Abstract
Aim
To analyze relative weight gain by 2-week intervals up to 6 weeks after birth in order to predict the development of retinopathy of prematurity (ROP) requiring treatment among very low birth weight (BW) infants.
Methods
A prospective study including infants with BW ≤1500 g born in a single tertiary intensive care unit over 1-year period was conducted. Body weight measurements were recorded weekly and relative weight gains (g/kg/day) were calculated. The main outcome was development of ROP requiring treatment.
Results
Mean BW and gestational age (GA) of the whole cohort were 1165±223 g and 29.3±2.3 weeks, respectively. Relative weight gain at 2 weeks and 4 weeks postnatal age were significantly lower in infants with severe ROP (P=0.041 and P=0.017, respectively). Relative weight gain at 6 weeks was not different between groups. Infants with severe ROP gained 6.7±4 g/kg/day in the first 4 weeks of life, compared with 9.3±4.5 g/kg/day for those with mild or no ROP. After adjusted for BW and GA in logistic regression poor relative weight gain in the first 4 weeks was found to be related to severe ROP (P=0.015). When all the other risk factors significant for severe ROP were included in the logistic regression poor weight gain did not arise as an independent risk factor.
Conclusion
Poor postnatal weight gain in the first 4 weeks of life is the end result of several comorbidities rather than being an independent risk factor. Poor weight gain can be an additional predictor of severe ROP in very low BW infants.
Keywords: retinopathy of prematurity, weight gain, risk factors
Introduction
Retinopathy of prematurity (ROP) is a major cause of preventable blindness in children all over the world.1, 2, 3 It is a disease of the retina associated with preterm birth in which retinal blood vessels fail to grow and develop normally. ROP is a multifactorial disease. Low gestational age (GA), low birth weight (BW), oxygen therapy, blood transfusion, and several well-known morbidities of prematurity, such as necrotizing enterocolitis (NEC), sepsis, intraventricular hemorrhage (IVH) are shown to be associated with ROP.4, 5, 6 Recent data suggest that one of the strongest predictors of ROP is poor weight gain during the first weeks of life.7, 8, 9, 10, 11
In this prospective study, we aimed to evaluate relative weight gain by 2 weeks intervals up to 6 weeks after birth in order to predict the development of ROP requiring treatment among very low birth weight (VLBW) infants.
Patients and methods
In this prospective study, preterm infants born with BW ≤1500 g at Zekai Tahir Burak Maternity Hospital, Ankara, Turkey between March 2009 and March 2010 were recruited. Neonates with hydrocephalus, congenital anomalies, those who died or lost to follow-up before development of ROP requiring treatment or full vascularization of the retina were excluded. The study was approved by the hospital ethics committee and informed written consent was obtained from the parents or guardians before enrollment.
The first eye examination was performed at the postnatal age of 4–6 weeks by two senior ophthalmologists. After pupillary dilation with application of mydriatic eye drops (2.5% phenylephrine and 0.5% tropicamide), the eyes were examined by a lid speculum, depressor, binocular indirect ophthalmoscope, and 20-diopter lenses. Staging of ROP was recorded according to the international classification of ROP.12 Each child was classified according to the most advanced ROP stage observed. Patients were divided in to two groups as having no ROP or mild ROP and severe ROP. In this study, mild ROP was defined as the ROP that did not meet the criteria for treatment and severe ROP was defined as that needed treatment. The criteria for treatment were: zone I any stage of ROP with plus disease or zone I stage 3 without plus and zone 2 stage 2 or 3 with plus disease as defined by Early Treatment for Retinopathy of Prematurity Cooperative Group.13 Follow-up examinations were performed once or twice a week depending on the severity of the disease until the eyes were fully vascularized. The main clinical outcome was occurrence of severe ROP requiring treatment.
Body weight measurements weekly up to 6 weeks chronological age and day of regain of BW were recorded. Relative weight gains (body weight minus BW, divided by BW and chronological age, g/kg/day) at second, fourth, and sixth week were calculated. The data recorded for each neonate also included GA, BW, gender, 5-min APGAR score, oxygen therapy, mechanical ventilation, respiratory distress syndrome (RDS), hemodynamically significant patent ductus arteriosus (PDA), culture proven sepsis, NEC (≥stage 2), IVH (grade 3 or 4), and transfusion volumes.
Statistical analyses were conducted using the SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). The results are presented as numbers (n), frequencies (%), means with respective standard deviation (SD) and as medians with their interquartile ranges (IQR). Non-parametric tests were used to analyze continuous variables. Chi-square test was used to compare categorical variables. Statistical significance was accepted P<0.05. Two different logistic regression models were used. In the first model BW, GA, relative weight gain at second and fourth week of life were analyzed. In the second model, all the risk factors found to be significant in univariate analysis were included. Backward stepwise method was used in logistic regression. Odds ratios and 95% confidence intervals for each risk factor were determined. Receiver operating characteristic (ROC) curve was used for determination of the best discriminative cut-off of relative weight gain at fourth week of life to predict severe ROP.
Results
During the study period among the infants admitted to our NICU, 487 infants fulfilled the inclusion criteria. Complete clinical and eye examination data were available for 300 patients, 149 (49%) of whom were male. Mean BW and GA for the total cohort was 1165±223 g (range 600–1500 g) and 29.3±2.3 weeks (range 23–34 weeks), respectively. Of the total cohort 67 (22.3%) of the infants were <1000 g BW. Severe ROP needing treatment occurred in 21 babies (7%). Patients with severe ROP had significantly lower BW (959±185 g, range 680–1400 g, P<0.001) and GA (27.2±1.9 weeks, range 24–31 weeks, P<0.001) compared with those with mild ROP and no ROP. Male gender (P=0.033), PDA (P<0.001), NEC (P=0.03), and culture proven sepsis (P<0.001) were more common in patients with severe ROP. Transfusion volume (P<0.001), number of days on mechanical ventilation (P<0.001), and supplemental O2 (P<0.001) were significantly higher among patients with severe ROP. Relative weight gain at second and fourth week of life were significantly lower in infants with severe ROP (P=0.041 and P=0.017, respectively). Relative weight gain at sixth week was not different between groups. Infants with severe ROP gained 6.7±4 g/kg/day in the first 4 weeks of life, compared with 9.3±4.5 g/kg/day for those with mild or no ROP. Infants with severe ROP required longer time to regain BW (P=0.003). RDS and IVH were not associated with increased risk of severe ROP (Table 1).
Table 1. Univariate analysis of risk factors for the development of severe ROP.
| No ROP/Mild ROP (n=279) | Severe ROP (n=21) | P-value | |
|---|---|---|---|
| Gestational age (week)a | 29.4±2.2 (23–33) | 27.2±1.9 (24–31) | <0.001 |
| Birth weight (g)a | 1182±219 (600–1500) | 959±185 (680–1400) | <0.001 |
| Sex (M/F) | 132/147 | 15/6 | 0.003 |
| Relative weight gain at 2 weeks (g/kg/day)a | 2.6±5.8 (−21.7–17.8) | −0.004±6.9 (−11.3–17.1) | 0.041 |
| Relative weight gain at 4 weeks (g/kg/day)a | 9.3±4.5 (−8.1–21.8) | 6.7±4.0 (−0.9–13.7) | 0.017 |
| Relative weight gain at 6 weeks (g/kg/day)a | 12.1±4.7 (−0.63–28.6) | 9.9±5.7 (0.0–19.6) | 0.133 |
| Time to regain birth weight (day)b | 10±7 (4–33) | 14±8 (8–30) | 0.003 |
| 5-min APGARb | 8±2 (3–10) | 7±3 (3–10) | 0.063 |
| Days on MVb | 0±1 (0–20) | 6±9 (0–28) | <0.001 |
| Total days on supplemental O2b | 5±9 (0–102) | 44±45 (0–121) | <0.001 |
| PDA | 74 (26.5%) | 15 (71.4%) | <0.001 |
| RDS | 111 (40%) | 12 (57%) | 0.119 |
| Proven sepsis | 91(32.6%) | 16 (76.2%) | <0.001 |
| NEC (≥stage2) | 11 (4%) | 3 (14.3%) | 0.03 |
| IVH (grade 3 or 4) | 23 (8%) | 3 (14.3%) | 0.343 |
| Transfusion volume (ml)a | 24±22.7 (0–128) | 57.1±29 (13–110) | <0.001 |
Abbreviations: IVH, intraventricular hemorrhage; NEC, necrotizing enterocolitis; PDA, patent ductus arteriosus; RDS, respiratory distress syndrome.
Data presented as mean±SD, min–max values are given in parenthesis.
Data presented as median±interquartile range.
Birth weight, GA, relative weight gain at second and fourth week of life were put into a logistic regression model and relative weight gain in the first 4 weeks (P=0.015) besides BW (P<0.001) were found to be independently related to severe ROP (Table 2). When all the risk factors found to be significant in univariate analysis were put in to a logistic regression model BW (P=0.061), duration on MV (P<0.001), PDA (P=0.006), proven sepsis (P=0.007) were independent risk factors and poor weight gain did not arise as an independent risk factor at this model (Table 3).
Table 2. Relative weight gain adjusted for birth weight and gestational age in logistic regression model.
| Adjusted odds ratio | 95% confidence interval | P-value | |
|---|---|---|---|
| Birth weighta | 0.99 | 0.994–0.998 | <0.001 |
| Relative weight gain at 4 weeks (g/kg/day) | 0.88 | 0.795–0.976 | 0.015 |
OR for every 1 gram.
Table 3. Independent risk factors for severe retinopathy of prematurity.
| Adjusted odds ratio | 95% confidence interval | P-value | |
|---|---|---|---|
| Birth weighta | 0.99 | 0.995–1.000 | 0.061 |
| Mechanical ventilationb | 1.20 | 1.095–1.331 | <0.001 |
| PDA | 5.07 | 1.593–16.164 | 0.006 |
| Proven sepsis | 5.36 | 1.575–18.277 | 0.007 |
Abbreviation: PDA, patent ductus arteriosus.
OR for every 1 gram.
OR for each day on mechanical ventilation.
Receiver operating curve analysis revealed a cut-off of 9.1 g/kg/day weight gain in the first 4 weeks of life (area under the curve: 0.656, 95% confidence interval: 0.542–0.770, P=0.017) with a sensitivity of 76.2% and specificity of 50.4% for detection of ROP requiring treatment. We divided the cohort in to two groups as low weight gain and high weight gain groups using 9.1 g/kg/day weight gain cut-off. Days on mechanical ventilation (P<0.001) and supplemental oxygen (P<0.001), PDA (P=0.038), NEC (P=0.009) and transfusion volume (P=0.026) were higher in the low weight gain group.
Discussion
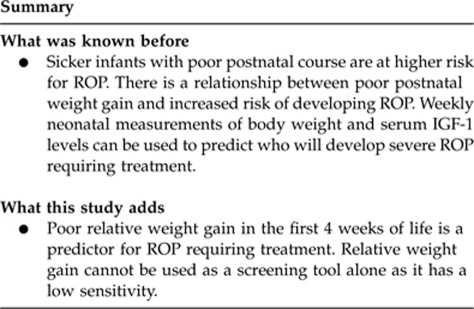
Current screening guidelines for ROP use only GA and BW as a criteria and does not take postnatal factors into consideration. However, it is widely accepted that sicker infants with poor postnatal course are at higher risk for ROP. Identifying postnatal factors that can be used to predict who will develop severe ROP requiring treatment would be beneficial for screening. A few studies reported a relationship between poor postnatal weight gain and increased risk of developing ROP. Wallace et al7 in a multiple regression model showed that GA and poor relative weight gain in the first 6 weeks of life were independent risk factors for ≥stage 3 ROP. In contrast, Allagaert et al8 found that poor absolute weight gain (g/day) but not relative weight gain in the first 6 weeks was associated with threshold ROP. Filho et al14 reported that low weight gain proportion (baby's weight measured at 6 weeks of life minus the BW, divided by the BW) under 51.2% of the BW at 6 weeks can predict severe ROP with a sensitivity of 66.3% and specificity of 62.6% in VLBW infants. Recently, an online surveillance system was developed in Sweden based on weekly neonatal measurements of body weight and serum IGF-1 levels. Weight IGF-1 Neonatal ROP (WINROP) algorithm was designed to detect a slowing of a rise in IGF-1 levels or weight gain compared with expected values of infants who have no ROP or only stage 1 ROP. It has 100% sensitivity to detect infants who will need treatment for ROP.9 Later it was shown that only serial weight measurement part of WINROP algorithm, excluding IGF-1 measurements, can also predict severe ROP requiring treatment with 100% sensitivity.10 This algorithm was validated in a different cohort of infants in Sweden and USA.11, 15 The first three studies we have mentioned were focused on weight gain during the first 6 weeks of life. With the WINROP algorithm, infants at risk were identified at a median age of 3.5 weeks after birth. In this study, we evaluated relative weight gain of VLBW infants at second, fourth, and sixth weeks of life. We found that relative weight gain at 2 and 4 weeks but not 6 weeks postnatal age were significantly lower in infants with severe ROP. When BW, GA, relative weight gain in second and fourth weeks of life are put in to a logistic regression model, BW and relative weight gain at 4 weeks were independently related to severe ROP. Weight loss and subsequent late regain of BW in the first 2 weeks of life is mostly related to degree of prematurity, so it lost significance in logistic regression. Relative weight gain at 4 weeks is related to ROP independent of GA and BW. Poor postnatal weight gain did not arise as an independent risk factor when all the other risk factors significant for severe ROP in univariate analysis were included in the logistic regression. We believe that poor weight gain is strongly associated with other risk factors in this model, therefore lost significance in logistic regression. Most of the morbidities related to prematurity are experienced in the first month of life. Thereafter most of the babies are in better general health and start to gain weight. This may explain why poor weight gain at 4 weeks postnatal age is better correlated with ROP than that at 6 weeks.
Poor postnatal weight gain in premature infants is caused by a combination of poor nutrition and poor postnatal outcome. Metabolic rate is increased in premature infants to compensate for heat loss. Rate of protein loss is high. Lung disease and sepsis increase energy consumption even more. Feeding intolerance and NEC are important factors contributing to insufficient enteral nutrition.16 In our cohort of VLBW infants, several well-defined morbidities of prematurity, such as PDA, NEC, respiratory support, and transfusion requirement were more common in infants with poor postnatal weight gain. Relation of poor postnatal weight gain and ROP may be attributed to common postnatal risk factors causing them. Poor postnatal weight gain is a good predictor but probably not an independent risk factor for ROP.
Role of prenatal growth restriction had been mentioned by some investigators. It was shown that infants born small-for-GA (SGA) were significantly more likely to develop ROP and more severe disease than infants born appropriate-for-GA.17 Darlow et al18 reported that infants below the 3rd percentile of weight for GA have four times greater odds of severe ROP than those between the 25th and 75th percentiles. Allagaert et al8 found that being SGA and BW below the 25th percentile are risk factors for threshold ROP. In our cohort, among infants with severe ROP only one patient was SGA.
In conclusion, results of this study suggest that poor relative weight gain in the first 4 weeks of life is a predictor for ROP requiring treatment. However, it cannot be used as a screening tool alone as it has a low sensitivity, but it can help to identify infants with poor postnatal course and are at greater risk. It is especially useful for the ophthalmologist at the time of the initial visit when he is not well informed about the postnatal course of the infant.
Acknowledgments
The study is not supported by any company.
The authors declare no conflict of interest.
References
- Munoz B, West SK. Blindness and visual impairment in the Americans and the Caribbean. Br J Ophthalmol. 2002;86:498–504. doi: 10.1136/bjo.86.5.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miada JM, Mathers K, Alley CL. Pediatric ophthalmology in the developing world. Curr Opin Ophthalmol. 2008;19:403–408. doi: 10.1097/ICU.0b013e328309f180. [DOI] [PubMed] [Google Scholar]
- Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, International NO-ROP Group et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115:e518–e525. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- Arrøe M, Peitersen B. Retinopathy of prematurity: review of a seven-year period in a Danish neonatal intensive care unit. Acta Paediatr. 1994;83:501–505. doi: 10.1111/j.1651-2227.1994.tb13067.x. [DOI] [PubMed] [Google Scholar]
- Fortes Filho JB, Eckert GU, Procianoy L, Barros CK, Procianoy RS. Incidence and risk factors for retinopathy of prematurity in very low and in extremely low birth weight infants in a unit-based approach in southern Brazil. Eye (Lond) 2009;23:25–30. doi: 10.1038/sj.eye.6702924. [DOI] [PubMed] [Google Scholar]
- Sears JE, Pietz J, Sonnie C, Dolcini D, Hoppe G. A change in oxygen supplementation can decrease the incidence of retinopathy of prematurity. Ophthalmology. 2009;116:513–518. doi: 10.1016/j.ophtha.2008.09.051. [DOI] [PubMed] [Google Scholar]
- Wallace DK, Kylstra JA, Phillips SJ, Hall JG. Poor postnatal weight gain: a risk factor for severe retinopathy of prematurity. J AAPOS. 2000;4:343–347. doi: 10.1067/mpa.2000.110342. [DOI] [PubMed] [Google Scholar]
- Allegaert K, Vanhole C, Casteels I, Naulaers G, Debeer A, Cossey V. Perinatal growth characteristics and associated risk of developing threshold retinopathy of prematurity. J AAPOS. 2003;7:34–37. doi: 10.1067/mpa.2003.S1091853102420150. [DOI] [PubMed] [Google Scholar]
- Löfqvist C, Andersson E, Sigurdsson J, Engström E, Hard A, Niklasson A. Longitudinal postnatal weight and insulin-like growth factor I measurements in the prediction of retinopathy of prematurity. Arch Ophthalmol. 2006;124:1711–1718. doi: 10.1001/archopht.124.12.1711. [DOI] [PubMed] [Google Scholar]
- Hellström A, Hård AL, Engström E, Niklasson A, Andersson E, Smith L, et al. Early weight gain predicts retinopathy in preterm infants: new, simple, efficient approach to screening. Pediatrics. 2009;123:e638–e645. doi: 10.1542/peds.2008-2697. [DOI] [PubMed] [Google Scholar]
- Löfqvist C, Hansen-Pupp I, Andersson E, Holm K, Smith LE, Ley D, et al. Validation of a new retinopathy of prematurity screening method monitoring longitudinal postnatal weight and insulin like growth factor I. Arch Ophthalmol. 2009;127:622–627. doi: 10.1001/archophthalmol.2009.69. [DOI] [PubMed] [Google Scholar]
- An International Classification of Retinopathy of Prematurity The committee for the classification of retinopathy of prematurity. Arch Ophthalmol. 1984;102:1130–1134. doi: 10.1001/archopht.1984.01040030908011. [DOI] [PubMed] [Google Scholar]
- Early Treatment For Retinopathy of Prematurity Cooperative Group Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–1694. doi: 10.1001/archopht.121.12.1684. [DOI] [PubMed] [Google Scholar]
- Fortes Filho JB, Bonomo PP, Maia M, Procianoy RS. Weight gain measured at 6 weeks after birth as a predictor for severe retinopathy of prematurity: study with 317 very low birth weight preterm babies. Graefes Arch Clin Exp Ophthalmol. 2009;247:831–836. doi: 10.1007/s00417-008-1012-3. [DOI] [PubMed] [Google Scholar]
- Wu C, VanderVeen DK, Hellström A, Löfqvist C, Smith LE. Longitudinal postnatal weight measurements for the prediction of retinopathy of prematurity. Arch Ophthalmol. 2010;128:443–447. doi: 10.1001/archophthalmol.2010.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellström A, Ley D, Hansen-Pupp I, Niklasson A, Smith L, Löfqvist C, et al. New insights into the development of retinopathy of prematurity--importance of early weight gain. Acta Paediatr. 2010;99:502–508. doi: 10.1111/j.1651-2227.2009.01568.x. [DOI] [PubMed] [Google Scholar]
- Dhaliwal CA, Fleck BW, Wright E, Graham C, McIntosh N. Retinopathy of prematurity in small-for-gestational age infants compared with those of appropriate size for gestational age. Arch Dis Child Fetal Neonatal Ed. 2009;94:193–195. doi: 10.1136/adc.2008.143552. [DOI] [PubMed] [Google Scholar]
- Darlow BA, Hutchinson JL, Handerson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics. 2005;115:990–996. doi: 10.1542/peds.2004-1309. [DOI] [PubMed] [Google Scholar]


