Abstract
A link between circadian rhythm and metabolism has long been discussed. Circadian rhythm is controlled by positive and negative transcriptional and translational feedback loops composed of several clock genes. Among clock genes, the brain and muscle Arnt-like protein-1 (BMAL1) and circadian locomotor output cycles kaput (CLOCK) play important roles in the regulation of the positive rhythmic transcription. In addition to control of circadian rhythm, we have previously shown that BMAL1 regulates adipogenesis. In metabolic syndrome patients, the function of BMAL1 is dysregulated in visceral adipose tissue. In addition, analysis of SNPs has revealed that BMAL1 is associated with susceptibility to hypertension and type II diabetes. Furthermore, the significant roles of BMAL1 in pancreatic β cells proliferation and maturation were recently reported. These results suggest that BMAL1 regulates energy homeostasis. Therefore, in this study, we examined whether loss of BMAL1 function is capable of inducing metabolic syndrome. Deficient of the Bmal1 gene in mice resulted in elevation of the respiratory quotient value, indicating that BMAL1 is involved in the utilization of fat as an energy source. Indeed, lack of Bmal1 reduced the capacity of fat storage in adipose tissue, resulting in an increase in the levels of circulating fatty acids, including triglycerides, free fatty acids, and cholesterol. Elevation of the circulating fatty acids level induced the formation of ectopic fat in the liver and skeletal muscle in Bmal1 -/- mice. Interestingly, ectopic fat formation was not observed in tissue-specific (liver or skeletal muscle) Bmal1 -/- mice even under high fat diet feeding condition. Therefore, we were led to conclude that BMAL1 is a crucial factor in the regulation of energy homeostasis, and disorders of the functions of BMAL1 lead to the development of metabolic syndrome.
Introduction
In recent years, the metabolic syndrome has become increasingly prevalent with major public consequences. Various lifestyle changes compared with a few decades ago are suspected to be the cause of the rapid increase in the number of metabolic syndrome patients. These changes include excessive energy intake from lipid-based foods, late dinners, reduced sleeping time, lack of exercise, excessive stress, etc. In addition to these factors, there is accumulating epidemiological evidence that shift work increases the risk of metabolic syndrome [1]–[4]. Tenkanen et al. reported that, in Finland, when all shift workers were compared with all day workers, the relative risk for ischemic heart disease was 1.4-fold greater in the former after adjustment for lifestyle factors, blood pressure, and serum lipid levels [1]. Similarly, the Nurses' Health Study in the United States reported that the multivariate-adjusted relative risks for ischemic heart disease were 1.51-fold higher among women reporting 6 or more years of rotating night shifts, compared with women who had never done shift work [2]. Karlsson et al. reported that high triglycerides (TG) and low concentrations of high-density lipoprotein (HDL) cholesterol seem to cluster together more often in shift workers than in day workers [3]. A large-scale prospective cohort study in Japanese workers showed that, compared with day workers, rotating-shift workers had a significantly higher risk of death due to ischemic heart disease, whereas fixed-night work was not associated with ischemic heart disease or obesity [4].
The mechanism by which shift work increases metabolic syndrome onset risk is not clear, but it is speculated that shift work has an influence on the circadian rhythms of physiologic functions such as blood pressure, heart rate, and the secretion and excretion of hormones, etc. [5]–[11]. The machinery of circadian rhythm has been conserved throughout evolution. In the regulation of circadian rhythms, two transcription factors, the brain and muscle Arnt-like protein-1 (BMAL1; also referred to as MOP3 or Arnt3) and circadian locomotor output cycles kaput (CLOCK), play central roles [12]–[15]. BMAL1 and CLOCK form a heterodimer and drive transcription from E-box elements found in the promoters of circadian-responsive genes, including period (Per) 1 and cryptochrome (Cry). After translation of the Per and Cry proteins, the Per/Cry complex translocates to the nucleus, where it inhibits gene expression driven by BMAL1 and CLOCK [16]–[19].
In addition to its roles in the control of circadian rhythms, BMAL1 has been suggested to contribute to the regulation of metabolism for the following reasons. First, genome-wide profiling of BMAL1 targets revealed their strict relationship with metabolism [20]. Second, SNP analysis revealed that BMAL1 is associated with type II diabetes and hypertension [21]. In addition, BMAL1 is strongly induced during adipogenesis and regulates adipocyte functions [22]. BMAL1 activity is disturbed in the visceral adipose tissue of metabolic syndrome patients [23], [24]. A recent study revealed that BMAL1 and CLOCK play critical roles in proliferation and functions of pancreatic β cells [25]. In addition, Hemmeryckx et al. reported that lack of Bmal1 increases the arterial and venous thrombosis [26]. In regard to food intake, Bmal1-deficient (-/-) mice show robust food anticipatory activity [27]. Moreover, mice carrying mutation in the Clock gene are obese and develop a metabolic syndrome consisting of hyperleptinemia, hyperlipidemia, and hyperglycemia [28]. These results suggest that loss of functions of BMAL1 may lead to the development of metabolic syndrome.
We show here that global (whole body) Bmal1 -/- mice, derived from the embryonic stem (ES) cells of C57BL/6J mice, exhibited a metabolic syndrome-like onset, i.e., elevation of the level of circulating fatty acids, including TG, free fatty acids, and low-density lipoprotein (LDL)-cholesterol. In addition, ectopic fat formation was observed in the liver and skeletal muscle. The mechanism of these effects may involve loss of the functions of adipose tissue, since ectopic fat formation was not observed in tissue-specific (liver or skeletal muscle) Bmal1 -/- mice even under high fat diet feeding condition. Consequently, we are led to conclude that BMAL1 plays crucial roles in the control of energy homeostasis.
Results
Loss of the Bmal1 gene results in an increase of the respiratory quotient (RQ)
In this study, we first generated conditional Bmal1 (flox/flox) mice carrying the conditional Bmal1 allele containing exons 6 to 8 flanked by loxP sites (Fig. S1 and S2). Since genetic background-specific phenotypes were observed in Clock-mutant mice [28], [29], conditional Bmal1 (flox/flox) mice were obtained using ES cells derived from C57BL/6J mice, and the genetic background of the mice was maintained on C57BL/6J. These mice are useful to generate both global- and tissue-specific mice. In all experiments, littermate mice were used as a “control”. Similar to the Mop3 -/- mice established previously [14], the Bmal1 -/- mice exhibited loss of circadian rhythm in locomotor activity (Fig. S3). In contrast, locomotor activity of liver-specific (L-) Bmal1 -/- mice and skeletal muscle-specific Bmal1 -/- mice showed no significant differences with that of control mice (Fig. S3).
To characterize the metabolic activity of the Bmal1 -/- mice, in a first set of experiments, the respiratory quotient (RQ) was determined. Mice were housed in a chamber connected to indirect calorimeter under a light/dark (12 h/12 h) condition (LD) or constant darkness condition (DD). To obtain RQ, the amount of CO2 eliminated from the body and the amount of O2 consumed were measured. As shown in Fig. 1, the daily value of the RQ in the Bmal1 -/- mice was greater than that in control mice under both the LD condition and DD condition.
Figure 1. Abnormal respiration activity in Bmal1 -/- mice.
(A) The respiratory quotient (RQ) of male mice housed under the light/dark condition (LD) or constant darkness condition (DD) was determined by indirect calorimeter. The daily average of RQ corrected by body weight was calculated. Data represent the means ± SEM (n = 6 for each genotype). Asterisks indicate significant differences (P<0.05).
High-fat diet increases circulating fatty acids level and ectopic fat accumulation in Bmal1 -/- mice
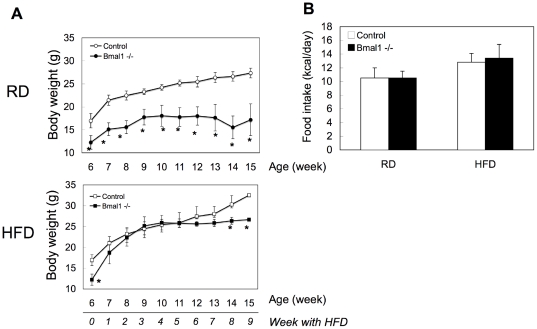
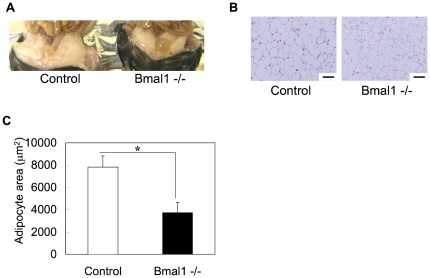
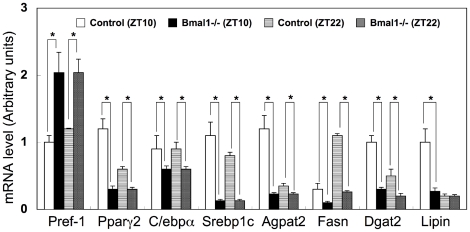
The higher RQ value in Bmal1 -/- mice compared with control mice suggested lower utilization of fat as an energy source in Bmal1 -/- mice (Fig. 1). To confirm this, Bmal1 -/- mice were subjected to a high-fat diet challenge. As reported previously [30], the body weight of Bmal1 -/- mice was lighter than that of control mice under a regular diet condition (Fig. 2A). Feeding with a high-fat diet induced body-weight gain in both control mice and Bmal1 -/- mice (Fig. 2A). However, while the body weight of control mice continuously increased during the challenge, that of Bmal1 -/- mice remained almost constant after 4 weeks of the challenge (Fig. 2A). There were no substantial differences in the calorie intake of control mice and Bmal1 -/- mice during the challenge (Fig. 2B). After 5 weeks of the high-fat diet challenge, the adipose tissue mass in Bmal1 -/- mice was smaller than that in control mice (Fig. 3A). Also, a histological study showed that the size of adipocytes in Bmal1 -/- mice was smaller than that in control mice (Fig. 3B and C). As summarized in Fig. 4 and Fig. S4, gene expression of adipogenesis-related transcription factors and a series of factors responsible for synthesis of TG and fatty acids were substantially decreased in adipose tissue in Bmal1 -/- mice. Furthermore, a significant decrease in the expression of factors involved in fat burning, such as Ucp3 and β3 adrenalin receptor, was observed in Bmal1 -/- mice (Fig. S4). In contrast, Pref-1, a specific marker gene for preadipocytes, was highly expressed in adipose tissue in Bmal1 -/- mice (Fig. 4).
Figure 2. Effects of a high-fat diet feeding on the body weight.
(A) Male control mice and Bmal1 -/- mice were subjected to a high-fat diet (HFD) challenge at 6 weeks of age. The body weights of the mice fed either a regular diet (RD) or HFD were determined. Data represent the means ± SEM (n = 8 for each genotype). Asterisks indicate significant differences (P<0.05). (B) The daily average of the calorie intake of male mice at 11 weeks of age (5 weeks with a HFD) was determined. Data represent the means ± SEM (n = 8 for each genotype and treatment).
Figure 3. Effects of a high-fat diet feeding on histology of adipocytes in Bmal1 -/- mice.
Adipose tissue was excised at zeitgeber time (ZT) 10. (A) Representative morphology of adipose tissue in control mice and Bmal1 -/- mice fed a HFD for 5 weeks. (B) Representative HE staining of epididymal white adipose tissue isolated from male control mice and Bmal1 -/- mice fed a HFD for 5 weeks. Scale bars indicate 100 µm. (C) Average cross-sectional area of individual adipocytes in control mice and Bmal1 -/- mice fed a HFD. Data represent the means ± SEM (n = 5 for each genotype). Asterisks indicate significant differences (P<0.05).
Figure 4. Comparison of gene expressions in adipose tissues.
Gene expressions in adipose tissues in control mice and Bmal1 -/- mice at ZT10 and 22 were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represents the means ± SEM (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
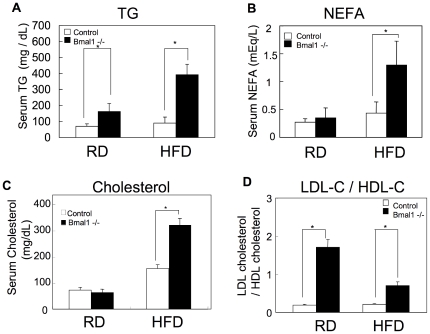
In the next set of experiments, several biochemical markers were determined. The level of serum TG in Bmal1 -/- mice was higher than that in control mice under the regular-diet feeding condition, and the difference was further pronounced in mice fed a high-fat diet (Fig. 5A). Also, the level of serum NEFA and cholesterol in Bmal1 -/- mice became higher than that in control mice by feeding a high-fat diet (Fig. 5B and C). Detailed profiling of the cholesterol content in the lipoprotein fractions revealed an increase of the cholesterol level in chylomicron (CM), very low density lipoprotein (VLDL), and low density lipoprotein (LDL) in Bmal1 -/- mice fed a regular diet (Table 1). Calculation of the TG/cholesterol molar ratio revealed a reduction in the relative content of TG in the lipoprotein complex in Bmal1 -/- mice (Table 2). The LDL cholesterol/HDL cholesterol ratio, a potent marker for risk of arteriosclerosis, in Bmal1 -/- mice was remarkably greater than that in control mice (Fig. 5D).
Figure 5. Alteration of circulating fatty acids level in Bmal1 -/- mice.
Serum samples were prepared from male mice fed a regular diet (RD) or a high-fat diet (HFD) for 5 weeks. All samples were collected at ZT 10. (A) Triglycerides (TG). (B) Non-esterified fatty acids (NEFA). (C) Total cholesterol. Data represent the means ± SEM (n = 8 for each genotype and treatment). Asterisks indicate significant differences (P<0.05). (D) The LDL cholesterol/HDL cholesterol ratio was calculated based on the data shown in Table 1. Data represent the means ± SEM (n = 8 for each genotype and treatment). Asterisks indicate significant differences (P<0.05).
Table 1. Content of cholesterol and triglycerides in lipoproteins.
| Cholesterol (mg/dL) | Triglyceride (mg/dL) | ||||||||
| CM | VLDL | LDL | HDL | CM | VLDL | LDL | HDL | ||
| RD | Control | 0.1±0.0 | 2.9±0.2 | 11.1±0.1 | 59.4±5.8 | 0.6±0.1 | 15.6±1.4 | 9.5±1.1 | 1.7±0.2 |
| Bmal1-/- | 0.3±0.0* | 7.3±0.8* | 20.5±0.3* | 35.2±4.8* | 4.6±0.5* | 19.4±2.1 | 12.7±1.4* | 2.3±0.2* | |
| HFD | Control | 0.2±0.0 | 5.7±0.6 | 25.9±3.8 | 123.2±20 | 3.5±0.4 | 18.8±1.9 | 6.5±0.7 | 1.8±0.1 |
| Bmal1-/- | 0.3±0.0 | 8.3±1.0* | 128.2±14* | 184.7±23* | 5.3±0.6* | 9.1±1.1* | 14.9±1.8* | 3.4±0.4* | |
Blood samples were collected at ZT 10. Plasma samples were prepared from male control mice and Bmal1 -/- mice fed either a regular diet (RD) or a high fat diet (HFD) for 5 weeks. Plasma lipoproteins were separated and analyzed by an on-line dual enzymatic method for simultaneous quantification of cholesterol and triglycerides by HPLC. Data represent the means ± SEM (n = 5 for each genotype). Asterisks indicate significant differences (P<0.05).
Table 2. Molar ratio of triglycerides/cholesterol.
| CM | VLDL | LDL | HDL | ||
| RD | Control | 2.60 | 2.36 | 0.38 | 0.01 |
| Bmal1-/- | 7.76 | 1.17 | 0.27 | 0.03 | |
| HFD | Control | 7.67 | 1.45 | 0.11 | 0.01 |
| Bmal1-/- | 7.74 | 0.48 | 0.05 | 0.01 |
Molar ratio was calculated from the data shown in Table 1. Molecular weights of 882.43 and 386.65 were used for triglycerides and cholesterol, respectively.
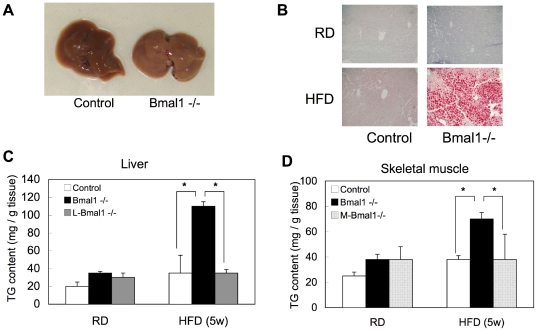
High fat diet feeding induced fatty liver in Bmal1 -/- mice but not in control mice (Fig. 6A and B). Quantification of tissue TG content revealed significant accumulation of TG in the liver and skeletal muscle in Bmal1 -/- mice (Fig. 6C and D). Interestingly, under both normal diet and high fat diet conditions, TG contents in the liver in liver-specific (L-) Bmal1 -/- mice and the skeletal muscle in skeletal muscle-specific (M-) Bmal1 -/- mice were almost equal to those in control mice (Fig. 6C and D).
Figure 6. Ectopic fat accumulation in liver and skeletal muscle in Bmal1 -/- mice.
All tissue samples were excised at ZT10. (A) Representative morphology of the livers from control mice and Bmal1 -/- mice fed a HFD for 5 weeks. (B) Representative oil red O staining of liver tissue samples isolated from male control mice and Bmal1 -/- mice fed either a RD or HFD for 5 weeks. (C and D) Triglyceride (TG) contents in the liver (C) and skeletal muscle (D) from male control mice and Bmal1 -/- mice fed a RD or HFD for 5 weeks. Data represent the means ± SEM (n = 8 for each genotype and treatment). Asterisks indicate significant differences (P<0.05).
Loss of the Bmal1 gene alters the expression level of metabolism-related genes
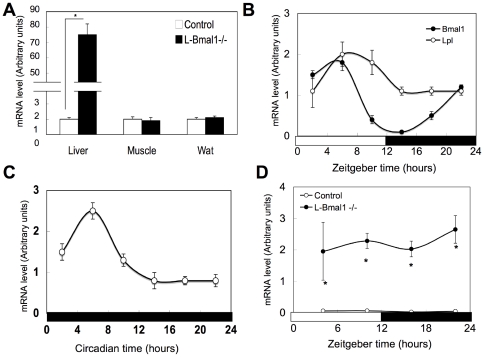
To gain insight into the ectopic fat accumulation in Bmal1 -/- mice, gene expression in the liver and muscle was compared to that in control mice by RT-qPCR. Changes in the expression of selected lipid metabolism-related genes are summarized in Table 3 and S1. In the Bmal1 -/- mice liver, a robust (∼78-fold) increase in Lpl expression was observed (Table 3). This increased expression of Lpl gene was also observed in the liver in L-Bmal1 -/- mice (Fig. 7A and D) and in the Bmal1 knockdown cultured hepatocytes prepared from control mice (Fig. S5). The expression pattern of Lpl showed clear circadian oscillations in the liver of control mice under both the LD and DD condition (Fig. 7B–D). The expression of genes involved in fatty acid binding and transport, namely Cd36, Fabp5, and Srbi, were induced in the Bmal1 -/- mice liver (Table 3). In the skeletal muscle, the expression of genes in the pathway for de novo fatty acid synthesis such as Fasn and Scd1, and Agpat3 were highly induced (Table 3). Conversely, Ldlr expression was significantly decreased in Bmal1 -/- skeletal muscle (Table 3). Expression of the Lpl gene in Bmal1 -/- skeletal muscle was not significantly different compared to that in control mice (Table 3). In both liver and muscle, expression of genes responsible for oxidation of fatty acids was decreased (Table 3).
Table 3. Gene expressions in Bmal1 -/- mice.
| Liver | Muscle | |||
| ZT10 | ZT22 | ZT10 | ZT22 | |
| Fatty acid binding and transpot | ||||
| Cd36 | 2.7±0.3* | 1.1±0.1 | 1.2±0.2 | 1.4±0.2 |
| Fabp5 | 4.3±0.4* | 1.5±0.1* | 1.1±0.1 | 0.9±0.2 |
| Ldlr | 0.8±0.3 | 1.0±0.2 | 0.2±0.1* | 0.2±0.2* |
| Lpl | 77.9±8.5* | 79.3±9.1* | 1.1±0.2 | 0.9±0.1 |
| Srbi | 2.7±0.3* | 1.5±0.1* | 0.7±0.3 | 1.1±0.2 |
| TG and fatty acid synthesis | ||||
| Agat2 | 0.8±0.8 | 0.6±0.3 | 1.1±0.1 | 1.3±0.2 |
| Agat3 | 1.0±0.2 | 1.1±0.1 | 2.0±0.2* | 1.8±0.2* |
| Dgat1 | 0.6±0.2* | 0.7±0.1 | 0.9±0.2 | 1.1±0.1 |
| Dgat2 | 0.5±0.1* | 0.5±0.1* | 0.6±0.2* | 0.4±0.2* |
| Fasn | 0.3±0.0* | 0.3±0.0* | 6.3±0.6* | 1.1±0.2 |
| Scd1 | 1.3±0.2 | 0.3±0.1* | 5.0±1.1* | 2.0±0.3* |
| Fatty acid oxidation | ||||
| Acaa 1a | 0.6±0.1* | 0.5±0.1* | 0.8±0.2 | 0.7±0.2 |
| Acaa 1b | 0.3±0.1* | 0.2±0.0* | 0.6±0.3 | 0.6±0.3 |
| Acadl | 1.7±0.2 | 0.7±0.2 | 1.6±0.2* | 0.9±0.2 |
| Acadm | 0.7±0.3 | 0.7±0.2 | 1.7±0.3* | 1.3±0.1 |
| Echdc1 | 0.6±0.1* | 0.5±0.1* | 1.3±0.3 | 0.9±0.1 |
Gene expressions in control mice and Bmal1 -/- mice were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Each value represented the mean fold-changes (± SEM) of Bmal1 -/- mice in comparison to control mice (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
Figure 7. Induction of Lpl gene expression in the liver by the deletion of Bmal1 gene.
(A) Tissue samples were excised form male control mice and L-Bmal1 -/- mice at ZT10. The total RNA was extracted from these tissues and the expression of Lpl mRNA was determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represent the mean ± SEM (n = 5 for each genotype). Asterisks indicate significant differences (P<0.05). Data represent the means ± SEM (n = 5 for each genotype and point). (B) The liver was excised male control mice at the indicated times. The open bar indicates the lights-on phase, and the dark bar indicates lights-off. The total RNA was extracted, and the expression of Bmal1 and Lpl mRNA was determined as described in (A). Data represent the means ± SEM (n = 5 for each point). (C) The liver was excised from the control mice housed in constant darkness for 10 days. The expression of Lpl mRNA was determined as described in (A). Data represent the means ± SEM (n = 5 for each point). (D) The liver was excised male control mice and L-Bmal1 -/- mice at the indicated times. The open bar indicates the lights-on phase, and the dark bar indicates lights-off. The total RNA was extracted, and the expression of Lpl mRNA was determined as described in (A). Data represent the means ± SEM (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
Discussion
A link between circadian rhythm and metabolism has long been discussed [31], [32]. Therefore, in this study, we aimed to study whether loss of BMAL1 functions induces metabolic syndrome. Deletion of the Bmal1 gene resulted in an elevation of the daily average value of the RQ under both the LD and DD conditions (Fig. 1). An increase in the RQ represents oxidation of carbohydrates, and a decrease of the value represents oxidation of fatty acids. Thus, the elevation of RQ in Bmal1 -/- mice indicates that BMAL1 is involved in the utilization of fat as an energy source. Indeed, under the high-fat diet challenge, the levels of circulating fatty acids, including TG, NEFA and cholesterol, in Bmal1 -/- mice were remarkably increased (Fig. 5A–C). Elevation of circulating fatty acids induced ectopic fat accumulation in the liver and muscle (Fig. 6A–D). A detailed profile analysis of the cholesterol contents in lipoprotein fractions revealed that the ratio of LDL cholesterol to HDL cholesterol, a potent marker for risk of arteriosclerosis, in Bmal1 -/- mice was significantly higher than that in control mice even under a regular-diet condition (Fig. 5D). Furthermore, Hemmeryckx et al. recently reported endothelial dysfunction and progression of the prothrombotic state in Bmal1 -/- mice [26]. Consequently, we were led to conclude that the loss of the Bmal1 gene induced metabolic syndrome.
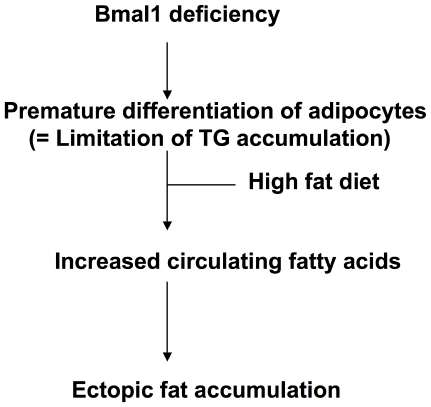
Ectopic fat formation by high fat feeding was not observed in L-Bma1 -/- mice and M-Bmal1 -/- mice, suggesting that elevation of the level of circulating fatty acids level was a main cause of ectopic fat formation in the tissues. As described above, the RQ value in Bmal1 -/- mice is higher than that in control mice (Fig. 1). Also, excess secretion of an oily, waxy substance (sebum) was observed in Bmal1 -/- mice fed a high-fat diet (Fig. S6). These results suggest that the ability to utilize and store fat in Bmal1 -/- mice is inferior to that in control mice. Excess fatty acids are largely deposited in the adipose tissue. Histological analysis showed that the size of adipocytes in Bmal1 -/- mice fed a high-fat diet was significantly smaller than that in control mice (Fig. 3A–C). Since expression of Ucp3 and β3 adrenalin receptor was down-regulated in the Bmal1 -/- mice, excess of fatty acid oxidation was unlikely the cause of decrease of adipocyte size (Fig. S4). As we previously demonstrated, BMAL1 plays central roles in the regulation of high fat diet-induced adipogenesis [22]. Indeed, the expression level of the Pref-1 gene, a marker for preadipocytes, in Bmal1 -/- mice adipose tissue was greater than that in control mice (Fig. 4). In contrast, the genes preferentially expressed in mature adipocytes, such as Pparγ2, C/ebpα, and Srebp1c, were expressed at lower levels in Bmal1 -/- mice (Fig. 4). Furthermore, the expressions of Agpat 2 and lipin were significantly reduced in Bmal1 -/- mice adipose tissue (Fig. 4). Mutations in Agpat 2 and lipin cause congenital generalized lipodystrophy [33], [34]. As has been demonstrated in lipodystrophy, the failure of adipose tissue mass to expand and accommodate a high-energy influx causes accumulation of ectopic fat [35], [36]. Therefore, we are led to conclude that an increase of the circulating fatty acids level followed by the ectopic fat accumulation in the Bmal1 -/- mice was mainly due to the insufficient function of adipose tissue resulting from lower adipogenesis activity (Fig. 8).
Figure 8. A schematic diagram of Bmal1 deficiency-induced abnormal lipid metabolism.
Although both Bmal1 -/- mice and Clock mutant mice develop metabolic syndrome-like symptoms, Bmal1 -/- mice are thin and Clock mutant mice are obese (28, 29, this study). As mentioned above, metabolic disorder in Bmal1 -/- mice was induced as a result of lower adipogenesis activity, as observed in lipodystrophy. On the other hand, Clock mutant mice develop metabolic syndrome-like symptoms presumably as a result of obesity. In Clock mutant mice, expression level of Bmal1 is significantly increased [37]. Therefore, one possibility is that BMAL1 overexpressed alone or in cooperation with other genes, such as Npas2, promotes adipogenesis. Alternatively, BMAL1/mutated CLOCK complex may act as a dominant negative factor and affect several gene expression involved in regulation of lipid metabolism.
Recently, Marcheva et al. reported that BMAL1 and CLOCK play roles in the regulation of pancreas functions, including the proliferation of islets and secretion of insulin in response to glucose [25]. Impaired insulin secretion and glucose intolerance in Bmal1-/- mice were also observed in this study, as summarized in Text S1, Fig. S7 and S8. Therefore, one can speculate that the elevation of circulating fatty acids is partly due to impaired insulin secretion in Bmal1 -/- mice. Under the condition of the impaired insulin actions, phosphorylation of Ser residues at 563 and 660 in hormone sensitive lipase (HSL) in adipose tissue is accelerated, resulting in increase of lipolysis [38]. In Bmal1-/- mice, despite the lower insulin secretion, the phosphorylation status of Ser563 and 660 was substantially lower than that in control mice (Fig. S9). Therefore, although we do not exclude the possibility that, in Bmal1 -/- mice, impaired insulin secretion is partly responsible for development of dyslipidemia, its contribution via acceleration of lipolysis is relatively smaller.
Lack of Bmal1 induced a robust induction of Lpl expression in the liver (Table 3). A detailed analysis of the lipoprotein complex revealed that VLDL and LDL in Bmal1 -/- mice were relatively TG poor (Table 2), suggesting that LPL activity is substantially increased in Bmal1 -/- mice. This strong induction of Lpl gene expression was observed in the liver of L-Bmal1 -/- mice, but not in other tissues, and Bmal1-knockdown cultured hepatocytes (Fig. 7A and D, Table 3, and Fig. S5). These results indicate that overexpression of the hepatic Lpl gene was mainly due to the lack of BMAL1 functions in the liver. Previous studies using liver-specific Lpl transgenic mice demonstrated that overexpression of the Lpl gene resulted in accumulation of TG in the liver even under a regular-diet condition [39]. Loss of the Bmal1 gene also induced Cd36, Fabbp5, and Srbi in the liver (Table 3). Consequently, ectopic fat formation in the liver may be induced by increased fatty acid transport under the condition of elevated levels of circulating fatty acids.
Overall, this study showed that BMAL1 activity is closely associated with lipid metabolism. It is known that several factors regulating metabolic activity affect Bmal1 functions. One of the well-characterized examples is the redox state of NAD [40]. The reduced forms of the redox cofactors, NAD (H) and NADP (H), strongly enhanced DNA binding of the BMAL1/CLOCK, whereas the oxidized forms inhibited it [40]. Not only is NAD important in cellular redox reactions and the DNA-binding activity of BMAL1/CLOCK, as described above, but it also serves as a substrate for sirtuin (SIRT) 1, an NAD-dependent and nutrient-responsive deacetylase [41], [42]. SIRT1 activated with NAD reduces the acetylation status of BMAL1, resulting in the suppression of BMAL1/CLOCK activity [43]. In diabetic rats lacking insulin, the phase of the circadian gene expression in the heart is advanced, suggesting that high blood glucose levels can phase-shift the clock in peripheral tissues [44]. It has been shown that ethanol consumption alters the circadian expression pattern of Per genes [45]. Although it is unknown how ethanol affects the circadian clock, it may be possible that NADH generated by alcohol metabolism affects the activity of BMAL1/CLOCK.
In conclusion, the results in this study revealed that loss of the functions of BMAL1 leads to the development of ectopic fat formation and dyslipidemia. Therefore, the present results may provide an excellent opportunity to gain new insights into the regulation of energy homeostasis by BMAL1.
Materials and Methods
Animals
Conditional Bmal1 (flox/flox) mice, which carry the conditional Bmal1 allele containing exons 6 to 8 flanked by loxP sites, were generated using ES cells derived from C57BL/6J mice. Splicing of exons 6 to 8 should cause a deletion of the bHLH domain and a frameshift mutation with the introduction of an early stop codon (TGA). Global (whole body) Bmal1 deficient (-/-) mice were generated by breeding of Bmal1 (flox/flox) mice with knockin C57BL/6J mice carrying the Cre recombinase gene driven by a PGK promoter (Ozgene, Perth, Australia). Genotyping for exons 6–8 was performed by PCR on DNA isolated from tail biopsies by using the forward primer A (5′- GGGGATTTCCATCTGTGTTTAC-3′) and primer B (5′- CTCATCTGCTTATCTGCTCTGGGG -3′). The Bmal1-excised allele amplified a 280-bp band, whereas amplification from the Bmal1-unexcised allele resulted in a 2500-bp band. Analysis of the excision of exon 8 was carried out by PCR using primer C (5′-CCTGGAACTCACTTTGTAGACC-3′) and primer D (5′- AACAGCCATCCTTAGCACG-3′). A 250-bp band confirmed the presence of a gene corresponding to exon 8. To obtain mice harboring liver or skeletal muscle with excision at Bmal1, mice expressing the Bmal1 (flox/flox) allele were crossed to mice expressing a Cre transgene driven by either the albumin (Alb) or the muscle creatine kinase (Mck) promoter (Jackson Laboratories, Bar Harbor, ME). Mice homozygous for the floxed allele and hemizygous for the Cre transgene (Bmal1 (flox/flox/CreAlb) or Bmal1 (flox/flox/CreMck)) were obtained by crossing Bmal1 (flox/+/CreAlb) or Bmal1 (flox/+/CreMck) mice to Bmal1 (flox/flox) mice. Littermates that were negative for the Cre transgenes (Bmal1 (flox/flox)) were used as experimental controls. All mice were maintained at 23±1°C with 50±10% relative humidity under a 12 h light/12 h dark cycle (light: zeitgeber time (ZT) 0–12; dark; ZT12-24). For the experiments under constant darkness (DD), mice were entrained to DD condition for 7 days. All procedures during the dark period were conducted using infrared vision and dim red lighting. Food and water were available ad libitum. The high-fat diet consisted of 58% lard (wt/wt), 30% fish powder, 10% skim milk, and a 2% vitamin and mineral mixture (equivalent to 7.5% carbohydrate, 24.5% protein, and 60% fat) (OYC, Tokyo, Japan). The regular diet proportions were 54% carbohydrate, 20% protein, and 4.5% fat (OYC). The experimental protocol was approved by the Ethics Review Committee for Animal Experimentation of Nihon University (Permit number:AP10P006).
Metabolic studies
Locomotor activity was measured by using an infrared passive sensor system (Muromachi, Tokyo, Japan). Energy expenditure was measured by an indirect calorimeter (Muromachi). For oral glucose tolerance testing (OGTT), dextrose solution (2 g/kg body weight) was administered by oral gavage. Glucose levels were monitored before and at 15, 30, 60, and 120 min postgavage using blood glucose strips (Arkray, Kyoto, Japan). Plasma insulin levels during OGTT were measured by enzyme-linked immunosorbent assay (MIoBS, Yokohama, Japan). Insulin tolerance tests were performed by injecting 0.5 U insulin (Eli Lilly, Indianapolis, IN)/kg body weight intraperitoneally, followed by blood collection at 0, 30, 60, 120, and 180 min after injection. Blood glucose values were determined as described above.
Biochemical analysis of blood and tissue
Plasma lipoproteins were analyzed by an on-line dual enzymatic method for simultaneous quantification of cholesterol and triglycerides by HPLC at Skylight Biotech Inc. (Akita, Japan) according to the procedure described by Usui et al. [46]. The levels of serum TG, non-esterified fatty acid (NEFA), and total cholesterol were determined using a commercially available reagent (Wako, Tokyo, Japan). Hepatic and muscular lipids were extracted according to the methods of Folch et al. [47]. The extract was dissolved in 2-propanol and subsequently analyzed for TG as described above.
Analysis of gene expression
Total RNA was extracted using TRIzol reagent (Invitrogen, Carlsbad, CA) according to the manufacturer's instructions. To perform RT-qPCR, total RNA (1 µg) was reverse-transcribed using oligo dT primers. A portion of the cDNA (corresponding to 0.04 µg of total RNA) was amplified on an MX3000P real-time PCR system (Stratagene, La Jolla, CA) using Platinum SYBR Green qPCR SuperMix-UDG (Invitrogen). Information on the sequences of primers is available upon request. Standard curves (R2>0.99) were generated using a serial dilution of cDNA, and expression of all genes was normalized to the 36B4 level.
Supporting Information
Schematic diagram of the targeting construct and the resulting mutant allele. Dotted lines represent the fragment sizes generated by PCR genotyping of control and mutant alleles.
(TIF)
Genotyping of Bmal1 -/- mice. PCR genotyping of tail biopsies showing bands of 2500 bp and 280 bp indicating the presence of the control and mutant alleles, respectively (Top). The absence of 250 bp indicates deletion of exon 8 (bottom).
(TIF)
Representative activity records of individual control mice and Bmal1 -/- mice. Animals were individually housed under a light–dark (LD) cycle or constant darkness (DD). The activity was measured by using an infrared passive sensor system (Muromachi, Tokyo, Japan).
(TIF)
Comparison of gene expressions in adipose tissues. Gene expressions in adipose tissues in control mice and Bmal1 -/- mice at ZT10 and 22 were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represents the means ± SEM (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(TIF)
Expression of Lpl mRNA in Bmal1 -knockdown cultured hepatocytes. Primary hepatocytes were prepared from control mice and treated with siRNA solution (control and Bmal1, final concentration 100 nM each) for 48 h. The total RNA was extracted from these cells, and the gene expression was determined as described in Fig. 7A (n = 4 for each treatment).
(TIF)
Representative images of control mice and Bmal1 -/- mice fed a high-fat diet. Control mice and Bmal1 -/- mice were subjected to high-fat diet challenge for 3 days. Excess sebum was observed only in Bmal1 -/- mice.
(TIF)
Impaired insulin in Bmal1 -/- mice. All experiments were performed at ZT10. (A, B) Male control mice and Bmal1 -/- mice were fasted for 16 h. After oral glucose administration (2 g/kg), the levels of blood glucose (A) and plasma insulin (B) were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (C) Male control mice and Bmal1 -/- mice were fasted for 6 h. After i. p. injection of insulin (0.5 U/kg), blood glucose levels were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (D) Blood glucose levels in male control mice and Bmal1 -/- mice fed ad libitum or fasted for 16 h are shown. Data represent the means ± SEM (n = 8 for each genotype and treatment). (E) The pancreas was isolated from male control mice and Bmal1 -/- mice. Insulin contents in the tissues were determined by ELISA. The values were corrected by the amount of protein in the tissue. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (F) Response of male control mice and Bmal1 -/- mice to i.p. injection of glibenclamide (2.5 mg/kg). Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (G) Representative morphology of islets stained with anti-insulin antibody. Scale bars indicate 100 µm. (H) The average cross-sectional area of the islets in Bmal1 -/- mice was compared with that in control mice. Data represent the means ± SEM (n = 4 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(TIF)
Lowered gluconeogenesis activity in the Bmal1 -/- mice liver. All experiments were performed at ZT10. (A) Male control mice and Bmal1 -/- mice were fasted for 16 h. After i.p. injection of pyruvate (2 g/kg), blood glucose levels were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). Gene expression levels in the liver of male control and Bmal1 -/- mice were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represent the means ± SEM (n = 5 for each genotype). Asterisks indicate significant differences (P<0.05). Levels of G6P and AMP in the liver in male control and Bmal1 -/- mice were determined by capillary electrophoresis time-of-flight mass spectrometry. Data represent the means ± SEM (n = 4 for each genotype). Asterisks indicate significant differences (P<0.05).
(TIF)
Phosphorylation status of HSL in Bmal1 -/- mice adipose tissue. Total HSL protein level and phosphorylated form of HSL protein in the adipose tissue isolated from male control mice and Bmal1 -/- mice at ZT10 were determined by Western blot.
(TIF)
Gene expressions in Bmal1 -/- mice. Gene expressions in control mice and Bmal1 -/- mice were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4level. N.D. not determined. Each value represented the mean fold-changes (± SEM) of Bmal1 -/- mice in comparison to control mice (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(DOC)
Impaired glucose deposition and acceleration of gluconeogenesis in Bmal1 -/- mice.
(DOC)
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported in part by a grant from the Ministry of Education, Sciences, Sports, and Culture of Japan (to S.S.); a General Individual Research grant from Nihon University (to S.S.); an Interdisciplinary General Joint Research grant from Nihon University (to S.S.); and the “High-Tech Research Center” Project for Private Universities, a matching fund subsidy from the Ministry of Education, Culture, Sports, Science, and Technology 2007. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tenkane L, Sjöblom T, Kalimo R, Alikoski T, Härmä M. Shift work, occupation and coronary heart disease over 6 years of follow-up in the Helsinki Heart Study. Scand J Work Environ Health. 1977;23:257–265. doi: 10.5271/sjweh.218. [DOI] [PubMed] [Google Scholar]
- 2.Kawachi I, Colditz GA, Stampfer MJ, Willett WC, Manson JE, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92:3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- 3.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujino Y, Iso H, Tamakoshi A, Inaba Y, Koizumi A, et al. A prospective cohort study of shift work and risk of ischemic heart disease in Japanese male workers. Am J Epidemiol. 2006;164:128–135. doi: 10.1093/aje/kwj185. [DOI] [PubMed] [Google Scholar]
- 5.Theorell T, Akerstedt T. Day and night work: changes in cholesterol, uric acid, glucose and potassium in serum and in circadian patterns of urinary catecholamine excretion. A longitudinal cross-over study of railway workers. Acta Med Scand. 1976;200:47–53. doi: 10.1111/j.0954-6820.1976.tb08194.x. [DOI] [PubMed] [Google Scholar]
- 6.van Amelsvoort LG, Schouten EG, Maan AC, Swenne CA, Kok FJ. Changes in frequency of premature complexes and heart rate variability related to shift work. Occup Environ Med. 2001;58:678–681. doi: 10.1136/oem.58.10.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fujiwara S, Shinkai S, Kurokawa Y, Watanabe T. The acute effects of experimental short-term evening and night shifts on human circadian rhythm: the oral temperature, heart rate, serum cortisol and urinary catecholamines levels. Int Arch Occup Environ Health. 1992;63:409–418. doi: 10.1007/BF00386937. [DOI] [PubMed] [Google Scholar]
- 8.Orth-Gomer K. Intervention on coronary risk factors by adapting a shift work schedule to biologic rhythmicity. Psychosom Med. 1983;45:407–415. doi: 10.1097/00006842-198310000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Vokac Z, Gundersen N, Magnus P, Jebens E, Bakka T. Circadian rhythmicity of the urinary excretion of mercury, potassium and catecholamines in unconventional shift-work systems. Scand J Work Environ Health. 1980;6:188–196. doi: 10.5271/sjweh.2617. [DOI] [PubMed] [Google Scholar]
- 10.Waldhauser F, Vierhapper H, Pirich K. Abnormal circadian melatonin secretion in night-shift workers. N Engl J Med. 1986;315:1614. [PubMed] [Google Scholar]
- 11.Yamasaki F, Schwartz JE, Gerber LM, Warren K, Pickering TG. Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. Hypertension. 1998;32:417–423. doi: 10.1161/01.hyp.32.3.417. [DOI] [PubMed] [Google Scholar]
- 12.Hogenesch JB, Gu YZ, Jain S, Bradfield CA. The basic-helix-loop-helix-PAS orphan MOP3 forms transcriptionally active complexes with circadian and hypoxia factors. Proc Natl Acad Sci USA. 1998;95:5474–5479. doi: 10.1073/pnas.95.10.5474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takahata S, Sogawa K, Kobayashi A, Ema M, Mimura J, et al. Transcriptionally active heterodimer formation of an Arnt-like PAS protein, Arnt3, with HIF-1a, HLF, and clock. Biochem Biophys Res Commun. 1988;248:789–794. doi: 10.1006/bbrc.1998.9012. [DOI] [PubMed] [Google Scholar]
- 14.Bunger MK, Wilsbacher LD, Moran SM, Clendenin C, Radcliffe LA, et al. Mop3 is an essential component of the master circadian pacemaker in mammals. Cell. 2000;103:1009–1017. doi: 10.1016/s0092-8674(00)00205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vitaterna MH, King DP, Chang AM, Kornhauser JM, Lowrey PL, et al. Mutagenesis and mapping of a mouse gene, Clock, essential for circadian behavior. Science. 1994;264:719–725. doi: 10.1126/science.8171325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunlap JC. Molecular bases for circadian clocks. Cell. 1999;96:271–290. doi: 10.1016/s0092-8674(00)80566-8. [DOI] [PubMed] [Google Scholar]
- 17.Young MW, Kay SA. Time zones: a comparative genetics of circadian clocks. Nat Rev Genet. 2001;2:702–715. doi: 10.1038/35088576. [DOI] [PubMed] [Google Scholar]
- 18.Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature. 2002;418:935–941. doi: 10.1038/nature00965. [DOI] [PubMed] [Google Scholar]
- 19.Lowrey PL, Takahashi JS. Mammalian circadian biology: elucidating genome-wide levels of temporal organization. Annu Rev Genomics Hum Genet. 2004;5:407–441. doi: 10.1146/annurev.genom.5.061903.175925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatanaka F, Matsubara C, Myung J, Yoritaka T, Kamimura N, et al. Genome-wide profiling of the core clock protein BMAL1 targets reveals a strict relationship with metabolism. Mol Cell Biol. 2010;30:5636–48. doi: 10.1128/MCB.00781-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woon PY, Kaisaki PJ, Bragança J, Bihoreau MT, Levy JC, et al. Aryl hydrocarbon receptor nuclear translocator-like (BMAL1) is associated with susceptibility to hypertension and type 2 diabetes. Proc Natl Acad Sci U S A. 2007;104:14412–14417. doi: 10.1073/pnas.0703247104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimba S, Ishii N, Ohta Y, Ohno T, Watabe Y, et al. Brain and muscle Arnt-like protein-1 (BMAL1), a component of the molecular clock, regulates adipogenesis. Proc Natl Acad Sci USA. 2005;102:12071–12076. doi: 10.1073/pnas.0502383102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gómez-Abellán P, Hernández-Morante JJ, Luján JA, Madrid JA, Garaulet M. Clock genes are implicated in the human metabolic syndrome. Int J Obes. 2008;32:121–128. doi: 10.1038/sj.ijo.0803689. [DOI] [PubMed] [Google Scholar]
- 24.Gómez-Santos C, Gómez-Abellán P, Madrid JA, Hernández-Morante JJ, Lujan JA, et al. Circadian rhythm of clock genes in human adipose explants. Obesity. 2009;17:1481–1485. doi: 10.1038/oby.2009.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature. 2010;466:627–631. doi: 10.1038/nature09253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hemmeryckx B, Van Hove CE, Fransen P, Emmerechts J, Kauskot A, et al. Progression of the Prothrombotic State in Aging Bmal1-Deficient Mice. Arterioscler Thromb Vasc Biol. In press. 2011 doi: 10.1161/ATVBAHA.111.229062. [DOI] [PubMed] [Google Scholar]
- 27.Pendergast JS, Nakamura W, Friday RC, Hatanaka F, Takumi T, et al. Robust food anticipatory activity in BMAL1-deficient mice. PLoS One. 2009;4:e4860. doi: 10.1371/journal.pone.0004860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 308:1043–1045. doi: 10.1126/science.1108750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oishi K, Atsumi G, Sugiyama S, Kodomari I, Kasamatsu M, et al. Disrupted fat absorption attenuates obesity induced by a high-fat diet in Clock mutant mice. FEBS Lett. 2006;580:127–130. doi: 10.1016/j.febslet.2005.11.063. [DOI] [PubMed] [Google Scholar]
- 30.Kondratov RV, Kondratova AA, Gorbacheva VY, Vykhovanets OV, Antoch MP. Early aging and age-related pathologies in mice deficient in BMAL1, the core component of the circadian clock. Genes Dev. 2006;20:1868–1873. doi: 10.1101/gad.1432206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kovac J, Husse J, Oster H. A time to fast, a time to feast: the crosstalk between metabolism and the circadian clock. Mol Cells. 2009;28:75–80. doi: 10.1007/s10059-009-0113-0. [DOI] [PubMed] [Google Scholar]
- 32.Maury E, Ramsey KM, Bass J. Circadian rhythms and metabolic syndrome: from experimental genetics to human disease. Circ Res. 2010;106:447–462. doi: 10.1161/CIRCRESAHA.109.208355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agarwal AK, Arioglu E, De Almeida S, Akkoc N, Taylor SI, et al. AGPAT2 is mutated in congenital generalized lipodystrophy linked to chromosome 9q34. Nat Genet. 2002;31:21–23. doi: 10.1038/ng880. [DOI] [PubMed] [Google Scholar]
- 34.Péterfy M, Phan J, Xu P, Reue K. Lipodystrophy in the fld mouse results from mutation of a new gene encoding a nuclear protein, lipin. Nat Genet. 2001;27:121–124. doi: 10.1038/83685. [DOI] [PubMed] [Google Scholar]
- 35.Robbins DC, Danforth E, Jr, Horton ES, Burse RL, Goldman RF, et al. The effect of diet on thermogenesis in acquired lipodystrophy. Metabolism. 1979;28:908–916. doi: 10.1016/0026-0495(79)90090-8. [DOI] [PubMed] [Google Scholar]
- 36.Robbins DC, Horton ES, Tulp O, Sims EA. Familial partial lipodystrophy: complications of obesity in the non-obese? Metabolism. 1982;31:445–452. doi: 10.1016/0026-0495(82)90232-3. [DOI] [PubMed] [Google Scholar]
- 37.Oishi K, Fukui H, Norio Ishida N. Rhythmic expression of BMAL1 mRNA is altered in Clock mutant mice. Biochem Biophys Res Commun. 2000;268:164–167. doi: 10.1006/bbrc.1999.2054. [DOI] [PubMed] [Google Scholar]
- 38.Yeaman SJ. Hormone-sensitive lipase-new roles for an old enzyme. Biochem J. 2004;379:11–22. doi: 10.1042/BJ20031811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim JK, Fillmore JJ, Chen Y, Yu C, Moore IK, et al. Tissue-specific overexpression of lipoprotein lipase causes tissue-specific insulin resistance. Proc Natl Acad Sci USA. 2001;98:7522–7527. doi: 10.1073/pnas.121164498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rutter J, Reick M, Wu LC, McKnight SL. Regulation of clock and NPAS2 DNA binding by the redox state of NAD cofactors. Science. 2001;293:510–514. doi: 10.1126/science.1060698. [DOI] [PubMed] [Google Scholar]
- 41.Blander G, Guarente L. The Sir2 family of protein deacetylases. Annu Rev Biochem. 2004;73:417–435. doi: 10.1146/annurev.biochem.73.011303.073651. [DOI] [PubMed] [Google Scholar]
- 42.Dali-Youcef N, Lagouge M, Froelich S, Koehl C, Schoonjans K, et al. Sirtuins The ‘magnificent seven’, function, metabolism and longevity. Ann Med. 2007;39:335–345. doi: 10.1080/07853890701408194. [DOI] [PubMed] [Google Scholar]
- 43.Nakahata Y, Kaluzova M, Grimaldi B, Sahar S, Hirayama J, et al. The NAD+-dependent deacetylase SIRT1 modulates CLOCK-mediated chromatin remodeling and circadian control. Cell. 2008;134:329–340. doi: 10.1016/j.cell.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Young ME, Wilson CR, Razeghi P, Guthrie PH, Taegtmeyer H. Alterations of the circadian clock in the heart by streptozotocin-induced diabetes. J Mol Cell Cardiol. 2002;34:223–231. doi: 10.1006/jmcc.2001.1504. [DOI] [PubMed] [Google Scholar]
- 45.Chen CP, Kuhn P, Advis JP, Sarkar DK. Chronic ethanol consumption impairs the circadian rhythm of pro-opiomelanocortin and period genes mRNA expression in the hypothalamus of the male rat. J Neurochem. 2004;88:1547–1554. doi: 10.1046/j.1471-4159.2003.02300.x. [DOI] [PubMed] [Google Scholar]
- 46.Usui S, Hara Y, Hosaki S, Okazaki MJ. A new on-line dual enzymatic method for simultaneous quantification of cholesterol and triglycerides in lipoproteins by HPLC. J Lipid Res. 2002;43:805–814. [PubMed] [Google Scholar]
- 47.Folch J, Lees M, Sloane-Stanley GH. A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem. 1957;226:497–509. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Schematic diagram of the targeting construct and the resulting mutant allele. Dotted lines represent the fragment sizes generated by PCR genotyping of control and mutant alleles.
(TIF)
Genotyping of Bmal1 -/- mice. PCR genotyping of tail biopsies showing bands of 2500 bp and 280 bp indicating the presence of the control and mutant alleles, respectively (Top). The absence of 250 bp indicates deletion of exon 8 (bottom).
(TIF)
Representative activity records of individual control mice and Bmal1 -/- mice. Animals were individually housed under a light–dark (LD) cycle or constant darkness (DD). The activity was measured by using an infrared passive sensor system (Muromachi, Tokyo, Japan).
(TIF)
Comparison of gene expressions in adipose tissues. Gene expressions in adipose tissues in control mice and Bmal1 -/- mice at ZT10 and 22 were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represents the means ± SEM (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(TIF)
Expression of Lpl mRNA in Bmal1 -knockdown cultured hepatocytes. Primary hepatocytes were prepared from control mice and treated with siRNA solution (control and Bmal1, final concentration 100 nM each) for 48 h. The total RNA was extracted from these cells, and the gene expression was determined as described in Fig. 7A (n = 4 for each treatment).
(TIF)
Representative images of control mice and Bmal1 -/- mice fed a high-fat diet. Control mice and Bmal1 -/- mice were subjected to high-fat diet challenge for 3 days. Excess sebum was observed only in Bmal1 -/- mice.
(TIF)
Impaired insulin in Bmal1 -/- mice. All experiments were performed at ZT10. (A, B) Male control mice and Bmal1 -/- mice were fasted for 16 h. After oral glucose administration (2 g/kg), the levels of blood glucose (A) and plasma insulin (B) were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (C) Male control mice and Bmal1 -/- mice were fasted for 6 h. After i. p. injection of insulin (0.5 U/kg), blood glucose levels were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (D) Blood glucose levels in male control mice and Bmal1 -/- mice fed ad libitum or fasted for 16 h are shown. Data represent the means ± SEM (n = 8 for each genotype and treatment). (E) The pancreas was isolated from male control mice and Bmal1 -/- mice. Insulin contents in the tissues were determined by ELISA. The values were corrected by the amount of protein in the tissue. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (F) Response of male control mice and Bmal1 -/- mice to i.p. injection of glibenclamide (2.5 mg/kg). Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). (G) Representative morphology of islets stained with anti-insulin antibody. Scale bars indicate 100 µm. (H) The average cross-sectional area of the islets in Bmal1 -/- mice was compared with that in control mice. Data represent the means ± SEM (n = 4 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(TIF)
Lowered gluconeogenesis activity in the Bmal1 -/- mice liver. All experiments were performed at ZT10. (A) Male control mice and Bmal1 -/- mice were fasted for 16 h. After i.p. injection of pyruvate (2 g/kg), blood glucose levels were monitored. Data represent the means ± SEM (n = 8 for each genotype and point). Asterisks indicate significant differences (P<0.05). Gene expression levels in the liver of male control and Bmal1 -/- mice were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4 level. Data represent the means ± SEM (n = 5 for each genotype). Asterisks indicate significant differences (P<0.05). Levels of G6P and AMP in the liver in male control and Bmal1 -/- mice were determined by capillary electrophoresis time-of-flight mass spectrometry. Data represent the means ± SEM (n = 4 for each genotype). Asterisks indicate significant differences (P<0.05).
(TIF)
Phosphorylation status of HSL in Bmal1 -/- mice adipose tissue. Total HSL protein level and phosphorylated form of HSL protein in the adipose tissue isolated from male control mice and Bmal1 -/- mice at ZT10 were determined by Western blot.
(TIF)
Gene expressions in Bmal1 -/- mice. Gene expressions in control mice and Bmal1 -/- mice were determined by RT-qPCR. Relative mRNA levels were normalized to the 36B4level. N.D. not determined. Each value represented the mean fold-changes (± SEM) of Bmal1 -/- mice in comparison to control mice (n = 5 for each genotype and point). Asterisks indicate significant differences (P<0.05).
(DOC)
Impaired glucose deposition and acceleration of gluconeogenesis in Bmal1 -/- mice.
(DOC)