Sir,
Fungal keratitis (FK) is a severe blinding eye disease and a major cause of ocular morbidity.1 The clinical features of FK are not specific and the diagnosis is frequently not suspected until an aggressive treatment for bacterial, viral, or amebic keratitis has failed.
Case report
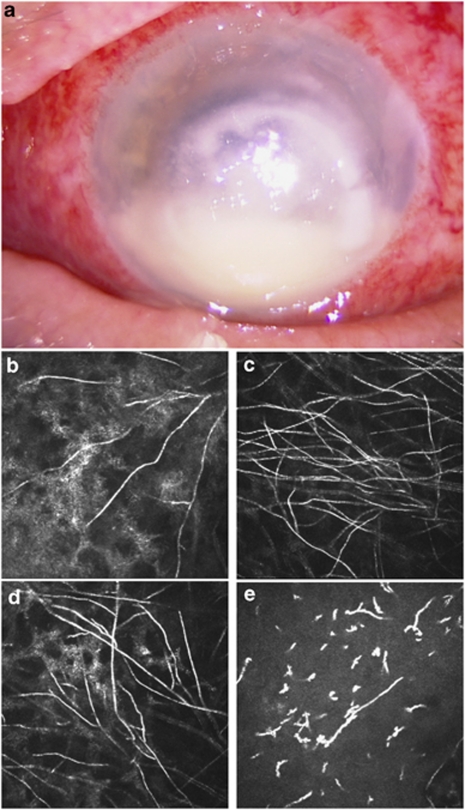
We report a case of a 65-year-old woman who developed a severe infectious keratitis in her left eye after a corneal injury caused by a tree branch and was initially treated by her family doctor with a local combination of tobramycin and dexamethasone. After 4 days she presented to an ophthalmology department for decreased vision and increased pain in her left eye. On initial evaluation, best-corrected visual acuity was hand movement in her left eye. Clinical examination revealed numerous purulent secretions, a conjunctival hyperaemia, and a large irregular whitish central corneal infiltrate (4.5 mm × 5 mm) with 1 mm hypopyon. The left eye fundus could not be visualized. Examination of her right eye was normal. Corneal scrapings were analysed by direct examination and culture. She was started on hourly topical fortified tobramycin, gentamicin and vancomycin, and oral levofloxacin. After 3 days, presence of Pseudomonas aeruginosa was identified, vancomycin and tobramycin were stopped, and topical fortified ceftazidime was added according to bacterial sensitivity. However, after 5 days of this treatment the corneal infiltrate increased in size and depth, and the hypopyon increased to 2 mm (Figure 1a). The patient was referred to our department for an in vivo confocal microscopy (IVCM) examination.
Figure 1.
(a) Photography of the left eye showing a large corneal central whitish irregular infiltrate with 2 mm hypopion. (b–d) In vivo confocal microscopy images (400 × 400 μm2) showing numerous hyper-reflective interlocking and branching linear structures, 5–7 μm width and 200–400 μm length, possibly corresponding to fungal hyphae. These images were obtained in the stroma at the boundaries of the central corneal infiltrate: (b) in the nasal area, depth: 115 μm; (c) in the superior area, depth: 223 μm; (d) in the superior area, depth: 106 μm. (e) In vivo confocal microscopy image (400 × 400 μm2) of the corneal stroma (45 μm depth) showing a stromal oedema with infiltration of inflammatory cells. The stroma appeared as a dark background with hyper-reflective small structures with an occasional dendritic-like pattern corresponding to inflammatory cells.
Interestingly, IVCM images (Heidelberg Retina Tomograph 3—Rostock Cornea Module, Heidelberg Engineering, Heidelberg, Germany) of the left eye showed hyper-reflective, thin, and branching interlocking linear structures in the stroma, 5–7 μm in width and 200–400μm in length, possibly corresponding to filamentous fungi (Figure 1b and c and Supplementary video online). These hyper-reflective structures were detected on the boundaries of the central corneal infiltrate at depths varying from 100 to 300 μm and were surrounded by oedema and infiltration of inflammatory cells (Figure 1d).
Topical amphotericin B and topical and systemic voriconazole were added to the previous treatment. A penetrating keratoplasty was performed because of a perforation that occurred 5 days later, and the direct examination and culture of the cornea confirmed the presence of a Fusarium sp within the stroma.
Comments
This case of bacterial and FK demonstrates the usefulness of IVCM for the diagnosis of filamentous fungal keratitis. Initial corneal scrapings were negative for fungi probably because of the localization of the hyphae deeper in the stroma. In such cases, IVCM can visualize filamentous fungi within the whole cornea of patients and may be helpful in managing this disease by providing a rapid diagnosis so that treatment may be initiated earlier.2
Fungal hyphae were observed with IVCM at the boundaries of the corneal infiltrate, where a better visualization of corneal structures and probably fungal hyphae is obtained. To carry out this dynamic examination and to enhance the effectiveness of IVCM, it must be performed but also interpreted by an experience operator.2 Despite these limitations, IVCM remains a valuable diagnostic modality for FK as recently confirmed by Vaddavalli et al.,3 who demonstrated in a controlled study a sensitivity of 89.2% and a specificity of 92.7% of IVCM for the diagnosis of FK as compared to standard microbiology.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on Eye website (http://www.nature.com/eye)
Supplementary Material
References
- Thomas PA, Geraldine P. Infectious keratitis. Curr Opin Infect Dis. 2007;20:129–141. doi: 10.1097/QCO.0b013e328017f878. [DOI] [PubMed] [Google Scholar]
- Labbé A, Khammari C, Dupas B, Gabison E, Brasnu E, Labetoulle M, et al. Contribution of in vivo confocal microscopy for the diagnosis and the management of infectious keratitis. Ocul Surf. 2009;7:41–52. doi: 10.1016/s1542-0124(12)70291-4. [DOI] [PubMed] [Google Scholar]
- Vaddavalli PK, Garg P, Sharma S, Sangwan VS, Rao GN, Thomas R. Role of confocal microscopy in the diagnosis of fungal and acanthamoeba keratitis. Ophthalmology. 2011;118 (1:29–35. doi: 10.1016/j.ophtha.2010.05.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.