Abstract
OBJECTIVE
Chronic exercise and obesity both increase intramyocellular triglycerides (IMTGs) despite having opposing effects on insulin sensitivity. We hypothesized that chronically exercise-trained muscle would be characterized by lower skeletal muscle diacylglycerols (DAGs) and ceramides despite higher IMTGs and would account for its higher insulin sensitivity. We also hypothesized that the expression of key skeletal muscle proteins involved in lipid droplet hydrolysis, DAG formation, and fatty-acid partitioning and oxidation would be associated with the lipotoxic phenotype.
RESEARCH DESIGN AND METHODS
A total of 14 normal-weight, endurance-trained athletes (NWA group) and 7 normal-weight sedentary (NWS group) and 21 obese sedentary (OBS group) volunteers were studied. Insulin sensitivity was assessed by glucose clamps. IMTGs, DAGs, ceramides, and protein expression were measured in muscle biopsies.
RESULTS
DAG content in the NWA group was approximately twofold higher than in the OBS group and ~50% higher than in the NWS group, corresponding to higher insulin sensitivity. While certain DAG moieties clearly were associated with better insulin sensitivity, other species were not. Ceramide content was higher in insulin-resistant obese muscle. The expression of OXPAT/perilipin-5, adipose triglyceride lipase, and stearoyl-CoA desaturase protein was higher in the NWA group, corresponding to a higher mitochondrial content, proportion of type 1 myocytes, IMTGs, DAGs, and insulin sensitivity.
CONCLUSIONS
Total myocellular DAGs were markedly higher in highly trained athletes, corresponding with higher insulin sensitivity, and suggest a more complex role for DAGs in insulin action. Our data also provide additional evidence in humans linking ceramides to insulin resistance. Finally, this study provides novel evidence supporting a role for specific skeletal muscle proteins involved in intramyocellular lipids, mitochondrial oxidative capacity, and insulin resistance.
Skeletal muscle insulin resistance (IR) is associated with obesity and physical inactivity and is crucial for the development of type 2 diabetes (1). Unfortunately, the causes of IR within muscle are not known. Concerted efforts have been made over the past several years to understand the potential role of intramyocellular lipid (IMCL) accumulation in the development of IR (2). Studies in both animal models (3) and humans (4) provided early evidence that IMCLs, such as triglycerides, were associated with skeletal muscle IR. However, we subsequently reported on the athletes paradox in which chronically exercised humans were markedly insulin-sensitive despite having high intramyocellular triglycerides (IMTGs) (5), a phenomenon corroborated by others (6). These observations gave pause to the widely held view that IMCLs cause IR within the muscle and lent support to the concept that other potentially damaging IMCLs may play a role in the development of IR.
Diacylglycerols (DAGs) and ceramides are lipid intermediates widely believed to be the true lipotoxic culprits underlying the reported associations between muscle triglycerides and IR, thereby explaining the athletes paradox and the root cause of muscle IR. Indeed, several lines of evidence from cell systems and animal models indicate that elevated DAGs (7) or ceramides (8) are associated with impaired insulin signaling and IR. Previous studies examining skeletal muscle DAG and ceramide content related to human IR, however, are limited and inconsistent (9,10). Because it has become clear that chronic exercise training increases IMTGs (5,11), recent studies have been conducted to examine whether both DAGs and ceramides are reduced with exercise (12–14). Another prevalent notion is that higher mitochondria content and capacity for fatty acid oxidation caused by exercise training are responsible for lower DAG and ceramide content (15). We recently have shown that exercise training does indeed decrease these IMCLs in conjunction with increased oxidative capacity and improved insulin sensitivity (12). The distinct roles that chronic exercise and obesity may play in the link between these potentially harmful lipid species and skeletal muscle IR, however, remain to be elucidated. Moreover, it is not known whether specific molecular species of these complex lipids are associated with skeletal muscle IR according to their fatty acid chain length or degree of saturation. Therefore, we used mass spectrometry to quantify the content and molecular species profile of both DAGs and sphingolipids within skeletal muscle biopsies in human subjects widely disparate for physical activity and obesity to test the following primary hypothesis: endurance-trained athletes, despite having higher IMTGs, would have the lowest muscular DAG and ceramide content, the highest insulin sensitivity, and the highest mitochondrial content compared with both normal weight and obese sedentary subjects and that these differences would be more pronounced for saturated DAG and ceramide species. In addition, we investigated several proteins associated with lipid droplet esterification and lipolysis: oxidative perilipin adipophilin TIP47 (OXPAT)/perilipin-5 or lipid storage protein 5 because of its reported role in lipid droplet formation and enhanced fatty acid oxidation (16,17); the lipogenic enzymes stearoyl-CoA desaturase 1 (SCD1) and diacylglycerol acyltransferase 1 (DGAT1); and adipose triglyceride lipase (ATGL). These data provide novel insight into the role of lipid-induced IR within human skeletal muscle.
RESEARCH DESIGN AND METHODS
A total of 42 older (aged 66.2 ± 0.7 years [range 60–]75) volunteers were recruited and classified as obese (BMI >30 kg/m2) and sedentary (OBS group; n = 21), normal weight (BMI 18–25 kg/m2) and sedentary (NWS group; n = 7), and normal weight and endurance trained (NWA group; n = 14). Sedentary was defined as ≤1 day per week of a structured exercise session of <20 min. Endurance trained was defined as five or more structured aerobic exercise sessions per week.
Subjects were in good general health, nonsmokers, and weight stable (±3 kg) for at least 6 months. Fasting lipid profile, electrolytes, plasma glucose, complete blood count, platelet count, HbA1c, kidney function, thyroid-stimulating hormone, and liver function were determined. A standard 75-g oral glucose tolerance test (OGTT) was performed. Potential subjects were excluded if they had fasting glycemia ≥126 or ≥200 mg/dL after a 2-h OGTT, hematocrit level <34%, or a thyroid-stimulating hormone level >8 μIU/mL or if they were taking chronic medication known to affect glucose homeostasis. The University of Pittsburgh Institutional Review Board approved the protocol. All volunteers gave written consent.
Body composition.
Total body fat mass and lean body mass (LBM) were measured by dual-emission X-ray absorptiometry (Lunar Prodigy; GE Healthcare, Milwaukee, MI). Visceral (VAT), subcutaneous (SAT), and total (TAT) abdominal adipose tissue were measured from a single slice (L3–L4 level) by magnetic resonance imaging (Siemens 3T Trio; Medicals Systems, Erlangen, Germany) or computed tomography (9800 CT scanner; GE Healthcare) (2,18). To account for possible differences in the two imaging methods, the following ratios were computed: VAT-to-TAT, SAT-to-TAT, and VAT-to-SAT.
Physical fitness.
Vo2 peak was measured with a graded exercise protocol on an electronically braked cycle ergometer (Ergoline 800S; Sensormedics, Yorba Linda, CA) with indirect calorimetry (Moxus, AEI Technologies, Pittsburgh, PA), as described previously (11).
Insulin sensitivity.
Insulin sensitivity was measured as the rate of insulin-stimulated glucose disposal (Rd) during a 4-h hyperinsulinemic-euglycemic clamp (40 mU/m2/min) coupled with stable isotope tracer dilution, as described previously (5). Subjects were instructed not to perform physical exercise 48 h before the clamp to avoid the acute effects of exercise on insulin sensitivity. Indirect calorimetry (Parvomedics TrueOne, Sandy, UT) was used during the clamp to calculate oxidative and nonoxidative glucose disposal.
Muscle biopsy.
Percutaneous muscle biopsies were performed before the clamp, following the same standardized conditions as described above. Biopsies were obtained from the vastus lateralis as described previously (19). After trimming of visible adipose tissue with a dissecting microscope (Leica EZ4; Leica Microsystems, Wetzlar, Germany), two portions of the specimen (~30 mg each) were flash-frozen in liquid nitrogen and stored at −80°C for Western blotting and for ceramide and DAG analysis. A third portion was used for histochemical analysis. A fourth portion (~5 mg) was used for transmission electron microscopy. All analyses were then performed in a blind manner.
Histochemistry.
Histochemical analysis was performed on serial sections using methods previously described (11,12). IMTG content was determined by the Oil Red O (ORO). To quantify fiber-specific IMTGs, the sections were costained with ORO and human myosin heavy-chain MYH7 (type I) and MYH2 (type IIa) (all antibodies from Santa Cruz Biotechnology, Santa Cruz, CA). Succinate dehydrogenase (SDH) staining was used as a marker for oxidative capacity. Images were visualized using a Leica microscope (DM4000B; Leica Microsystems) and digitally captured (Retiga 2000R; Q Imaging, Surrey, BC, Canada), and semiquantitative image analysis was performed (Northern Eclipse; Empix Imaging, Cheektowaga, NY). All units for the histology are in average gray and reported as arbitrary units (AUs). The proportion of type I, type IIa, and type IIx was computed from ~150 to 300 fibers per subject. The interassay variability for the fiber type–specific ORO measure assessed on three subjects was <6%.
Analysis of DAGs, ceramides, and sphingolipids.
Quantification of intramuscular DAGs, ceramides, and sphingolipids was performed using high-performance liquid chromatography–tandem mass spectrometry, as described previously (20). Tissue homogenates were fortified with internal standards and extracted into a one-phase neutral organic solvent system (ethyl acetate/isopropyl alcohol/water; 60:30:10 vol/vol/vol), evaporated and reconstituted in methanol, and analyzed by a surveyor/TSQ 7000 LC/MS System (Thermo Electron Finnigan; Thermo Fisher Scientific, Waltham, MA) (21). Quantitative analysis was performed in a positive multiple-reaction–monitoring mode, based on calibration curves generated by adding to an artificial matrix known amounts of target analytes, synthetic standards, and an equal amount of internal standard. The DAG and ceramide levels were normalized to total protein levels.
Protein expression.
Frozen tissue was homogenized in ice-cold cell lysis buffer (Cell Signaling Technology, Danvers, MA) with protease inhibitor cocktail tablets (Roche Diagnostics, Mannheim, Germany). Protein content was determined in triplicate with a bicinchoninic acid assay (ThermoScientific, Rockford, IL). The homogenates were mixed with 5× Laemmli buffer and heated for 5 min at 95°C. The samples were loaded in equal amounts of protein and resolved in a 12% SDS-PAGE followed by transfer onto polyvinylidene difluoride membranes (Bio-Rad Laboratories, Hercules, CA). After blocking, membranes were probed overnight at 4°C with the anti-myocardial lipid droplet protein (MLDP) (OXPAT/perilipin-5) antibody (American Research Products, Belmont, MA), anti-SCD1 (Alpha Diagnostic International, San Antonio, TX), anti-DGAT1 (Novus Biologicals, Littleton, CO), and anti-ATGL (Cell Signaling, Boston, MA). Blots were normalized to either anti–β-actin (Santa Cruz Biotechnology, Santa Cruz, CA). A prestained molecular-mass marker (10–170 kDa) was used to determine protein size (Fermentas International, Burlington, Ontario, Canada). Immunoreactive proteins were detected by chemiluminescence (Bio-Rad Laboratories) using appropriate horseradish peroxidase–conjugated secondary antibodies. Specific bands were quantified by densitometry using the software ImageJ (National Institutes of Health, Bethesda, MD). To reduce bias, all samples were loaded on the same day, and all gels and membranes were processed at the exact same time with the same solutions.
Transmission electron microscopy.
Transmission electron microscopy analysis was conducted in batches, as described previously (22). Approximately 18–20 micrographs were obtained from randomly sampled transverse sections of muscle fibers and were acquired (JEM-1210; Jeol, Tokyo, Japan) at ×36,000 magnification using stereological analysis with digital-imaging software (Metamorph 6.3; Molecular Devices, Sunnyvale, CA) .
Statistical analysis.
Data are presented as means ± SEM. After checking normality with the Shapiro-Wilk test and equality of variance with the Levene test, one-way ANOVAs were performed to examine group differences. Post hoc tests were performed with the Tukey-Kramer honestly significant adjustment. If assumptions were not met, comparisons between groups were performed with the Welch adaptation to the ANOVA test. Pairwise correlations were performed with the Spearman ρ correlation.
To identify patterns of distribution and reduce the dimensionality of the data, while retaining as much of the variance as possible, a principal component analysis (PCA) of the individual moieties of DAGs (13 subspecies) and ceramides (8 subspecies) was performed. PCA was used as exploratory data analysis to convert a set of possibly correlated variables into a set of data of uncorrelated variables called principal components or factors, thus revealing the internal structure of the data in a way that best explains the variance of the data. After inspecting the correlation matrix, factors were identified on the basis of the strength of the loading; thus the first factor had as high a variance as possible, and each succeeding factor had the highest variance possible under the constraint that it be uncorrelated with the preceding factor. For each factor, Cronbach α was computed to assess the degree of homogeneity among the indicators. To assess the physiological relevance of PCA findings, we combined the indictors loading on each PCA factor by summing the different species scores within each factor and then performed one-way ANOVAs of these combined scores to compare groups. The α level was set a priori to 0.05. Statistical analyses were performed using JMP 5.0.1.2 and SPSS version 16.0 for the Macintosh.
RESULTS
Subject characteristics, body composition, and physical fitness.
Subject characteristics are presented in Table 1. OBS subjects had higher BMI and more body fat than both the NWA and the NWS subjects. Vo2 peak was >50% higher in NWA subjects compared with both NWS and OBS subjects.
TABLE 1.
Subjects’ characteristics, body composition, and physical fitness
| Athletes | Normal-weight subjects | Obese subjects | |
|---|---|---|---|
| n | 14 | 7 | 21 |
| Sex (male/female) | 10/4 | 3/4 | 11/10 |
| Age (years) | 65.1 ± 1.3 | 66.5 ± 1.8 | 66.8 ± 1.0 |
| Weight (kg) | 68.1 ± 2.4B | 70.4 ± 3.4B | 93.8 ± 2.0A |
| BMI (kg/m2) | 23.7 ± 0.6B | 24.5 ± 0.9B | 32.9 ± 0.5A |
| Waist circumference (cm) | 79.5 ± 2.3B | 85.5 ± 3.9B | 109.7 ± 2.2A |
| LBM (kg) | 51.5 ± 2.5 | 43.4 ± 3.5 | 51.1 ± 2.0 |
| Fat mass (kg) | 13.9 ± 1.9A | 23.7 ± 2.6B | 38.8 ± 1.5C |
| Body fat (%) | 20.3 ± 2.4B | 34.6 ± 3.3A | 41.9 ± 1.9A |
| TAT (cm2) | 223.6 ± 32.4B | 359.5 ± 52.3B | 592.3 ± 26.8A |
| VAT (cm2) | 68.3 ± 15.0B | 105.3 ± 24.2B | 204.8 ± 12.4A |
| SAT (cm2) | 155.3 ± 26.9B | 254.2 ± 43.4B | 374.8 ± 22.3A |
| Vo2 peak (L/min) | 2.81 ± 0.17A | 1.84 ± 2.36B | 1.71 ± 1.36B |
| Vo2 peak/LBM (mL/min/kg) | 53.8 ± 2.0A | 41.5 ± 2.8B | 33.3 ± 1.6C |
Data are means ± SEM.
A,B,CSignificant differences between groups (one-way ANOVA).
Insulin sensitivity and metabolic variables.
Peripheral insulin sensitivity was higher in NWA subjects compared with NWS subjects, who in turn were more insulin-sensitive than the OBS subjects (Table 2). These differences were explained by differences in nonoxidative glucose disposal (P < 0.01) but not in oxidative glucose disposal (P = 0.25). These differences remained after adjusting for the higher VAT in the obese subjects. Hepatic insulin sensitivity was lower in OBS compared with NWA and NWS subjects.
TABLE 2.
Metabolic variables
| Athletes | Normal-weight subjects | Obese subjects | |
|---|---|---|---|
| n | 14 | 7 | 21 |
| Rd (mg/min/kg LBM) | 12.31 ± 0.55A | 9.74 ± 0.77B | 6.29 ± 0.45C |
| HGP (%) | 99.99 ± 3.49A | 99.61 ± 4.75A | 85.87 ± 2.74B |
| Fasting blood glucose (mmol/L) | 4.84 ± 0.17B | 4.56 ± 0.25B | 5.31 ± 0.12A |
| HbA1c (%) | 5.40 ± 0.12B | 5.61 ± 0.18AB | 5.84 ± 0.10A |
| Fasting insulin (pmol/L) | 17.91 ± 4.70B | 18.68 ± 6.42B | 45.08 ± 3.70A |
| Glucose 2-h OGTT (mmol/L) | 6.35 ± 0.44B | 6.75 ± 0.64B | 8.26 ± 0.37A |
| Total cholesterol (mmol/L) | 4.82 ± 0.18 | 4.67 ± 0.26 | 4.96 ± 0.15 |
| HDL (mmol/L) | 1.67 ± 0.09A | 1.43 ± 0.12AB | 1.33 ± 0.07B |
| LDL (mmol/L) | 2.83 ± 0.15 | 2.86 ± 0.21 | 3.04 ± 0.12 |
| VLDL (mmol/L) | 0.33 ± 0.04B | 0.37 ± 0.06B | 0.59 ± 0.04A |
| Triglycerides (mmol/L) | 0.88 ± 0.12B | 1.03 ± 0.17B | 1.62 ± 0.10A |
Data are means ± SEM. HGP, hepatic insulin sensitivity expressed as the suppression of hepatic glucose production. Rd, whole-body insulin sensitivity expressed as the rate of insulin-simulated glucose disposal.
A,B,CSignificant differences between groups (one-way ANOVA).
OBS subjects had higher fasting and 2-h blood glucose levels, along with higher fasting insulin levels, reflecting their overall worse metabolic profile (Table 2). Total and LDL cholesterols were similar across groups, although it is important to note that the proportion of subjects who were taking lipid-lowering medication was significantly different across the three groups as follows: 0% in the NWA group, 29% in the NWS group, and 38% in the OBS group. HDL cholesterol and plasma triglycerides, however, were both more favorable in NWA and NWS subjects.
IMTG and lipid droplet volume density.
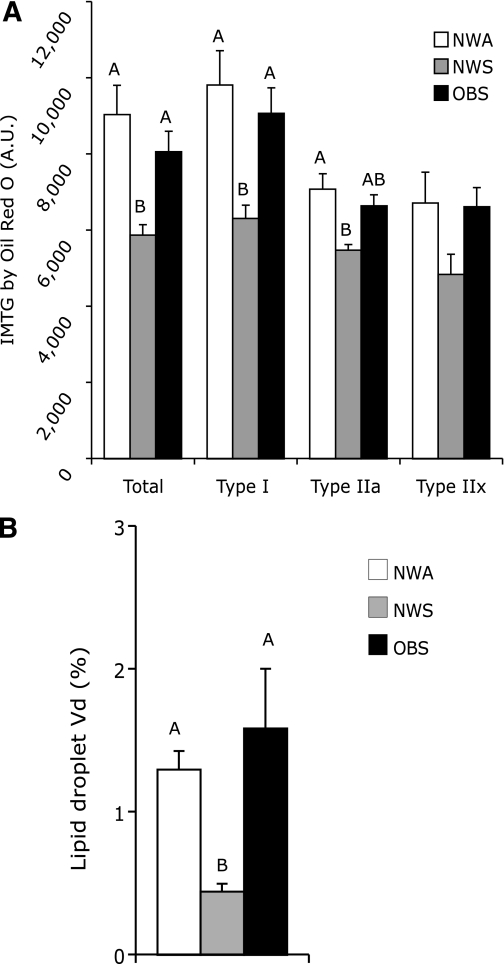
Total-muscle IMTG content, measured by ORO staining and electron microscopy, was higher in NWA and OBS subjects compared with NWS subjects (P = 0.024) (Fig. 1). These differences were consistent for type I and type IIa myofibers. Neither IMTG measured by the ORO staining nor lipid droplet density was correlated with insulin sensitivity (r = −0.008 and r = −0.25, respectively, both P > 0.05).
FIG. 1.
IMCLs and lipid droplet protein content in vastus lateralis. IMTG measured by the ORO stain (A) and lipid droplet volume density measured by electron microscopy (B). Bars are mean values and error bars are SEMs. The letters A and B above the bars denote significant differences between groups (P < 0.05, one-way ANOVA).
Skeletal muscle DAGs.
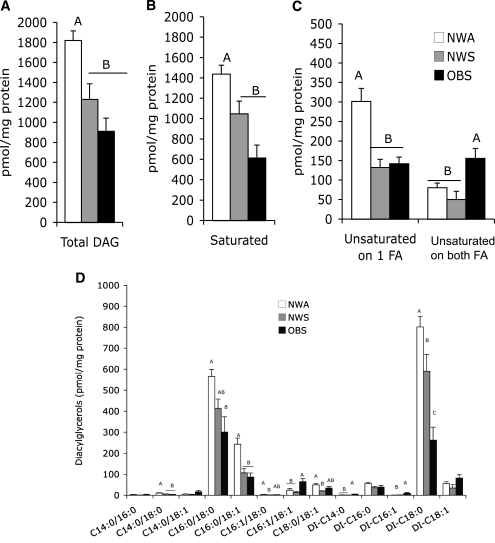
Total DAG content was ~50% higher (P < 0.01) in the skeletal muscle of NWA compared with NWS subjects and approximately twofold higher in NWA compared with OBS subjects (Fig. 2). Similar differences were observed for saturated DAGs (P < 0.01) and for DAG species in which one of the fatty acids was unsaturated (P < 0.01). In contrast, OBS subjects had elevated DAG species that contained an unsaturated fatty acid on both positions compared with both NWS and NWA subjects (P < 0.01). These disparate results also are evident across the individual DAG species shown in Fig. 2.
FIG. 2.
DAGs in vastus lateralis. Total DAG content (A), saturated species (B), unsaturated species (C), and individual species (D). Bars are mean values, and error bars are SEMs. The letters A, B, and C above the bars denote significant differences between groups (P < 0.05, one-way ANOVA).
PCA identified three factors that combined to explain 89.1% of the total variance in DAGs (Table 3). When the species belonging to factor 1 were summed and compared across groups, NWA subjects had a higher (P < 0.01) content (1,774 ± 118 pmol/mg protein) than both NWS (1,203 ± 167) and OBS (807.9 ± 112.4) subjects. When the species of factor 2 were summed, OBS subjects had a higher (P = 0.046) content (17.8 ± 2.3) than NWS (7.6 ± 3.4) subjects; NWA subjects were not different (12.2 ± 2.4) from the OBS subjects or from NWS subjects. The sum of the components of factor 3 was higher in OBS subjects than in the NWS and NWA subjects (82.1 ± 15.6, 19.1 ± 23.6, and 32.1 ± 16.7, respectively, P = 0.036). Total DAGs was positively correlated with insulin sensitivity (r = 0.57, P < 0.05). This positive association was similar for the sum of the species of factor 1 (r = 0.57, P < 0.05). Factors 2 and 3, however, were not correlated with insulin sensitivity (r = −0.21 and r = −0.17, respectively, P > 0.05).
TABLE 3.
Exploratory PCAs
| Exploratory PCA on DAG species |
|---|
| Factor 1, eigenvalue 5.7 (43.6%) |
| Di-C16:0, C18:0/18:1, C16:0/18.1, C16:1/18:0, C16:0/18:0, Di-C18:0, and Di-C18:1 |
| Factor 2, eigenvalue 3.7 (28.4%) |
| Di-C16:1, Di-C14:0, and C14:0/18:0 |
| Factor 3, eigenvalue 2.2 (17.1%) |
| C14:0/18:1, C14:0/16:0, and C16:1/18:1 |
| Exploratory PCA on ceramides species |
|---|
| Factor 1, eigenvalue 3.3 (41.3%) |
| Lingoceric (C24:0), nervonic (C24:1), stearic (C18:0), and arachidic (C20:0) |
| Factor 2, eigenvalue 1.3 (16.6%) |
| Dihydroceramide 16 and palmitoleic (C18:1) |
| Factor 3, eigenvalue 1.2 (15.1%) |
| Palmitic (C16:0) |
| Factor 4, eigenvalue 1.1 (14.3%) |
| Myristic (C14:0) |
% refers to the percentage of variance of the data explained by each factor.
Skeletal muscle ceramides and other sphingolipids.
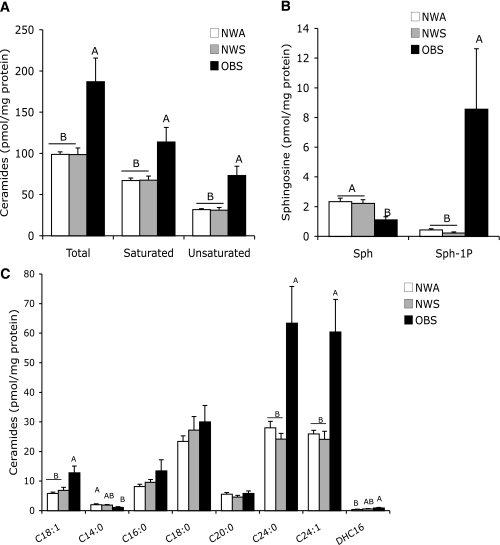
Total ceramide content was higher (P < 0.01) in the skeletal muscle of OBS subjects compared with both NWS and NWA subjects (Fig. 3). These differences were consistent across both saturated (P = 0.03) and unsaturated (P < 0.01) ceramide species, as well as fatty acid chain length. Sphingosine-1-phosphate (S1P) also was higher in obesity (Fig. 3). In contrast, sphingosine was significantly lower in OBS compared with both NWA and NWS subjects.
FIG. 3.
Ceramides and other sphingolipids in vastus lateralis. Total, saturated, and unsaturated ceramide content (A), sphingosine and S1P (B), and individual species of ceramides (C). Bars are mean rates, and error bars are SEMs. The letters A and B above the bars denote significant differences between groups (P < 0.05, one-way ANOVA).
PCA identified four significant factors, explaining 87.2% of the total variance in ceramides (Table 3). When the molecular species belonging to factor 1 were summed and compared across groups, OBS subjects were found to have a higher (P = 0.02) content (159.6 ± 18.4 pmol/mg protein) than NWS (80.2 ± 27.1) and NWA (82.8 ± 21.0) subjects. The same pattern was found for factor 2, with a higher content in OBS (13.7 ± 1.7) than NWS (7.1 ± 2.4) and NWA (6.2 ± 1.9, P = 0.03) subjects. The component of factor 3 revealed no differences (P = 0.28) across the groups, whereas component factor 4 was significantly (P = 0.04) higher in NWA (1.99 ± 0.27) and NWS (1.87 ± 0.35) compared with OBS (1.10 ± 0.24) subjects. Total ceramide content was negatively correlated with insulin sensitivity (r = −0.48, P < 0.05). Similar associations were observed for saturated ceramide and unsaturated ceramide (r = 0.44 and r = 0.50, respectively, P < 0.05). When the sum of the species belonging to the PCA factors were correlated to insulin sensitivity, factors 1 and 2 were significantly negatively correlated with insulin sensitivity (r = −0.46 and r = −0.47, respectively, P < 0.05), whereas factor 4 was positively correlated (r = 0.38, P < 0.05) and factor 3 was not significantly correlated (r = −0.08, P > 0.05) with insulin sensitivity.
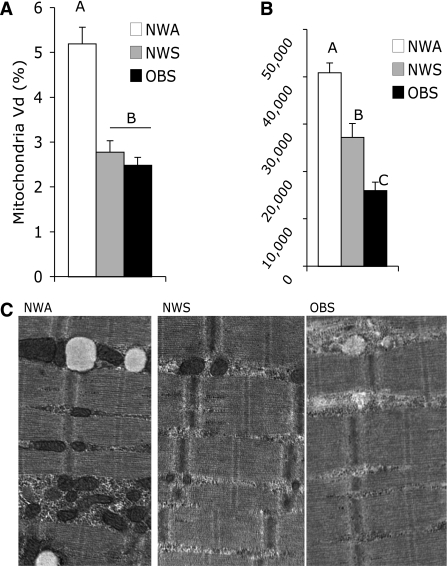
Mitochondria, oxidative capacity, and proportion of skeletal muscle fiber types.
Mitochondria volume density was significantly higher in NWA than in the two sedentary groups (P < 0.001) (Fig. 4A). SDH content was higher in NWA than NWS subjects, who in turn had higher SDH than OBS subjects (P < 0.001) (Fig. 4B). Mitochondria volume density and SDH content were positively correlated with insulin sensitivity (r = 0.51 and r = 0.67, respectively, all P < 0.05).
FIG. 4.
Mitochondria and markers of oxidative capacity in vastus lateralis. Mitochondria volume density (A), example of micrographs (B), and SDH content (C). Bars are mean values, and error bars are SEMs. The letters A, B, and C above the bars denote significant differences between groups (P < 0.05, one-way ANOVA).
NWA subjects had a higher (P < 0.01) proportion of type 1 myofibers (70.2 ± 4.2%) compared with NWS (34.4 ± 4.0%) and OBS (43.7 ± 2.1%) subjects and a correspondingly lower proportion of type 2 fibers. The proportion of type I fibers was positively correlated with insulin sensitivity (r = 0.56, P > 0.05), whereas the proportion of type IIa and IIx fibers was negatively correlated with insulin sensitivity (r = −0.39 and r = −0.59, respectively, P < 0.05).
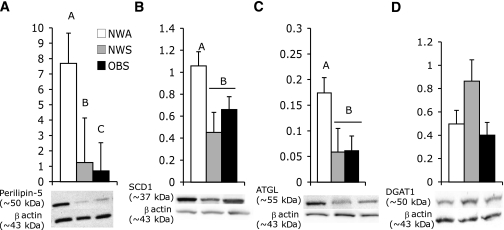
Lipid droplet protein content.
NWA subjects had significantly more OXPAT/perilipin-5, SCD1, and ATGL than the two sedentary groups (all P < 0.05) (Fig. 5). No differences between groups were observed for DGAT1. There was notably more variability in OXPAT/perilipin-5 expression, as indicated by the larger error bars, although this greater variation is not adequately depicted in the representative bands for this protein. This was likely a result of the greater biological variability. OXPAT/perilipin-5 content was positively correlated with insulin sensitivity (r = 0.52, P < 0.01) and lipid droplet volume density (r = 0.45, P < 0.05). SCD1 was positively correlated with insulin sensitivity (r = 0.58, P < 0.01) and with lipid droplet volume density (r = 0.33, P < 0.01). ATGL was positively correlated with insulin sensitivity (r = −0.48, P < 0.01) but not with lipid droplet density (r = 0.28, P = 0.25). DGAT1 was not significantly correlated with BMI, insulin sensitivity, or lipid droplet density.
FIG. 5.
Lipid droplet protein content in vastus lateralis. Perilipin-5 (A), SCD1 (B), ATGL (C), and DGAT1 (D) protein contents measured by Western blotting. Bars are mean values, and error bars are SEMs. The letters A, B, and C above the bars denote significant differences between groups (P < 0.05, one-way ANOVA). The bands depicted in the Western blots are from one subject of each group.
DISCUSSION
A primary finding of our study was that DAG content was approximately twofold higher within the highly insulin-sensitive skeletal muscle compared with obese skeletal muscle. This clearly does not support a common contemporary view, largely based on evidence from animal models, that muscular DAGs explain IR of obesity, aging, and type 2 diabetes (23). To the contrary, our data suggest that higher DAG content in chronically exercised, insulin-sensitive muscle represents another athletes paradox (i.e., total cellular DAG content is associated with better insulin sensitivity). These data are particularly significant given that few studies have examined skeletal muscle DAG content in association with IR, and still fewer studies have been performed in human muscle (10,11,13,24). Our data also are in accord with recent findings that DAGs are not elevated in insulin-resistant muscle after controlling for obesity and physical fitness (24) and higher levels of DAGs in lean subjects compared with obese volunteers (25), as well as with an animal study indicating that increased DAG content in muscle and IR are not necessarily related (26). Our results also differ somewhat from our previous report demonstrating that moderate exercise reduced muscle DAG content in previously sedentary obese subjects (12,27). It is possible that these discrepancies are a result of the amount and/or intensity of chronic exercise and the model system used (acute lipid oversupply) or a result of subcellular DAG location (i.e., membrane-bound or part of neutral lipid droplets). It also is possible that particular DAG species may differentially affect insulin action.
Ours is the first study to provide a comprehensive profile of the distinct molecular species of DAG within muscle of obese, normal-weight, and athletic human subjects, suggesting that particular DAG species may be associated with IR in muscle, whereas others clearly are not. This did not seem to be related to the fatty acid chain length of the DAG or the total degree of fatty acid saturation because we found that exercised muscle had higher levels of both saturated and unsaturated DAG species. It is difficult to reconcile our results with those in a recent study by Bergman et al. (28), who found that the degree of saturation of DAGs within muscle in athletes was lower compared with sedentary subjects and was related to higher insulin sensitivity. One possible explanation is that the younger athletes in their study had a different diet composition. In addition, they measured the total fatty acid content within the DAG pool, whereas we quantified specific DAG species. Our methods revealed that DAG species containing one unsaturated and one saturated fatty acid are lower in obese muscle but that DAG species containing unsaturated fatty acids on both positions was higher in obese muscle. The PCA supports this and suggests that it is not the overall concentration of DAGs that is deleterious but that particular DAG moieties may be lipotoxic even in relatively smaller amounts. Additional studies are needed to determine whether specific fatty acids stimulate DAG synthesis and whether this is linked to IR.
Another key finding of our study was that ceramide content was twofold higher in the obese muscle compared with normal-weight sedentary and exercise-trained muscles. These results are supported by previous studies in human subjects reporting higher total ceramide levels in obese muscle (8) and associations with IR and a lower oxidative capacity (24,29). This also is in accord with our previous report that moderate exercise training decreased intramuscular ceramide levels in previously sedentary obese subjects (12). Likewise, Bruce et al. (14) found that exercise training tended to reduce both the total ceramide content and the saturated ceramide species in obese insulin-resistant subjects without significant weight loss. In agreement with Helge et al. (30), we did not find significant differences between the athletes and normal-weight sedentary subjects with respect to total muscle content of ceramides, which could be simply attributed to the levels of ceramide required for normal physiological function. Our results also are consistent with animal models and cell systems linking ceramide content in muscle to impaired insulin signaling and IR (31–33). Higher ceramide levels in obesity and in association with IR were consistent for both saturated and unsaturated ceramides, which is consistent with our recent report (24). The PCA for ceramides suggests, however, that a specific group of ceramides may be related to better insulin sensitivity. Because ceramides have several functions in normal biology, including comprising mitochondria membranes (34), mechanistic investigations are needed to examine the specific role of these ceramide species on insulin action.
To our knowledge, this is the first observation of higher S1P in obese, insulin-resistant muscle. Among the bioactive sphingolipids, ceramide, sphingosine, and S1P have been proposed to exert differential effects on cells (35). Ceramide is converted to sphingosine by the action of ceramidases, and, subsequently, sphingosine is phosphorylated to generate S1P (29,36). Ceramides and sphingosine inhibit growth and are involved in apoptosis (37–39), in contrast to the effects of S1P, which are to promote cellular proliferation, survival, and inhibition of apoptosis (35). Furthermore, S1P is implicated in the clearance of ceramide (40), is a potential regulator of de novo ceramide synthesis (41,42), and has been shown to inhibit Jun NH2-terminal kinase activation (43). Samad et al. (44) reported a similar observation in ob/ob mice, which had higher plasma levels of total ceramide, sphingosine, and S1P compared with their lean counterparts. Additional inquiry is needed to determine whether these specific sphingolipids actually affect insulin action within muscle.
We also placed our novel lipid data within the context of specific proteins associated with lipid droplet esterification, lipolysis, and oxidation. First, the lipid droplet protein OXPAT/perilipin-5, reported to be highly expressed in highly oxidative tissues (16,45,46), was more than sevenfold more abundant in the skeletal muscle of the endurance-trained athletes, corresponding significantly with their higher lipid droplet volume and their higher insulin sensitivity. One previous study in humans demonstrated no correlation between OXPAT/perilipin-5 protein content in the skeletal muscle and insulin sensitivity in obese type 2 diabetic subjects and BMI-matched control subjects (17). Our data support a role for OXPAT/perilipin-5 in both higher lipid droplet content and fatty acid oxidation, and, although our observed associations with insulin sensitivity are intriguing, additional studies are needed to determine whether it directly mediates insulin action. Second, we investigated two key lipogenic enzymes, SCD1 and DGAT1. SCD1 is a rate-limiting enzyme that converts saturated fatty acids to monounsaturated fatty acids and, in animal and cell culture models, has been previously implicated in the development of dysregulated fatty acid metabolism, increased triglyceride storage, and obesity (47,48). In contrast, although confirming that it tracks with higher muscle triglycerides, our data in human muscle clearly demonstrate that SCD1 is higher in metabolically healthy, more insulin-sensitive muscle. This is in agreement with observations of increases in SCD1 content after acute (49) and chronic aerobic exercise training (27). The lack of differences in DGAT between the groups is in accord with our previous report (27). Third, we report elevated levels of ATGL in endurance-trained athletes compared with sedentary subjects. These data are supported by previous exercise-training studies (50,51). ATGL is important as the first step in hydrolyzing triglycerides to DAG on its way to further hydrolysis and ultimate energy generation, which could explain the higher DAG levels in the muscle of the athletes. Our interpretation of this finding is that these alterations in esterification and lipolysis within exercise-trained muscle lead to an elevated pool of neutral DAGs, similar to that of triglycerides that can be used as a fuel source during physical activity. Taken together, these data suggest an enzymatic profile of enhanced neutral lipid storage and oxidation associated with enhanced insulin sensitivity with exercise training.
These human studies cannot directly determine mechanisms or causes of IR. Although we did not determine whether IMCLs are associated with specific defects in insulin signaling, we clearly show that insulin-stimulated glucose disposal in skeletal muscle differed according to study groups. Additional studies are needed to examine whether the specific lipid species or their cellular location, in particular DAG within muscle, are mechanistically linked with impaired insulin signaling. It will also be important to determine whether the fatty acid composition of the diet affects insulin action within muscle because dietary patterns have been shown to influence lipid metabolite content and saturation (3). We did not measure other intracellular lipids that have been implicated in muscle IR, such as long-chain fatty acyl-CoA (52,53) because of the limited availability of tissue within the relatively small biopsy samples. Another important element to consider is that the amount and intensity of physical activity performed by these highly trained athletes do not allow us to extrapolate these findings in athletes to more moderate physical activity as emphasized for general health. Thus, the possibility remains that there is some threshold level or dose-response effect of physical activity on insulin sensitivity and these lipids.
In summary, high-level exercise training was unexpectedly associated with considerably higher total DAG content within skeletal muscle concomitant with higher insulin sensitivity, thus extending the athletes paradox to muscle DAGs and to triglycerides across fiber types. Therefore, the total cellular DAG content cannot explain skeletal muscle IR. This suggests instead a role for specific molecular species of DAGs and possibly their subcellular location in this metabolic abnormality. Ceramides and S1P, on the other hand, are consistently elevated in obese and insulin-resistant muscle. Moreover, formation and metabolism of these complex lipids were associated with key proteins expressed in human muscle, which in turn corresponded significantly with IR. These novel translational data form a basis for more mechanistic studies to be performed in model systems to determine exact causes of lipid-induced IR.
ACKNOWLEDGMENTS
This study was supported by National Institutes of Health (NIH) Grants (R01-AG20128 to B.H.G. and R01-DK068046 to P.E.B.), funding from the American College of Sports Medicine Foundation (to F.A.), University of Pittsburgh Student and Faculty Grants (to B.H.G. and F.A.), an NIH/National Center for Research Resources/Clinical and Translational Science Award (UL1 RR024153), and University of Pittsburgh Obesity and Nutrition Research Center Grant 1P30DK46204.
No potential conflicts of interest relevant to this article were reported.
F.A. researched data; contributed to the study concept, design, analysis, and interpretation of the data; and wrote the manuscript. J.J.D. researched data and reviewed and edited the manuscript. E.A.-C., M.M.E., P.C., and M.S.-R. researched data. P.M.C. reviewed and edited the manuscript. G.E.S. contributed to the statistical analyses and reviewed and edited the manuscript. P.E.B. contributed to the discussion and reviewed and edited the manuscript. F.G.S.T. researched data and contributed to the discussion. B.H.G. contributed to the study concept and design and the analysis and interpretation of the data and wrote the manuscript.
Parts of this article were presented in abstract form at the 27th Annual Scientific Meeting of The Obesity Society, Washington, District of Columbia, 24–28 October 2009.
We appreciate the cooperation of our research volunteers, along with the skills of Steve Anthony and the nursing staff of the Clinical and Translational Research Center of the University of Pittsburgh.
REFERENCES
- 1.Saltiel AR. Series introduction: the molecular and physiological basis of insulin resistance: emerging implications for metabolic and cardiovascular diseases. J Clin Invest 2000;106:163–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelley DE, Goodpaster BH. Skeletal muscle triglyceride: an aspect of regional adiposity and insulin resistance. Diabetes Care 2001;24:933–941 [DOI] [PubMed] [Google Scholar]
- 3.Lee JS, Pinnamaneni SK, Eo SJ, et al. Saturated, but not n-6 polyunsaturated, fatty acids induce insulin resistance: role of intramuscular accumulation of lipid metabolites. J Appl Physiol 2006;100:1467–1474 [DOI] [PubMed] [Google Scholar]
- 4.Pan DA, Lillioja S, Kriketos AD, et al. Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 1997;46:983–988 [DOI] [PubMed] [Google Scholar]
- 5.Goodpaster BH, He J, Watkins S, Kelley DE. Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. J Clin Endocrinol Metab 2001;86:5755–5761 [DOI] [PubMed] [Google Scholar]
- 6.Russell AP, Gastaldi G, Bobbioni-Harsch E, et al. Lipid peroxidation in skeletal muscle of obese as compared to endurance-trained humans: a case of good vs. bad lipids? FEBS Lett 2003;551:104–106 [DOI] [PubMed] [Google Scholar]
- 7.Itani SI, Ruderman NB, Schmieder F, Boden G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IκB-α. Diabetes 2002;51:2005–2011 [DOI] [PubMed] [Google Scholar]
- 8.Adams JM, 2nd, Pratipanawatr T, Berria R, et al. Ceramide content is increased in skeletal muscle from obese insulin-resistant humans. Diabetes 2004;53:25–31 [DOI] [PubMed] [Google Scholar]
- 9.Skovbro M, Baranowski M, Skov-Jensen C, et al. Human skeletal muscle ceramide content is not a major factor in muscle insulin sensitivity. Diabetologia 2008;51:1253–1260 [DOI] [PubMed] [Google Scholar]
- 10.Perreault L, Bergman BC, Hunerdosse DM, Eckel RH. Altered intramuscular lipid metabolism relates to diminished insulin action in men, but not women, in progression to diabetes. Obesity (Silver Spring) 2010;18:2093–2100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pruchnic R, Katsiaras A, He J, Kelley DE, Winters C, Goodpaster BH. Exercise training increases intramyocellular lipid and oxidative capacity in older adults. Am J Physiol Endocrinol Metab 2004;287:E857–E862 [DOI] [PubMed] [Google Scholar]
- 12.Dubé JJ, Amati F, Stefanovic-Racic M, Toledo FG, Sauers SE, Goodpaster BH. Exercise-induced alterations in intramyocellular lipids and insulin resistance: the athlete’s paradox revisited. Am J Physiol Endocrinol Metab 2008;294:E882–E888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bergman BC, Perreault L, Hunerdosse DM, Koehler MC, Samek AM, Eckel RH. Intramuscular lipid metabolism in the insulin resistance of smoking. Diabetes 2009;58:2220–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bruce CR, Thrush AB, Mertz VA, et al. Endurance training in obese humans improves glucose tolerance and mitochondrial fatty acid oxidation and alters muscle lipid content. Am J Physiol Endocrinol Metab 2006;291:E99–E107 [DOI] [PubMed] [Google Scholar]
- 15.Zhang D, Christianson J, Liu ZX, et al. Resistance to high-fat diet-induced obesity and insulin resistance in mice with very long-chain acyl-CoA dehydrogenase deficiency. Cell Metab 2010;11:402–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolins NE, Quaynor BK, Skinner JR, et al. OXPAT/PAT-1 is a PPAR-induced lipid droplet protein that promotes fatty acid utilization. Diabetes 2006;55:3418–3428 [DOI] [PubMed] [Google Scholar]
- 17.Minnaard R, Schrauwen P, Schaart G, et al. Adipocyte differentiation-related protein and OXPAT in rat and human skeletal muscle: involvement in lipid accumulation and type 2 diabetes mellitus. J Clin Endocrinol Metab 2009;94:4077–4085 [DOI] [PubMed] [Google Scholar]
- 18.Pham DL, Xu C, Prince JL. Current methods in medical image segmentation. Annu Rev Biomed Eng 2000;2:315–337 [DOI] [PubMed] [Google Scholar]
- 19.Goodpaster BH, Theriault R, Watkins SC, Kelley DE. Intramuscular lipid content is increased in obesity and decreased by weight loss. Metabolism 2000;49:467–472 [DOI] [PubMed] [Google Scholar]
- 20.Bielawski J, Szulc ZM, Hannun YA, Bielawska A. Simultaneous quantitative analysis of bioactive sphingolipids by high-performance liquid chromatography-tandem mass spectrometry. Methods 2006;39:82–91 [DOI] [PubMed] [Google Scholar]
- 21.Shah C, Yang G, Lee I, Bielawski J, Hannun YA, Samad F. Protection from high fat diet-induced increase in ceramide in mice lacking plasminogen activator inhibitor 1. J Biol Chem 2008;283:13538–13548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toledo FG, Menshikova EV, Azuma K, et al. Mitochondrial capacity in skeletal muscle is not stimulated by weight loss despite increases in insulin action and decreases in intramyocellular lipid content. Diabetes 2008;57:987–994 [DOI] [PubMed] [Google Scholar]
- 23.Erion DM, Shulman GI. Diacylglycerol-mediated insulin resistance. Nat Med 2010;16:400–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coen PM, Dubé JJ, Amati F, et al. Insulin resistance is associated with higher intramyocellular triglycerides in type I but not type II myocytes concomitant with higher ceramide content. Diabetes 2010;59:80–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jocken JW, Moro C, Goossens GH, et al. Skeletal muscle lipase content and activity in obesity and type 2 diabetes. J Clin Endocrinol Metab 2010;95:5449–5453 [DOI] [PubMed] [Google Scholar]
- 26.Levin MC, Monetti M, Watt MJ, et al. Increased lipid accumulation and insulin resistance in transgenic mice expressing DGAT2 in glycolytic (type II) muscle. Am J Physiol Endocrinol Metab 2007;293:E1772–E1781 [DOI] [PubMed] [Google Scholar]
- 27.Dubé JJ, Amati F, Toledo FG, et al. Effects of weight loss and exercise on insulin resistance, and intramyocellular triacylglycerol, diacylglycerol and ceramide. Diabetologia 2011;54:1147–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bergman BC, Perreault L, Hunerdosse DM, Koehler MC, Samek AM, Eckel RH. Increased intramuscular lipid synthesis and low saturation relate to insulin sensitivity in endurance-trained athletes. J Appl Physiol 2010;108:1134–1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Straczkowski M, Kowalska I, Baranowski M, et al. Increased skeletal muscle ceramide level in men at risk of developing type 2 diabetes. Diabetologia 2007;50:2366–2373 [DOI] [PubMed] [Google Scholar]
- 30.Helge JW, Dobrzyn A, Saltin B, Gorski J. Exercise and training effects on ceramide metabolism in human skeletal muscle. Exp Physiol 2004;89:119–127 [DOI] [PubMed] [Google Scholar]
- 31.Consitt LA, Bell JA, Houmard JA. Intramuscular lipid metabolism, insulin action, and obesity. IUBMB Life 2009;61:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holland WL, Scherer PE. PAQRs: a counteracting force to ceramides? Mol Pharmacol 2009;75:740–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ussher JR, Koves TR, Cadete VJ, et al. Inhibition of de novo ceramide synthesis reverses diet-induced insulin resistance and enhances whole body oxygen consumption. Diabetes 2010;59:2453–2464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lanza IR, Nair KS. Mitochondrial function as a determinant of life span. Pflugers Arch 2010;459:277–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spiegel S, Milstien S. Sphingosine-1-phosphate: an enigmatic signalling lipid. Nat Rev Mol Cell Biol 2003;4:397–407 [DOI] [PubMed] [Google Scholar]
- 36.Straczkowski M, Kowalska I. The role of skeletal muscle sphingolipids in the development of insulin resistance. Rev Diabet Stud 2008;5:13–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hannun YA. Sphingolipid second messengers: tumor suppressor lipids. Adv Exp Med Biol 1997;400A:305–312 [DOI] [PubMed] [Google Scholar]
- 38.Cuvillier O. Sphingosine in apoptosis signaling. Biochim Biophys Acta 2002;1585:153–162 [DOI] [PubMed] [Google Scholar]
- 39.Cuvillier O, Pirianov G, Kleuser B, et al. Suppression of ceramide-mediated programmed cell death by sphingosine-1-phosphate. Nature 1996;381:800–803 [DOI] [PubMed] [Google Scholar]
- 40.van Echten-Deckert G, Klein A, Linke T, Heinemann T, Weisgerber J, Sandhoff K. Turnover of endogenous ceramide in cultured normal and Farber fibroblasts. J Lipid Res 1997;38:2569–2579 [PubMed] [Google Scholar]
- 41.Le Stunff H, Galve-Roperh I, Peterson C, Milstien S, Spiegel S. Sphingosine-1-phosphate phosphohydrolase in regulation of sphingolipid metabolism and apoptosis. J Cell Biol 2002;158:1039–1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taha TA, Kitatani K, El-Alwani M, Bielawski J, Hannun YA, Obeid LM. Loss of sphingosine kinase-1 activates the intrinsic pathway of programmed cell death: modulation of sphingolipid levels and the induction of apoptosis. FASEB J 2006;20:482–484 [DOI] [PubMed] [Google Scholar]
- 43.Edsall LC, Cuvillier O, Twitty S, Spiegel S, Milstien S. Sphingosine kinase expression regulates apoptosis and caspase activation in PC12 cells. J Neurochem 2001;76:1573–1584 [DOI] [PubMed] [Google Scholar]
- 44.Samad F, Hester KD, Yang G, Hannun YA, Bielawski J. Altered adipose and plasma sphingolipid metabolism in obesity: a potential mechanism for cardiovascular and metabolic risk. Diabetes 2006;55:2579–2587 [DOI] [PubMed] [Google Scholar]
- 45.Yamaguchi T, Matsushita S, Motojima K, Hirose F, Osumi T. MLDP, a novel PAT family protein localized to lipid droplets and enriched in the heart, is regulated by peroxisome proliferator-activated receptor alpha. J Biol Chem 2006;281:14232–14240 [DOI] [PubMed] [Google Scholar]
- 46.Dalen KT, Dahl T, Holter E, et al. LSDP5 is a PAT protein specifically expressed in fatty acid oxidizing tissues. Biochim Biophys Acta 2007;1771:210–227 [DOI] [PubMed] [Google Scholar]
- 47.Biddinger SB, Almind K, Miyazaki M, Kokkotou E, Ntambi JM, Kahn CR. Effects of diet and genetic background on sterol regulatory element-binding protein-1c, stearoyl-CoA desaturase 1, and the development of the metabolic syndrome. Diabetes 2005;54:1314–1323 [DOI] [PubMed] [Google Scholar]
- 48.Hulver MW, Berggren JR, Carper MJ, et al. Elevated stearoyl-CoA desaturase-1 expression in skeletal muscle contributes to abnormal fatty acid partitioning in obese humans. Cell Metab 2005;2:251–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schenk S, Horowitz JF. Acute exercise increases triglyceride synthesis in skeletal muscle and prevents fatty acid-induced insulin resistance. J Clin Invest 2007;117:1690–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yao-Borengasser A, Varma V, Coker RH, et al. Adipose triglyceride lipase expression in human adipose tissue and muscle: role in insulin resistance and response to training and pioglitazone. Metabolism 2010;60:1012–1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alsted TJ, Nybo L, Schweiger M, et al. Adipose triglyceride lipase in human skeletal muscle is upregulated by exercise training. Am J Physiol Endocrinol Metab 2009;296:E445–E453 [DOI] [PubMed] [Google Scholar]
- 52.Ellis BA, Poynten A, Lowy AJ, et al. Long-chain acyl-CoA esters as indicators of lipid metabolism and insulin sensitivity in rat and human muscle. Am J Physiol Endocrinol Metab 2000;279:E554–E560 [DOI] [PubMed] [Google Scholar]
- 53.Bajaj M, Suraamornkul S, Romanelli A, et al. Effect of a sustained reduction in plasma free fatty acid concentration on intramuscular long-chain fatty acyl-CoAs and insulin action in type 2 diabetic patients. Diabetes 2005;54:3148–3153 [DOI] [PubMed] [Google Scholar]