht.119.10.1455. [DOI] [PubMed] [Google Scholar]
- Kahn HA, Leibowitz HM, Ganley JP, Kini MM, Colton T, Nickerson RS, et al. The Framingham Eye Study. II. Association of ophthalmic pathology with single variables previously measured in the Framingham Heart Study. Am J Epidemiol. 1977;106 (1:33–41. doi: 10.1093/oxfordjournals.aje.a112429. [DOI] [PubMed] [Google Scholar]
- Goldberg J, Flowerdew G, Smith E, Brody JA, Tso MO. Factors associated with age-related macular degeneration. An analysis of data from the first National Health and Nutrition Examination Survey. Am J Epidemiol. 1988;128 (4:700–710. doi: 10.1093/oxfordjournals.aje.a115023. [DOI] [PubMed] [Google Scholar]
- Mueller CW, Parcel TL. Measures of socioeconomic status: alternatives and recommendations. Child Development. 1981;52:13–30. [Google Scholar]
- Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82 (6:816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121. doi: 10.1093/oxfordjournals.epirev.a036030. [DOI] [PubMed] [Google Scholar]
- Hawkins BS, Bird A, Klein R, West SK. Epidemiology of age-related macular degeneration. Mol Vis. 1999;5:26. [PubMed] [Google Scholar]
- Hyman LG, Lilienfeld AM, Ferris FL, III, Fine SL. Senile macular degeneration: a case-control study. Am J Epidemiol. 1983;118 (2:213–227. doi: 10.1093/oxfordjournals.aje.a113629. [DOI] [PubMed] [Google Scholar]
- Khan JC, Thurlby DA, Shahid H, Clayton DG, Yates JR, Bradley M, et al. Smoking and age related macular degeneration: the number of pack years of cigarette smoking is a major determinant of risk for both geographic atrophy and choroidal neovascularisation. Br J Ophthalmol. 2006;90 (1:75–80. doi: 10.1136/bjo.2005.073643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith W, Mitchell P, Leeder SR. Smoking and age-related maculopathy. The Blue Mountains Eye Study. Arch Ophthalmol. 1996;114 (12:1518–1523. doi: 10.1001/archopht.1996.01100140716016. [DOI] [PubMed] [Google Scholar]
- Cong R, Zhou B, Sun Q, Gu H, Tang N, Wang B. Smoking and the risk of age-related macular degeneration: a meta-analysis. Ann Epidemiol. 2008;18 (8:647–656. doi: 10.1016/j.annepidem.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Christen WG, Glynn RJ, Manson JE, Ajani UA, Buring JE. A prospective study of cigarette smoking and risk of age-related macular degeneration in men. JAMA. 1996;276 (14:1147–1151. [PubMed] [Google Scholar]
- Klein R, Klein BE, Linton KL, DeMets DL. The Beaver Dam Eye Study: the relation of age-related maculopathy to smoking. Am J Epidemiol. 1993;137 (2:190–200. doi: 10.1093/oxfordjournals.aje.a116659. [DOI] [PubMed] [Google Scholar]
- Bressler NM, Frost LA, Bressler SB, Murphy RP, Fine SL. Natural course of poorly defined choroidal neovascularization associated with macular degeneration. Arch Ophthalmol. 1988;106 (11:1537–1542. doi: 10.1001/archopht.1988.01060140705039. [DOI] [PubMed] [Google Scholar]
- Seddon JM, Willett WC, Speizer FE, Hankinson SE. A prospective study of cigarette smoking and age-related macular degeneration in women. JAMA. 1996;276 (14:1141–1146. [PubMed] [Google Scholar]
- Seddon JM, George S, Rosner B, Rifai N. Progression of age-related macular degeneration: prospective assessment of C-reactive protein, interleukin 6, and other cardiovascular biomarkers. Arch Ophthalmol. 2005;123 (6:774–782. doi: 10.1001/archopht.123.6.774. [DOI] [PubMed] [Google Scholar]
- Boekhoorn SS, Vingerling JR, Witteman JC, Hofman A, de Jong PT. C-reactive protein level and risk of aging macula disorder: The Rotterdam Study. Arch Ophthalmol. 2007;125 (10:1396–1401. doi: 10.1001/archopht.125.10.1396. [DOI] [PubMed] [Google Scholar]
- Schaumberg DA, Christen WG, Buring JE, Glynn RJ, Rifai N, Ridker PM. High-sensitivity C-reactive protein, other markers of inflammation, and the incidence of macular degeneration in women. Arch Ophthalmol. 2007;125 (3:300–305. doi: 10.1001/archopht.125.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seddon JM, Gensler G, Milton RC, Klein ML, Rifai N. Association between C-reactive protein and age-related macular degeneration. JAMA. 2004;291 (6:704–710. doi: 10.1001/jama.291.6.704. [DOI] [PubMed] [Google Scholar]
- Seddon JM, Gensler G, Klein ML, Milton RC. C-reactive protein and homocysteine are associated with dietary and behavioral risk factors for age-related macular degeneration. Nutrition. 2006;22 (4:441–443. doi: 10.1016/j.nut.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Vine AK, Stader J, Branham K, Musch DC, Swaroop A. Biomarkers of cardiovascular disease as risk factors for age-related macular degeneration. Ophthalmology. 2005;112 (12:2076–2080. doi: 10.1016/j.ophtha.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Boey PY, Tay WT, Lamoureux E, Tai ES, Mitchell P, Wang JJ, et al. C-reactive protein and age-related macular degeneration and cataract: the singapore malay eye study. Invest Ophthalmol Vis Sci. 2010;51 (4:1880–1885. doi: 10.1167/iovs.09-4063. [DOI] [PubMed] [Google Scholar]
- Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, et al. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci USA. 2002;99 (23:14682–14687. doi: 10.1073/pnas.222551899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson DH, Mullins RF, Hageman GS, Johnson LV. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol. 2002;134 (3:411–431. doi: 10.1016/s0002-9394(02)01624-0. [DOI] [PubMed] [Google Scholar]
- Elliott P, Chambers JC, Zhang W, Clarke R, Hopewell JC, Peden JF, et al. Genetic Loci associated with C-reactive protein levels and risk of coronary heart disease. JAMA. 2009;302 (1:37–48. doi: 10.1001/jama.2009.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasch B, Fuhs A, Behrens T, Meister A, Wellmann J, Fobker M, et al. Inflammatory markers in age-related maculopathy: cross-sectional analysis from the Muenster Aging and Retina Study. Arch Ophthalmol. 2005;123 (11:1501–1506. doi: 10.1001/archopht.123.11.1501. [DOI] [PubMed] [Google Scholar]
- Hyman L, Schachat AP, He Q, Leske MC. Hypertension, cardiovascular disease, and age-related macular degeneration. Age-Related Macular Degeneration Risk Factors Study Group. Arch Ophthalmol. 2000;118 (3:351–358. doi: 10.1001/archopht.118.3.351. [DOI] [PubMed] [Google Scholar]
- Smith W, Mitchell P, Leeder SR, Wang JJ. Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol. 1998;116 (5:583–587. doi: 10.1001/archopht.116.5.583. [DOI] [PubMed] [Google Scholar]
- Vinding T, Appleyard M, Nyboe J, Jensen G. Risk factor analysis for atrophic and exudative age-related macular degeneration. An epidemiological study of 1000 aged individuals. Acta Ophthalmologica. 1992;70 (1:66–72. doi: 10.1111/j.1755-3768.1992.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Delcourt C, Michel F, Colvez A, Lacroux A, Delage M, Vernet MH, et al. Associations of cardiovascular disease and its risk factors with age-related macular degeneration: the POLA study. Ophthal Epidemiol. 2001;8 (4:237–249. doi: 10.1076/opep.8.4.237.1613. [DOI] [PubMed] [Google Scholar]
- Klein BE, Klein R. Cataracts and macular degeneration in older Americans. Arch Ophthalmol. 1982;100 (4:571–573. doi: 10.1001/archopht.1982.01030030573002. [DOI] [PubMed] [Google Scholar]
- Sun C, Klein R, Wong TY. Age-related macular degeneration and risk of coronary heart disease and stroke: the Cardiovascular Health Study. Ophthalmology. 2009;116 (10:1913–1919. doi: 10.1016/j.ophtha.2009.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong EW, Robman LD, Simpson JA, Hodge AM, Aung KZ, Dolphin TK, et al. Fat consumption and its association with age-related macular degeneration. Arch Ophthalmol. 2009;127 (5:674–680. doi: 10.1001/archophthalmol.2009.60. [DOI] [PubMed] [Google Scholar]
- Seddon JM, Cote J, Rosner B. Progression of age-related macular degeneration: association with dietary fat, transunsaturated fat, nuts, and fish intake. Arch Ophthalmol. 2003;121 (12:1728–1737. doi: 10.1001/archopht.121.12.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman E. The role of the atherosclerotic process in the pathogenesis of age-related macular degeneration. Am J Ophthalmol. 2000;130 (5:658–663. doi: 10.1016/s0002-9394(00)00643-7. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Jensen SC. The relation of cardiovascular disease and its risk factors to the 5-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1997;104 (11:1804–1812. doi: 10.1016/s0161-6420(97)30023-2. [DOI] [PubMed] [Google Scholar]
- van LR, Ikram MK, Vingerling JR, Witteman JC, Hofman A, de Jong PT. Blood pressure, atherosclerosis, and the incidence of age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci. 2003;44 (9:3771–3777. doi: 10.1167/iovs.03-0121. [DOI] [PubMed] [Google Scholar]
- Tan JS, Mitchell P, Smith W, Wang JJ. Cardiovascular risk factors and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study. Ophthalmology. 2007;114 (6:1143–1150. doi: 10.1016/j.ophtha.2006.09.033. [DOI] [PubMed] [Google Scholar]
- Vingerling JR, Klaver CC, Hofman A, de Jong PT. Epidemiology of age-related maculopathy. Epidemiol Rev. 1995;17 (2:347–360. doi: 10.1093/oxfordjournals.epirev.a036198. [DOI] [PubMed] [Google Scholar]
- Douglas IJ, Cook C, Chakravarthy U, Hubbard R, Fletcher AE, Smeeth L. A case-control study of drug risk factors for age-related macular degeneration. Ophthalmology. 2007;114 (6:1164–1169. doi: 10.1016/j.ophtha.2006.09.018. [DOI] [PubMed] [Google Scholar]


