Abstract
Allergic reactions to local anesthetics are very rare and represent <1% of all adverse local anesthetics reactions. A 54-year-old man was admitted to the hospital in the winter because of shortness of breath. The patient reportedly had an inhalation lung injury due to butane gas fuel. On the fifth day, he developed an asthmatic attack and anaphylactic shock immediately after lidocaine aerosol administration to prepare for bronchoscopy to confirm an acute inhalational lung injury diagnosis. Cardiopulmonary resuscitation was performed immediately after respiratory arrest, and the patient was admitted to the intensive care unit intubated and on a ventilator. He was extubated safely on the third post-cardiopulmonary resuscitation day. These observations suggest that aerosol lidocaine anesthesia may cause airway narrowing and anaphylactic shock. Practitioners should be aware of this potential complication. We report on this case with a brief review of the literature.
Keywords: Anaphylaxis, immediate hypersensitivity, inhalation, lidocaine
INTRODUCTION
Allergic reactions to local anesthetics are very rare and represent <1% of all adverse local anesthetics reactions.1-4 Contact dermatitis is the most commonly reported allergic reaction to several amide-type local anesthetics.5-7 Adverse local anesthetic-induced reactions through an IgE-mediated allergic mechanism (type I reaction) are still debated.5-8 Butane is a gas with the formula C4H10.9 When oxygen is plentiful, butane burns to form carbon dioxide and water vapor; when oxygen is limited, carbon (soot) or carbon monoxide may also be formed. Butane inhalation can cause euphoria, drowsiness, narcosis, asphyxia, cardiac arrhythmias, and frostbite, which can result in death from asphyxiation and ventricular fibrillation. We report a case of immediate lidocaine hypersensitivity following local anesthesia in a patient with a butane gas inhalation lung injury.
CASE REPORT
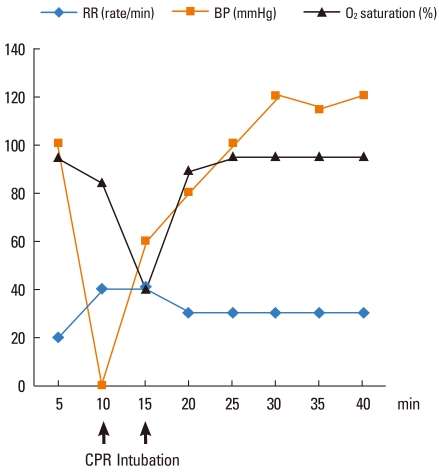
A 54-year-old man presented to the hospital with dyspnea after inhaling butane gas while melting a water pipe during winter. On physical examination, late inspiratory crackles were evident in both auscultated lower lung fields. His history showed no lidocaine allergy, allergic rhinitis, asthma, or allergies to other drugs. On examination, blood pressure was 125/75 mmHg, pulse was 65 beats per minute, oral temperature was 36.5℃, respiratory rate was 18 breaths per minute, oxygen saturation was 76.0%, pH was 7.27, PaO2 was 46.0 mmHg, and PaCO2 was 47.2 mmHg, as the patient breathed ambient air. Total IgE was 129 kU/L. An electrocardiogram revealed a normal sinus rhythm. A pulmonary function test revealed forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) of 78%, FVC of 2.24 L (60%), FEV1 of 1.75 L (62%), and a diffusing capacity for carbon momoxide of 15.1 mL/mmHg (71%) indicating a restrictive pattern. Chest radiographs revealed bilateral patchy opacities, more in the right lung than in the left lung. Computed tomography of the chest revealed multifocal consolidation and ground-glass opacities in all lobes of both lungs, indicating an acute inhalation lung injury (Fig. 1). The patient recovered after oxygen and supportive care. On the fifth day, we planned to conduct a bronchoscopy to diagnose an inhalational lung injury. We used lidocaine aerosol as local anesthesia for reducing the gag reflex. After administering the lidocaine anesthesia, the patient complained of dizziness without urticaria and angioedema and shortness of breath, which was associated with an increased respiratory rate and decreased oxygen saturation. Coarse expiratory wheezes were auscultated on a physical examination. Blood pressure subsequently dropped, and a radial pulse was not palpable. The patient was treated with nebulized salbutamol and systemic steroid. However, the patient did not recover, and blood pressure continued to decrease accompanied by an increase in respiratory rate and a decrease of oxygen saturation (Fig. 2) followed by cardiorespiratory arrest. Cardiopulmonary resuscitation (CPR) with epinephrine, inotropics, and fluid therapy was performed immediately, and the patient was admitted to the intensive care unit under tracheal intubation and ventilator treatment. After 2 hours, his CPR tryptase level was 1.68 µg/L. He was extubated safely on the third post-CPR day.
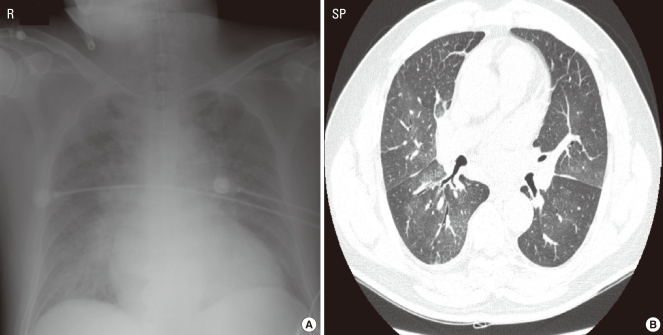
Fig. 1.
(A) Chest radiographs revealed bilateral patchy opacities. (B) Computed tomography of the chest revealed multifocal consolidation and ground-glass opacities in all lobes of both lungs as well as right pleural effusion, indicating an acute inhalation lung injury.
Fig. 2.
Changes in oxygen saturation, respiratory rate, and blood pressure. CPR, cardiopulmonary resuscitation.
DISCUSSION
Local anesthetics are among the most commonly used drugs in clinical medicine; however, a variety of adverse drug reactions have been reported.1-5 Acute disorientation or seizures may occur after overdosing or inadvertent intravenous injection. Many local anesthetics contain adrenaline or other excipients such as anti-oxidants or preservatives (bisulphites, parabens, carboxymethylcellulose, and para-aminobenzoic acid). Local anesthetics can also produce sympathetic effects (tachycardia or arterial hypertension) irrespective of the presence or absence of vasoconstricting agents.5 Immunological reactions to local anesthetics, particularly the newer amides, remain anecdotal, and symptoms usually result from vasovagal episodes or anxiety reactions.5
Allergic reactions to local anesthetics occur mostly in young people, and female gender is involved in the majority of cases.1,2 Lidocaine is the most often used local anesthetic involved in such reactions, because it is the most commonly used in clinical practice.1-5 Allergic reactions after an intravenous injection of local anesthetic include contact dermatitis, which most often shows cutaneous signs such as erythema, pruritus, urticaria, or eczema that occur between 6 hours and 1 month after administration.5 True type I allergic reactions are reported in <1% of local anesthetic adverse drug reactions.6,7 In a large French survey reporting the incidence of anaphylaxis during anesthesia over a 2-year period, local anesthetics were involved in only one case (0.2%). Three cases of lidocaine anaphylaxis have been reported in the literature in Korea.10
In this case, the anaphylaxis and asthma attack may have been an immediate hypersensitivity reaction. Notably, all amide-type local anesthetics are associated with inhalation and not epidural, local anesthesia, or peripheral nerve blocks. Lidocaine and mepivacaine are involved in immediate hypersensitivity allergic reactions.1,8
A diagnosis of true allergic reactivity is difficult because the history of a prior reaction may be equivocal and the inability to identify the actual specific local anesthetic hapten-carrier complex limits the potential usefulness of immunological tests.4 In addition to general principles regarding the diagnostic approach, history taking, and the importance of quantifying tryptase, more specific confirmatory diagnostic procedures are organized based on the major causes of perioperative anaphylactic reactions.5 This patient showed normal total IgE and tryptase levels. An allergic skin test using lidocaine was not conducted; therefore, lidocaine, preservatives, and other additives could not be excluded.
Butane gas is sold bottled as a fuel for cooking and camping. Spraying butane directly into the throat can cool it rapidly to -20℃ by expansion, causing prolonged laryngospasm and sudden sniffer's death syndrome, resulting in 55% of the known fatal cases.9
Our patient developed dyspnea 5 min after using butane gas fuel to thaw a water supply device. The diagnosis was an inhalation lung injury, suggesting that butane gas inhalation can induce an acute inhalation lung injury.
Correct management of anaphylaxis during anesthesia requires a multidisciplinary approach with prompt recognition and treatment of the acute event by the attending doctors and subsequent identification of the responsible agent(s) with strict avoidance of subsequent administration of all incriminated and/or cross-reacting compounds.5
In conclusion, although allergic reactions to local anesthetics are very rare, this case suggests that aerosol lidocaine anesthesia may cause airway narrowing and anaphylactic shock as a potentially life-threatening complication. Practitioners should be aware of this potential complication.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Fuzier R, Lapeyre-Mestre M, Mertes PM, Nicolas JF, Benoit Y, Didier A, Albert N, Montastruc JL French Association of Regional Pharmacovigilance Centers. Immediate- and delayed-type allergic reactions to amide local anesthetics: clinical features and skin testing. Pharmacoepidemiol Drug Saf. 2009;18:595–601. doi: 10.1002/pds.1758. [DOI] [PubMed] [Google Scholar]
- 2.Mertes PM, Laxenaire MC. Allergic reactions occurring during anaesthesia. Eur J Anaesthesiol. 2002;19:240–262. doi: 10.1017/s0265021502000418. [DOI] [PubMed] [Google Scholar]
- 3.Laxenaire MC, Mertes PM Groupe d'Etudes des Réactions Anaphylactoïdes Peranesthésiques. Anaphylaxis during anaesthesia. Results of a two-year survey in France. Br J Anaesth. 2001;87:549–558. doi: 10.1093/bja/87.4.549. [DOI] [PubMed] [Google Scholar]
- 4.Schatz M. Skin testing and incremental challenge in the evaluation of adverse reactions to local anesthetics. J Allergy Clin Immunol. 1984;74:606–616. doi: 10.1016/0091-6749(84)90114-3. [DOI] [PubMed] [Google Scholar]
- 5.Ebo DG, Fisher MM, Hagendorens MM, Bridts CH, Stevens WJ. Anaphylaxis during anaesthesia: diagnostic approach. Allergy. 2007;62:471–487. doi: 10.1111/j.1398-9995.2007.01347.x. [DOI] [PubMed] [Google Scholar]
- 6.Cuesta-Herranz J, de las Heras M, Fernández M, Lluch M, Figueredo E, Umpierrez A, Lahoz C. Allergic reaction caused by local anesthetic agents belonging to the amide group. J Allergy Clin Immunol. 1997;99:427–428. doi: 10.1016/s0091-6749(97)70064-2. [DOI] [PubMed] [Google Scholar]
- 7.Astarita C, Gargano D, Romano C, Cutajar M, Manguso F, Montanaro D, Napolitano A, Pezzuto F, Lo Schiavo M, Altucci P, Abbate G. Long-term absence of sensitization to mepivacaine as assessed by a diagnostic protocol including patch testing. Clin Exp Allergy. 2001;31:1762–1770. doi: 10.1046/j.1365-2222.2001.01226.x. [DOI] [PubMed] [Google Scholar]
- 8.Gall H, Kaufmann R, Kalveram CM. Adverse reactions to local anesthetics: analysis of 197 cases. J Allergy Clin Immunol. 1996;97:933–937. doi: 10.1016/s0091-6749(96)80067-4. [DOI] [PubMed] [Google Scholar]
- 9.Ramsey J, Anderson HR, Bloor K, Flanagan RJ. An introduction to the practice, prevalence and chemical toxicology of volatile substance abuse. Hum Toxicol. 1989;8:261–269. doi: 10.1177/096032718900800403. [DOI] [PubMed] [Google Scholar]
- 10.In JH, Choi JW, Joo JD, Kim DW, Jung HS, Park HJ. Intraoperative anaphylaxis after local infiltration of lidocaine for dental treatment under general anesthesia -A case report. Korean J Anesthesiol. 2008;55:395–398. [Google Scholar]