Abstract
Purpose
To review the ability of current imaging technologies to provide estimates of rates of structural change in glaucoma patients.
Patients and methods
Review of literature.
Results
Imaging technologies, such as confocal scanning laser ophthalmoscopy (CSLO), scanning laser polarimetry (SLP), and optical coherence tomography (OCT), provide quantifiable and reproducible measurements of the optic disc and parapapillary retinal nerve fibre layer (RNFL). Rates of change as quantified by the rim area (RA) (for CSLO) and RNFL thickness (for SLP and OCT) are related to glaucoma progression as detected by conventional methods (eg, visual fields and optic disc photography). Evidence shows that rates of RNFL and RA loss are significantly faster in progressing compared with non-progressing glaucoma patients.
Conclusion
Measurements of rates of optic disc and RNFL change are becoming increasingly precise and individualized. Currently available imaging technologies have the ability to detect and quantify progression in glaucoma, and their measurements may be suitable end points in glaucoma clinical trials.
Keywords: glaucoma, rate of change, scanning laser polarimetry, confocal scanning laser ophthalmoscopy, optical coherence tomography, imaging technology
Introduction
Glaucoma is a complex and progressive disease characterized by an optic neuropathy that is usually associated with typical visual function loss.1 Although most glaucoma patients will show some evidence of progression, if followed long enough, the rate of deterioration can be highly variable among them. Some patients may progress slowly over the course of many years or decades with minimal impact on the quality of vision, whereas others may have aggressive disease with rapid rates of change that can eventually result in blindness or substantial impairment unless appropriate interventions take place. Therefore, the evaluation of rates of change in glaucoma is essential to allow proper allocation of resources towards the patients who are most likely to develop impairment. In fact, according to the Consensus on Medical Treatment from the World Glaucoma Association, glaucoma treatment is indicated for patients whose rates of progression will most likely result in loss in vision-related quality of life over the projected remaining years of life.2
A complete assessment of rates of disease progression requires both structural and functional measures, as it is known that many patients seem to progress by one method and not the other.3, 4, 5, 6 Although functional outcomes have an unquestionable relevance to patients, it has been shown that structural changes can often precede functional losses and be an earlier marker of deterioration. More importantly, a recent study showed that structural changes observed on optic disc stereophotographs are predictive of future functional losses and, therefore, carry clinically relevant prognostic information.7 However, although optic disc stereophotographs have been considered the gold standard for evaluation of structural damage in glaucoma, evaluation of rates of structural change using stereophotographs is difficult because of the qualitative and subjective nature of this assessment.
Over the past two decades, several technologies, such as confocal scanning laser ophthalmoscopy (CSLO), scanning laser polarimetry (SLP), and optical coherence tomography (OCT), have been used to quantitatively and objectively measure the topography of the optic disc and thickness of the parapapillary retinal nerve fibre layer (RNFL).8 Results from these imaging technologies can be used to predict glaucoma development,9, 10, 11, 12, 13 and have the potential to detect and measure structural progression.7, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 Recent literature has focused on the ability of these instruments to provide estimates of rates of change over time. In this review, we discuss the evidence with regard to the ability of current imaging technologies in measuring rates of structural change in glaucoma and their relationship to conventional methods for assessment of disease progression.
CSLO
CSLO was introduced more than 20 years ago. It enables reproducible measurements of the surface height of the optic nerve head (ONH) and parapapillary retina.9 The most recent implementation of this technology (Heidelberg Retina Tomograph (HRT), Heidelberg Engineering GmbH, Heidelberg, Germany) has been widely used to evaluate topographic changes of the ONH to detect progression of glaucoma.13, 24, 25, 26 Although different stereometric parameters have been suggested as useful markers of progression, some studies have suggested that the neuroretinal rim area (RA) is the most reliable and reproducible measure for detection of change.27, 28 Changes in RA have been demonstrated in glaucoma patients followed over time and are associated with disease progression.14, 15, 22, 28, 29, 30, 31, 32, 33, 34 Baseline measurements obtained by the HRT have also been shown to predict future conversion to glaucoma in patients suspected of having the disease, although the predictive accuracy of the measurements on individual patients is generally low.13
CSLO measurements have been used to evaluate rates of glaucoma progression in several studies. Strouthidis et al22 initially used rates of change in RA to compare detection of progression by visual fields and CSLO in patients with ocular hypertension. They did not, however, report absolute values of change. See et al,33 observing 94 glaucoma patients and 54 normal controls over 8.6±2.9 years, found a rate of change (RA loss/year) of −0.0053 and −0.0012 mm2/year, respectively (Figure 1). Strouthidis et al35 found that the rate of RA loss was greatest in the inferotemporal (−1.43%/year) and superotemporal sectors (−1.05%/year). Poli et al36 also assessed rates of change with the CSLO. In 31 subjects with ocular hypertension and reproducible visual field loss and 19 normal subjects, they reported global RA mean slopes of −0.0123 mm2/year. Alencar et al15 studied 629 eyes of 390 patients. Over an average of 3.3±0.7 years of follow-up, the average rate of RA decline was not significantly different between glaucoma progressors and non-progressors (−0.0058 vs −0.0073 mm2/year, respectively; P=0.727). The area under the receiver-operating characteristic (ROC) curve for this parameter showed a poor discriminatory ability, no better than chance. However, when eyes that had undergone glaucoma surgery were excluded, the rates of RA loss became significantly different between progressors (−0.020 mm2/year) and non-progressors (−0.007 mm2/year; P=0.015). This is probably explained by the effect of intraocular pressure (IOP) reduction in causing a significant reversal of ONH cupping, which may be interpreted as an increase in RA by the CSLO and confound evaluation of RA change in patients who underwent surgery during follow-up.29, 37, 38
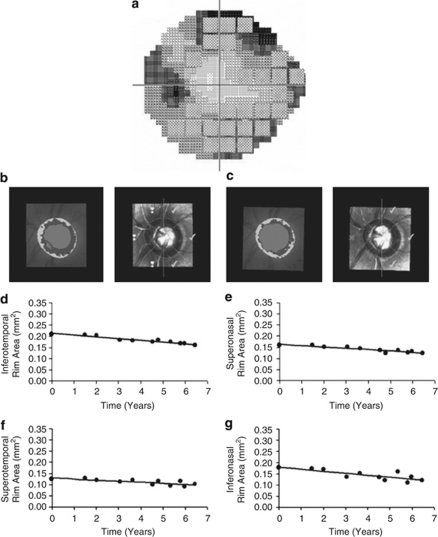
Figure 1.
Disc and field progression in subject 9. (a) Visual field grey scale at the conclusion of the study; the hatched squares indicate the test points flagged as progressing according to the standard PLR criteria; (b) HRT baseline mean topography; (c) HRT mean topography at the conclusion of the study period. (d–g) Scatterplots with regression line for sectoral RA against time. (From Strouthidis et al22).
A shortcoming of the CSLO technology stems from the variation induced by tracing a contour line to outline the optic disc. Alternative approaches for detecting progression in series of CSLO images, such as the topographic change analysis,26, 31, 39, 40 the glaucoma probability score,14, 25, 41, 42 and statistic image mapping,43, 44 have been developed and obviate the need for a contour line. These methods, however, exhibit only moderate agreement with each other and have poor agreement with expert-assessed change in optic disc stereophotographs.45
In the context of detecting progressive glaucoma, one advantage of the CSLO, when comparing it to other imaging devices, is that latest commercially available versions of the instrument have shown relatively good compatibility with older ones, which is of significant benefit to clinicians and researchers who need to follow up patients for long periods of time.
SLP
SLP (GDx; Carl Zeiss Meditec Inc., Dublin, CA, USA) is a confocal scanning laser ophthalmoscope with an integrated polarimeter that measures the amount of retardation (phase shift) of a polarized near-infrared laser beam as it passes through the RNFL.45 Changes in RNFL have been suggested to be the earliest sign of glaucoma development in many patients and to precede visual field loss.46 The SLP enables clinicians to evaluate the parapapillary RNFL objectively and quantitatively. This technology has been shown to provide reproducible RNFL measurements and to differentiate glaucoma patients from normal subjects with sensitivities and specificities between 72 and 78%, and 56 and 92%, respectively.47, 48, 49, 50, 51, 52
Imaging artifacts such as a poorly compensated corneal birefringence can hamper the accuracy of the device in clinical practice.53 The introduction of a variable corneal polarization compensator (GDxVCC) attempted to alleviate this problem and resulted in improved diagnostic accuracy.54 The GDxVCC scans, however, were found to be limited by atypical retardation patterns (ARPs). ARPs result from poor noise-to-signal ratio as a consequence of light scattering in the eye. Medeiros et al18 have shown that the presence of ARP on SLP scans adversely affects the detection of progressive glaucomatous RNFL loss. The most recent commercially available version (GDxPRO) is a modification of the GDxVCC and provides an enhanced corneal compensation (ECC) to eliminate artifacts associated with ARP.54, 55
The GDx software has been recently upgraded with the addition of a guided progression analysis (GPA). The GPA software compares SLP images acquired during follow-up and reports a summary analysis for progression in an individual eye after automated consideration of the expected test–retest variability. It has been shown to be able to identify a significant proportion of glaucoma progression with 50% sensitivity and 96% specificity compared with optic disc stereophotographs and visual fields.16 Repeatability of GDxVCC was demonstrated to be stable for all stages of disease severity with a repeatability coefficient within 4 μm (compared with 6 μm with Stratus OCT, Carl Zeiss Meditec Inc.).42
Recently, several authors calculated rates of change for the GDx. Using GDxVCC, Medeiros et al17 imaged individuals with suspected and established glaucoma. They reported an average loss of RNFL thickness of −0.70 μm/year in glaucoma progressors (based on GPA software for standard automated perimetry (SAP)) vs −0.14 μm/year in non-progressors (P<0.001), very similar to rates of change reported elsewhere by the same group (−0.65 and −0.11 μm/year, respectively).15 Da Pozzo et al,56 in a cross-sectional design estimated the age-related loss of RNFL thickness in 384 healthy adults and found a rate of −0.08 μm/year attributed to ageing.
To date, four longitudinal studies have evaluated GDxECC for detection of progression in glaucoma, with two of them comparing measurements obtained by GDxECC with GDxVCC.19, 21, 57, 58 Medeiros et al19 evaluated the relationship between IOP and progressive RNFL loss in a cohort recruited from the Diagnostic Innovations in Glaucoma Study (DIGS). Patients who manifested progression of glaucoma on SAP–GPA showed a significantly higher rate of RNFL change compared with non-progressors (−0.95 vs −0.17 μm/year; P=0.001). Considering an average baseline thickness of 47 μm for the RNFL, this amount of loss in progressors would represent an almost 2% loss per year. Each 1-mmHg higher IOP was associated with an additional RNFL loss of 0.13 μm/year in progressors compared with 0.05 μm/year overall. They further showed that rates of change were higher in inferior and temporal sectors, which is in agreement with the expected pattern of glaucomatous damage to the RNFL and to the neuroretinal rim (Figure 2).59 The same investigators in a subsequent publication reported an average rate of decline for RNFL thickness measurements of −1.24 μm/year in progressors vs −0.34 μm/year in non-progressors, with a significantly higher area under the ROC curve for detecting change for ECC compared with VCC (0.89 vs 0.65; P<0.001) (Figure 3).21 Grewal et al57 demonstrated that ECC identified more cases of progression than VCC (11.8 vs 8.8%), with only moderate agreement (κ=0.57). In a subsequent publication,58 the same investigators using ECC found rates of annual RNFL loss of −1.11 μm/year (progressors) vs −0.41 μm/year (non-progressors), when progression was defined based on the SAP visual field index.
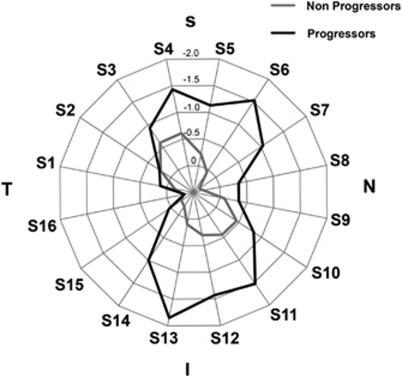
Figure 2.
Radar plot illustrating the rates of change in SLP with ECC retinal nerve fibre layer measurements according to the sectors around the optic disc. Eyes that showed progression on visual fields and/or optic disc stereophotographs had greater loss of the RNFL in the inferior and superior sectors. I, inferior; N, nasal; S, superior; T, temporal. (From Medeiros et al19).
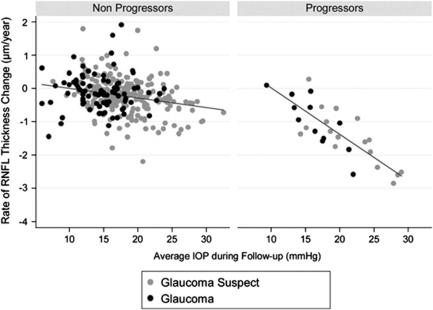
Figure 3.
Scatterplot illustrating the relationship between rates of change in the SLP with ECC parameter temporal–superior–nasal–inferior–temporal average and IOP. Rates of change are shown for eyes that progressed by visual fields and/or stereophotographs (progressors) as well as for eyes that did not (non-progressors). (From Medeiros et al19).
A significant limitation of SLP is the lack of interchangeability among serial generations of the commercial instrument. RNFL thickness measurements obtained with the GDxVCC and GDxECC are not interchangeable. Thus, a new baseline must be established in the case of conversion to GDxECC.
OCT
OCT is a non-contact and non-invasive technique for examination of the human retina. Briefly, the instrument uses a super luminescent diode light and works similar to a B-scan ultrasound, using light instead of sound. Unlike the CSLO and the SLP, OCTs are currently available from several different manufactures, with different axial resolution and lower acquisition time. We focus, herein, on the Stratus OCT because very little longitudinal data are currently available for the spectral-domain OCTs.
Wollstein et al60 showed the potential use of OCT in detecting glaucomatous progression with an event-based approach (ie, a change greater than the expected variability was considered progression). Using a prototype, they concluded that the OCT was more sensitive than standard visual fields for the detection of progression. In fact, 22% of eyes had a significant change measured by the OCT without corresponding deterioration of the visual fields. However, it was not clear whether these eyes were true progressors undetected by visual fields or false positives due to variability of the measurements or age-related thinning of the RNFL.
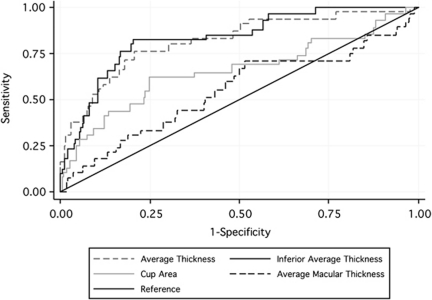
Medeiros et al20 evaluated the ability of RNFL thickness, ONH, and macular thickness measurements to detect glaucomatous progression. In their study, progression was determined by SAP and longitudinal assessment of optic disc stereophotographs. They reported the RNFL thickness parameters as having better ability than ONH and macular thickness parameters to detect progression (Figure 4). This is in agreement with previous cross-sectional studies that showed a poor performance of Stratus OCT-derived macular and ONH parameters for cross-sectional detection of glaucoma.61 For average RNFL thickness, a rate of change of −0.72 μm (∼1%)/year for the progressors compared with 0.14 μm/year in non-progressors was reported. The authors found a wide variation of rates of change, which has also been reported by Leung et al62 in a study evaluating the GPA software of Stratus OCT. Although this wide range can be explained by individual characteristics, such as stage of disease and response to treatment, it is possible that non-centered scans and signal strength affected the ability to detect change.63, 64 Nonetheless, the wide individual variation should be considered when evaluating patients on a case-by-case basis.
Figure 4.
ROC curves of rates of change for discriminating progressors from non-progressors of the three parameters with largest areas under the ROC curves in each scanning area and the average RNFL thickness. (From Medeiros et al20).
The recent introduction of spectral domain OCT (SDOCT) has enhanced resolution and decreased scan acquisition time compared with Stratus OCT. With more reproducible images,65, 66 there is potential for improved ability to detect glaucomatous progression. Further, with this higher resolution, new scan types are now possible. One example is the ganglion cell complex (GCC) that selectively measures the inner retina in the macular region. The GCCs have shown similar diagnostic accuracy for detecting glaucoma as the RNFL thickness, and may be useful for monitoring the disease.67 Recently, Leung et al (Leung CK et al, personal communication) evaluated the ability to detect RNFL progression using Stratus OCT and SDOCT. A total of 128 eyes were followed for a minimum of 24 months. They found more progressors using SDOCT compared with Stratus OCT (23.5% of patients with SDOCT vs 4.9% with Stratus OCT). The agreement with visual field progression was also better with SDOCT. In addition, five eyes had an increasing RNFL thickness with Stratus OCT, indicating an inherent measurement variability of the instrument. The agreement for detection of RNFL progression was poor between the two instruments (k=0.188). The rate of change ranged between −1.52 and −5.03 μm/year with SDOCT, and between −2.22 and −7.60 μm/year with Stratus OCT.
Table 1 summarizes the ability of all the three imaging technologies to provide rates of change.
Table 1. Mean rates of change for patients with progressive glaucoma as measured by CLSO, SLP (GDxVCC and GDxECC), and Stratus OCT.
| Imaging technology | Study | Parameter |
Mean rates of change |
AROC | |
|---|---|---|---|---|---|
| Progressors | Non-progressors | ||||
| CSLO | Alencar et al1 | RA average (mm2/year) | −0.0058 | −0.0073 | 0.51 (95% CI, 0.40–0.61) |
| Poli et al2a | RA average (mm2/year) | −0.0123 | NA | NA | |
| See et al3 | RA average (mm2/year) | −0.0053 | −0.0012 | NA | |
| GDxECC | Medeiros et al4 | TSNIT average (μm/year) | −0.95 | −0.17 | NA |
| Medeiros et al5 | TSNIT average (μm/year) | −1.24 | −0.34 | 0.89 (95% CI, 0.83–0.95) | |
| Grewal et al6b | TSNIT average (μm/year) | −1.11 | −0.41 | NA | |
| GDxVCC | Medeiros et al7c | TSNIT average (μm/year) | −0.70 | −0.14 | NA |
| Medeiros et al5d | TSNIT average (μm/year) | −0.46 | −0.15 | 0.65 (95% CI, 0.53–0.77) | |
| Alencar et al1 | TSNIT average (μm/year) | −0.65 | −0.11 | 0.81 (95% CI, 0.74–0.88) | |
| Stratus OCT | Medeiros et al8 | TSNIT average (μm/year) | −0.72 | −0.14 | 0.83 (95% CI, 0.72–0.92) |
| Leung et al9 | TSINT average (μm/year) | −3.30 (median) | NA | NA | |
Abbreviations: AROC, area under the receiver operating characteristic curve; ARP, atypical patterns of retardation; CI, confidence interval; CLSO, confocal scanning laser ophthalmoscopy; ECC, enhanced corneal compensation; NA, not applicable; OCT, optical coherence tomography; RA, rim area; SAP, standard automated perimetry; SLP, scanning laser polarimetry; TSNIT, temporal–superior–nasal–inferior–temporal.
Calculated for ‘converters' (defined as normal or ocular hypertensive subjects who progressed to glaucoma).
Progression was defined by the slope of the visual field index on SAP.
Included scans with ARP.
Excluded scans with ARP.
Summary and future directions
Currently available imaging technologies have been demonstrated to detect and quantify glaucomatous progression in a reproducible manner. Rates of change in RNFL thickness and optic disc topographic measurements as measured by different instruments have been shown to correlate significantly with conventional methods for assessment of change, such as SAP and optic disc stereophotographs. Several studies have shown that rates of structural damage are faster in eyes with progressive glaucoma, and show a correlation with important risk factors for the disease such as IOP.
Advances in the assessment of change with imaging devices may shift the macroscopic standard of optic disc photographs towards the microscopic and three-dimensional imaging of the retinal layers. With the increasing resolution and reliability of imaging technologies, it is likely that the estimation of these rates of change will be more precise and individualized in the near future. In addition, advances and implementation of image stabilization technologies should improve reproducibility of structural measurements to enable better differentiation of variability from true progression.
At present, the Food and Drug Administration (FDA) recognizes IOP as an efficacy end point for IOP-lowering drugs and visual field testing, visual acuity, contrast sensitivity, and colour vision as functional end points.68 IOP is an imperfect surrogate for the clinical outcomes of glaucoma, as disease can progress despite low IOP or remain stable despite IOP levels considered high.69, 70, 71 The use of visual fields as an end point is potentially limited by the need for large samples, long follow-up, variability of results, and inconsistency in criteria for defining progression.72 The absence of regulatory support for other glaucoma end points has been identified as a weakness in exploring candidate agents for neuroprotective therapy and alternative surrogate end points have been sought. Structural measurements obtained by imaging technologies have the potential to overcome these obstacles, and could potentially act as useful biomarkers and surrogate end points to be used in glaucoma clinical trials. Future research should be directed at evaluating, quantifying, and comparing the abilities of structural change measured by different imaging technologies in predicting clinically relevant outcomes in glaucoma.
Acknowledgments
This study was supported, in part, by NEI R01-EY08208 (FAM) and CAPES Grant BEX1327/09-7 (MTL).
K Mansouri, none; MT Leite, none; FA Medeiros, Carl Zeiss Meditec Inc. (F, R), Alcon (C, R), Allergan (C, F), Merck (C, F), Pfizer Inc. (C, F, R), and Reichert Inc. (R); RN Weinreb, Carl Zeiss Meditec Inc. (C, F); Heidelberg Engineering, GmbH (F); Optovue Inc. (C, F); and Topcon Medical Systems Inc. (F, R).
References
- Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363 (9422:1711–1720. doi: 10.1016/S0140-6736(04)16257-0. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Susanna R, Singh K.Who should be treatedIn: Weinreb RN, Araie M, Susanna R, Goldberg I, Migdal C, Liebmann J (eds).Medical Treatment of Glaucoma Kugler Publications: Amsterdam/The Netherlands; 20101–19. [Google Scholar]
- Nicolela MT, McCormick TA, Drance SM, Ferrier SN, LeBlanc RP, Chauhan BC. Visual field and optic disc progression in patients with different types of optic disc damage: a longitudinal prospective study. Ophthalmology. 2003;110 (11:2178–2184. doi: 10.1016/S0161-6420(03)00801-7. [DOI] [PubMed] [Google Scholar]
- Wollstein G, Schuman JS, Price LL, Aydin A, Stark PC, Hertzmark E, et al. Optical coherence tomography longitudinal evaluation of retinal nerve fiber layer thickness in glaucoma. Arch Ophthalmol. 2005;123 (4:464–470. doi: 10.1001/archopht.123.4.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan BC, McCormick TA, Nicolela MT, LeBlanc RP. Optic disc and visual field changes in a prospective longitudinal study of patients with glaucoma: comparison of scanning laser tomography with conventional perimetry and optic disc photography. Arch Ophthalmol. 2001;119 (10:1492–1499. doi: 10.1001/archopht.119.10.1492. [DOI] [PubMed] [Google Scholar]
- Harwerth RS, Wheat JL, Fredette MJ, Anderson DR. Linking structure and function in glaucoma. Prog Retin Eye Res. 2010;29 (4:249–271. doi: 10.1016/j.preteyeres.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol. 2009;127 (10:1250–1256. doi: 10.1001/archophthalmol.2009.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield DS, Weinreb RN. Role of optic nerve imaging in glaucoma clinical practice and clinical trials. Am J Ophthalmol. 2008;145 (4:598–603. doi: 10.1016/j.ajo.2007.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreher AW, Tso PC, Weinreb RN. Reproducibility of topographic measurements of the normal and glaucomatous optic nerve head with the laser tomographic scanner. Am J Ophthalmol. 1991;111 (2:221–229. doi: 10.1016/s0002-9394(14)72263-9. [DOI] [PubMed] [Google Scholar]
- Mohammadi K, Bowd C, Weinreb RN, Medeiros FA, Sample PA, Zangwill LM. Retinal nerve fiber layer thickness measurements with scanning laser polarimetry predict glaucomatous visual field loss. Am J Ophthalmol. 2004;138 (4:592–601. doi: 10.1016/j.ajo.2004.05.072. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Bowd C, Weinreb RN. Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol. 2004;122 (6:827–837. doi: 10.1001/archopht.122.6.827. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Bowd C, Mohammadi K, Weinreb RN. Comparison of scanning laser polarimetry using variable corneal compensation and retinal nerve fiber layer photography for detection of glaucoma. Arch Ophthalmol. 2004;122 (5:698–704. doi: 10.1001/archopht.122.5.698. [DOI] [PubMed] [Google Scholar]
- Zangwill LM, Weinreb RN, Beiser JA, Berry CC, Cioffi GA, Coleman AL, et al. Baseline topographic optic disc measurements are associated with the development of primary open-angle glaucoma: the Confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2005;123 (9:1188–1197. doi: 10.1001/archopht.123.9.1188. [DOI] [PubMed] [Google Scholar]
- Alencar LM, Bowd C, Weinreb RN, Zangwill LM, Sample PA, Medeiros FA. Comparison of HRT-3 glaucoma probability score and subjective stereophotograph assessment for prediction of progression in glaucoma. Invest Ophthalmol Vis Sci. 2008;49 (5:1898–1906. doi: 10.1167/iovs.07-0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alencar LM, Zangwill LM, Weinreb RN, Bowd C, Sample PA, Girkin CA, et al. A comparison of rates of change in neuroretinal rim area and retinal nerve fiber layer thickness in progressive glaucoma. Invest Ophthalmol Vis Sci. 2010;51 (7:3531–3539. doi: 10.1167/iovs.09-4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alencar LM, Zangwill LM, Weinreb RN, Bowd C, Vizzeri G, Sample PA, et al. Agreement for detecting glaucoma progression with the GDx guided progression analysis, automated perimetry, and optic disc photography. Ophthalmology. 2010;117 (3:462–470. doi: 10.1016/j.ophtha.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Vizzeri G, Sample PA, et al. Detection of progressive retinal nerve fiber layer loss in glaucoma using scanning laser polarimetry with variable corneal compensation. Invest Ophthalmol Vis Sci. 2009;50 (4:1675–1681. doi: 10.1167/iovs.08-2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Alencar LM, Zangwill LM, Sample PA, Susanna R, Jr, Weinreb RN.Impact of atypical retardation patterns on detection of glaucoma progression using the GDx with variable corneal compensation Am J Ophthalmol 2009148(1155–163.e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Alencar LM, Zangwill LM, Sample PA, Weinreb RN.The Relationship between intraocular pressure and progressive retinal nerve fiber layer loss in glaucoma Ophthalmology 2009116(61125–1133.e1121–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Alencar LM, Bowd C, Sample PA, Susanna R, Jr, et al. Detection of glaucoma progression with stratus OCT retinal nerve fiber layer, optic nerve head, and macular thickness measurements. Invest Ophthalmol Vis Sci. 2009;50 (12:5741–5748. doi: 10.1167/iovs.09-3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Alencar LM, Sample PA, Weinreb RN. Rates of progressive retinal nerve fiber layer loss in glaucoma measured by scanning laser polarimetry. Am J Ophthalmol. 2010;149 (6:908–915. doi: 10.1016/j.ajo.2010.01.010. [DOI] [PubMed] [Google Scholar]
- Strouthidis NG, Scott A, Peter NM, Garway-Heath DF. Optic disc and visual field progression in ocular hypertensive subjects: detection rates, specificity, and agreement. Invest Ophthalmol Vis Sci. 2006;47 (7:2904–2910. doi: 10.1167/iovs.05-1584. [DOI] [PubMed] [Google Scholar]
- Tan JC, Hitchings RA. Approach for identifying glaucomatous optic nerve progression by scanning laser tomography. Invest Ophthalmol Vis Sci. 2003;44 (6:2621–2626. doi: 10.1167/iovs.02-0850. [DOI] [PubMed] [Google Scholar]
- Tan JC, Hitchings RA. Optimizing and validating an approach for identifying glaucomatous change in optic nerve topography. Invest Ophthalmol Vis Sci. 2004;45 (5:1396–1403. doi: 10.1167/iovs.03-0025. [DOI] [PubMed] [Google Scholar]
- Weinreb RN, Zangwill LM, Jain S, Becerra LM, Dirkes K, Piltz-Seymour JR, et al. Predicting the onset of glaucoma: the confocal scanning laser ophthalmoscopy ancillary study to theOcular Hypertension Treatment Study. Ophthalmology. 2010;117 (9:1674–1683. doi: 10.1016/j.ophtha.2010.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan BC, Blanchard JW, Hamilton DC, LeBlanc RP. Technique for detecting serial topographic changes in the optic disc and peripapillary retina using scanning laser tomography. Invest Ophthalmol Vis Sci. 2000;41 (3:775–782. [PubMed] [Google Scholar]
- Strouthidis NG, White ET, Owen VM, Ho TA, Hammond CJ, Garway-Heath DF. Factors affecting the test-retest variability of Heidelberg retina tomograph and Heidelberg retina tomograph II measurements. Br J Ophthalmol. 2005;89 (11:1427–1432. doi: 10.1136/bjo.2005.067298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan JC, Garway-Heath DF, Hitchings RA. Variability across the optic nerve head in scanning laser tomography. Br J Ophthalmol. 2003;87 (5:557–559. doi: 10.1136/bjo.87.5.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowd C, Weinreb RN, Lee B, Emdadi A, Zangwill LM. Optic disk topography after medical treatment to reduce intraocular pressure. Am J Ophthalmol. 2000;130 (3:280–286. doi: 10.1016/s0002-9394(00)00488-8. [DOI] [PubMed] [Google Scholar]
- Chauhan BC, Hutchison DM, Artes PH, Caprioli J, Jonas JB, LeBlanc RP, et al. Optic disc progression in glaucoma: comparison of confocal scanning laser tomography to optic disc photographs in a prospective study. Invest Ophthalmol Vis Sci. 2009;50 (4:1682–1691. doi: 10.1167/iovs.08-2457. [DOI] [PubMed] [Google Scholar]
- Chauhan BC, Nicolela MT, Artes PH. Incidence and rates of visual field progression after longitudinally measured optic disc change in glaucoma. Ophthalmology. 2009;116 (11:2110–2118. doi: 10.1016/j.ophtha.2009.04.031. [DOI] [PubMed] [Google Scholar]
- Fayers T, Strouthidis NG, Garway-Heath DF. Monitoring glaucomatous progression using a novel Heidelberg Retina Tomograph event analysis. Ophthalmology. 2007;114 (11:1973–1980. doi: 10.1016/j.ophtha.2007.01.035. [DOI] [PubMed] [Google Scholar]
- See JL, Nicolela MT, Chauhan BC. Rates of neuroretinal rim and peripapillary atrophy area change: a comparative study of glaucoma patients and normal controls. Ophthalmology. 2009;116 (5:840–847. doi: 10.1016/j.ophtha.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Zangwill LM, Weinreb RN, Berry CC, Smith AR, Dirkes KA, Liebmann JM, et al. The confocal scanning laser ophthalmoscopy ancillary study to the ocular hypertension treatment study: study design and baseline factors. Am J Ophthalmol. 2004;137 (2:219–227. doi: 10.1016/j.ajo.2003.08.031. [DOI] [PubMed] [Google Scholar]
- Strouthidis NG, Gardiner SK, Sinapis C, Burgoyne CF, Garway-Heath DF. The spatial pattern of neuroretinal rim loss in ocular hypertension. Invest Ophthalmol Vis Sci. 2009;50 (8:3737–3742. doi: 10.1167/iovs.08-2844. [DOI] [PubMed] [Google Scholar]
- Poli A, Strouthidis NG, Ho TA, Garway-Heath DF. Analysis of HRT images: comparison of reference planes. Invest Ophthalmol Vis Sci. 2008;49 (9:3970–3975. doi: 10.1167/iovs.08-1764. [DOI] [PubMed] [Google Scholar]
- Topouzis F, Peng F, Kotas-Neumann R, Garcia R, Sanguinet J, Yu F, et al. Longitudinal changes in optic disc topography of adult patients after trabeculectomy. Ophthalmology. 1999;106 (6:1147–1151. doi: 10.1016/S0161-6420(99)90248-8. [DOI] [PubMed] [Google Scholar]
- Lesk MR, Spaeth GL, Azuara-Blanco A, Araujo SV, Katz LJ, Terebuh AK, et al. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology. 1999;106 (5:1013–1018. doi: 10.1016/S0161-6420(99)00526-6. [DOI] [PubMed] [Google Scholar]
- Bowd C, Balasubramanian M, Weinreb RN, Vizzeri G, Alencar LM, O'Leary N, et al. Performance of confocal scanning laser tomograph Topographic Change Analysis (TCA) for assessing glaucomatous progression. Invest Ophthalmol Vis Sci. 2009;50 (2:691–701. doi: 10.1167/iovs.08-2136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros FA, Weinreb RN.Visual field progression Ophthalmology 2010117(4851–852.author reply 852. [DOI] [PubMed] [Google Scholar]
- Strouthidis NG, Demirel S, Asaoka R, Cossio-Zuniga C, Garway-Heath DF. The Heidelberg retina tomograph Glaucoma Probability Score: reproducibility and measurement of progression. Ophthalmology. 2010;117 (4:724–729. doi: 10.1016/j.ophtha.2009.09.036. [DOI] [PubMed] [Google Scholar]
- DeLeon Ortega JE, Sakata LM, Kakati B, McGwin G, Jr, Monheit BE, Arthur SN, et al. Effect of glaucomatous damage on repeatability of confocal scanning laser ophthalmoscope, scanning laser polarimetry, and optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48 (3:1156–1163. doi: 10.1167/iovs.06-0921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson AJ, Garway-Heath DF, Strouthidis NG, Crabb DP. A new statistical approach for quantifying change in series of retinal and optic nerve head topography images. Invest Ophthalmol Vis Sci. 2005;46 (5:1659–1667. doi: 10.1167/iovs.04-0953. [DOI] [PubMed] [Google Scholar]
- O'Leary N, Crabb DP, Mansberger SL, Fortune B, Twa MD, Lloyd MJ, et al. Glaucomatous progression in series of stereoscopic photographs and Heidelberg retina tomograph images. Arch Ophthalmol. 2010;128 (5:560–568. doi: 10.1001/archophthalmol.2010.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knighton RW, Huang X, Zhou Q. Microtubule contribution to the reflectance of the retinal nerve fiber layer. Invest Ophthalmol Vis Sci. 1998;39 (1:189–193. [PubMed] [Google Scholar]
- Sommer A, Katz J, Quigley HA, Miller NR, Robin AL, Richter RC, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991;109 (1:77–83. doi: 10.1001/archopht.1991.01080010079037. [DOI] [PubMed] [Google Scholar]
- Weinreb RN, Zangwill L, Berry CC, Bathija R, Sample PA. Detection of glaucoma with scanning laser polarimetry. Arch Ophthalmol. 1998;116 (12:1583–1589. doi: 10.1001/archopht.116.12.1583. [DOI] [PubMed] [Google Scholar]
- Tjon-Fo-Sang MJ, Lemij HG. The sensitivity and specificity of nerve fiber layer measurements in glaucoma as determined with scanning laser polarimetry. Am J Ophthalmol. 1997;123 (1:62–69. doi: 10.1016/s0002-9394(14)70993-6. [DOI] [PubMed] [Google Scholar]
- Kogure S, Iijima H, Tsukahara S. A new parameter for assessing the thickness of the retinal nerve fiber layer for glaucoma diagnosis. Eur J Ophthalmol. 1999;9 (2:93–98. doi: 10.1177/112067219900900204. [DOI] [PubMed] [Google Scholar]
- Bowd C, Zangwill LM, Berry CC, Blumenthal EZ, Vasile C, Sanchez-Galeana C, et al. Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Invest Ophthalmol Vis Sci. 2001;42 (9:1993–2003. [PubMed] [Google Scholar]
- Fabre K, Michiels I, Zeyen T. The sensitivity and specificity of TOP, FDP and GDX in screening for early glaucoma. Bull Soc Belge Ophtalmol. 2000;275:17–23. [PubMed] [Google Scholar]
- Trible JR, Schultz RO, Robinson JC, Rothe TL. Accuracy of scanning laser polarimetry in the diagnosis of glaucoma. Arch Ophthalmol. 1999;117 (10:1298–1304. doi: 10.1001/archopht.117.10.1298. [DOI] [PubMed] [Google Scholar]
- Bowd C, Medeiros FA, Weinreb RN, Zangwill LM. The effect of atypical birefringence patterns on glaucoma detection using scanning laser polarimetry with variable corneal compensation. Invest Ophthalmol Vis Sci. 2007;48 (1:223–227. doi: 10.1167/iovs.06-0787. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Bowd C, Zangwill LM, Patel C, Weinreb RN. Detection of glaucoma using scanning laser polarimetry with enhanced corneal compensation. Invest Ophthalmol Vis Sci. 2007;48 (7:3146–3153. doi: 10.1167/iovs.06-1139. [DOI] [PubMed] [Google Scholar]
- Toth M, Hollo G. Enhanced corneal compensation for scanning laser polarimetry on eyes with atypical polarisation pattern. Br J Ophthalmol. 2005;89 (9:1139–1142. doi: 10.1136/bjo.2005.070011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Pozzo S, Iacono P, Marchesan R, Minutola D, Ravalico G. The effect of ageing on retinal nerve fibre layer thickness: an evaluation by scanning laser polarimetry with variable corneal compensation. Acta Ophthalmol Scand. 2006;84 (3:375–379. doi: 10.1111/j.1600-0420.2006.00655.x. [DOI] [PubMed] [Google Scholar]
- Grewal DS, Sehi M, Greenfield DS.Detecting glaucomatous progression using GDx with variable and enhanced corneal compensation using Guided Progression Analysis Br J Ophthalmol 2010. e-pub ahead of print 22 July 2010; doi: 10.1136/bjo.2010.180810 [DOI] [PubMed]
- Grewal DS, Sehi M, Greenfield DS.Comparing rates of retinal nerve fibre layer loss with GDxECC using different methods of visual-field progression Br J Ophthalmol 2010. e-pub ahead of print 9 September 2010; doi: 10.1136/bjo.2010.183483 [DOI] [PMC free article] [PubMed]
- Jonas JB, Fernandez MC, Sturmer J. Pattern of glaucomatous neuroretinal rim loss. Ophthalmology. 1993;100 (1:63–68. doi: 10.1016/s0161-6420(13)31694-7. [DOI] [PubMed] [Google Scholar]
- Wollstein G, Ishikawa H, Wang J, Beaton SA, Schuman JS. Comparison of three optical coherence tomography scanning areas for detection of glaucomatous damage. Am J Ophthalmol. 2005;139 (1:39–43. doi: 10.1016/j.ajo.2004.08.036. [DOI] [PubMed] [Google Scholar]
- Medeiros FA, Zangwill LM, Bowd C, Vessani RM, Susanna R, Jr, Weinreb RN. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol. 2005;139 (1:44–55. doi: 10.1016/j.ajo.2004.08.069. [DOI] [PubMed] [Google Scholar]
- Leung CK, Cheung CY, Weinreb RN, Qiu K, Liu S, Li H, et al. Evaluation of retinal nerve fiber layer progression in glaucoma: a study on optical coherence tomography guided progression analysis. Invest Ophthalmol Vis Sci. 2010;51 (1:217–222. doi: 10.1167/iovs.09-3468. [DOI] [PubMed] [Google Scholar]
- Vizzeri G, Bowd C, Medeiros FA, Weinreb RN, Zangwill LM. Effect of improper scan alignment on retinal nerve fiber layer thickness measurements using Stratus optical coherence tomograph. J Glaucoma. 2008;17 (5:341–349. doi: 10.1097/IJG.0b013e31815c3aeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung CY, Leung CK, Lin D, Pang CP, Lam DS.Relationship between retinal nerve fiber layer measurement and signal strength in optical coherence tomography Ophthalmology 2008115(81347–1351.1351, e1341–1342. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Garcia AO, Vizzeri G, Bowd C, Medeiros FA, Zangwill LM, Weinreb RN.Reproducibility of RTVue retinal nerve fiber layer thickness and optic disc measurements and agreement with Stratus optical coherence tomography measurements Am J Ophthalmol 2009147(61067–1074.1074, e1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojtkowski M, Srinivasan V, Fujimoto JG, Ko T, Schuman JS, Kowalczyk A, et al. Three-dimensional retinal imaging with high-speed ultrahigh-resolution optical coherence tomography. Ophthalmology. 2005;112 (10:1734–1746. doi: 10.1016/j.ophtha.2005.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao HL, Zangwill LM, Weinreb RN, Sample PA, Alencar LM, Medeiros FA. Comparison of Different Spectral Domain Optical Coherence Tomography Scanning Areas for Glaucoma Diagnosis. Ophthalmology. 2010;117 (9:1692–1699. doi: 10.1016/j.ophtha.2010.01.031. [DOI] [PubMed] [Google Scholar]
- Weinreb RN, Kaufman PL. The glaucoma research community and FDA look to the future: a report from the NEI/FDA CDER Glaucoma Clinical Trial Design and Endpoints Symposium. Invest Ophthalmol Vis Sci. 2009;50 (4:1497–1505. doi: 10.1167/iovs.08-2843. [DOI] [PubMed] [Google Scholar]
- Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma Arch Ophthalmol 2002120(6701–713.discussion 829–730. [DOI] [PubMed] [Google Scholar]
- Miglior S, Zeyen T, Pfeiffer N, Cunha-Vaz J, Torri V, Adamsons I. Results of the European Glaucoma Prevention Study. Ophthalmology. 2005;112 (3:366–375. doi: 10.1016/j.ophtha.2004.11.030. [DOI] [PubMed] [Google Scholar]
- Drance SM. The Collaborative Normal-Tension Glaucoma Study and some of its lessons. Can J Ophthalmol. 1999;34 (1:1–6. [PubMed] [Google Scholar]
- Katz J, Congdon N, Friedman DS. Methodological variations in estimating apparent progressive visual field loss in clinical trials of glaucoma treatment. Arch Ophthalmol. 1999;117 (9:1137–1142. doi: 10.1001/archopht.117.9.1137. [DOI] [PubMed] [Google Scholar]