Abstract
Background
Cognitive performance has been associated with mental and physical health, but it is unknown whether the strength of these associations changes with ageing and with age-related social transitions, such as retirement. We examined whether cognitive performance predicted mental and physical health from midlife to early old age.
Methods
Participants were 5414 men and 2278 women from the Whitehall II cohort study followed for 15 years between 1991 and 2006. The age range included over the follow-up was from 40 to 75 years. Mental health and physical functioning were measured six times using SF-36 subscales. Cognitive performance was assessed three times using five cognitive tests assessing verbal and numerical reasoning, verbal memory, and phonemic and semantic fluency. Socioeconomic status and retirement were included as covariates.
Results
High cognitive performance was associated with better mental health and physical functioning. Mental health differences associated with cognitive performance widened with age from 39 to 76 years of age, while physical functioning differences widened only between 39 and 60 years but not after 60 years of age. Socioeconomic status explained part of the widening differences in mental health and physical functioning before the age of 60. Cognitive performance was more strongly associated with mental health in retired than non-retired participants, which contributed to the widening differences after 60 years of age.
Conclusions
The strength of cognitive performance in predicting mental and physical health may increase from midlife to early old age, and these changes may be related to socioeconomic status and age-related transitions, such as retirement.
Introduction
It is widely accepted that cognitive status in the elderly predicts mortality and functional status (Holland & Rabbitt, 1991). High cognitive performance has been associated with better mental health, e.g., lower risk of psychiatric disorders (Zammit et al. 2004; Hatch et al. 2007; Martin et al. 2007) and the emerging field of cognitive epidemiology has begun to explore the role of cognitive ability in physical health and disease outcomes (Gottfredson, 2004; Deary & Batty, 2007). Good performance on cognitive tests has been shown to be associated with lower mortality (Whalley & Deary, 2001; Hart et al. 2003; Singh-Manoux et al. 2005; Batty, Deary, Gottfredson 2007; Jokela et al. 2009, in press; Sabia et al. in press), better self-reported health, and lower prevalence of chronic diseases (Hart et al. 2004; Schnittker, 2005; Bosma et al. 2007).
Despite the increasing number of cognitive epidemiologic studies, there has been little, if any, research addressing whether the relationship between cognitive performance and health changes over the adult life course, i.e., whether this relationship remains stable, diminishes, or grows stronger with age. This issue is particularly important in understanding the role of cognitive factors in successful aging. Furthermore, it remains unknown whether age-related social transitions, such as retirement, modify associations between cognitive performance and health. Retirement is one of the most important social transitions in late adulthood, as it involves substantial changes in daily life and social environments, and retirement has been associated with health outcomes, mental health gains in particular (Kim & Moen, 2001; Drentea, 2002; Mein et al. 2003).
In the present study using the Whitehall II occupational cohort (Marmot et al. 1991; Marmot & Brunner, 2005), we examined whether cognitive performance predicted mental health and physical functioning differently at different parts of the adult life course from midlife to early old age. Previous studies have shown that social inequalities in health increase with age (Sacker et al. 2005; Chandola et al. 2007). Given that cognitive abilities are known to be associated with socioeconomic status (SES) (Strenze, 2007), we assessed the role of SES in explaining the link between cognitive performance and health. In addition, we examined whether retirement modified the association between cognitive performance and health. Assuming that being retired is less cognitively demanding than work life, we hypothesized that cognitive performance would be less strongly related to health in retired than in non-retired participants.
Methods
Participants
The ongoing longitudinal Whitehall II cohort study has followed a sample (n=10308) of male and female civil servants in London, UK, since 1985–1988 when the participants were 35–55 years of age (Marmot et al. 1991; Marmot & Brunner, 2005). We used data from 6 follow-up phases (phases 3 through 8, collected in 1991–3, 1995–6, 1997–9, 2001–9, 2003–4, and 2006). The participants were 39–64 years of age at baseline for the present study (phase 3) and 50–76 years of age at the most recent follow-up. Thus, different participants provided data across the whole age range (39–76) depending on their age at baseline and year of follow-up. Here we included all participants who provided data at least at one follow-up phase (n=7692; 5414 men, 2278 women). At phases 3, 4, 5, 6, 7, and 8 data were available for 3379, 2994, 5749, 5116, 6180, and 5799 participants, respectively. Thus, the total number of observations used in the multilevel model was 29217. Ethical approval for the Whitehall II study was obtained from the University College London Medical School committee on the ethics of human research.
Cognitive performance
Cognitive performance was measured as the first factor derived from principal component analysis of five standard tests: (1) Verbal memory was assessed by a 20-word free recall test of short-term memory, (2) The AH 4-I 32-item verbal reasoning test (Heim, 1970); (3) The AH 4-I 33-item mathematical reasoning test (Heim, 1970); (4) Phonemic fluency was assessed via “S” words and (5) semantic fluency via “animal” words (Borkowski et al. 1967). In the short-term memory test, participants were presented a list of 20 one or two syllable words at 2-second intervals and were then asked to recall in writing as many of the words in any order within 2 minutes. The AH 4-I is a test of inductive reasoning that measures the ability to identify patterns and infer principles and rules. Participants had 10 minutes to complete this section. In the phonemic and semantic fluency tests, subjects were asked to recall in writing as many words beginning with “S” and as many animal names as they could. One minute was allowed for these tests. Factor analysis of these cognitive tests indicated that the first factor accounted for 59% of the variance in these tests, and this factor score was used as the indicator of cognitive performance in the analyses (Mean=0, SD=1). The factor analysis was performed across phases so that the factor loadings were the same at each phase. Cognitive tests were administered to a subsample of the participants at phase 3 (n=3489) and to all participants at phases 5 (n=5882) and 7 (n=6286).
Mental and physical health
Mental and physical health was assessed using the SF-36 questionnaire (Ware et al. 1993; Ware, 2000) at all six follow-ups from phase 3 to phase 8. In the present study, we used two of the subscales, i.e., mental health and physical functioning, representing the main SF-36 subscales for mental and physical health, respectively (Ware, 2005). The mental health scale includes 5 items assessing psychological wellbeing (e.g., feeling happy, feeling nervous) and the physical functioning scale includes 10 items assessing the ability to carry out daily activities (e.g., difficulties in carrying groceries, difficulties in walking long distances). Both scales were negatively skewed, so they were transformed by cubic transformations, i.e., XT=X3/10000. Following common practice for using the SF-36, the scales were then transformed into T-scores so that the overall mean score across participants and follow-up phases was M=50 (standard deviation=10). The scales were scored so that higher values indicated better health.
Socioeconomic status and retirement
SES was assessed on the basis of the participant’s civil service employment grade (0=low, 1=middle, 2=high) reported by the participants at each phase. For participants who did not have these data (e.g., participants who had retired or were no longer working in the civil service), SES was assigned to be the employment grade at most recent follow-up in which data on grade were provided.
At each follow-up phase, the participants reported whether or not they were retired, and this was used as the indicator of retirement status (0=not retired, 1=retired). Although the statutory retirement age is 60 in the civil service, some participants retired earlier, e.g., voluntarily or due to illness, while others had not retired by age 60, e.g., because they continued to work outside the civil service. Thus, even though retirement status was strongly associated with age, they were not completely collinear (correlations between retirement status and age r=0.53 before age 60 and r=0.57 after age 60; see details of modelling the effects of age below), which allowed us to examine the moderating role of retirement status in addition to the aging effect.
Statistical analysis
We applied multilevel longitudinal modelling (Singer & Willett, 2003; Gelman & Hill, 2007) to evaluate whether cognitive performance predicted the shape of health trajectories over the adult life course. Data were structured so that measurement times (observations at each phase) were nested within individuals, and the standard errors were calculated by taking into account the non-independence of the observations, i.e., that the same individuals contributed more than one observation to the dataset. On average, participants provided data at 4 of the 6 possible follow-up phases. In the multilevel models, regression coefficients are interpreted in the same way as non-standardized coefficients in ordinary linear regression. All predictors, apart from sex, were entered as time-varying covariates. Models included a random term for intercept but we did not include random terms for age or other covariates (data on the random part of the model not shown).
Based on preliminary analysis of the mental health trajectory, we modelled the effect of age using a piecewise approach (Naumova et al. 2001) where the age range (from 39 to 76) was divided into two parts: before and after the age of 60. This was accomplished by creating one age variable for the age period of 39 to 59 (Agebefore 60y, short-handed as Ageb, and 0 otherwise) and another age variable for the age period 60 to 76 (Ageafter 60y, short-handed as Agea, and 0 otherwise). Both of these variables were centred on age 60 (i.e., were equal to age minus 60). Although the average physical functioning trajectory had a different shape than the mental health trajectory, we applied the same piecewise approach in modelling physical functioning, because it provided a flexible model to examine whether cognitive performance predicted health trajectories differently before and after the age of 60.
In order to test whether the association between cognitive performance and health trajectories increased or decreased with age, we assessed interaction effects between cognitive performance and age with each age term included in the model. These interactions were assessed by first testing interaction terms with linear indicators of age and then with quadratic indicators of age. Only significant interaction terms were retained in the models. The interaction effects between SES and health were assessed in the same way. To test whether cognitive performance predicted health differently in retired and in non-retired participants, we assessed interaction effects between cognitive performance and retirement. The results were illustrated by plotting predicted mental health and physical functioning trajectories by age for three selected scores of cognitive performance (1 standard deviation below the mean, the mean value, and 1 standard deviation above the mean).
All models were adjusted for sex and its statistically significant interaction effects with age, i.e., allowing the association between sex and the outcomes to change over time. As data on cognitive performance were not available at phases 4, 6, and 8, we assigned cognitive performance scores assessed at phase 3, 5, and 7 to phases 4, 6, and 8, respectively, in order to include all health outcome measures (assessed at each phase) in modelling the mental and physical health trajectories. Given that different participants were followed over different age periods, the study design allowed the role of period or cohort effects to be taken into account in addition to aging effects. Following previous research from the Whitehall II cohort (Chandola et al. 2007), we decided to adjust for period effects. The multilevel models were fitted using the xtreg command in STATA 9.2 (StataCorp, College Station, TX) statistical program.
Results
Mental health
Preliminary analysis of mental health and age indicated that a model including linear and quadratic effects of age fitted the data well, describing an S-shaped trajectory. On average, mental health increased between 39 and 60 years of age, after which the increase begun to level off. Women had lower mental health than men (table 1).
Table 1.
Predicting mental health trajectories from 40 to 75 years of age by cognitive performance, SES, and retirement status. Beta coefficients (and standard errors) ofnested multilevel models (n=7692)
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Intercept | 56.50* (0.37) | 55.11* (0.48) | 54.53* (0.48) |
| Ageb | 0.63* (0.03) | 0.53* (0.04) | 0.43* (0.04) |
| Ageb2 | 0.02* (0.00) | 0.02* (0.00) | 0.01* (0.00) |
| Agea | 0.33* (0.05) | 0.34* (0.05) | 0.24* (0.05) |
| Agea2 | −0.01* (0.00) | −0.01* (0.00) | −0.01* (0.00) |
| Period | |||
| Phase 3 | (reference) | (reference) | (reference) |
| Phase 4 | −1.57* (0.17) | −1.57* (0.17) | −1.59* (0.17) |
| Phase 5 | −1.78* (0.19) | −1.79* (0.19) | −1.79* (0.19) |
| Phase 6 | −2.25* (0.22) | −2.26* (0.22) | −2.26* (0.22) |
| Phase 7 | −2.74* (0.24) | −2.80* (0.24) | −2.72* (0.24) |
| Phase 8 | −2.47* (0.28) | −2.53* (0.28) | −2.46* (0.28) |
| Sex | −2.45* (0.21) | −2.15* (0.23) | −2.17* (0.23) |
| Cognitive performance | 0.50* (0.12) | 0.21 (0.13) | 0.00 (0.14) |
| Cognitive performance × Ageb | 0.05* (0.01) | 0.02 (0.01) | 0.00 (0.02) |
| Cognitive performance × Agea | 0.05* (0.02) | 0.05* (0.02) | 0.02 (0.02) |
| SES | 0.35* (0.07) | 0.35* (0.07) | |
| SES × Ageb | 0.03* (0.01) | 0.03* (0.01) | |
| Retirement | 0.55* (0.13) | ||
| Retirement × cognitive performance | 0.55* (0.14) | ||
Note:
p<0.05 level (minimum). Ageb=Age before 60y; Agea=Age after 60y; Sex: 0=men, 1=women; Retirement:0=not retired, 1=retired. The main effect of cognitive performance refers to 60-year-olds (model 1), low-SES (model 2), and non-retired (model 3) participants. Mental health is scored as a T-score (M=50, SD=10).
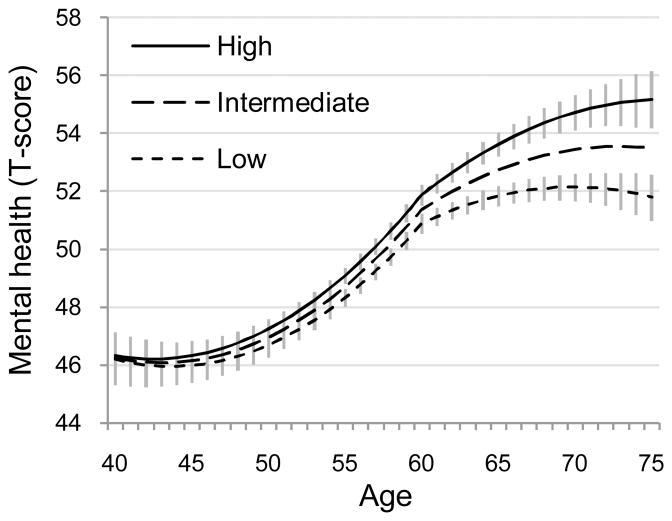
Interaction effects between cognitive performance and age before and after 60 years (table 1, model 1) indicated that the association between cognitive performance and mental health increased with age (figure 1). The predicted mental health scores in those with high (+1 SD) compared to low (−1 SD) cognitive performance levels was better by 0.5, 1.0, and 2.6 units at 50, 60, and 70 years of age, respectively.
Figure 1.
Predicted mental health trajectories (and 95% confidence intervals) by levels of cognitive performance (low=1SD below the mean, intermediate= mean, high=1SD above the mean). For clarity, the 95% confidence intervals (vertical lines) are not shown for the intermediate group.
The association between cognitive performance and health was accounted, in part, by SES (table 1, model 2). In an analysis that included cognitive performance and other covariates in the model, there was a significant interaction effect between SES and age before 60 years but not between SES and age after 60 years (B=0.00, SE=0.03, p=0.99; not included in the model), suggesting widening mental health differences associated with SES before age 60 years. Including SES and its interaction effect with age in the model attenuated the interaction between cognitive performance and age before 60 years (table 1, model 2), indicating that SES accounted for the mental health differences associated with cognitive performance before but not after age 60.
We found evidence to suggest that retirement modified the association between cognitive performance and mental health (table 1, model 3). There was an interaction effect between cognitive performance and retirement indicating that cognitive performance was associated with mental health more strongly in retired than in non-retired participants. Inclusion of this interaction term in the model attenuated the interaction effect between cognitive performance and age after 60 years. In other words, the widening mental health differences associated with cognitive performance after the age of 60 were related to retirement becoming more common, as retirement strengthened the association between cognitive performance and mental health.
Physical functioning
We then repeated the above analysis with physical functioning as the dependent variable. Physical functioning scores declined with age and this decline accelerated after the age of 60, as indicated by the significant quadratic effect of age after 60 years (table 2, model 1). Women had lower physical functioning than men. The effects of period on physical functioning were not consistent across the phases.
Table 2.
Predicting physical functioning trajectories from 40 to 75 years of age by cognitive performance, SES, and retirement status. Beta coefficients (and standard errors) of nested multilevel models (n=7692).
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Intercept | 55.35* (0.36) | 52.67* (0.46) | 52.58* (0.46) |
| Ageb | −0.28* (0.02) | −0.37* (0.03) | −0.38* (0.03) |
| Agea | −0.17* (0.04) | −0.18* (0.04) | −0.20* (0.04) |
| Agea2 | −0.02* (0.00) | −0.02* (0.00) | −0.02* (0.00) |
| Period | |||
| Phase 3 | (reference) | (reference) | (reference) |
| Phase 4 | −0.56* (0.16) | −0.56* (0.16) | −0.55* (0.16) |
| Phase 5 | 0.00 (0.17) | 0.04 (0.17) | 0.06 (0.17) |
| Phase 6 | −0.62* (0.20) | −0.58* (0.20) | −0.57* (0.20) |
| Phase 7 | −0.09 (0.23) | −0.17 (0.23) | −0.14 (0.23) |
| Phase 8 | 0.29 (0.26) | 0.22 (0.26) | 0.24 (0.26) |
| Sex | −4.55* (0.21) | −3.88* (0.22) | −3.89* (0.22) |
| Cognitive performance | 1.63* (0.10) | 1.14* (0.11) | 1.15* (0.11) |
| Cognitive performance × Ageb | 0.06* (0.01) | 0.03* (0.01) | 0.03* (0.01) |
| SES | 0.64* (0.07) | 0.64* (0.07) | |
| SES × Ageb | 0.03* (0.01) | 0.03* (0.01) | |
| Retirement | 0.24* (0.12) | ||
Note:
p<0.05 level (minimum). Ageb=Age before 60y; Agea=Age after 60y; Sex: 0=men, 1=women; Retirement: 0=not retired, 1=retired. The main effect of cognitive performance refers to 60-year-olds (model 1), low-SES (model 2), and non-retired (model 3) participants. Physical functioning is scored as a T-score (M=50, SD=10).
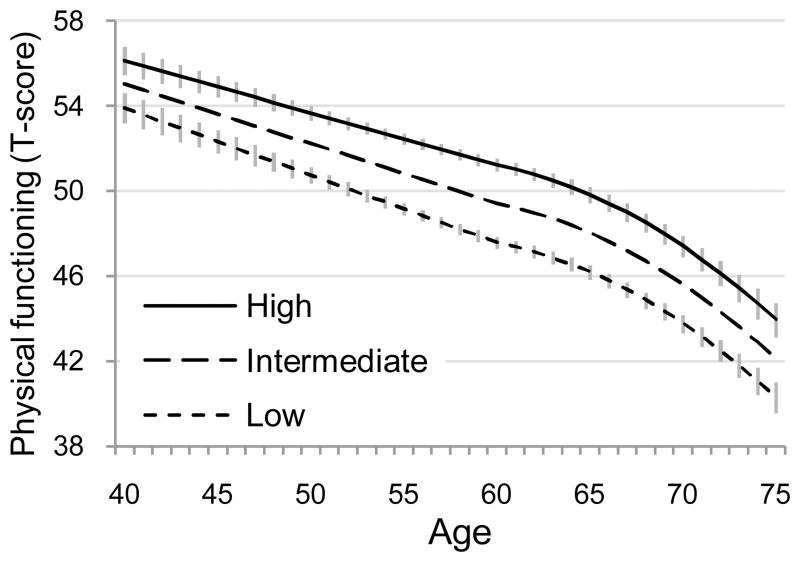
There was a significant interaction effect between cognitive performance and age before 60 years but not with other age indicators (model 1), indicating that physical functioning differences associated with cognitive performance increased with age only before but not after the age of 60 (figure 2). The predicted difference between high and low cognitive performance groups was 2.2, 2.8, 3.6, and 3.6 units at ages 40, 50, 60, and 70, respectively.
Figure 2.
Predicted physical functioning trajectories (and 95% confidence intervals) by levels of cognitive performance (low=1SD below the mean, intermediate= mean, high=1SD above the mean). The 95% confidence intervals (vertical lines) are shown only for the high and low groups.
Table 2 (model 2) shows that there was an interaction effect between SES and age before 60 but not after 60 (B=0.01, SE=0.02, p=0.82; not included in the model) indicating that physical functioning differences associated with SES increased before but not after age 60. Inclusion of this interaction effect halved the magnitude of the interaction between cognitive performance and agebefore 60, suggesting that the widening differences in physical functioning between participants with high and low cognitive performance were partially explained by differences in SES. There was no interaction effect between cognitive performance and retirement (table 3, model 3). Thus, retirement did not modify the association between cognitive performance and physical functioning (p-value for interaction = 0.56; not included in the model).
Attrition analysis
Attrition analysis suggests that our findings are not biased by selective attrition. For each phase, we created a dichotomous variable indicating whether or not the participant had data at the next phase. We then fitted a multilevel logistic model in order to predict this probability for cognitive performance, mental health, and physical functioning, in analysis adjusted for sex, period, and linear terms for age. Higher probability of attrition was associated with lower cognitive performance (standardized OR=0.71, SE=0.02, p<0.001), poorer mental health (standardized OR=0.89, SE=0.02, p<0.001), and poorer physical functioning (standardized OR=0.86, SE=0.02, p<0.001). However, these attrition patterns did not contribute to the widening associations between cognitive performance and health because, if anything, the attrition attenuated rather than strengthened the estimated associations. For instance, regressing mental health on cognitive performance at phase 5 (adjusted for sex and age) in all participants who had data at phase 5 yielded the coefficient of B=1.27 (SE=0.34, p<0.001; n=5776). When the same linear regression model was fitted in participants who had data at phases 5 and 6 (i.e., excluding drop-outs between phases 5 and 6), the regression coefficient was B=1.01 (SE=0.36, p<0.001; n=5033). A similar, small attenuation effect was evident at other follow-up phases (data not shown).
Discussion
Findings from the longitudinal Whitehall II occupational cohort indicate that the importance of cognitive performance in predicting adult mental health and physical functioning may increase with age, resulting in widening health differences associated with cognitive performance. On average, cognitive performance was more strongly related to physical functioning than to mental health. However, the age-related changes in these associations were more pronounced for mental health than for physical functioning: mental health differences associated with cognitive performance widened with age from 39 to 76 years of age, while the physical functioning differences widened only between 39 and 60 years but not after 60 years of age.
Methodological strengths of the study include a large sample size and a longitudinal design with repeated measures of cognitive performance and health outcomes. Attrition analyses suggested that although cognitive performance and health measures were associated with selective attrition, the selective attrition in question was unlikely to contribute to the widening health differences associated with cognitive performance observed in the data. The main caveat to our findings is that the participants were from an occupational cohort which may limit the generalizability of the findings.
Performance in cognitive tests has been shown to predict a wide range of mental and physical health outcomes (e.g., Bosma et al. 2007; Der, Batty, Deary, in press; Gale et al. in press; Hart et al. 2004). Although this association has been observed in samples representing different age periods in adulthood, there appear to be no previous longitudinal studies examining this association at different ages in the same sample. The widening health differences observed in our data are therefore novel and imply that cognitive performance may become a more salient correlate of health at older ages.
There are at least four plausible mechanisms that may explain associations between cognitive performance and health (Whalley & Deary, 2001; Batty, Deary, Gottfredson 2007; Gottfresdon & Deary, 2004) and these could be extended to explain the effects of age observed in this study. First, cognitive performance and health may share a common cause, and such a common cause might account for the present findings if its impact were increasingly evident with age. For instance, vascular risk factors, e.g., hypertension, coronary heart disease, and dyslipidaemia, become more prevalent with age and they have been associated with both cognitive performance (Singh-Manoux & Marmot, 2005; Singh-Manoux et al. 2008; Singh-Manoux et al. in press) and health (Rugulies, 2002; Kumari et al. 2004).
Second, cognitive performance may be related to health behaviours (Batty, Deary, Macintyre 2007; Batty, Deary, Schoon et al 2007). In this case, one would expect any association between cognitive performance and health, physical health in particular, to strengthen as physical illnesses associated with adverse health behaviours become more prevalent with age. However, as we observed widening differences in physical functioning before but not after the age of 60, this seems an unlikely explanation of our findings. Third, in spite of the prospective study design, the association between cognitive performance and health may reflect reverse causality, i.e., cognitive performance may be affected by mental and physical health (Yaffe et al. 1999; Ganguli et al. 2006; Chodosh et al. 2007; Dotson et al. 2008).
Fourth, cognitive performance may predict selection into more “healthy” social environments, e.g., high SES (Batty, Deary, Gottfredson 2007; Batty et al. 2008; Jokela et al. 2009) or be a marker of such environments. Previous research in the present and other cohorts suggests that health inequalities associated with SES may increase with age (Sacker et al. 2005; Chandola et al. 2007). In agreement with these observations, we found that before the age of 60 SES explained the increasing role of cognitive performance either completely (in the case of mental health) or in part (in the case of physical functioning). However, SES did not attenuate the association between cognitive performance and health after age 60, implying that socioeconomic circumstances may be relevant in explaining the cognition-health association primarily in working-age populations. Alternatively, the SES measure used in the present study, employment grade, may have failed to capture post-retirement socioeconomic conditions completely, so the lack of attenuation might be caused by residual confounding.
Contrary to our hypothesis, cognitive performance predicted mental health more strongly in retired than in non-retired participants. This finding suggests that retirement might involve cognitively challenging social changes, as retiring individuals reorganize their lives and adjust to new daily activities without the structure of work that has characterized most of their adult lives (Kim & Moen, 2001). The modifying role of retirement accounted for the widening differences in mental health after the age of 60. That is, mental health differences associated with cognitive performance became more pronounced as more participants became retired. Retirement did not moderate the association between cognitive performance and physical functioning, indicating that the changing circumstances related to retirement may not be as relevant for physical health in early old age.
The observed associations between cognitive performance and health trajectories need to be interpreted keeping in mind the examined age range of 39 to 76 years. On average, mental health was at its lowest level between ages 45 and 50 and began to increase after this age period, while physical functioning decreased consistently between the ages of 39 and 76 years. Thus, cognitive performance was associated with a steeper age-related increase in mental health and a less steep decline in age-related physical functioning. This suggests that high cognitive performance may be associated with both health gains and health losses related to aging. However, it is noteworthy that these were only modifications of a general age-related trend because individuals with different levels of cognitive performance all followed the same general mental health and physical functioning trajectories. Further research is needed to assess whether the relationship of cognitive performance with mental and physical health reflect common or separate underlying mechanisms.
In sum, the present findings indicate that the association between cognitive performance and health may be dependent on age and age-related social transitions. Our data suggest that cognitive epidemiology, the study of the role of cognition on health (Deary & Batty, 2007), would benefit from closer attention to the role played by aging in shaping this association across the life course. This is particularly relevant as the importance of multiple psychological and social factors in explaining the cognition-health association is likely to vary over the life course. Future research should assess the extent to which other social (and biological) factors, in addition to SES and retirement, contribute to these age-related changes.
Acknowledgments
The Whitehall II study has been supported by grants from the British Medical Research Council (MRC); the British Heart Foundation; the British Health and Safety Executive; the British Department of Health; the National Heart, Lung, and Blood Institute (grant HL36310); the National Institute on Aging (grant AG13196); the Agency for Health Care Policy and Research (grant HS06516); and the John D. and Catherine T. Mac Arthur Foundation Research Networks on Successful Midlife Development and Socioeconomic Status and Health. MK was supported by the Academy of Finland (grants no: 117604, 124322, and 124271). JEF was supported by the Medical Research Council (grant G8802774), ASM by a “European Young Investigator Award” by the European Science Foundation, MJS by the British Heart Foundation and MGM by an MRC Research Professorship.
Footnotes
Declaration of interest: None of the authors has competing interests.
References
- Batty GD, Deary IJ, Gottfredson LS. Premorbid (early life) IQ and later mortality risk: systematic review. Annals of Epidemiology. 2007;17:278–288. doi: 10.1016/j.annepidem.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Batty GD, Deary IJ, Macintyre S. Childhood IQ in relation to risk factors for premature mortality in middle-aged persons: the Aberdeen Children of the 1950s study. Journal of Epidemiology and Community Health. 2007;61:241–247. doi: 10.1136/jech.2006.048215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty GD, Deary IJ, Schoon I, Gale CR. Mental ability across childhood in relation to risk factors for premature mortality in adult life: the 1970 British Cohort Study. Journal of Epidemiology and Community Health. 2007;61:997–1003. doi: 10.1136/jech.2006.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty GD, Shipley MJ, Mortensen LH, Boyle SH, Barefoot J, Grønbaek M, Gale CR, Deary IJ. IQ in late adolescence/early adulthood, risk factors in middle age and later all-cause mortality in men: the Vietnam Experience Study. Journal of Epidemiology and Community Health. 2008;62:522–531. doi: 10.1136/jech.2007.064881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkowski JG, Benton AL, Spreen O. Word fluency and brain damage. Neurophysiologia. 1967;5:135–140. [Google Scholar]
- Bosma H, van Boxtel MP, Kempen GI, van Eijk JT, Jolles J. To what extent does IQ ‘explain’ socio-economic variations in function? BMC Public Health. 2007;25:179. doi: 10.1186/1471-2458-7-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandola T, Ferrie J, Sacker A, Marmot M. Social inequalities in self reported health in early old age: follow-up of prospective cohort study. British Medical Journal. 2007;334:990. doi: 10.1136/bmj.39167.439792.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chodosh J, Kado DM, Seeman TE, Karlamangla AS. Depressive symptoms as a predictor of cognitive decline: MacArthur Studies of Successful Aging. American Journal of Geriatric Psychiatry. 2007;15:406–415. doi: 10.1097/01.JGP.0b013e31802c0c63. [DOI] [PubMed] [Google Scholar]
- Deary IJ, Batty GD. Cognitive epidemiology. Journal of Epidemiology and Community Health. 2007;61:378–384. doi: 10.1136/jech.2005.039206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der G, Batty GD, Deary IJ. The association between IQ in adolescence and a range of health outcomes at 40 in the 1979 US National Longitudinal Study of Youth. Intelligence. doi: 10.1016/j.intell.2008.12.002. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson VM, Resnick SM, Zonderman AB. Differential association of concurrent, baseline, and average depressive symptoms with cognitive decline in older adults. American Journal of Geriatric Psychiatry. 2008;16:318–330. doi: 10.1097/JGP.0b013e3181662a9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drentea P. Retirement and mental health. Journal of Aging and Health. 2002;14:167–194. doi: 10.1177/089826430201400201. [DOI] [PubMed] [Google Scholar]
- Ganguli M, Du Y, Dodge HH, Ratcliff GG, Chang CC. Depressive symptoms and cognitive decline in late life: a prospective epidemiological study. Archives of General Psychiatry. 2006;63:153–160. doi: 10.1001/archpsyc.63.2.153. [DOI] [PubMed] [Google Scholar]
- Gale CR, Hatch SL, Batty GD, Deary IJ. Intelligence in childhood and risk of psychological distress in adulthood: The 1958 National Child Development Survey and the 1970 British Cohort Study. Intelligence (in press) [Google Scholar]
- Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- Gottfredson LS. Intelligence: is it the epidemiologists’ elusive “fundamental cause” of social class inequalities in health? Journal of Personality and Social Psychology. 2004;86:174–199. doi: 10.1037/0022-3514.86.1.174. [DOI] [PubMed] [Google Scholar]
- Gottfredson LS, Deary IJ. Intelligence predicts health and longevity, but why? Current Directions in Psychological Science. 2004;13:1–4. [Google Scholar]
- Hart CL, Taylor MD, Davey Smith G, Whalley LJ, Starr JM, Hole DJ, Wilson V, Deary IJ. Childhood IQ, social class, deprivation, and their relationships with mortality and morbidity risk in later life: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Psychosomatic Medicine. 2003;65:877–883. doi: 10.1097/01.psy.0000088584.82822.86. [DOI] [PubMed] [Google Scholar]
- Hart CL, Taylor MD, Smith GD, Whalley LJ, Starr JM, Hole DJ, Wilson V, Deary IJ. Childhood IQ and cardiovascular disease in adulthood: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Social Science & Medicine. 2004;59:2131–2138. doi: 10.1016/j.socscimed.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Hatch SL, Jones PB, Kuh D, Hardy R, Wadsworth ME, Richards M. Childhood cognitive ability and adult mental health in the British 1946 birth cohort. Social Science & Medicine. 2007;64:2285–2296. doi: 10.1016/j.socscimed.2007.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heim AW. AHA4 group test for general intelligence ASE. NFER-Nelson Publishing Co.Ltd; 1970. [Google Scholar]
- Holland CA, Rabbitt PMA. The course and causes of cognitive change with advancing age. Reviews in Clinical Gerontology. 1991;1:81–86. [Google Scholar]
- Jokela M, Elovainio M, Singh-Manoux A, Kivimäki M. IQ, socioeconomic status, and early mortality: The U.S National Longitudinal Survey of Youth. Psychosomatic Medicine. 2009;71:322–328. doi: 10.1097/PSY.0b013e31819b69f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokela M, Batty GD, Deary IJ, Gale CR, Kivimäki M. Childhood IQ and early mortality: Assessing the role of childhood and adult risk factors in the 1958 British birth cohort. Pediatrics. doi: 10.1542/peds.2009-0334. (in press) [DOI] [PubMed] [Google Scholar]
- Kim JE, Moen P. Is retirement good or bad for subjective well-being? Current Directions in Psychological Science. 2001;10:83–86. [Google Scholar]
- Kumari M, Seeman T, Marmot M. Biological predictors of change in functioning in the Whitehall II study. Annals of Epidemiology. 2004;14:250–257. doi: 10.1016/j.annepidem.2003.09.011. [DOI] [PubMed] [Google Scholar]
- Marmot M, Brunner E. Cohort Profile: the Whitehall II study. International Journal of Epidemiology. 2005;34:251–256. doi: 10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Davey Smith G, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Martin LT, Kubzansky LD, LeWinn KZ, Lipsitt LP, Satz P, Buka SL. Childhood cognitive performance and risk of generalized anxiety disorder. International Journal of Epidemiology. 2007;36:769–775. doi: 10.1093/ije/dym063. [DOI] [PubMed] [Google Scholar]
- Mein G, Martikainen P, Hemingway H, Stansfeld S, Marmot M. Is retirement good or bad for mental and physical health functioning? Whitehall II longitudinal study of civil servants. Journal of Epidemiology and Community Health. 2003;57:46–49. doi: 10.1136/jech.57.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naumova EN, Must A, Laird NM. Tutorial in biostatistics: Evaluating the impact of ‘critical periods’ in longitudinal studies of growth using piecewise mixed effects models. International Journal of Epidemiology. 2001;30:1332–1341. doi: 10.1093/ije/30.6.1332. [DOI] [PubMed] [Google Scholar]
- Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. American Journal of Preventive Medicine. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- Sabia S, Guéguen A, Marmot MG, Shipley MJ, Ankri J, Singh-Manoux A. Does cognition predict mortality in midlife? Results from the Whitehall II cohort study. Neurobiology of Aging. doi: 10.1016/j.neurobiolaging.2008.05.007. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacker A, Clarke P, Wiggins RD, Bartley M. Social dynamics of health inequalities: a growth curve analysis of aging and self assessed health in the British household panel survey 1991–2001. Journal of Epidemiology and Community Health. 2005;59:495–501. doi: 10.1136/jech.2004.026278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J. Cognitive abilities and self-rated health: Is there a relationship? Is it growing? Does it explain disparities? Social Science Research. 2005;34:821–842. [Google Scholar]
- Singer JB, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- Singh-Manoux A, Ferrie JE, Lynch JW, Marmot M. The role of cognitive ability (intelligence) in explaining the association between socioeconomic position and health: Evidence from the Whitehall II prospective cohort study. American Journal of Epidemiology. 2005;161:831–839. doi: 10.1093/aje/kwi109. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Gimeno D, Kivimäki M, Brunner E, Marmot MG. Low HDL cholesterol is a risk factor for deficit and decline in memory in midlife: the Whitehall II study. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28:1556–1562. doi: 10.1161/ATVBAHA.108.163998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot M. High blood pressure was associated with cognitive function in middle-age in the Whitehall II study. Journal of Clinical Epidemiology. 2005;58:1308–1315. doi: 10.1016/j.jclinepi.2005.03.016. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Sabia S, Lajnef M, Ferrie JE, Nabi H, Britton AR, Marmot MG, Shipley MJ. History of coronary heart disease and cognitive performance in midlife: the Whitehall II study. European Heart Journal. doi: 10.1093/eurheartj/ehn298. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strenze T. Intelligence and socioeconomic success: A meta-analytic review of longitudinal research. Intelligence. 2007;35:401–426. [Google Scholar]
- Ware JE., Jr SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health survey manual and interpretation guide. Boston: New England Medical Center; 1993. [Google Scholar]
- Whalley LJ, Deary IJ. Longitudinal cohort study of childhood IQ and survival up to age 76. British Medical Journal. 2001;322:819. doi: 10.1136/bmj.322.7290.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K, Blackwell T, Gore R, Sands L, Reus V, Browner WS. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Archives of General Psychiatry. 1999;56:425–430. doi: 10.1001/archpsyc.56.5.425. [DOI] [PubMed] [Google Scholar]
- Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, Lewis G. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Archives of General Psychiatry. 2004;61:354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]