Sir,
The association between RP and exudative retinopathy was first reported by G. Zamorani in 1956.1 Coats'-like retinal changes are seen in 1–3% of patients affected by RP.2 The aetiology is unknown. Mutations in the Crumbs homologue 1 (CRB1) gene have been reported3 as a risk factor for developing Coats'-like changes in patients with autosomal recessive RP.
We present a case of a young patient with Coats'-like autosomal dominant retinitis pigmentosa (ADRP), exudative retinal detachment (E-RD), and cystoid macular oedema (CME), successfully treated with cryotherapy.
Case report
A 10-year-old boy presented at the Retina Clinic in Southampton Eye Unit with marked deterioration in visual acuity (VA) in his right eye. VAs were 0.67 logMAR OD and 0.14 logMAR OS. There was a family history of ADRP (Figure 1). RP was diagnosed in the proband by retinal findings (Figure 2) and by electrophysiology performed 7 years before presentation (ERG, VEP). Mixed cone/rod ERGs as well as independent testing of the cone and rod-mediated responses were of borderline amplitude and binocular occipital pattern VEPs were present to the smallest checks. No funding for genetic testing for RP was available for any of the patient's affected relatives. In the right eye fundoscopy demonstrated mild vitreous haze, ‘bone spicule like' pigment accumulation in the periphery bilaterally, Coats'-like E-RD, CME, teleangectatic vessels, and preretinal haemorrhages in the infero-temporal quadrant.
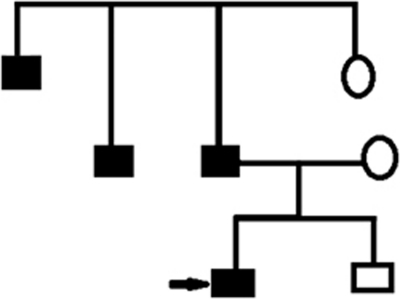
Figure 1.
Patient's pedigree demonstrating autosomal dominant inheritance of RP in the family.
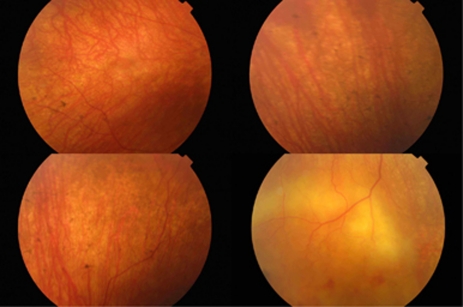
Figure 2.
Colour fundus photograph of the right eye demonstrating exudative retinal detachment in the infero-temporal quadrant. Bone spicule like pigmentation, retinal exudates, teleangectatic vessels, and superficial haemorrhages are also present.
CME had been treated previously with Acetazolamide 250 mg bid for 3 months. There was no significant improvement. Similarly, neither Dorzolamide hydrochloride drops tid for another 3 months or subsequently an orbital floor injection of Depo-Medrone (40 mg) were effective.
On 3D-OCT retinal oedema and increased retinal thickness were present in the right macula (Figure 3a). OS OCT findings were unremarkable. Cryotherapy was applied to the infero-temporal quadrant. At 6 months after treatment, VA OD increased slightly to 0.62 logMAR, while 3D-OCT showed very mild residual CME (Figure 3b).
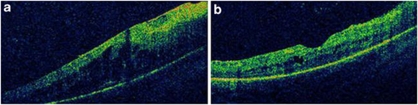
Figure 3.
(a) Right eye: 3D-OCT before cryotherapy demonstrates significant cystoid macular oedema and signs of an epiretinal membrane (ERM) (b) Right eye: 3D OCT after cryotherapy demonstrating mild residual cystoid macular oedema and ERM.
Comments
This is an unusual ADRP-Coats'-like case of unilateral retinal involvement. Coats reactions are infrequently seen in ADRP patients.
Lee et al4 tried vitrectomy, drainage of subretinal fluid, cryotherapy, endolaser, and silicone oil tamponade in a similar case in the past. The detachment was successfully treated, but VA did not improve. Laser photocoagulation as used by Kan et al5 resulted in a slight reduction of the exudation.
We treated our patient on the basis that CME developed because of inflammation generated from this area of Coats'-like exudation. Our hypothesis appeared correct, as cryotherapy alone led to complete resolution of the detachment with a resulting increase in VA and minimal residual CME. We suggest cryotherapy to be considered as an effective treatment option in the management of E-RD and CME in patients with Coats'-like RP.
The authors declare no conflict of interest.
References
- Zamorani G. Una rara associazone di retinite di coats con retinite pigmentosa. Gior Ital Oftalmol. 1956;9:429–443. [Google Scholar]
- Khan JA, Ide CH, Strickland MP. Coat's-type retinitis pigmentosa. Surv Ophthalmol. 1988;32 (5:317–332. doi: 10.1016/0039-6257(88)90094-x. [DOI] [PubMed] [Google Scholar]
- den Hollander AI, Heckenlively JR, van den Born LI, de Kok YJ, van der Velde-Visser SD, Kellner U, et al. Leber congenital amaurosis and retinitis pigmentosa with coats-like exudative vasculopathy are associated with mutations in the Crumbs homologue 1 (CRB1) gene. Am J Hum Genet. 2001;69:198–203. doi: 10.1086/321263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SY, Yoon YH. Pars plana vitrectomy for exuduative retinal detachment in coats-type retinitis pigmentosa. Retina. 2004;24 (3:450–452. doi: 10.1097/00006982-200406000-00017. [DOI] [PubMed] [Google Scholar]
- Kan E, Yilmaz T, Aydemir O, Güler M, Kurt J. Coats-like retinitis pigmentosa: reports of three cases. Clin Ophthalmol. 2007;1 (2:193–198. [PMC free article] [PubMed] [Google Scholar]